![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
71 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
what is meant by homeostasis |
Homeostasis- the maintenance of a constant internal environment of a living organism irrespective of the external conditions |
|
|
|
Give 3 examples of homeostatic control |
-osmoregulation -thermoregulation -blood glucose levels (endocinine system controls) |
|
|
|
what effect might a change in temperature and pH have on an enzyme catalysed reaction |
extreme temperature and pH away from the optimum set point can cause the enzymes to denature. The 3D globular structure of the enzymes change shape irreversibly. This causes a change in shape of the active site, the substrate and active site are no longer complementary and no enzyme-substrate complexes are formed. Rate of reaction decreases as no products are made/broken down. |
|
|
|
What is meant by 'The body is kept in a dynamic equilibrium' |
Changes in pH , temperature and solute potentials may occur but fluctuate around the set point. Homeostasis is the ability to return to the set point. |
|
|
|
Definition: Negative feedback |
a change in a system produces a second change, which reverses the first change |
|
|
|
What are the differences between negative feedback and positive feedback? what do they have in common? |
negative feedback- it is the output from an effector (e.g. muscle or glands) which REDUCES the effect of a stimulus positive feedback- it is the output from an effector which INCREASES a change Their intention is to return the system to its set point |
|
|
|
What is meant by set point? |
The set point for a factor is the norm at which a system operates
|
|
|
|
How does negative feedback work? |
1) the set point for a factor is the norm at which a system operates 2) A receptor detects a change in the levels of the factor and its deviation from the set point 3) the receptor sends instructions to a coordinator- control centre 4) The control centre communicates with one or more effectors (muscle or glands). This creates a response designed to take away the deviation 5) The set point is restored, this is monitored by the receptor, instructions are sent to the effector to stop making the response |
|
|
|
Give 2 examples of positive feedback |
OXYTOCIN- oxytocin stimulates the contraction of the uterus at the end of pregnancy. The contractions stimulate the production of more oxytocin Paper cut- When you cut yourself, the first stage of blood clotting is that the platelets adhere to the surface of the cut. They secrete signalling molecules, which attract more platelets |
oxytocin, paper cut |
|
|
Complete the flow diagram for thermoregulation: Set point > Receptor > control centre > Effector |
Set point- 37 degrees Receptor- thermo-receptors and cutaneous Control centre- hypothalamus effector- smooth muscle in the wall of the arteriole |
|
|
|
Definition: Excretion
|
the removal of metabolic waste made by the body |
|
|
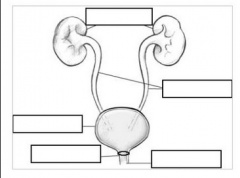
Label the human urinary system |
Top from bottom: kidney ureter bladder sphincter urethra |
|
|
|
functions: ureter bladder sphincter urethra |
ureter- carries the urine from the kidney to the bladder bladder- stores urine prior to elimination sphincter- a muscle that allows the conscious control of urine elimination urethra- carries the urine outside for elimination |
|
|
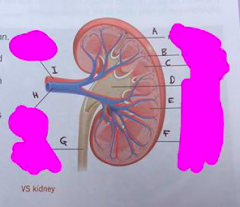
Label the structure of the kidney:
|
A- Nephron B- cortex C- medulla D- pelvis E- apex of pyramid F- fibrous renal capsule G- ureter H- renal vein I- renal arery |
|
|
|
function of: -renal artery -renal vein |
renal artery- carries blood from the heart to the kidney (contains toxins) renal vein- carries blood towards the heart from the kidney (toxin free) |
|
|
|
What is the cortex? |
area of the kidney which contains nephrons, which are the functional units of the kidney and has a dense capillary network |
|
|
|
Function of the pelvis |
acts as a funnel for urine, following into the ureter |
|
|
|
Function of medulla |
contains the loop of Henle, involved in osmoregulation |
|
|
|
purpose of the fibrous renal capsule |
it is fat and fibrous connective tissue which protects the kidney from mechanical damage |
|
|
|
What are the two main functions of the kidney? |
excretion removal of metabolic waste made by the body osmoregulation |
|
|
|
what is meant my osmoregulation |
