![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
226 Cards in this Set
- Front
- Back
|
List three characteristics that will help you distinguish cardiac muscle from skeletal muscle:
|
Cardiac Muscle: Skeletal M.:
-1-2 Nuclei -multi-nucl. -Centrally Placed -Periphery -Intercalated Discs-None -Purkinje Fibers -None |
|
|
Which leukocyte can enter tissues and then go back into the circulatory system?
|
Lymphocyte
|
|
|
Which lymphatic organs undergo age related involution?
|
-Thymus
-Cloacal Bursa |
|
|
Where do you expect to see B lymphocytes and where do you expect to find T lymphocytes in a
normal lymph node? |
-B lymphocytes lymph nodules
-T lymphocytes diffuse lymphatic tissue of the paracortical zone and/or deep cortex |
|
|
Where do you expect to see B lymphocytes and where do you expect to find T lymphocytes in a
normal spleen? |
-B lymphocytes are found in splenic nodules ( lymph nodules)
-T lymphocytes are found in PALS (periarterial lymphoid sheaths) |
|
|
What types of glands are found in the anal sac of CATS?
|
-Apocrine sweat glands
-Sebaceous glands |
|
|
Which of our domestic animal species possess circumanal glands?
|
Dogs
|
|
|
Layers of Epidermis:
-Which layer contacts the basement membrane? |
Stratum Basale
|
|
|
Layers of Epidermis:
-Which layer has cells that have lost their nuclei? |
Stratum corneum
|
|
|
Layers of Epidermis:
-Which layer is only seen in areas of wear & tear? |
Stratum lucidum
|
|
|
Layers of Epidermis:
-In which layer do you usually find Langerhans cells? |
Stratum spinosum
|
|
|
Layers of Epidermis:
-In which layer or layers do you find melanocytes? |
-Stratum basale
-Stratum spinosum |
|
|
Growth of Equine Hoof:
-Layers of Hoof Wall (3): |
-Stratum externum
-Stratum medium -Stratum internum |
|
|
Growth of Equine Hoof:
-Layers of Hoof Wall: -Direction of Growth: -Stratum externum: -Stratum medium: -Stratum internum: |
Growth of Equine Hoof:
-Layers of Hoof Wall: -Direction of Growth: -From proximal to distal: -From proximal to distal: -From inside to outside: |
|
|
The stratum basale and stratum spinosum (stratum germinativum) found on the surface of the
perioplic dermis (corium) gives rise to which specific layer of the cornified epidermal hoof wall? |
Stratum externum
|
|
|
What is the major histological difference that is seen when comparing equine hooves to cloven
hooves (non-equine hoof)? |
Non-Equine hoof has NO secondary laminae
|
|
|
Which laminae of the equine hoof/foot are considered to be “insensitive”?
|
Epidermal laminae
|
|
|
What is the function of the crista ampullaris of the ear?
|
Sense angular or rotational movement
|
|
|
Which specific cranial nerve is associated with the ear (both balance and hearing)?
|
CN 8
|
|
|
List the four types of support cells of the CNS:
|
-Astrocytes
-Oligodendrocytes -Microglia -Ependymal cells |
|
|
Of the support cells of the CNS, which one produces myelin?
|
Oligodendrocyte
|
|
|
List the three layers that comprise the mucous membrane of the typical tubular organs of
digestive system: |
-Epithelium
-Lamina propria -Muscularis mucosae |
|
|
In which of the three tunics (layers) AND which specific part of that tunic of the eye do you find the tapetum lucidum?
|
Uvea (vascular layer) specifically the choroid
|
|
|
List the different types or classifications of lingual papillae (5):
|
-Filiform
-Foliate -Vallate (circumvalate) -Fungiform -Conical |
|
|
Which types of lingual papillae have taste buds associated with them (3)?
|
-Foliate
-Vallate (circumvalate) -Fungiform |
|
|
List two species for which the tunica muscularis of the esophagus is entirely skeletal muscle:
|
-Ruminants
-Dog |
|
|
Which salivary gland is typically regarded as being composed entirely of serous ascini?
|
Parotid salivary gland
|
|
|
What specific duct drains the individual secretory units in salivary glands?
|
Intercalated ducts
|
|
|
You examine a cat and you find a lesion on palatine surface of a premolar. Describe what is meant by the palatine surface:
|
The palatine surface is the inside surface of a tooth in the upper arcade of teeth. This is the surface closest to the hard/soft palate.
|
|
|
What cells make the dentin of teeth?
|
Odontoblasts
|
|
|
What type of connective tissue is found in the umbilical cord?
|
Mucous CT
|
|
|
questions concerning cilia and microvilli:
A) Compare cilia and microvilli based on the cytoskeletal elements that they contain. B) What structure or cytoplasmic component anchors or provides attachement for each: C) TRUE or FALSE: Both cilia and microvilli are covered by plasma membrane. |
-Cilia contain microtubules
-Microvilli cont. microfilaments -Cilia – basal bodies -Microvillia ‐ terminal web -TRUE |
|
|
What specific cell type produces platelets and where is this cell found in the adult mammal.
|
Megakaryocyte – found in bone marrow
|
|
|
With respect to the equine hoof:
A) Which specific laminae contain the living epidermal stratum germinativum (stratum basale + stratum spinosum)? B) Which specific region of dermis (corium) supports the stratum germinativum (stratum basale + stratum spinosum) that produces the stratum medium? |
A)Secondary (2º) epidermal laminae
B)Coronary dermis (corium) |
|
|
What specific tissue makes up the periodontal ligament (membrane) that holds the tooth in the
alveolar bone? |
CCT
|
|
|
The three non‐glandular compartments of the ruminants stomach look similar. How do you tell them
apart, histologically? |
-Rumen – has papillae that do not have any muscularis mucosa
-Reticulum – has papillae and reticular crests – there is muscularis mucosa only in the tips (ends of the reticular crests. -Omasum – has laminae and muscularis mucosa is found throughout the length of the lamina. |
|
|
What component of the blood-brain barrier is the most important in creating an effective barrier in the mature animal?
|
Endothelial cells of the blood capillaries that are joined by tight junctions
|
|
|
List the components that make up each of the three parts of the ear:
|
-external ear : pinna and external auditory canal (meatus)
-middle ear : three ear bones (ossicles).], tympanic cavity (auditory tube) -inner ear : vestibule, semicircular canals and the cochlea |
|
|
What is koilin and where do you find it?
