![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
56 Cards in this Set
- Front
- Back

What is seen here?
|

Petechiae
|
|

What is seen here?
|

Purpura
|
|
|
Thrombocytopenia is...
Thrombocytosis is... |
...too few platelets.
...too many platelets. |
|
|
What is the first thing to rule out when you see a low platelet count? How do we do this?
|
pseudothrombocytopenia, AKA “platelet clumping”
... makes the count artifactually low. make a peripheral blood smear. |
|
|
When do we see the first symptoms of low platelet count? When to we need to treat? When do we need to transfuse?
|
<50,000
20k to 10k... maybe not transfuse tho'. sub 10k, transfuse now. |
|
|
Three broad categories of causes of thrombocytopenia?
**THIS IS EXTREMELY IMPORTANT TO KNOW** |
Underproduction
Peripheral Destruction Splenic sequestration |
|
|
What are some causes of platelet underproduction?
|
Marrow failure: myelodysplasia, aplastic anemia, vitamin deficiencies
Marrow infiltration: tumor, granulomatous diseases, fibrosis, leukemias, lymphomas Marrow toxins: drugs, radiation, infections |
|
|
Two types of peripheral destruction of platelets (and examples of 'em)?
|
Non-immune - DIC, TTP
Immune mechanism - provoked by drugs, associated w/ HIV, can be associated with other autoimmune disease, can be ideopathic. |
|
|
What is DIC? What is another word for it?
|
A process, characterized by abnormal activation of coagulation, generation of thrombin, consumption of clotting factors, destruction of platelets, and activation of fibrinolysis.
Consumptive coagulopathy |
|
|
How can we treat DIC? What can cause it?
What supportive measures can we take? |
TREAT THE UNDERLYING CAUSE
Can be associated with gram negative sepsis, severe burns, obstetrical disasters, certain leukemias or tumors, shock, insect or snake venoms platelet transfusion, clotting factors (FFP), fibrinogen (cryoprecipitate) |
|
|
How do we diagnose DIC?
|
Elevated PT - due to consumption of Factor VII, which has the shortest half-life (4 hrs) of all clotting factors.
When advanced, the PTT can be prolonged as well, as the other clotting factor levels fall. Low platelets Low/falling fibrinogen Elevated fibrin degradation products (FDPs/FSPs) or D-Dimers Can see a few schistocytes on the peripheral smear in most cases. |
|
|
What clotting factor has the shortest half0life of all clotting factors?
|
factor VII.
|
|
|
What is TTP?
|
A process, characterized by abnormal activation of platelets and endothelial cells, with VWF and fibrin deposition in the microvasculature, and peripheral destruction of platelets and red cells
|
|
|
What is "the pentad" of Dx features for TTP?
Which 2 MUST be present for Dx? |
Microangiopathic Hemolytic Anemia (MAHA)
Elevated LDH, elevated bilirubin Schistocytes on the peripheral smear MUST BE PRESENT Low platelets - MUST BE PRESENT Fever Neurologic Manifestations - headache, sleepiness, confusion, stupor, stroke, coma, seizures Renal Manifestations hematuria, proteinuria, ^ BUN/Creatinine Schistocytes (MAHA), Low platelets |
|
What is seen here? What disease likely underlies this smear?
|
Low platelets, schistocytes.
TTP |
|
|
What disease requires a hematologist to diag. and treat? What happens if it's not Dx-ed?
|
TTP. Death (possible, I guess)
|
|
|
Differentiate bt DIC and TTP?
|
DIC - actv liquid coag, and the platelets are being consumed.
TTP - process begins with the platets. |
|
|
What is the etiology of TTP? What is the name of the involved protease?
|
normally vWF is secreted from the endothelial cells, and a protease cuts it down to normal size. W/o this snipping, it's WAY TOO LONG. Platelets get stuck on this ultra-long multimer, and get stuck in the vasculatrue.
TTP people have an antibody directed against the protease. ADAMTS-13 |
|
|
Is TTP an autoimmune disorder?
|
Yes. It's just that the antibodies aren't against the platelets.
|
|
|
How do we differentiate b/t DIC and TTP clinically if both can show schistocytes?
|
DIC will have eleveated PT and low fibrogenogen.
|
|
|
What drug can induce TTP? Which two drugs can induce something like TTP but don't involve ADAMTS-13
|
quinine
cyclosporine, tacrolimus - drugs that block T-cell function used in organ transplant... can incite antibodies to other things, not ADAMTS-13 |
|
|
Increased incidence of TTP with...
|
pregnancy or HIV
|
|
|
What is the treatment for TTP?
What kind of transfusions should be avoided? Why? What if their platelet count is sub-10k? What about in the middle of a head bleed? Are glucocorticoids and anti-platelet agents any help in TTP Tx? |
PLEX - Exchange plasma transfusions.
Remove all inciting agents Platelet transfusions, they fuel the fire. Still don't do it. Do it, but damn. uncertain benefit, but are used sometimes. |
|
|
What precipitates HUS? What is it produced by? What does it do?
|
Shiga toxin, produced by E.coli 0157:H7.
It b/endothelial cells in the kidney --> cell death. |
|
|
Which drugs can lead to drug-induced immune-mediated thrombocytopenia?
|
Beta-lactam antibiotics
