![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
21 Cards in this Set
- Front
- Back
How are Acute and Chronic leukemia classified?
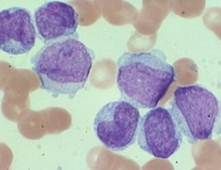
How are they different? What is this a picture of? |
Acute = blasts (immature), rapid proliferation, more rapidly fatal (<6mo without Rx). Picture was of an acute leukemia.
Chronic= mature, gradual proliferation, more indolent (2-6 yr survival without Rx). |
|
|
What are the four major types of leukemia?
|
1. Acute myelogenous leukemia = AML (most common!)- granulocytes, erythrocytes, and megakaryocytes
2. Acute lymphocytic leukemia = ALL 3. Chronic Myelogenous leukemia = CML 4.Chronic lymphocytic leukemia = CLL |
|
|
What is the most common type of acute leukemia in adults? The most common type in children?
Development of acute leukemia requires the acquisition of what? |
Adults = AML, Chldren = ALL
Acute leukemia's typically require acquisition of multiple hits (mutations) in the progenitors. |
|
|
A patient who had Hodgkin's lymphoma 5 years ago comes in with symptoms consistent with anemia, excessive mucosal bleeding, and infection. What do you suspect and why?
|
This sounds like AML that occurs post exposure to alkylating agents and chemo for Hodgkins. There is an increased risk in these patients (AML can depress cell production in bone marrow causing a pancytopenia).
|
|
|
What is a prototype for leukemia's that cause a block in differentiation?
Describe how it can cause a block in differentiation. |
Core Binding Factor (CBF) Leukemias
CBF- a complex with α and β subunits that binds with HAT (histone acetyl transferase) --> transcription of genes involved in normal blood cell development (growth arrest, differentiation, etc.) *translocations form novel fusion protein that recruits HDAC (a repressor complex) and acetylation is not possible, thus transcription doesn't occur. |
|
|
What are the three most common translocations in Acute Leukemia's involving CBF?
|
t (8;21)
inv (16) t (12;21) |
|
|
What is the prototype for gene defects related to autonomous cell proliferation?
Describe how it works and what the prognosis is. |
FLT3 (fms-like Tyrosine kinase). Mutation causes ligand-independent activation of the tyrosine kinase and constitutive activation of proliferation signals.
Very poor prognosis in AML BUT there is a targeted therapy (FLT3 inhibitors) |
|
|
What is a prototypic mutation that can result in blocked apoptosis (and is also the most common genetic lesion in AML)?
|
NPM-1 (nucleophosmin)
No one really knows what it does, but it can impair apoptosis. It is a shuttling protein (goes back and forth between nucleus and nucleolus), and plays a role in DNA, ribosome, and cell proliferation and death. |
|
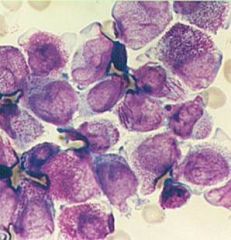
What characteristic features in this cell help identify the type of malignancy?
|
This is AML. You can make out auer rods (crystallized granules), which is a distinctive feature of large, immature, MYELOBLASTS,
*in addition, they show granulation. |
|
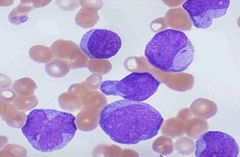
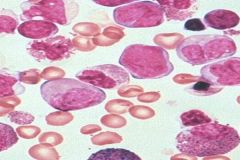
What morphologic features help you identify this malignancy?
|
This is an ALL. You can tell because small, lymphoblast looking cells without granules.
|
|
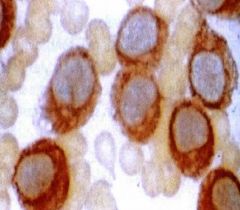
This is an MPO stain (which is positive). What type of cells do you think this is?
What else would these cells stain positive for (that is unique to their line)? |
Myeloperoxidase stains positive in MYELOID BLASTS (found in primary granules).
They are also positive for Sudan Black (which stain lipid particles in the granules). LYMPHOBLASTS are negative to both these stains. |
|
|
What CD antigen would Acute Myeloid Leukemia's be positive for? What about Acute Lymphoid Leukemias?
|
AML- CD 13 or CD33
ALL- TdT or specific B and T cell markers (CD20, CD5, etc.) |
|
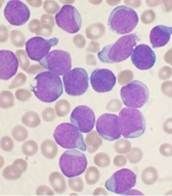
What type of AML is this? How can you tell?
|
M3 or Acute Promyelocytic Leukemia
You can make out heavy granulation and bundles of crystallized granules (Auer Rods). This is seen in APL. |
|
|
What is the unique molecular basis of AML? Why is it important to accurately diagnose this?
|
Translocation t(15;17). Which causes a novel fusion protein (PML/RAR where RAR = retinoic acid receptor).
This is a bad form of Leukemia (can lead to DIC because promyelocytes release granules causing full system clotting). There IS a unique treatment- ORAL ATRA (all trans retinoic acid). Thus, it's crucial to accurately diagnose this. |
|
|
How doe the oral ATRA (all trans retinoic acid) help with M3 (acute promyelocytic leukemia)?
|
Retinoic acid usually binds the fusion protein (PML-RAR) that is in this disease and this recruits tha bad HDAC (which blocks acetylation and transcription of necessary differentiation factors)
ATRA will occupy the PML-RAR binding site and recruit normal HAT which allow acetylation and transcription. |
|
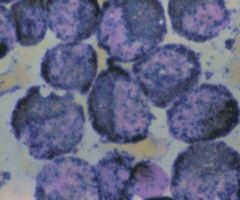
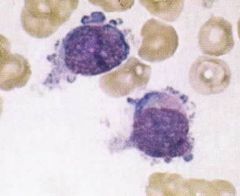
What type of leukemia might this person have (provide the FAB classification)? How can you tell? What would it possible stain positive for?
|
M4 leukemia (both myeloblast and monoblast leukemia).
M5 (just monocytic) This stains positive for NSE (non specific esterase) which corresponds to Monoblasts. |
|
This type of leukemia stains positive for NSE (non specific esterase). What symptoms might it cause patients to present with?
|

M4 and M5 (acute myelomonocytic leukemia and acute monocytic leukemia). Monoblasts stain positive for NSE.
Associated with EXTRAMEDULLARY infiltration (gums, CNS, lymph nodes, and skin) |
|
What type of Leukemia is this (include FAB classification)? What genetic condition might this individual have?
|
This is M7 (Acute Megakaryoblastic Leukemia)- note the platelets budding off of the surface of this megakaryocyte.
This is associated with Down's syndrome. |
|
|
What is the most common type of ALL (acute lymphoblastic leukemia) as indicated by the WHO classification?
What marker could you use to diagnose it? What is their FAB classification? Which occurs more commonly in children? |
Pre-B cell (80% of cases). Use TdT to diagnose! (early B cell)
L1 and L2 (L1 - childhood, highly curable. L2- Adult type, large varied cells) |
|
|
If a young 17 year old male comes to see you with presenting symptoms of a mediastinal mass and malaise, weight loss, and fever for the past 3 months, what type of ALL would you suspect? (go by WHO criteria)?
|
Suspect T-cell lymphoblastic leukemia
|
|
|
What is the FAB criteria for Burkitt's lymphoma? What about the WHO classification?
|
FAB = F3
WHO = B-cell ALL Acute lymphoblastic leukemia/lymphoma *very poor prognosis* |