|
Koilin is a non cellular membrane or secreted material that lines the luminal surface of the bird
ventriculus (gizzard) |
|
|
Which type of glands of the monogastric stomach (or the abomasums) appear serous ?
|
cardiac glands
|
|
|
What do the chief cells of the proper gastric glands secrete?
|
Pepsinogen
|
|
|
List the four(4) modifications that are seen in the small intestine to increase surface area ?
|
-length of small intestine
-plicae circulares -villi -microvilli (brush border) |
|
|
HYPSODONT TEETH
SPECIES VARIATION: – Carnivores: – Pigs: – Ruminants: – Horses: |
– Carnivores: no hypsodont
teeth – Pigs:only canines hypsodont – Ruminants: cheek teeth are hypsodont – Horses: all teeth hypsodont, but canines cease growth |
|
|
BRACHYDONT
-3 Components: |
-Dental Pulp (Pulp Cavity)
-Odontoblasts -Dentin |
|
|
BRACHYDONT
-DENTAL PULP: -Widest In? -Tissues? |
– widest in young animals
– Central area; CCT; ? mucous CT – Contains nerves & blood vessels |
|
|
BRACHYDONT
-ODONTOBLASTS: -Location: -Function: |
– Cells at periphery of dental pulp
– Produce dentin • predentin = unmineralized • predentin - closest to odontoblasts |
|
|
AMELOBLASTS:
-Function? -Orientation? -Destroyed when? |
-Produce enamel before teeth erupt
-Apical surface faces developing tooth -Destroyed with tooth eruption |
|
|
ENAMEL:
-Covers? -Description: |
-Covers crown only
-Hardest substance in body ~97% inorganic (calcium salts) |
|
|
CEMENTUM:
-Covers? -Produced by? -Description? |
– Covers root (i.e. stops at
gum line) – Produced by cementocytes housed in lacunae – Cellular & acellular areas |
|
|
PERIODONTAL MEMBRANE:
-Tissue? -Function? |
– Dense CCT
– Holds tooth root in alveolar bone (“socket”) |
|
|
ALVEOLAR BONE:
-Type? -Function? |
– Compact & cancellous
bone that forms the socket |
|
|
SALIVARY GLANDS
General features (4): |
• Compound tubuloalveolar or tubuloacinar glands
• Lobulated w/ CCT btw lobules • Types of secretory acini within lobules - varies with different glands&with species • Prominent duct system |
|
|
SALIVARY GLANDS
• Types of secretory acini within lobules (3): |
Varies with different glands and with species:
• Serous • Mucous • Mixed |
|
|
SALIVARY GLANDS
• Prominent duct system (4): |
(small to large)
– Intercalated ducts – Striated ducts – Interlobular ducts – Principal (main) ducts |
|
|
SALIVARY GLANDS
• Intercalated Ducts -Size? -Drain? -Tissue? -Classification? |
– Smallest ducts within lobules
– Drain individual secretory units – Simple cuboidal -- may only see nuclei (“purple beaded bracelet”) • Striated Ducts |
|
|
SALIVARY GLANDS
• Striated Ducts: -Size: -Drain: -Tissue: -Classification: |
– Most prominent ducts within
lobules – Drain several secretory units – Simple cuboidal to columnar – Striations at basal aspect (= infoldings of plasmalemma) |
|
|
SALIVARY GLANDS
•Interlobular Ducts -Location: -Tissue: |
–Between lobules
within CCT –Columnar (simple or stratified) or stratified cuboidal |
|
|
SALIVAR GLANDS
-General Types (2): |
• Parotid Salivary Gland
• Mixed Salivary Gland |
|
|
• PAROTID SALIVARY GLAND
-Only what kind of cells? -Frequently confused with? |
– Only serous acini
– Frequently confused with pancreas |
|
|
•MIXED SALIVARY GLAND
-Types (2): -Cells present? -Description? |
– Mandibular & Sublingual salivary glands
– Both serous and mucous cells present – Part of sublingual polystomatic portion) empties directly into oral cavity so has decreased intralobular duct system |
|
|
SALIVARY GLANDS
-Functions (4): -Prevalent Cells? -Function? |
• Moistens oral mucosa & food
• Some CHO digestion (salivary amylase) • Saliva contains antibodies (IgA) => protection from pathogens – Plasma cells prevalent • Secrete IgA |
|
|
OROPHARYNX
• Location: -Contains: |
– Transitional area between oral cavity & digestive tract
– Contains the tonsils: • Palantine (2) lateral wall • Pharyngeal (1) posterior wall |
|
|
ESOPHAGUS
-Microscopic Layers (7): |
• Mucous Membrane (Mucosa)
– Epithelium = NKSS – Lamina propria – Muscularis mucosae • Submucosa • Tunica Muscularis • Adventitia/Serosa |
|
|
ESOPHAGUS
• Mucous Membrane (Mucosa) – Epithelium = ? – Lamina propria - typically? – Muscularis mucosae = ? |
– Non-keratinized stratified
squamous – Typically aglandular in mammals – Variably developed in mammals |
|
|
ESOPHAGUS
• Submucosa -Tissues: -In Birds: |
– +/- glands ( predominantly mucous)
– +/- lymphoid nodules – Very thin layer in birds |
|
|
ESOPHAGUS
• Tunica Muscularis – Description: • Adventitia/Serosa – Location: |
– Spiraled; 2 layers
– Adventitia = cervical & thoracic – Serosa = abdominal |
|
|
ESOPHAGUS
Species Variations: • Tunica Muscularis – Ruminants & Dogs: – Birds: – Others: • Cranial 1/3 = ? • Middle 1/3 = ? • Caudal 1/3 = ? • Esophageal Glands – Mammals: – Birds: |
• Tunica Muscularis
– Ruminants & Dogs: all skeletal muscle – Birds: all smooth muscle – Others: • Cranial 1/3 = skeletal muscle • Middle 1/3 = skeletal & smooth muscle • Caudal 1/3 = smooth muscle • Esophageal Glands – Mammals: mixed (mainly mucous) glands in submucosa – Birds: mucous glands in lamina propria |
|
|
CROP:
-What Species? -Ventral Diverticulum of? -Function? • Same as esophagus microscopically except (2): |
• Avian feature
• Esophagus • Used for storage – Epithelium usually thicker in the crop – Glands are absent in crop |
|
|
Muscularis Mucosae is thinner in Stomach or Small Intestine?