the control of the water potential of the body's fluids by the regulation of the water content of the body |
|
|
|
true or false Amino acids can be stored |
False amino acids cannot be stored |
|
|
|
what happens to surplus amino acids |
amino acids that are not used for protein synthesis are deaminated in the liver |
|
|
|
Describe deamination |
1) proteins are hydrolysed into its constituent amino acids 2) the NH2 group from the amino acids are removed 3) the amine group: enters respiration as pyruvate or an intermediate in the krebs cycle OR it is excreted as urea, it is transported in the blood to the kidneys to be removed |
|
|
|
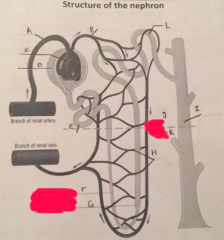
A- afferent arteriole B- efferent arteriole C- glomerulus D- bowmans capsule E- proximal convoluted tubule F- descending limb G- ascending limd H- vasa recta I- collecting duct J- cortex K- medulla L- distal convoluted tubule |
|
|
|
state the three functions of the nephron |
-ultrafiltration -selective reabsorption -osmoregulation |
|
|
|
Definition: ultrafiltration |
It is filtration under pressure that separates small soluble molecules from the blood plasma |
|
|
|
A- squamous epithelial cells B- glomerular capillary C- cuboidal epithelial cells lining the proximal convoluted tubule D- E- podocyte cells F- bowmans space/ bowmans capsule filtrate G- afferent arteriole H- efferent arteriole |
|
|
|
What stays in the blood? What is seperated from the blood and passed into the Bowmans capsule filtrate/ Bowmans space |
Stays in the blood: RBC, WBC, plasma proteins, platelets Passes into the bowmans capsule filtrate: glucose, amino acids, water, urea, salts |
|
|
|
Why is there a high hydrostatic pressure in the glomerulus |
- The afferent arteriole has a wider diameter lumen than the efferent arteriole - the hearts contraction increases the pressure of the arterial blood |
|
|
|
How is the blood in the glomerular capillary separated from the bowman's capsule filtrate/ bowman's space |
It is seperated by three layers. -the wall of the glomerular capillary is a single layer of epithelial cells with pores called fenestrae - the basement membrane is an extra-cellular of proteins. It acts as a molecular sieve. - podocyte cells |
|
|
|
what are podocyte cells ? where are they found ? |
podocyte cells are the squamous epithelial cells that constitute the bowmans capsule wall. |
|
|
|
what are pedicels and filtration slits? |
pedicels are the feet of the podocyte cells filtration slits- gaps in between the pedicels |
|
|
|
Explain ultrafiltration/ how small molecules are seperated from the blood |
1) There is a high hydrostatic pressure in the glomerulus due to the afferent arteriole having a wider lumen diameter than the efferent arteriole. 2) this high hydrostatic pressure forces solutes and water out of the blood in the glomerular capillary, through the pores in between the epithelial cells of the capillary walls (fenestrae) and then through the pores in the basement membrane 3) the basement membrane acts as a molecular sieve. Allowing small molecules (glucose and amino acids) to pass through but preventing large cells from passing through (white blood cells, plasma proteins) 4) the pedicels of the podocytes wrap around the capillaries, pulling them closer to the basement membrane. the filtrate is then filtered through the filtration slits. this forms glomerular filtrate |
|
|
|
Define selective reabsorption Where does selective reabsorption occur? |
selective reabsorption: the uptake of specific molecules and ions from the glomerular filtrate in the nephron back into the bloodstream proximal convoluted tubule |
|
|
|
what are the specific molecules/ ions that are reabsorbed? Why? |
Glucose, amino acids, sodium ions, chloride ions they are reabsorbed because they are useful for the body |
|
|
|
How is glucose and amino acids reabsorbed? Give the amount |
All of the glucose and the amino acids are reabsorbed.
by co transport with a sodium ion. 1 glucose molecule and 2 sodium ions bind to a carrier protein on the cuboidal epithelial cell membrane. they are carried into the cell by facilitated diffusion and they are released from the carrier protein. They diffuse through the cell cytoplasm separately. Sodium diffuses into the capillary down its concentration gradient. This provides energy for the secondary active transport of glucose into the blood, against the concentration gradient. |
|
|
|
how are mineral ions reabsorbed? how much? |
70% of salts are reabsorbed into the blood.
