![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
17 Cards in this Set
- Front
- Back
|
outline the 3 main functions of the heart
state the ultimate role of the heart |
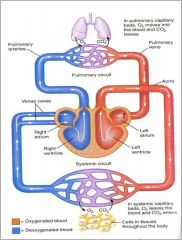
Propels blood through blood vessels to various organs
Blood carries O2 and nutrients to tissues and removes CO2 and waste Performs sensory and endocrine functions that regulate cardiovascular variables such as blood volume and pressure Ultimate role ‘to provide adequate blood flow to all the organs and tissues of the body’ |
|
|
outline the heart anatomy features that are involved in te cardiac cycle
|
he
|
|
|
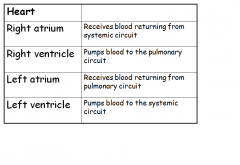
outline the function of all the ventricles and all the atria
|
|
|
|
outline what happens in pulmonary capillary beds
and also in systemic capillary beds |
|
|
|
defin autorhythmicity
pacemaker cells where are pacemaker cells located what do conduction fibres do? how? what makes up the conduction system of the heart |
Myogenic-signals itself
Autorhythmicity-generates own rhythm Pacemaker Cells- spontaneously generate action potentials Located in Sinoatrial Node (upper right atrium) and AtrioVentricular Node (near tricuspid valve in interatrial septum) Conduction fibres conduct AP through the myocardium (4M/s). It has low electrical resistance. Pacemaker cells and Conduction fibres make up conduction system of heart |
|
|
what allows the rapid transmission of action potentials to occur
|
Rapid transmission of AP from pacemakers to conduction fibres to contractile cells is possible because all cardiac cells are connected by Gap junctions, inside intercalated disks
|
|
|
what else do intercalated disks contain and what is the benefit of these
|
Intercalated disks also contain desosomes which are protein fibres which form physical bonds between cells to resist mechanical stress.
This enables myocardium to resist stretching which occurs every time heart fills with blood. |
|
|
outline Initiation and Conduction of an Impulse during a Heartbeat
|
Impulse initiated SA node →AV node via conduction fibres and through most of atrial muscle
AV node transmits AP less rapidly, therefore delayed by 0.1s AV node →atrioventricular bundle (bundle of His) in interventricular septum Signals splits into left and right branches to ventricles From the bundle branches, signals travel through a network of branches known as Purkinje fibres which spread through ventricular myocardium |
|
|
outline the places where the action potential passes through in order
|
1. sinoatrial node (pacemaker)
2. av node 3. av bundle of his 4. right and left bundle branches 5. purkinje fibres |
|
|
what do pacemaker cells fire
after and action potiential what happens to the pacemaker cell what are slow depolarisations known as what are they caused by |
Pacemaker cells fire AP spontaneously-doesn’t have a steady resting potential
After AP, pacemaker cell immediately depolarises slowly until membrane potential reaches threshold, which triggers next AP. Slow depolarisations are known as pacemaker potentials caused by Changes in membrane permeability to different ions. |
|
|
outline the 4 stages of an action potential in a cardiac contractile cell
i.e. the 5 points on the graph 0-4 |
Cells responsible for the contraction of the heart.
0- Depolarisation PNa, into cell, massive rise in MP to +30-+40mV. 1- Repolarisation Na channels inactivate, ↓PNa . MP more –ve. ↓ PK & open Ca channels PCa, MP repolarises but counteracts ↓PNa. 2-Plateau K channels stay shut, Ca channels stay open, keep membrane depolarised. 3-Repolarisation PK (delayed rectifier channels) K out of cell. MP more –ve. Inward rectifiers open due to -ve MP. Ca channels close, membrane repolarised ending AP. 4-Resting potential PK, PNa and PCa at resting values. PK > PNa & PCa membrane potential |
|
|
what does an electrocardiogram do
how is it recorded why can it be done what makes the amplitute larger |
Records the spread of electrical current through the heart as a function of time through the cardiac cycle.’
Recorded by means of electrodes placed on the skin. Electrical activity generated by muscle tissue spreads through the body because body fluids act as conductors. More synchronised the activity, the larger the amplitude. |
|
|
what did eithovens triangel propose
|
Equilateral triangle surrounding heart
Right arm, left arm and left leg. Electrodes connected to an oscilloscope |
|
|
outline what the p wave
qrs complex t wave all stand for then write down all the intervals and say which one is which |

loook at the diagram above
|
|
|
what are arrythmias
|
Abnormal SA firing causes fast (more than 100 bpm)
Or slow (less than 50 bpm) heart rates. |
|
|
outline the 3 different types/modes of arrythmias
|
Altered conduction through the AV node causes degrees in heart block.
Third degree block no conduction though the AV node causing dissociation between atrial and ventricular contractions, lethal. Depolarisation can occur from electrical signal outside the conduction pathway, causing PAC or PVC. Not usually significant. Fibrillations, no longer synchronised heart beat. Can’t pump blood efficiently round body if ventricular. Deadly. + Atrial fibrillation, weakness but not deadly as ventricles still contract sufficiently |
|
|
when is the ecg important
|
ECG is an important tool in the diagnosis of heart conditions
|