|
Small Intestine
|
|
|
INTESTINAL ENTEROENDOCRINE CELLS
-Location: -2 Different Morphologies: -Secrete Hormones (2): |
-Deep (Basal) Portion of Intestinal Crypts
-1) Acidophilic granules face the lamina propria 2) cytoplasm is unstained surrounding the nucleus – Secretin => pancreatic duct cells to release bicarbonate => increases the pH of the chyme entering intestines (i.e. makes chyme more alkaline) – Cholecystokinin - CCK (Pancreozymin) => pancreatic acini to secrete digestive enzymes & gallbladder contraction |
|
|
MYENTERIC & SUBMUCOSAL PLEXUS
-Comprised of? -Encapsulated in CCT? -Function? -Regulation? |
♦ Neuron cell bodies & their
processes ♦ Not encapsulated with CCT ♦ Responsible for peristalsis ♦ Mainly autonomous but partially regulated by the autonomic N.S. (sympathetic & parasympathetic) |
|
|
What differentiates Large Intestine from Small Intestine Histologically?
|
NO VILLI in Large Intestine!
|
|
|
ANAL CANAL
-Main Layers (3): |
-Mucosa
-Tunica Muscularis -Adventitia (Typical) |
|
|
ANAL CANAL
-Mucosa: -Layers (2): |
-NKSS epith. becoming keratinized at end
-Lamina propria - blends with submucosa -Muscularis mucosa ABSENT! |
|
|
ANAL CANAL
-Mucosa: -Contents (3): |
-sweat glands
-sebaceous glands -circumanal glands in dogs |
|
|
ANAL CANAL
-Tunica Muscularis: -Types of muscle & what they form (3): |
-Inner circular layer --> forms internal anal sphincter
-Outer longitudinal layer -->forms rectococygeous m. -Skeletal muscle --> external anal sphincter |
|
|
LIVER
-Functions (2): -Secretory Units: -Ducts: |
-Endocrine (Islets of Lang.)&
-Exocrine (majority) -Serous Acini -Intercalated (NO STRIATED DUCTS!!) |
|
|
PANCREAS
-Exocrine Function (2): |
-Production of Bicarbonate
-Digestive Proenzymes / Enzymes |
|
|
PANCREAS
-Exocrine Function: -Production of Bicarbonate: -Process/Effect: |
♦ neutralizes acidic chyme
♦ secreted by centroacinar cells in response to secretin enteroendocrine cells of small intestine ---> secretin ---> goes to pancreas and acts on centroascinar cells to release bicarbonate |
|
|
PANCREAS
-Exocrine Function: -Digestive Proenzymes/ Enzymes: -Process/Effect: |
♦ breakdown proteins/ carbohydrates/lipids
♦ secreted by acinar cells in response to cholecystokinin enteroendocrine cells of small intestine ---> cholecystokinin --->goes to pancreas and acts on acinar cells to release several different enzymes and proenzymes -examples: trypsinogen, chymotrypsinogen, procarboxypeptidases amylase, lipase |
|
|
LIVER
-Stroma -Major Parts (3): |
• Capsule
• Interstitial (interlobular) CT • Reticular fiber network suspends hepatocytes (liver cells) – Not visible |
|
|
LIVER
-Stroma -Capsule: |
– CCT
– Serosa where exposed to abdominal cavity |
|
|
LIVER
-Stroma -Intersitial (Interlobular) CT: |
– Loose CCT
– Highly pronounced in the pig |
|
|
List the three zones of the adrenal cortex and list one hormone that is produced by each zone.
|
-Zona glomerulosa ‐ aldosterone
-Zona fasiculata ‐ cortisol, corticosterone (DHEA) -Zona reticularis ‐ DHEA (cortisol, corticosterone) |
|
|
List the two (2) major hormones (or substances) produced by the adrenal medulla.
|
Epinephrine
Norepinephrine |
|
|
List the two (2) nerve plexuses seen in the tubular portions of the gastrointestinal tract.
|
+Submucosal (Meissner’s) plexus
+Myenteric (Auerbach’s) plexus |
|
|
Which portion of the intestine is NOT covered with a serosa?
|
Terminal rectum
|
|
|
What type of epithelium is present in the anal canal?
|
Stratified squamous epithelium that is nonkeratinized proximally and becomes keratinized distally.
|
|
|
The inner circular layer of the smooth muscle of the anal canal forms what specific muscle associated with the anus?
|
Internal anal sphincter
|
|
|
CONCERNING MUSCLE
A) Which protein is the major component of thick filaments of striated muscle? |
Myosin
|
|
|
CONCERNING MUSCLE
B) Which protein is the major component of thin filaments of striated muscle? |
Actin (F and G)
|
|
|
CONCERNING MUSCLE
C) What are the other proteins that are also found in thin filaments of striated muscle? |
Tropomysoin, Troponin
|
|
|
CONCERNING MUSCLE
D) What is the function of the sarcoplasmic reticulum in muscle? |
(Modified smooth endoplasmic reticulum) is primarily concerned with:
- uptake, storage and release of calcium ions. |
|
|
MAMMALIAN LUNG
-General Functions (4): |
• A. AIR CONDUCTION/GAS EXCHANGE.
• B. WARMS, HUMIDIFIES, FILTERS AIR. • C. BACTERICIDAL SECRETIONS. • D. REGULATES BODY TEMPERATURE. |
|
|
MAMMALIAN LUNG
2 Principle Portions: |
-AIR-CONDUCTING PORTION
-RESPIRATORY PORTION |
|
|
MAMMALIAN LUNG
-AIR-CONDUCTING PORTION: -Parts (7): |
• a. nasal cavity & paranasal sinuses.
• b. nasopharynx. • c. larynx. • d. trachea. • e. principal (extrapulmonary) bronchi. • f. intrapulmonary bronchi. • g. bronchioles (including terminal bronchioles). |
|
|
MAMMALIAN LUNG
-RESPIRATORY PORTION -Location: -Parts (4): |
-Where gas exchange occurs:
In Lungs • a. respiratory bronchioles. • b. alveolar ducts. •c. alveolar sacs. •d. alveoli. |
|
|
NASAL CAVITY&
PARANASAL SINUSES -Regions of Nasal Cavity (3): - |
a. Vestibular region.
b. Respiratory region. c. Olfactory region. *Sec. Of both resp. & olfactory epithelium. |
|
|
NASAL CAVITY Microscopy
-VESTIBULAR REGION: -Layers/Assoc. Structures: -Function: |
-NKSS,
-LP/ submucosa -Short hairs, -Sebaceous/Sweat glds. -Remove large particles ! |
|
|
NASAL CAVITY Microscopy
-RESPIRATORY REGION: -Layers/Assoc. Structures: |
-Most of nasal cavity PSColEpiCil/Gob.
