![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
42 Cards in this Set
- Front
- Back
|
What is primary hemostasis?
|
Platelet plug formation at the site of vascular injury.
|
|
|
What are the three components of primary hemostasis?
|
1) Coag system activation (secondary hemostasis)
2) Platelet activation 3) Fibrinolytic system activation |
|
|
What's the difference between hemostasis and thrombosis?
|
Hemostasis is considered an adaptive response.
Thrombosis is mal-adaptive. |
|
|
What is the basic function of the fibrinolytic system?
|
To keep thrombus formation in check.
|
|
|
What are the three elements of Virchow's Triad?
|
1) Alterations in normal blood flow (stasis)
2) Damage to the vascular endothelium (injury) 3) Alterations to the constitution of blood (hypercoagulability) |
|
|
What initiates extrinsic pathway activation?
|
The exposure of plasma factors to Tissue Factor from blood vessel adventitia.
|
|
|
What is the central product of coagulation system activation?
|
Thrombin
|
|
|
What is the major action of Thrombin?
|
To cleave Fibrinogen into Fibrin, which then polymerizes into a fibrin network, the scaffold of a clot. (Thrombin has other functions too, such as platelet activation.)
|
|
|
What are the Vitamin K dependent factors?
|
Factors II, VII, IX and X
|
|
|
What are the two "tenase complexes"?
|
Intrinsic: VIIIa + IXa
Extrinsic: Tissue Factor + VIIa |
|
|
What makes up the "prothrombinase complex"?
|
Factors Xa + Va. This complex cleaves Factor II -> IIa
|
|
|
What subset of coag factors are liver patients most likely to lack?
|
Vitamin K-dependent factors:
II, VII, IX, X |
|
|
Where do the extrinsic and intrinsic pathways merge?
|
With Factor X
|
|
|
What class of enzymes are most coagulation cofactors?
|
Serine proteases.
|
|
|
What factors are activated by thrombin in a feedback amplification?
|
Activated Thrombin (Factor IIa) will activate Factors V, VIII and XI
|
|
|
What are three coagulation inhibitors which keep thrombus formation in check?
|
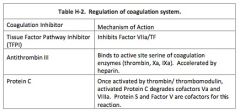
1) Tissue Factor Pathway Inhibitor
2) Antithrombin III 3) Protein C |
|
|
What coagulation regulator is specific to the extrinsic pathway?
|
Tissue Factor Pathway Inhibitor (TFPI)
|
|
|
How does Anti-Thrombin work?
|
Antithrombin (AT) irreversibly binds to the serine protease active site of coag factors (Factors IIa/Thrombin, IXa, Xa, XIa, XIIa)
|
|
|
How does Heparin work?
|
By activating Antithrombin (AT)
|
|
|
What are the two major activators of the fibrinolytic cascade?
|
1) Tissue Plasminogen Activator
2) Urokinase or uPA |
|
|
How is TPA inactivated?
|
1) Inhibition by circulating Plasminogen Activator Inhibitor 1
2) Clearance of the enzyme by the liver |
|
|
What is the role of plasmin in coagulation?
|
Plasmin degrades clots. Plasmin breaks down fibrin and fibrinogen.
|
|
|
What is the major, absolute contraindication of Plasmin inhibitors?
|
DIC
|
|
|
What does the D-Dimer test measure?
|
Specifically it measures a Plasmin-cleaved fragments of fibrin. The absence of D-Dimer fragments indicates an absence of active thrombosis.
|
|
|
Which blood test measures the factors within the INTRINSIC and COMMON coagulation pathways?
|
Activated Partial Thromboplastin Time
|
|
|
Which blood test measures the factors within the EXTRINSIC and COMMON coagulation pathways?
|
The Prothrombin Time
|
|
|
What does the Thrombin Time (TT) blood test measure?
|
The Thrombin Time assays only the final step in coagulation, the conversion of fibrinogen to fibrin.
|
|
|
What cells produce platelets?
|
Megakaryocytes, in the bone marrow.
|
|
|
What bone marrow growth factor supports megakaryocytes?
|
Thrombopoetin
|
|
|
Organomegaly of what organ my cause thrombocytopenia?
|
An enlarged spleen is likely to sequester high numbers of platelets.
|
|
|
Asplenic patients are at risk for what coagulopathy?
|
Hypercoagulopathy due to thrombocytosis.
|
|
|
What is the circulating lifespan of a platelet?
|
Platelets survive 9-10 days in the blood, although this may drop to minutes in certain pathologic conditions.
|
|
|
What two major organelle systems make up platelet cell biology?
|
1) Cannalicular system - for release of granules
2) Dense Tubular System - for Calcium release |
|
|
Give four examples of platelet adhesion factors produced by vascular endothelium
|
1) vWF
2) laminin 3) fibronectin 4) thrombospondin |
|
|
What is one adhesion protein produced by platelets?
|
Glycoprotein Ib is the main vWF adhesin.
|
|
|
Name three platelet agonists:
|
1) Collagen
2) ADP 3) thrombin 4) epinepherine 5) thromboxane A2 6) calcium |
|
|
What disorder is defined by the "pentad"?
|
Thrombotic Thrombocytopenic Purpura
1) microangiopathic hemolytic anemia 2) thrombocytopenia 3) neurologic abnormalities 4) fever 5) renal dysfunction |
|
|
What are possible causes of Reactive Thrombocytosis?
|
1) Iron deficiency
2) Inflammatory diseases |
|
|
What bone marrow signs correlate with Essential Thrombocytosis?
|
ET is myoproliferative with many, possibly bizarre, megakaryocytes.
|
|
|
How do platelets behave in Essential Thrombocytosis?
|
ET platelets are large and possibly hyperreactive. Thrombosis may be an issue.
|
|
|
1972 WEPT
|
Factors 10, 9 & 2 - Vit. K dependent
Warfarin acts on the Extrinsic Pathway PT (Prothrombin) time used to check it |
|
|
On which pathway does heparin act? Which test is used to check it?
|
The Intrinsic Pathway.
PTT (Partial Thromboplastin Time) is used to check it. |

