![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
22 Cards in this Set
- Front
- Back
|
Where does hematopoiesis occur in the fetus? At the end of the first trimester?
What about at birth? As an adult? |
Fetus- yolk sac
At the end of 1st trimester- liver and spleen At birth- entire skeleton (bone marrow) Adult- axial skeleton |
|
|
2 major sites from which to obtain bone marrow aspirate?
|
Iliac crest and sternum (axial skeleton)
|
|
|
How does the composition of BM change as you age?
|
As you age, fat replaces bone marrow.
|
|
|
An increase demand for blood cells (ex: chronic anemia, or myeloproliferative disorders), causes what changes to occur?
|
1. Yellow marrow can become hematopoietically active
2. Extramedullary hematopoiesis (production of blood cells outside the bone marrow, ex: liver, spleen, kidneys). |
|
|
What does the spaces between boney trabeculae hold?
What three things is it composed of? |
Bone marrow:
1.Hematopoietic cells “chords” 2. Stroma (supporting tissue) 3. Sinusoids |
|
|
Role of stromal cells in hematopoiesis?
|
1. Support hematopoietic “chords”
2. 2. Secrete growth factors (CSF) needed for stem cell survival/maturation |
|
|
T or F
It is abnormal to find hematopoietic stem cells in the peripheral blood. |
False- a small number circulate here. This is why harvesting stem cells from peripheral blood is possible.
|
|
|
What is a pluripotential cell?
What are it’s 2 major divisions? |
One that can make precursors that differentiate into all different blood cells (Myeloid= erythroid and granulocyte, Lymphoid= lymphocytes and NK cells)
|
|
|
How do you identify a hematopoietic stem cell?
Important property of pluripotent cells that allows them to retain their total number? |
Look for CD34 expression (otherwise they are rare and indistinguishable).
Self-renewal or Asymmetric mitosis |
|
|
How do you identify progenitor cells (ex: myeloid vs. lymphoid)?
|
Add Growth Factors (glycoproteins) and see them grow in vitro (CFUgm= colony forming unit granulocyte, monocyte, BFUe= burst forming unit erythroid)
|
|
|
What two growth factors are NOT produced by stromal cells of the bone marrow?
What are Interleukins? |
EPO (kidney), and Thrombopoeitin (liver)
Interleukin= cytokines produced by leukocytes that act on leukocytes |
|
|
What cytokines maintain the growth & survival or immature blood cells?
|
SCF (stem cell factor), Flt-L (Flt-Ligand), and IL-3
|
|
|
What is the mode of action of G-CSF and GM-CSF? (be specific)
|
GF binds to JAK receptor --> it dimerizes --> auto P* and P* STAT proteins -->activated STAT dimers travel to nucleus and transcribe necessary factors needed for cell maturation
|
|
|
What cytokine is most often used to mobilize peripheral stem cells? Why?
What are OTHER functions of this cytokine? |
G-CSF (increased efficacy and decreased toxicity, less broad than GM-CSF)
It also stimulates proliferation, recruitment of cells , suppression of apoptosis, and increases phagocytic ability of polys. |
|
|
What is a primary Granule?
What do the secondary granules of Eos and Basophils contain? |
Primary= Azurophilic. Lysosomes (contain Myeloperoxidase)
Eos- MBP (major basic protein) Basophils- Histamine, Leukotriene |
|
|
Stages of Poly formation? How long does the process take? How long do poly’s live?
|
Proliferation: Myeloblast> Promyelocyte > Myelocyte
Maturation: Metamyelocyte>Band>Seg (mature poly) Process takes ~10 days In blood for ~10 hrs, can enter tissue, die in about 1 day |
|
|
A person runs all the way to the doctor’s office and immediately has their blood drawn. Their WBCs are elevated but they are completely healthy. Why?
|
Epinephrine causes demargination of WBCs. Only circulating pool of WBCs is measured on a CBC.
Usually it is 50% circulating, 50% marginated |
|
|
What characteristic finding on a CBC would you expect to see when a patient has an acute infection or sepsis?
What findings seen on a peripheral blood smear would be consistent? |
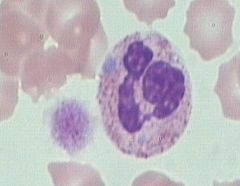
Left Shift (more bands beings pumped out, even metamyelocytes). Also sharp rise in WBC count.
Toxic granulations (dark primary granules and cytosolic vacuolization) & Dohle bodies (remnants of RER that stay within the cytoplasm) |
|
|
What is a May-Hegglin anomaly? What can it sometimes resemble?
|
AD, GIANT platelets, thrombocytopenia, and WBC inclusions (Dohle body-like)
You can tell that it’s not Dohle b/c not seen in infection and patient doesn’t bleed typically. |
|
|
What is the Pelger-Huet anomaly? What is pseudo-Pelger-Huet
|
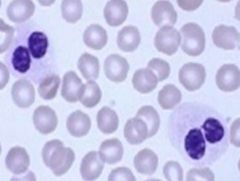
Congenital disorder (AD), granulocytes nuclei can’t segment properly “pince-nez” (spectacle cells)
Acquired form= pseudo-Pelger Huet. Seen in myelodysplasia. |
|
|
Hypersegmentation of the polys should trigger what workup in patients?
|
Should strike concern for Megaloblastic anemia. Workup for folic acid or B12 deficiency.
*can also be caused by chemotherapeutic agents that impair DNA synthesis. |
|
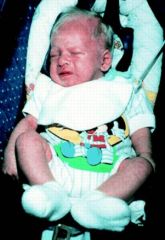
Baby with silver hair and red eyes (when light is shone on it), also has frequent infections with strep. What condition is this and what do anticipate seeing on a peripheral blood smear?
|

Chediak-Higashi (AR, problem with vesicle transport)
1. Fusion of primary lysosome --> chunky granules 2. Failure to fuse phagosome and lysosome --> infections 3. Abnormal melanosome transport into keratinocytes OCA (albinism) |