-LP/submucosa -Vascular, glds, lymph tissue. -Underlying tissue cart or Bone |
|
|
NASAL CAVITY Microscopy
-OLFACTORY REGION: -Layers/Assoc. Structures: |
-Post/superior area nasal
cavity: ModPSColEpi -3 Cell Types! -THICK! -NO Goblet cells. -LP/submucosa: -Serous glds -Nerve fibers. -Underlying tissue cart or BONE |
|
|
NASAL CAVITY Microscopy
-OLFACTORY REGION: -3 Cell Types in Epithelium: |
a) Olfactory Cells:
-Mod. Bipolar Neurons; Apex of Cell Mod. w/ Non- Motile Cilia=ODORreception -Axons form OLFACTORY n. b)Sustentacular(support) Cells: -COLUMNAR cells -May contain MELANIN, gives Yellow color to Epith. c) Basal Cells: - SHORT -Prob. Replace Support Cells |
|
|
RESPIRATORY SYSTEM
PARANASAL SINUSES -2 Specific to dog? -Functions? |
-Maxillary & Frontal Sinuses
•AIR-FILLED SPACES W/in CERTAIN BONES OF SKULL THAT: •Communicate Directly or indirectly to nasal cavity •EPITHELIUM VARIABLE: PSEUDOSTRATIFIED COL., SIMPLE CUBOIDAL, QUITE THIN. L.P. FUSES WITH UNDERLYING •PERIOSTEUM. LIGHTENS WT. OF SKULL, WARMS AIR, •PHONATION. |
|
|
RESPIRATORY SYSTEM
• NASOPHARYNX: -Similar to: -Leads into: |
• SIMILAR TO NASAL CAVITIES &
• LEADS INTO LARYNX. • SOME VARIATIONS IN SPECIES, BUT • BASICALLY SIMILAR. |
|
|
RESPIRATORY SYSTEM
-TERMINAL BRONCHIOLES: -Relative Size: -Epithelium: -Lamina Propria: -Gas Exchange: |
• SMALLEST Air-Conducting
Structures • SIMPLE CUBOIDAL Epith. • L.P. DIFFICULT to see & may fuse with • MUSCULARIS MUCOSA. +NO GAS EXCHANGE YET !! |
|
|
RESPIRATORY SYSTEM
RESPIRATORY PORTION: -Significance: -Respiratory Structures (4): |
+Where GAS Exchange Begins!!
a. RESPIRATORY BRONCHIOLES (EXCHANGE BEGINS). b. ALVEOLAR DUCTS. c. ALVEOLAR SACS. d. ALVEOLI. |
|
|
List three reasons why the normal cornea of the eye is transparent.
|
(1) the cornea is avascular
(2) the thin collagen fibers are very regularly arranged in the stroma of the cornea (3) sodium pumps in the epithelium removed sodium and water follows, keeping the stroma of the cornea in a relatively dehydrated state. |
|
|
What is Adnexa?
What are 4 Component structures? |
Accessory Skin Structures
-Hair & Hair follicles -Arrector pili muscle -Sebaceous glands -Sweat glands |
|
|
Where are postcapillary venules located & what is their importance in Lymph nodes?
|
IN DEEP CORTEX, HIGH ENDOTHELIUM,LYMPH’S LEAVE BLD. STREAM TO
RE-ENTER LN’s. |
|
|
List the 4 major types of connective tissue:
|
-COLLAGENOUS CT
-MUCOUS CT -RETICULAR CT -ELASTIC CT |
|
|
TYPE II PNEUMOCYTES
-Also called: -Produce: -Function: -When is it made: |
(Granular Pneumocytes/Septal
Cells). -Produce Surfactant -Lowers surface tension in alveoli preventing collapse of alveoli. Also possible bactericidal effect. -Made last weeks of gestation. Can give glucocorticoids to induce its formation. -Make-up about 3-7% of lining cells. |
|
|
What law does gas exchange follow?
|
Simple Diffusion
|
|
|
DIGESTIVE SYSTEM
LIVER -General Arrangement: |
-Lobules
-Central Vein -Portal Triad |
|
|
DIGESTIVE SYSTEM
LIVER -Central Vein: -Location: |
-Located in the center of each hepatic lobule
-Plates of hepatocytes radiate out toward periphery |
|
|
DIGESTIVE SYSTEM
LIVER -Portal Triad: |
-Located at “corners” of the lobules --- includes:
+branch of hepatic artery = smooth m. in wall +branch of bile duct = simple cuboidal epithelium +branch of portal vein = endothelium & no smooth m. |
|
|
DIGESTIVE SYSTEM
LIVER -Hepatic Subunits (3): |
-Hepatic Lobules
-Portal Lobules -Liver Acini |
|
|
DIGESTIVE SYSTEM
LIVER -Portal Lobule: -Formed by: -Associated with: |
-“triangles” formed by connecting 3 adjacent central veins around a portal triad
-associated with bile flow; exocrine function of Liver |
|
|
DIGESTIVE SYSTEM
LIVER -Hepatic Acinus -Formed By: -Associated with: |
-“diamond” formed with long axis between 2 central veins & short axis between 2 portal triads located between adjacent central veins
-Associated with blood flow/ metabolic function of liver |
|
|
DIGESTIVE SYSTEM
LIVER -Duct System: -Components (3): |
-Bile Canaliculi
-Bile Ductules -Interlobular Bile Ducts |
|
|
DIGESTIVE SYSTEM
LIVER -Duct System: -Bile Canaliculi: -Location: -Components |
-Between adjacent hepatocytes
-Microvilli of hepatocytes extend into canaliculi -Bile canaliculi not seen with H&E staining; microvilli not seen with light microscopy |
|
|
DIGESTIVE SYSTEM
LIVER -Duct System: -Bile Ductules: -Location: |
-Connect canaliculi
to interlobular bile ducts -+/- seen on edge of connective tissue |
|
|
DIGESTIVE SYSTEM
LIVER -Duct System: -Interlobular Bile Ducts: -Location: |
-Within portal triad in
CCT between lobules |
|
|
DIGESTIVE SYSTEM
LIVER -Two Sources of blood come to the liver: |
-Hepatic artery => oxygenated blood from the heart
-Portal vein => blood coming from a first pass through intestines (PRIMARY) +Allows liver to filter/detoxify impurities in blood coming from intestines |
|
|
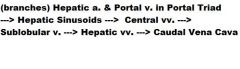
Blood Flow Pattern with Liver:
|
|
|
|
DIGESTIVE SYSTEM
LIVER -Blood Flow -Hepatic Sinuosoids -Function: |
-discontinuous capillaries so blood contacts hepatocytes
|
|
|
DIGESTIVE SYSTEM
LIVER -Blood Flow -Central Veins -[O2] of Hepatocytes: |
hepatocytes CLOSEST to central vein are LOWEST in O2
|
|
|
DIGESTIVE SYSTEM
LIVER -Blood Flow -Sublobular Veins: -Location: |
located within interlobular CCT
|
|
|
DIGESTIVE SYSTEM
LIVER -Blood Flow -Hepatic vv. -Collect From: -Deliver to: |
collect from sublobular veins & deliver to Caudal Vena Cava
|
|
|
DIGESTIVE SYSTEM
LIVER -Bile Acid Synthesis/Secretion -Bile Acid absorbed from: -Synthesis Pathways (2): |
-90% of bile acids - absorbed from intestine & transported to the liver.
