![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
88 Cards in this Set
- Front
- Back
|
Black tarry stools
|
Anemia - GI Bleed
|
|
|
No leafy greens
|
Anemia - low folate levels
|
|
|
Paresthesias in hands and feet
|
Anemia - Low B12
|
|
|
Anemia in African descent?
|
Sickle Cell or G6PD
|
|
|
Anemia in Asian descent?
|
Thalassemia
|
|
|
What are the four initial labs for an anemia work-up?
|
Complete Blood Count
Reticulocyte Count Mean Cell Volume Peripheral Blood Smear |
|
|
How is an uncorr reticulocyte count corrected?
|
(uncorr retic %) x (pt HCT / nml HCT)
|
|
|
Are there arbitrary good and bad values for reticulocyte counts?
|
No - reticulocyte counts must be interpreted in light of a patient's condition.
|
|
|
What are the causes of a high reticulocyte count?
|
1) Acute blood loss (last 5-10 days)
2) Chronic blood loss 3) Hemolysis |
|
|
What are the causes of a normal MCV anemia?
|
1) Renal Failure (low EPO)
2) Aplastic Anemia 3) Endocrine/Thyroid Disorders 4) Pure RBC Aplasia 5) Myelophthisic Process (CA mets to the marrow) |
|
|
In general, what causes, high MCVs?
|
A high MCV indicates a problem with RBC maturation, such as DNA synthesis
|
|
|
Myelodysplasia
|
Myelodysplasia is a diverse collection of neoplastic disorders of hematopoietic stem cells. Formerly called "pre-leukemia"
|
|
|
What are some specific causes of high MCV anemia?
|
B12 & Folate Deficiency
Chemotherapy Myelodysplasia |
|
|
In addition to the standard, what additional labs should be added for a high MCV?
|
1) B12 & Folate
2) Marrow Aspirate |
|
|
Describe the work-up for normocytic, macrocytic and microcytic anemia
|
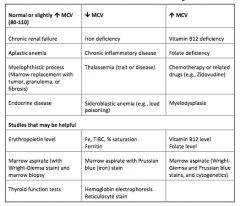
|
|
|
What are three ways to evaluate an Iron deficiency?
|
1) Marrow macrophages won't stain with Prussian blue.
2) Serum ferritin levels fall 3) Increases in Total Iron Binding Capacity |
|
|
What heme precursor level may be evaluated to determine if iron deficiency is affecting red cell maturation?
|
Protoporphyrin
|
|
|
What are sideroblasts?
|
Iron granules in the cytoplasm of bone marrow erythroid precursors.
|
|
|
What are the two major characteristics of iron deficient anemia?
|
1) Low reticulocyte index
2) Low MCV |
|
|
What work-up should all anemic adult males and anemic post-menopausal females receive?
|
Fecal hemoccult to exclude a malignant GI bleed.
|
|
|
What are some of the signs and symptoms of iron deficient anemia?
|
* Smooth, sore tongue
* Spooning of fingernails * "web" high in esophagus c/dysphagia * Pica (ice eating) |
|
|
What is the usual treatment for iron deficiency?
|
Ferrous sulfate tablets PO tid. Empty stomach.
|
|
|
How do you measure improvement of iron stores after therapy?
|
Ferritin levels will return to normal. This may take months, depending on the deficit.
|
|
|
What is the major problem in Anemia of Chronic Inflammation?
|
Iron sequestration. There's enough iron, but the marrow can't use it.
|
|
|
What's the molecule thought to be behind ACI?
|
Hepcidin production is thought to increase with inflammation, leading to iron sequestration
|
|
|
What's the major issue with anemia and renal failure?
|
EPO production falls of with advanced/chronic kidney disease.
|
|
|
Are all blood counts affected in chronic kidney disease?
|
No, platelets and WBCs are usually unaffected.
|
|
|
The FDA has posted two black-box warnings for EPO. What are they?
|
1) Risk of cancer progression
2) Risk of stroke |
|
|
What are the two major causes of iron overload?
|
1) Hereditary hemochromatosis
2) Transfusional Iron Overload |
|
|
What screening tests are used for hemochromatosis?
|
Transferrin saturation tests
|
|
|
What major complication can arise from hemochromatosis?
|
Hepatocellular carcinoma, especially in patients who develop a secondary cirrhosis.
|
|
|
What is the therapy for hemochromatosis?
|
Phlebotomy
|
|
|
What patient populations are at risk for transfusion iron overload?
|
Anemias associated with an underproduction of RBCs:
* Aplastic anemia * Myelodysplasia * Severe thalassemias |
|
|
What pharmacotherapy is available for iron overload?