This is by active transport against the concentration gradient using a carrier protein and ATP provided by the cell |
|
|
|
How much water is reabsorbed? How is it reabsorbed ? |
90% of the water from the glomerular filtrate is reabsorbed. by osmosis down a water potential gradient because the reabsorbed ions lowers the water potential of the blood |
|
|
|
What is the un-useful product that is sometimes reabsorbed, why? How much of it is reabsorbed |
urea and small proteins is reabsorbed by diffusion. This is because the water diffuses out of the filtrate by osmosis. There is a high concentration of urea and small proteins in the proximal convoluted tubule. they diffuse into the blood plasma down a concentration gradient |
|
|
|
At the base of the proximal convoluted tubule, describe the solution in that area |
It is isotonic. The filtrate is isotonic with the blood plasma |
|
|
|
How is the PCT's structure adapted for selective reabsorption |
-large surface area (due to the length and high numbers per kidney) -cuboidal cells with microvilli provide large surface area and basal channels - numerous mitochondria provide ATP for active transport - tight junctions preventing the leakage of reabsorbed materials back into the filtrate. |
|
|
|
define osmosis |
osmosis- the diffusion of water from an area of high water potential to an area of low water potential across a partially permeable membrane. |
|
|
|
Why are is the proximal convoluted tubule and the loop of henle stereotyped together? |
They always act in the same way, they absorb the same volume |
|
|
|
How does the distal convoluted tubule and the collecting duct differ from the PCT& the LOH |
They absorb different volumes of water depending on the needs of the body |
|
|
|
How is water reabsorbed? what does this do to the urine? |
salt is highly concentrated in the tissue fluid of the medulla. This causes water to diffuse out of the DCT+ CD by osmosis down a water potential gradient. This water is reabsorbed into the blood via the vasa recta. This makes the urine more concentrated.
|
|
|
|
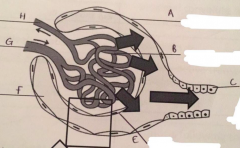
Describe the permeability of the defending limb and the ascending limb |
descending limb: permeable to water ascending limb: impermeable to water. Permeable to salts. |
|
|
|
Explain how water is reabsorbed (start from what happens at the ascending limb, what happens to the descending limb. What is the name of this mechanism? |
the walls of the ascending limb are impermeable to water. na+ and cl- are actively transported out of the filtrate into the tissue fluid of the medulla lowering the water potential and creating a hypertonic environment. This means water diffuses out from the descending limb by osmosis. Water is carried away by the vasa recta. THIS IS BECAUSE THE WALLS OF THE DESCENDING LIMB IS PERMEABLE TO WATER. At the same time, some sodium and chloride ions from the ascending limb diffuse into the descending limb. As the filtrate flows down the descending limb, it PROGRESSIVELY contains less water molecules and more ions. At the bottom of the hairpin, the filtrate is the most concentrated and there is a low water potential.
As the filtrate passes up the ascending limb it PROGRESSIVELY contains less ions as they are actively transported into the tissue fluid. So water potential increases. This is called the counter current multiplier
|
|
|
|
what is the advantage of having two limbs of the loop running side by side? |
the advantage of having two limbs of the loop running side by side, with the filtrate going up one and down the other, is that it enables maximum concentration of solutes to be built at the apex of the loop |
|
|
|
why is the mechanism called the 'counter current multiplier'? |
counter current: the flow of the filtrate in the limbs of the loop flow in opposite directions multiplied: the concentration of solutes at the apex of the loop is increased |
|
|
|
What happens in the collecting duct? |
Water leaves the collecting duct by osmosis down a concentration gradient. This is because the CD runs the filtrate back into the medulla which has a low water potential. |
|
|
|
What affects the permeability of the collecting duct? |
the hormone ANTI-diuretic-hormone |
|
|
|
definition: antidiuretic hormone |
It is the hormone produced in the hypothalamus and secreted by the posterior pituitary gland. It increases the permeability of the cells of the distal convoluted tubule and the collecting duct to water, increasing water reabsorption. |
|
|
|
what is osmoregulation |
it is the control of the water content and solute composition of body fluids. It is the homeostatic balance between water gain and water loss. |
|
|
|
how do humans gain water |
-drinking -food -metabolic water (water produced from the boys reactions) -respiration |
|
|
|
Describe the role of ADH in negative feedback of osmoregulation |
omsoreceptors in the hypothalamus (the receptor and the control centre) detect changes in the water potential of the blood.