1.The classic (neutral) pathway 2. The alternative (acidic) pathway. |
|
|
DIGESTIVE SYSTEM
LIVER -Bile Acid Synthesis -Classic (Neutral) Pathway -Location/Description: -Starting Product: |
-Occurs in the liver, and accounts for approximately 90% of bile acid synthesis.
-Cholesterol |
|
|
DIGESTIVE SYSTEM
LIVER -Cholestasis -Definition: -Induces: |
-Suppression or stoppage of bile flow.
-This bile “sludging” induces hepatocytes & bile duct epithelial cells to increase production of an enzyme, alkaline phosphatase, (ALP) whose levels are measured in the blood |
|
|
DIGESTIVE SYSTEM
LIVER -Cholestasis -Can also be caused by: |
Certain drugs (e.g. glucocortacoids, anticonvulsants ) also can trigger increased production of ALP
|
|
|
DIGESTIVE SYSTEM
LIVER -Functions (5): |
1. Production/secretion of bile
2. Synthesis of substances released into bloodstream 3. Detoxification/Inactivation of drugs and other substances 4. Metabolite Storage 5. Metabolic Functions |
|
|
DIGESTIVE SYSTEM
LIVER -Functions -1. Bile Synth/Secretion is responsible for: |
Responsible for emulsifying fats
|
|
|
DIGESTIVE SYSTEM
LIVER -Functions -2. Synthesis of Substances Released into Bloodstream: -Examples (3): |
+Albumin
+Fibrinogen +Clotting factors |
|
|
DIGESTIVE SYSTEM
LIVER -Functions -4. Metabolite Storage -Examples (3): |
-Lipids (in the form of triglycerides)
-Carbohydrates (in the form of glycogen) -Vitamin A |
|
|
DIGESTIVE SYSTEM
LIVER -Functions -3.Detoxification/Inactivation of drugs and other substances -Enzymes: |
(enzymes located in SER, which is abundant in hepatocytes)
|
|
|
DIGESTIVE SYSTEM
LIVER -Functions -5.Metabolic Functions -Examples (2): |
-Synthesis of glucose (gluconeogenesis)
-Amino acid deamination resulting in production of urea |
|
|
DIGESTIVE SYSTEM
GALLBLADDER -Species Without it: -Bile Storage/Secretion: |
-Horses, Rats, Deer, Pigeons
-They Dont store Bile, it is secreted directly into their Duodenum |
|
|
DIGESTIVE SYSTEM
GALLBLADDER -General Layers (5): |
1.Mucous Membrane
2.Submucosa 3.Tunica Muscularis 4.Perimuscular CT 5.Serosa |
|
|
DIGESTIVE SYSTEM
GALLBLADDER -Mucous Membrane -Components (2): |
++COMPLEX FOLDS
-Simple columnar epithelium with: +microvilli; NO goblet cells -Lamina Propria +/- mucous glands -NO Muscularis Mucosae!! |
|
|
DIGESTIVE SYSTEM
GALLBLADDER -Submucosa -Components: |
Blends with LP b/c NO MUSCULARIS MUCOSAE
|
|
|
DIGESTIVE SYSTEM
GALLBLADDER -Tunica Muscularis -Description: |
Thin; no obvious arrangement of muscle cells into layers
|
|
|
DIGESTIVE SYSTEM
GALLBLADDER -Perimuscular Connective Tissue: -Description: |
CCT layer (relatively thick) outside the tunica muscularis
|
|
|
DIGESTIVE SYSTEM
GALLBLADDER -Serosa: -Description: |
-Typical
-Only on surface AWAY from Liver! |
|
|
DIGESTIVE SYSTEM
GALLBLADDER -Functions (2): |
1.Stores & concentrates bile from liver
2.Gallbladder contracts to release bile |
|
|
DIGESTIVE SYSTEM
GALLBLADDER -Functions -After you eat a fatty meal: |
Enteroendocrine cells of duodenum release cholecystokinin (CCK) ----> gallbladder and gallbladder contracts to release bile
|
|
|
AVIAN RESPIRATORY SYSTEM
-Upper Respiratory Tract Variations (2): |
-Vestibular region of nasal cavity lined by keratinized stratified squamous epithelium
-Cells of stratum spinosum are often arranged like stacks of coins |
|
|
AVIAN RESPIRATORY SYSTEM
LUNGS -What is equivalent to Mammalian Alveoli? |
Air Capillaries
|
|
|
AVIAN RESPIRATORY SYSTEM
-Air Passageways (3): |
1. Primary Bronchi
2. Secondary Bronchi 3. Parabronchi (Tertiary Bronchi) |
|
|
AVIAN RESPIRATORY SYSTEM
-Where does gas exchange occur? |
-Thru Air Capillaries within Parabronchi (Tertiary Bronchi)
|
|
|
AVIAN RESPIRATORY SYSTEM
LUNGS -Primary Bronchi -Portions (2) -Composition (4): |
++Both extrapulmonary & intrapulmonary portions
– Respiratory epithelium – Lamina propria (= CCT support of epithelium) – Muscularis mucosae complete (= layer of smooth muscle deep to lamina propria) – Hyaline cartilage plates |
|
|
AVIAN RESPIRATORY SYSTEM
LUNGS -Primary Bronchi -Portions (2) -Composition (4): |
++Both extrapulmonary & intrapulmonary portions
– Respiratory epithelium – Lamina propria (= CCT support of epithelium) – Muscularis mucosae complete (= layer of smooth muscle deep to lamina propria) – Hyaline cartilage plates |
|
|
AVIAN RESPIRATORY SYSTEM
LUNGS -Secondary Bronchi -Portions: -Composition (3): |
++Only intrapulmonary
– Simple cuboidal (or columnar) epithelium – Lamina propria – Interrupted muscularis mucosae – NO hyaline cartilage -On rare occasion you will see air vesicles w/in walls |