Trimethoprim-sulfamethoxazole and other sulfa drugs Quinine/quinidine Heparin Abciximab (ReoPro®) |
|
|
How can drugs lead to immune-mediated thrombocytopenia? (3)
|
1) directly stimulating anti-platelet antibody production
2) a hapten mechanism 3) “innocent bystander” phenomenon. |
|
|
Do platelet counts have to be abnormal in Heparin-induced Thrombocytopenia? What does have to happen?
|
No. It just has to fall.
|
|
|
If a patient on heparin has their platelets fall a bit, what do we do?
|
STOP THE HEPARIN
|
|
|
What can Heparin-Induced Thrombocytopenia (HIT) cause (paradoxically)?
why can this be super bad? |
Thrombosis.
the initially feeling is to just increase the heparin. bad shit. |
|
|
What is ITP?
How do we make the Dx (methodologically speaking)? |
Immune/Idiopathic Thrombocytopenic Purpura
By exclusion. There is NO Dx test, unlike AIHA. |
|
|
What will be present in the marrow in ITP
|
megakaryocytes.
|
|
|
What is ITP usually provoked by in children? Tx?
When do we Tx adults? How do we Tx them acutely? |
viral illness. Nothing usually required.
In adults, specific therapy required if platelet count is <30-50 or if patient is bleeding. Initial: corticosteroids. If platelet count is <10k or patient is bleeding, use IVIg. If patient is Rh +, can use Anti-D (WinRho) in place of IVIg. |
|
|
Will most patients with ITP relapse after steroids/acute treatment? What is the 2nd line treatment?
Will this help all patients? |
Yes (2/3) Splenectomy.
No. 1/3 will relapse, and require more intense immunosuppression. |
|
|
Before taking out a spleen, if you have time, what should you do?
|
immunize against encapsulated organisms.
|
|
|
Is HUS seen more often in kids or adults? Where does it have a better prognosis?
|
kids. kids.
|
|
|
How does Anti-D (WinRho) work?
|
Rhogams induces hemolytic anemia by using the RBCs as a decoy, binds them and targets them for destruction. This gives the platelets time to get back up their #.
|
|
|
Normally, __ of total platelet mass resides in spleen.
Splenic enlargement, from any cause, can lead to _________ from peripheral circulation into splenic pool. |
1/3
displacement of placements |
|
|
Can we induce sequestered platelets in the spleen to come out? Given this, should the spleen be seen as a resevoir of platelets?
|
No.
No. |
|
|
Biggest cause of Splenomegaly in US? Other important ones?
|
Portal hypertension from cirrhosis
Some malignancies Chronic Hemolytic diseases |
|
|
Do we transfuse platelets to people w/ ITP if they're not bleeding? why?
|
no. cause they'll destroy 'em.
|
|
|
In splenic sequestration, should we transfuse platelets?
|
not really, because they'll home to the spleen too.
|
|
|
How do we Dx Qualitative disorders of platelets? What do we do here at UNC?
Will PT/PTT/TCT be changed? |
Bleeding time
Platelet Function screen - gives an in-vitro bleeding time. No, should be normal. |
|
|
What is Glanzmann's thrombaesthenia?
|
Congenital Qualitative Platelet disorder
defect in IIb/IIIa on platelet surface |
|
|
Bernard-Soulier disease?
|
Congenital Qualitative Platelet disorder
defect in Ib/IX on platelet surface |
|
|
What are 3 acquired qualitative platelet disorder?
|
uremia
ASA/NSAIDS Myeloproliferative diseases |
|
|
Asprin inhibits...
|
...COX-1
|
|
|
Does ASA reduce recurrent arterial event risk? Primary?
|
Yes. Yes.
|
|
|
What is Clopidogrel (Plavix)? When are they used?
|
Inhibit platelet function by blocking ADP action. ADP is a platelet agonist.
Used in cases where ASA has failed. |
|
|
What do GP IIb/IIIa inhibitors do?
|
act to block fibrogen receptor on platelets (IIb/IIIa), thus INHIBIT PLATELET AGGREGATION
|
|
|
Essential Thrombocythemia, Polycythemia Vera, CML, and myelofibrosis all are what type of disease?
Are these platelets hyper- or hypo- functional? Do these diseases lead to clotting or bleeding? |
Primary Thrombocytosis.
BOTH. Can lead to either or BOTH at the same time. |
|
|
Which type of thrombocytosis usually does not lead to thrombosis?
What are some causes of this type of thrombocytosis? |
Secondary (reactive) thrombocytosis.
inflammation, infection, bleeding, iron def. |
|
|
What is another word for myeloproliferative syndromes? examples?
|
primary throbocytosis syndromes
Essential Thrombocythemia, polycythemia vera, CML, myelofibrosis |
|
|
Platelets are made in the bone marrow from progenitor cells called...
Normal life span of a platelet? Normal Platelet count? |
...megakaryocytes.
10 days. 150-450,000/mL |
|
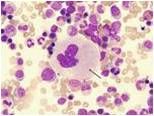
What is the cell in the middle? what is it the progenitor of?
|
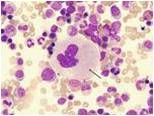
Megakaryocyte
Platelet. |
|
|
Describe the 3 ways that platelets form plugs.
|
Adhesion - Platelets stick to injured vessel wall.
Aggregation - Platelets stick to each other via fibrinogen bridges. Secretion - Platelets release granular contents and potentiate clotting |
|
|
what does vWF do?
|
It b/ to platelets and helps them adhere by also b/ collagen exposed during injury
carrier for VIII |