The cells of the posterior pituitary gland (the coordinator) secrete more or less ADH depending on the bloods water potential. The cells of the distal convoluted tubules and the collecting duct (effectors) become more or less permeable to water |
|
|
|
describe the effect of: more ADH secreted less ADH secreted |
more ADH: more permeable less ADH: less permeable |
|
|
|
Describe the osmoregulation of a hydrated person |
hydrated person: -increase in water potential -increase is detected by the osmoreceptors in the hypothalamus (acts as the receptor and control centre) -sends an instruction to the posterior pituitary gland (coordinator) to release LESS ADH - the effector, the cells of the DCT+CD are less permeable to water -less water is reabsorbed into the blood -urine is diluted, volume is high -decrease in the water potential in the blood |
|
|
|
what are aquaporins what is cytosol |
they are intrinsic proteins with a pore which allows water molecules to pass through cytosol- the aqueous part of the cytoplasm |
|
|
|
How does ADH enable more concentrated urine to be formed? |
1) ADH causes the aquaporins to become incorporated in the plasma membranes from within the cytosol 2) water is reabsorbed, by osmosis (down a concentration gradient) , from the filtrate into the surrounding hypertonic tissue fluid around the DCT and CD. 3) the concentration of the urine at the bottom of the collecting duct has a similar concentration of the tissue fluid near the apex of the loop. |
|
|
|
6 reasons as to why kidneys may fail
|
-diabetes- high glucose concentration in the plasma results in the glomeruli losing protein into the filtrate where some proteins link together. -raised blood pressure- damages the structure of the epithelial cells and basement membrane of the glomerulus, preventing ultrafiltration -autoimmune disease- the body makes antibodies against its own tissues -genetic conditions -crushing injuries- road accidents |
|
|
|
starts the ways in which kidney failure can be treated |
-dialysis -transplant -reduce the intake of protein -take medication to control blood potassium and calcium levels -take drugs to reduce high blood pressure |
|
|
|
How does reducing your intake of protein help treat kidney failure |
Surplus amino acids (monomers of protein) can't be stored. They are taken to the liver for deamination to make urea. Reducing protein intake reduces the amount of urea in the body |
|
|
|
Explain how taking drugs to reduce blood pressure can help treat kidney failure |
calcium channel blockers dilate blood vessels and reduce blood pressure. Beta blockers reduce the effect of adrenalin and reduces the heart rate |
|
|
|
How is high concentrations of potassium in the blood treated |
treated using a combination of glucose and insulin. if untreated it leads to heart arrhythmias
|
|
|
|
how is high concentrations of calcium in the blood treated |
high conc. of calcium is correlated to a high risk of heart disease and kidney stones. it is treated with biphosphates which reduce the activity of osteoclasts which are cells that break down the bone so less calcium circulates in the blood. |
|
|
|
explain how dialysis works how are glucose levels kept constant |
the blood and dialysis fluid is separated by a partially permeable membrane. The dialysis fluid has the same water potential as the blood but with a low concentration of ions and urea. The ions and urea and water in the blood diffuse out of the blood through the partially permeable membrane and into the dialysis fluid down a concentration gradient. the concentration o glucose in the blood and the the blood are the same, so non diffuses out |
|
|
|
What is haemodialysis? |
a tube connects a persons artery to the dialysis machine. Inside the machine, the blood is pumped through thousands of fibres made of selectively permeable dialysis membrane. The dialysis solution is on the other side of the dialysing membrane. the blood and the dialysis fluid run through the machine in opposite directions. Enhancing diffusion to of the blood but a counter-current mechanism. The fresh blood is returned to a vein. |
|
|
|
why is anticoagulant added to the blood before the dialysis machine? |
to thin the blood and prevent clotting |
|
|
|
why is no anticoagulant added towards the end of the procedure |
to allow blood to clot normally when it enters the body. |
|
|
|
state the advantages of the counter current mechanism advantageous |
maintains a diffusion gradient and doesn't reach equilibrium |
|