|
|
AVIAN RESPIRATORY SYSTEM
LUNGS -Tertiary or Parabronchi -Composition (3): |
– Simple cuboidal or simple squamous epithelium
– Lamina propria – Muscularis mucosae arranged in bundles ++Lumen diameter varies due to affect of this smooth m. |
|
|
AVIAN RESPIRATORY SYSTEM
LUNGS -Tertiary or Parabronchi: -Structures w/in walls (3): -Where gas exchange occurs: |
1. Air vesicles = first airways off main lumen
2. Air capillaries=Smaller airways off of air vesicles -Where gas exchangeoccurs! -Equivalent to mammalian alveoli -Indistinguishable from blood capillaries -IF not seen extending from air vesicles= 3. Blood capillaries |
|
|
AVIAN RESPIRATORY SYSTEM
LUNGS -Air Sacs: -Location: -Composition: -Extensions: |
Location:
– Cranial&Caudal Composition: – Simple squamous (or simple cuboidal) epithelium – Lamina propria Extensions: – Connect to lungs via bronchi – Extensions within several bones |
|
|
AVIAN RESPIRATORY SYSTEM
-Respiration: -Air Flow Dependant on: |
-2 cycle system in avians
-Air flow depends on movement of the intercostal muscles NOT on a muscular diaphragm |
|
|
AVIAN RESPIRATORY SYSTEM
-Air Flow Mechanics: |
++1st inspiration -- air in through trachea ---> through larger airways in lungs ---> into caudal air sacs
++1st expiration and 2nd inspiration -- air ---> through parabronchi and air capillaries (where gas exchange occurs) and into cranial air sacs ++There is unidirectional flow through the parabronchi!! +2nd expiration -- air from cranial air sacs ---> outside (via trachea) |
|
|
Where do you find Kupffer cells and what is their function?
|
-In the walls of the hepatic sinusoids
-They are phagocytic cells (macrophages) |
|
|
What are the two types of cells that can be found in the parathyroid gland (one cell type may not always be present):
|
-Principal (chief) cells
-Oxyphil cells |
|
|
Which cell type produces parathyroid hormone?
|
Principal (Chief) Cells in the Parathyroid Gland
|
|
|
List the layers that compose the air‐blood barrier found in the lung:
|
+ Alveolar lining cells
(Squamous cells of alveolus) + Basement Membrane of Alveolar cells + Basement Membrane of Capillary Endothelial cells + Capillary Endothelium ++(Note: sometimes the two basement membranes fuse to form one basement membrane) |
|
|
What is the specific respiratory structure in the AVIAN lung that serves the same function as ALVEOLI
in the mammalian lung? |
Air capillary
|
|
|
What is the SMALLEST AIR‐CONDUCTING structure of the mammalian respiratory system?
|
Terminal bronchiole
|
|
|
What type of muscle composes the trachealis muscle AND is the trachealis muscle present in the
avian trachea? |
-The trachealis muscle is smooth muscle
-The trachealis muscle is NOT present in birds |
|
|
DIGESTIVE SYSTEM
-What are taenia coli? |
Accumulations or thickened bands of the outer layer of longitudinal smooth muscle found in regions of the large intestine in some species of domestic animals (horse and swine)
|
|
|
DIGESTIVE SYSTEM
-List the two nerve plexuses seen in the tubular portions of the gastrointestinal tract: |
+Submucosal (Meissner’s) plexus
+Myenteric (Auerbach’s) plexus |
|
|
DIGESTIVE SYSTEM
-Which portion of the intestine is NOT covered with a serosa? |
Terminal rectum
|
|
|
DIGESTIVE SYSTEM
-The outer longitudinal layer of the smooth muscle of the anal canal becomes what specific muscle? |
Rectococcygeus muscle
|
|
|
ENDOCRINE SYSTEM
PITUITARY -Location: -Develops From (2): -Major Subdivisions (2): |
+ Sella turcica
1. Rathke’s Pouch (roof of prim. oral cavity) 2. Infundibulum (floor of early brain; remains attached to the brain). 1. Adenohypophysis (from Rathke’s Pouch). 2. Neurohypophysis (from infundibulum). |
|
|
ENDOCRINE SYSTEM
ADENOHYPOPHYSIS -Pars Distalis -Cell Types (3): -Cells in groups with: |
+Chromophils:
1.Acidophils (35%)-several types. Use special stains. 2.Basophils (15%)-several types; hematoxylin poor staining. Use special stains. 3. Chromophobes (50%)-stain poorly; may be reserve/degenerating cells. +Cells in groups with associated fenestrated capillaries. |
|
|
ENDOCRINE SYSTEM
ADENOHYPOPHYSIS -Pars Intermedia -Location: -Contents (3): |
-Cellular portion next to pars nervosa
-Nonspecific basophils and sometimes vesicles. -Residual cleft (Hypophyseal cleft) of Rathke’s Pouch adjacent to pars distalis |
|
|
ENDOCRINE SYSTEM
ADENOHYPOPHYSIS -Pars Intermedia -Considerable variation btw. species: -Pars Tuberalis -Location: -Cellular arrangement/ secretions: |
+ Encircles infundibular stalk(stem); most vascular portion of pituitary.
