![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
20 Cards in this Set
- Front
- Back
|
list the stages/features of the electro cardiogram
|
p wave is atrial depolarisation
qrs ventricular depolarisation t wave- ventricular repolarisation p-q interval - av node conduction time q-t ventricular systole t-q interval - ventricular diastole r-r interval time between heart beats |
|
|
5 things that the cardiac cycle involves
|
Phases in pumping action of heart-pump cycle
Opening and closing of valves Changes in aortic, ventricular and atrial pressure, contraction and relaxation of heart muscle Changes in ventricular volume Heart Sounds |
|
|
outline the various stages of the cardiac cycle starting from ventricular filling
|
ventricular filing
atrial contraction isovolumetric contraction ventricular ejection isovolumetric relaxation ventricular filling |
|
|
what is venous return
what is isovolumetric contraction ventricular ejection isovolumetric relaxation ventricular filling |
Venous Return: Blood returning to the heart from the systemic circulation and pulmonary circulation passes through the AV valves under its own pressure
Isovolumetric contraction: Ventricles contract but pressure is not yet enough the open semilunar valves therefore ventricular volume remains constant Ventricular Ejection: Exit of blood from the ventricles Isovolumetric relaxation: Ventricles relax but too much pressure still to allow AV valves to open and not enough pressure to maintain semilunar valves open therefore all valves are shut and there is no change in blood volume in ventricles Ventricular filling: Blood enters ventricles |
|
|
what is aortic pressure used as
what is the minimum pressure reached when does pressure increase what is dicrotic notch caused by what is the average aortic pressure occuring in the cardiac cycle |
Blood pressure measurement
Diastole-Aortic valve closed Decline as blood is leaving aorta Minimum reached is diastolic pressure Aortic valve opens and aortic pressure increases rapidly, maximum is systolic pressure Dicrotic notch is caused by shutting of Aortic valve Average aortic pressure occurring in cardiac cycle is mean arterial pressure |
|
|
formulae for pp is what
what is the average pp in the normal healthy adult formulae for MAP What is the average MAP occuring in the cardiac cycle |
PP=SP-DP
In normal healthy adult: PP=120mmHg-80mmHg=40mmHg If high can indicate hardening of arteries MAP=DP+(PP/3) In normal healthy adult MAP=80mmHg+1/3(40)=93.3mmHg Not average between DP and SP. Due to aortic pressure in a cardiac cycle being nearer max for less time than min values |
|
|
volume of blood in the ventricle at the end of diastole is?
what is esv how to work out stroke volume define ejection fraction |
Volume of blood in the ventricle at the end of diastole is EDV
Volume of blood in the ventricle at the end of systole is ESV SV=EDV-ESV 70ml=135ml-65ml 65ml blood left in ventricle at end of systole Ejection fraction (EF) ratio of the volume ejected in one beat to the volume immediately prior to ejection EF=SV/EDV 0.52=70/135ml 52% |
|
|
explain how the 2 sounds lup and dup occur in the cardiac cycle
what are'nt the sounds caused by |
‘lub’ ‘dup’
First sounds occurs at start of systole when AV valves close. Second at start of diastole when semi lunar valves close Not snapping shut of valves Turbulent rush of blood through valves as they narrow and close |
|
|
what is chd caused by
what does plaque restrict what type of things can it lead to |
Due to accumulation of atherosclerotic plaques in coronary arteries
Plaques restrict blood flow to the myocardium Can lead to chest pain (angina pectoris) and heart attack |
|
|
what are the risk factors of coronary heart disease
|
Risk factors:
High blood cholesterol High blood pressure Cigarette smoking Obesity Diabetes Sedentary lifestyle Genetic predisposition |
|
|
what are patients usually present with with chd
it is usual to inject patients with?? once thhe patient is stable what can be done and what does this involve |
Patients usually present with chest pain/acute heart attack
Usual to inject patients with streptokinase to break up blood clots. Once stable, can use angiography to detect blockages in coronary arteries. I nvolves the injection of a radio-opaque dye into the coronary circulation and detect blockages with X-rays. |
|
|
2 routine procedures to treat chd
|
Two routine procedures used to treat CAD
Percutaneous Transluminal Coronary Angioplasty (PTCA) Coronary Artery Bypass Graft (CABG) |
|
|
explain what does angioplasty entail
|
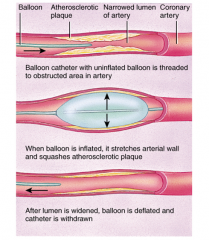
|
|
|
what are the problems associated with angioplasty
|
Problems: balloon inflation induces ischaemia (inadequate blood flow to an organ) in heart.
Damage to vessel may lead to closure of artery again in 3-6 months. |
|
|
what is done usually to counteract these problems
|
Stent is normally introduced into the artery to stop the artery narrowing again (restenosing).
|
|
|
what is bypass grafting
|
Bypass grafting:
Normally use the saphenous vein from the leg. Routine to have between 2 and 4 grafts to bypass blocked arteries. |
|
|
what are the problems associated with cabg
|
Problems:
Open chest surgery. Involves stopping the heart. Grafts can restenose. |
|
|
outline the congential heard disease
ventral defect and septal defect |
Septal defect: Allows blood to flow directly left to right
Venticular defect caused by incomplete development of septum. Oxygenated and deoxygenated blood mix 1:500 births |
|
|
outline the co arcation of the aorta
and patent ductus arteriosus |
Coarctation of the aorta: aorta too narrow, flow reduced, left ventricle pumps harder, high bp.
Patent ductus arteriosus: in some babies, ductus arteriosus, a temporary blood vessel between pulmonary trunk and aorta remains open. Blood destined for aorta instead flows to lower pressure pulmonary trunk, increasing trunk blood pressure and overworking ventricles. |
|
|
explain the tetralogy of the fallot
and the prevalence rates |
4 defects. Ventral septal defect, aorta that emerges from both ventricles, stenosed pulmonary valve and enlarged right ventricle. Very little blood reaches pulmonary circulation. Therefore cyanosis (lack of O2 in blood) occurs -blue baby. 1:2000 births
|