|
Deferoxamine
|
|
|
Name exemplary cells of the Myeloid Lineage:
|
Neutrophils, Eosinophils, Monocytes, Basophils
|
|
|
Name exemplary cells of the Erythroid Lineage:
|
Reticulocytes, Erythrocytes
|
|
|
What bone marrow cells give rise to platelets?
|
Megakaryocytes
|
|
|
What's the lifespan of a mature RBC? What about a myeloid cell?
|
RBCs = 120 days
Myeloids last less than 24 hours |
|
|
What are the major growth factors of the bone marrow?
|
1) Erythropoietin
2) Thrombopoietin 3) GM-CSF 4) Stem Cell Factor |
|
|
Where is DPG made? What biochemical pathway?
|
2,3-DPG is made in the RBC through the Luebering-Rapaport Pathway.
|
|
|
What are some of the major causes of sideroblastic anemia?
|
1) Myelodysplastic syndrome
2) Drugs (Isoniazid et al.) 3) Toxins (lead, EtOH) 4) Hereditary |
|
|
What is the fundamental problem in sideroblastic anemia?
|
Inhibition of heme synthesis.
|
|
|
Name the globin constituents of the following:
1) Hg-A 2) Hg-A2 3) Hg-F 4) Hg-H |
1) Hg-A alpha2-beta2
2) Hg-A2 alpha2-delta2 3) Hg-F alpha2-gamma2 4) Hg-H beta4 (only in alpha thal syndrome) |
|
|
What are some of the symptoms of sideroblastic anemia?
|
Microcytic, anisocytic RBCs. Normal WBCs and PLTs.
|
|
|
What's the function of transferrin?
|
Binds extracellular iron. Transferrin/Iron complex is then endocytosed by cells with a Transferrin receptor
|
|
|
Proteins modulating intestinal iron importation include:
|
* Iron Regulatory Proteins - block translation of ferritin, ferroportin when iron is low
* Hepcidin - decreases intestinal absorption of iron. Produced by liver in response to inflammation |
|
|
What is the hematocrit cutoff for anemia (female and male)?
|
Female < 36%, Male < 38%
|
|
|
What are the two major questions to ask about an anemia?
|
1) Are red cells being produced appropriately?
2) Do the red cells mature normally? |
|
|
What are the three major causes of low reticulocyte counts?
|
1) Marrow is missing something it needs
2) Something's keeping the marrow from doing what it's supposed to do 3) Primary stem cell defect |
|
|
What are the two big cases were we see anemias with high reticulocyte counts?
|
1) Blood Loss
2) Hemolysis (intrinsic, extrinsic) |
|
|
What are the three major types of intrinsic hemolytic anemias?
|
1) Membrane abnormalities (hereditary spherocytosis)
2) Enzyme abnormalities (G6PD...) 3) Hb abnormalities (thal, HbS, HbC...) |
|
|
What are the extrinsic causes of hemolytic anemia?
|
1) Fragmentation hemolysis (DIC, TTP, HUS)
2) Mechanical heart valve 3) Toxins 4) Immunohemolytic anemia |
|
|
What are the three RBC membrane disorders causing hemolytic anemia?
|
1) Paroxysmal Nocturnal Hemoglobinuria
2) Hereditary Spherocytosis 3) Hereditary Elliptocytosis |
|
|
PNH
|
Paroxysmal Nocturnal Hemoglobinurea: membrane disorder with PI membrane anchor. Sensitive to complement and hemolysis. Dx by flow cytometry.
|
|
|
Hereditary Spherocytosis
|
Defect in membrane proteins akyrin, spectrin, et al. Cells "sphere up" to minimize surface area.
|
|
|
How is Hereditary Spherocytosis diagnosed?
|
Morphology and osmotic fragility test.
|
|
|
What does the Direct Coombs Test measure?
|
Complement or antibody bound to RBCs
|
|
|
What does the Indirect Coombs Test measure?
|
Circulating antibodies specific to RBCs.
|
|
|
Warm reactive antibodies do what?
|
Warm antibodies (IgG) cause extravascular hemolysis. Cells in the spleen or liver pick out the tagged RBCs and destroy them.
|
|
|
Autoimmune Hemolytic Anemia (AIHA)
|
Destruction of RBCs caused by antibodies binding to the RBC surface.
|
|
|
What are the causes of Warm Reactive AIHA?
|
1) Idiopathic
2) Drug-induced 3) Chronic Lymphocytic Leukemia or Lymphoma 4) SLE |
|
|
What are the three mechanisms of Drug-Induced AIHA?
|
1) Hapten formation (i.e., PCN binding to RBC)
2) Immune Complex Formation (Quinine + AB) 3) Apparent Cross-Specificity (Methyldopa) |
|
|
How is Warm-Reactive AIHA treated?
|
1) Steroid therapy
2) Splenectomy |
|
|
What are the causes of Cold-Reactive AIHA?