+Cells arranged in cords & may secrete gonadotropins (FSH,LH) |
|
|
ENDOCRINE SYSTEM
ADENOHYPOPHYSIS -Pars Distalis -Cell Types -Acidophils -Types (2): -Basophils (3): |
1. Somatotropes
2. Mammotrophs (Lactotropes) + Gonadotrophs -1. FSH -2. LH 3. Thyrotrophs 4. Corticotrophs |
|
|
ENDOCRINE SYSTEM
ADENOHYPOPHYSIS -Pars Distalis -Somatotrope Functions (2): |
1. Produces STH, GH
-Increases size, protein synthesis. 2. Produces growth factors (somatomedins) via liver, kidneys, etc. |
|
|
ENDOCRINE SYSTEM
ADENOHYPOPHYSIS -Pars Distalis -Mammotroph Functions (3): |
1. Produce prolactin (lactogenic hormone, LTH)/ Luteotropin.
-Causes milk secretion after mammary gland development. 2. Maintains CL in some species. 3.Maternal behavior stimulated. |
|
|
ENDOCRINE SYSTEM
ADENOHYPOPHYSIS -Pars Distalis -FSH Functions (2): |
1. Promotes growth, development of ovarian follicles.
2. In males stimulates certain stages of spermatogenesis, via ABP |
|
|
ENDOCRINE SYSTEM
ADENOHYPOPHYSIS -Pars Distalis -LH Functions (3): |
1.Promotes Ovulation/develp. of corpus luteum and
2. Probably Progesterone secretion. 3. In males (ICSH) stimulates secretion of Testosterone (Androgens) from interstitial (Leydig) cells of testes. |
|
|
ENDOCRINE SYSTEM
ADENOHYPOPHYSIS -Pars Distalis -Thyrotroph Function: |
Produce Thyrotropic Hormone (TTH, TSH). Stimulation & maintenance of thyroid gland
|
|
|
ENDOCRINE SYSTEM
ADENOHYPOPHYSIS -Pars Distalis -Corticotroph Function: |
Produce Adrenocorticotropic Hormone (ACTH). Stimulates secretion of adrenal cortex.
|
|
|
ENDOCRINE SYSTEM
ADENOHYPOPHYSIS -Pars Distalis -Regulation of Secretory Activity involves (4): |
1. Hypothalamus
2. PORTAL BLOOD System, the Hypophyseal -Portal System (Hypothalamo- Hypophyseal (H-H) System). 3. Hypothalamic Neurons 4. Releasing factors via H-H Portal circulation to P.D. and (possibly) P.I. of Pituitary Gland. |
|
|
NEGATIVE FEEDBACK MECHANISM:
To activate appropriate Chromophil Cell in P.D. and (possibly) P.I. of Pituitary Gland: 1. Appropriate: 2. Goes to: 3. Results in: |
1. Appropriate Tropic Hormone
secreted. 2. Goes to Target Organs/Cells -which increases T.O. secretion, which, in turn, reduces sensitivity of Hypothalamic Neurons. 3. Results in Less Releasing Factor Hormones |
|
|
ADENOHYPOPHYSIS
P.I and P.T. -Functions: |
-Melanocyte Stimulating Hormone (MSH; intermedin) produced by cells of P.I.
-Exact role in domestic animals not clear. In lower vertebrates causes dispersion of melanocytes (amphibians, reptiles). -P.T. no exact function, but possibly FSH, LH in some species. |
|
|
NEUROHYPOPHYSIS
-Components (2): |
1. Nonmyelinated nerve fibers of the Hypothalamo-hypophyseal Nerve Tract comprise most of this part of pituitary.
2. Pituicytes, which considered to be modified neuroglial elements. As usual, very vascular |
|
|
NEUROHYPOPHYSIS
-Actions of ADH: |
Antidiuretic hormone (ADH; vasopressin) produced primarily by neurons of supraoptic nucleus of hypothalamus
-Travel down H-H Tract & stored in pars nervosa till used. -ADH increases tubular water absorption in kidney (mainly collecting tubules). -Minimal vasopressor effect. |
|
|
NEUROHYPOPHYSIS
-Actions of Oxytocin: |
-Oxytocin produced primarily by neurons of the paraventricular nucleus of the hypothalamus.
-Also travels down H-H tract and stored in pars nervosa till used. -Oxytocin stimulates milk ejection reflex in mother after animals born. -Also, stimulates myometrium of uterus during estrus and at parturition |
|
|
NEUROHYPOPHYSIS
-Produces (2): |
1. ADH (vasopressin)
2. Oxytocin 3. |
|
|
PINEAL GLAND
-Originates from: -Components (3): |
-Small cone-shaped organ originates from roof of diencephalon to which remains attached.
-Has capsule, CT septa forming indistinct lobules -Pinealocytes (Chief Cells) -Astrocytes |
|
|
PINEAL GLAND
-Pinealocytes (Chief Cells) -Description: |
main cells thought to be modified glia.
|
|
|
PINEAL GLAND
-Astrocytes -Description: -Function: |
+Glial cells.
+Also, may see brain sand (radiological landmark), melanin pigment. + Produces melatonin from serotonin |
|
|
PINEAL GLAND
-Main Functions (3): |
1. Acts as a “biological clock” in some animals to help regulate rhythmic changes in secretory activity of gonads, and possibly other organs.
2. Acts as a Photoreceptor in lower vertebrates. 3.Slows Aging Process ? Helps Prevents Jet Lag ? Stimulates Immune System ? |
|
|
THYROID GLAND
-Location/Anatomic Feature: |
+Caudal larynx/Cranial trachea in most mammals. +Consists of 2 lobes connected by isthmus.
-In pigs, rt. & lt. lobes fused ventrally. -In birds, adjacent to common carotid arteries |
|
|
THYROID GLAND
-Microscopic Features: |
Stroma of CCT forms capsule. Also Perifollicular CT, mainly reticular
|
|
|
THYROID GLAND
-1. Thyroid Follicles -Description: |
in general spherical, but vary in shape/size.
|
|
|
THYROID GLAND
-2. Follicular Epithelium -Description: |
-Usually simple cuboidal, but varies.
-Underactive = lower, -Overactive = taller epithelium. |
|
|
THYROID GLAND
-3. Colloid -Description: |
Is the stored secretory products of the follicular cells.
|
|
|
THYROID GLAND
-4. Parafollicular (Light or C cells) -Location: |
-Btw. follicules and among follicular cells.
-Hard to see without special staining |
|
|
THYROID GLAND
-Thyroid hormones (2): -Synthesized by: -Storage: |
-T4 = Thyroxin and T3
-follicular epithelial cells; they are able to concentrate Iodine. -attached to a globulin and stored as thyroglobulin in the colloid |
|
|
THYROID GLAND
-Uptake & Release -Stimulated by: -Brokendown by: -Released thru: -Enter: |
-TSH, thyroglobulin
-lysosomes in the follicular cells, and active hormones move into follicular cells -basal part of these cells -sinusoidal capillaries between follicular cells |
|
|
THYROID GLAND
-Major Actions (3) |
1. Influence basal metabolic rate(BMR).
-Only minimal amount of energy needed to maintain normal body function. 2. Influence normal growth and development in conjunction with other hormones 3. Produce Calcitonin |
|
|
CALCITONIN
-Produced by: -Major Action: |
-Parafollicular(C) cells.
-Lower/ regulate blood calcium levels. |
|
|
CALCITONIN ACTIVITY
Increased blood calcium level: |
++ Increase receptors (parafollicular cells)secrete calcitonin which inhibits:
1)osteoclastic activity 2) Intestinal absorption of calcium 3) increase: kidney excretion of calcium decrease: blood calcium level |
|
|
BRACHYDONT
-DENTIN: -Similar to: -Types -Striations: |
– Similar to bone but harder & acellular
• Inorganic = hydroxyapatite crystals (Ca++ salts) • Organic = Type I collagen, GAGS – Striations = dental tubules-> house odontoblast processes (Tomes fibers) |
|
|
PTH
-Secreted in response to: -2 Functions: |
-Low Blood Calcium Levels
1. Regulate Blood Calcium 2. Regulates Blood Phosphorus |
|
|
PTH
-INCREASES Calcium by (3): |
1) stimulating osteoclasts to reabsorb bone
2) stimulating synthesis of vitamin D => increases Ca2+ absorption from gut 3) causing decreased Ca2+ elimination through the kidney |
|
|
PTH
-Decreases Phosphorus by: |
– Decreases phosphate absorption in renal tubules thus
Increasing phosphate excretion in the urine |
|
|
If you remove the parathyroid glands while performing a
thyroidectomy, you must watch for: |
decreased blood Ca2+ levels
|
|
|
ADRENAL CORTEX
– Zona Glomerulosa -Produces: -Functions: |
-Mineralocorticoids (Aldosterone)
– Acts on Distal Tubules of Kidney to increase sodium absorption => increase water absorption => increase blood pressure |
|
|
ADRENAL CORTEX
– Zona Fasciculata (& Zona Reticularis) -Produce: -Functions: |
-Glucocorticoids (Cortisol; Corticosterone)
-– Metabolism of carbohydrates, proteins, fats • Gluconeogenesis (production of glucose from amino acids) • Promote protein and lipid breakdown • Suppress immune response in various ways |
|
|
ADRENAL CORTEX
– Zona Reticularis (& Zona Fasciculata) -Produce: -Functions: |
-Sex Hormones (Dehydroepiandrosterone - DHEA)
-– Produced in small amounts – Weak androgen – Virilizing & anabolic effects - can be converted into testosterone and estrogen |
|
|
Regulation of Cortical secretion
-Zona Glomerulosa -Trigger: -Cascade: |
-Low Na2+ and/or Low BP
-RENIN from JG cells in Kidney -Angiotensinogen--> Angiotensin I -Angiotensin I--> Angiotensin II -With ACE enzyme |
|
|
Regulation of Cortical secretion
RESULT -Antiotensin II acts on: -To Produce: -Which acts on: -To Increase: |
- ZG to produce
- Aldosterone which acts on - Distal Tubules of the kidney to increase - Na2+absorption => increases water absorption => increases blood volume which results in increased Blood Pressure. |
|
|
Regulation of Cortical secretion
-Zona Glomerulosa -Feedback: |
Increased Na+ & blood pressure levels provide
NEGATIVE feedback for the cascade |
|
|
ACE Inhibitors:
|
class of pharmaceuticals that reduce blood pressure
|
|
|
Regulation of cortical secretion
-Zona Fasciculata (zona reticularis) -Trigger: -Cascade: |
-Low Cortisol Levels
-CRH from Hypothalamus stimulates release of -ACTH from Pars Distalis (Basophils) and acts on -Zona Fasiculata to cause Increased Cortisol Levels |
|
|
Regulation of cortical secretion
-Zona Fasciculata (zona reticularis) -Results: -Feedback: |
- Numerous Results
- Increased Cortisol levels provides NEGATIVE feedback and less CRH is produced. |
|
|
ADRENAL MEDULLA
-1. Innervated by: -2. Acts like a: -3. Secretes -4. Response in the body is: |
1. Sympathetic preganglionic neurons from thoracolumbar
spinal cord 2. Sympathetic postganglionic neuron 3. Catecholamines (epinephrine ; norepinephrine) 4. “Fight or Flight” (sympathetic response) |
|
|
ADRENAL MEDULLA
-"Fight or Flight" Sympathetic Response -Results (3): -Hormones stored in: |
• Increases blood glucose
• Increases heart rate/BP • Vasoconstriction in skin/ Vasodilation in muscles -Hormones stored in granules |
|
|
ENDOCRINE PANCREAS
-3 Main cell types in the Islets of Langerhans: |
– Alpha (α)
– Beta (β) – Delta (Δ) |
|
|
Pancreatic Islets
set off from surrounding exocrine tissue by: |
a thin "capsule" of reticular
connective tissue - very difficult to see ! |
|
|
PANCREATIC ISLETS
-Characteristics: |
Highly Vascularized
-Each islet is essentially a capillary bed surrounded by secretory cells. |
|
|
PANCREATIC ISLETS
-ALPHA CELLS -Location: -Numbers: -Secrete: -Trigger: -Response: -Result: |
• NOT distinguishable with H&E stains
• peripherally located in Islets • fewer numbers than Beta cells • Glucagon -Hypoglycemia -Glycogenolysis in response to hypoglycemia (⇑ glucose) -Increase in blood Glucose |
|
|
ENDOCRINE SYSTEM
PANCREATIC ISLETS -B Cells: -Location: -Numbers: -Secrete: -Trigger: -Response: -Result |
• NOT distinguishable with H&E stain
• usually more central in Islets • most numerous of all the islet cells • Insulin -High levels of glucose in the blood -Promotes cellular uptake of glucose -Decrease in blood glucose levels |
|
|
ENDOCRINE SYSTEM
PANCREATIC ISLETS -Delta Cells: -Location: -Numbers: -Secrete: -Functions: |
• NOT distinguishable with H&E stain
• variable locations within the pancreatic islets • much less numerous than Alpha and Beta cells (3-10%) • secrete Somatostatin – multifunctional – inhibits release of glucagon, insulin, gastrin, secretin, and other hormones |
|
|
ENDOCRINE DISORDERS
-Most Common: -Less Common: |
MOST COMMON:
-Addison's Disease (Hypoadrenocorticism) -Cushing's Disease (Hyperadrenocorticism) -Hyperparathyroidism -Hypothyroidism -Diabetes LESS COMMON -Hypoparathyroidism -Hyperparathyroidism -Acromegaly (excessive secretion of growth hormone) |