|
1) Idiopathic
2) Mycoplasma pneumonia (resolves with infection) 3) Infectious mononucleosis (resolves with infection) 4) Chronic Lymphocytic Leukemia/Lymphoma 5) Drug-induced |
|
|
What are the symptoms of Cold-Reactive AIHA?
|
Acrocyanosis - plugging of the vasculature of the extremities by agglutinated RBCs.
|
|
|
What are the three microangiopathic hemolytic anemias?
|
1) Disseminated Intravascular Coagulation
2) Thrombotic Thrombocytopenic Purpura 3) Hemolytic Uremic Syndrome |
|
|
DIC
|
Disseminated Intravascular Coagulopathy: loss of fibrinolysis and consequent hypercoagulation state consumes clotting factors and infarcts small vessels. Therapy is supportive (organ support, transfusions.)
|
|
|
What are the general principles of managing hemolytic anemia?
|
1) Folic acid supplements
2) Transfusion 3) Splenectomy = Infection, so ABs if febrile 4) Aplastic Crisis (e.g. parvo on SCA) will require short-term transfusion 5) Monitor reticulocyte counts for improvement |
|
|
What are the compositions for the following hemoglobins: A, A2, F, H, Barts
|
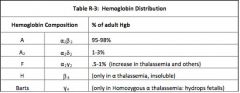
|
|
|
A SCA patient suddenly drops her hematocrit to 12% What's the differential dx?
|
1) Sequestration Crisis - sudden, massive splenomegaly due to trapping of RBCs by splenic REs
2) Aplastic Crisis: temporary cessation of erythropoiesis (parvo or bacterial) |
|
|
What neurotransmitter is depleted during a sickle cell crisis? How might this be treated?
|
Nitric oxide is depleted from the vascular endothelium. Sildenafil is a possible treatment.
|
|
|
What are the vaso-occlusive complications of SCA?
|
1) Acute pain crisis
2) Dactylitis 3) Splenic sequestration 4) Osteonecrosis |
|
|
What are the hemolytic complications of SCA?
|
1) Pulmonary arterial hypertension
2) Priapism 3) Leg ulcers 4) Bile calculi |
|
|
What are the systemic/long-term complications of SCA?
|
1) Stroke
2) Acute Chest Syndrome 3) Renal Concentrating Problems 4) Retinopathy 5) Sickle Hepatopathy 6) Infection (asplenia, encapsulated organisms) 7) Iron Overload |
|
|
What are the causes of RBC Macrocytosis?
|
1) B-12 / Folate deficiency
2) Drugs (anti-metabolite) 3) Myelodysplasia 4) Liver disease 5) Brisk reticulcytosis |
|
|
Hypersegmented Neutrophils
|
Pathognomonic of megaloblastic anemia. Think B12/Folate, etc.
|
|
|
What lab test helps differentiate Folate from B12 deficiency?
|
Serum Methylmalonic Acid
* MMA is high in B12 deficiency * MMA is normal in Folate deficiency |
|
|
Why would a Thalassemia Major (B0) patient show significant amounts of Hb-A on her Hb electrophoresis?
|
The transfused blood contains a normal complement of Hb-A. Whole blood electrophoresis can't distinguish the two.
|
|
|
Do Alpha Thalassemias come in major and minor?
|
No, only Beta Thalassemias are rated major, intermedia, and minor. Alpha Thalassemia pts have either trait or disease.
|
|
|
What is the differential diagnosis of pancytopenia?
|
* Acute leukemia
* Aplastic anemia * marrow replacement with tumor, fibrosis, or granuloma * Drug side effect * Myelodysplasia * Occasionally deficiency of vitamin B12 or folate |
|
|
How do you diagnose pancytopenia?
|
Marrow aspirate and stain.
|
|
|
What is the treatment of choice for aplastic anemia?
|
Allogenic bone marrow transplant if a matched donor can be found.
|
|
|
What is a shift cell?
|
A young reticulocyte released early from the bone marrow which retains much of its RNA.
|
|
|
What two disease classes would give a positive result to an osmotic fragility test?
|
Hereditary Spherocytosis
Autoimmune Hemolytic Anemia |
|
|
What is the cause of pernicious anemia?
|
The majority of cases involve autoimmunity against gastric parietal cells, or antibodies to Intrinsic Factor iteself (or both.)
|
|
|
How is Pernicious Anemia diagnosed?
|
Shilling Test: Radio-labelled B-12 is given and absorption tested.
|
|
|
What procedures/diseases are commonly associated with Pernicious Anemia?
|
1) Auto-immune disorders (Graves, etc.)
2) Gastric bypass surgery 3) Crohn's |
|
|
What are the causes of a warm autoimmune hemolytic anemia?
|
* Idiopathic
* Drug-induced * CLL * Lymphoma * SLE |

