![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
166 Cards in this Set
- Front
- Back
|
The anticoagulant most often used for cell counting is
|
EDTA ( Lavender top)
|
|
|
The anticoagulant most often used for coagulation testing is
|
Sodium Citrate ( Light Blue)
|
|
|
The main site of hematopoiesis in the fetus from the second to the seventh month is the:
|
Liver
The fetal liver assumes responsibility for hematopoiesis during the second month, with the yolk sac nucleated RBCs migrating to the liver and remaining in the liver until the seventh month. From the third to the sixth month, splenic hematopoiesis also occurs. At 7 months of fetal life it shifts from the liver to the bone marrow, which then becomes the major site in the fetus. |
|
|
In adulthood, the main site of hematopoiesis is in the:
|
Flat bones and the proximal ends of long bones are were hematopoiesis takes place. This includes pelvis, sternum, ribs, and skull.
|
|
|
The hematopoietic marrow of the bone is
|
Red marrow
|
|
|
The main function of the marrow is to:
|
Is to supply mature hematopoietic cells into the peripheral blood in a steady state condition as well as to respond to increased demands.
|
|
|
The site most often used for bone marrow biopsy and aspiration in adults is the:
|
Iliac crest
|
|
|
A bone biopsy is needed when:
|
Diagnosis and staging of hematologic disease is needed.
|
|
|
Marrow cellularity is determined by comparing:
|
The percentage of marrow space occupied by hematopoietic cells to the percentage of marrow space occupied by fat.
|
|
|
The M:E ratio is determined by dividing the number of:
|
Nucleated RBCs into the sum of all cells belonging to the granulocytic series.
|
|
|
The normal M: E ratio in adults is:
|
3:1
|
|
|
The RBC membrane is a (n):
|
The structure that regulates volume and shape
|
|
|
The main integral (extrinsic) protein in the RBC is:
|
Glycophorin
|
|
|
The main peripheral (intrinsic) protein in the RBC is:
|
Spectrin
|
|
|
The average life span of a normal RBC is__ days.
|
120
|
|
|
Spherocytes and bite cells are evidence of:
|
Membrane loss, G6PD deficiency
|
|
|
The purpose of the cationic pumps in the RBC are to:
|
Maintenance of cell volume and shape by pumping Na+ out of cell and K+ into cell
|
|
|
The carrier protein that delivers iron to the RBC membrane is:
|
Transferrin
|
|
|
If one of the normal enzymatic steps in heme synthesis is blocked of deficient, the resultant disorders are called:
|
Porphrias
|
|
|
The globin chains that are usually present only during embryonic development are:
|
Epsilon and Zeta
|
|
|
All normal adult hemoglobins contain a dinner of which chain?
|
Alpha
|
|
|
The RBC organic phosphate 2, 3-DPG:
|
• Is one of the most important controls of hemoglobin affinity of oxygen
• Is an inverse relationship between amount of 2, 3-DPG available for binding by Hgb and the affinity for Hgb for O2 • Produced via anaerobic glycolytic pathway (Embden- Meyerhof pathway) • When Hgb bind 2, 3-DPG, O2 decreases • When plasma level of 2, 3-DPG decreases, Hgb 2, 3-DPG is released, and Hgb affinity of O2 increases • Adequate tissue oxygenation requires adequate supplies of 2, 3-DPG to encourage Hgb to release O2 to tissue |
|
|
The hemoglobin pigment that cannot be converted to oxyhemoglobin is:
|
Sulfhemoglobin
|
|
|
Ninety percent of the ATP required for RBC energy is produced by the:
|
Embden-Meyerhof glycolytic pathway
|
|
|
A deficiency in the hexose monophosphate shunt results in:
|
Heinz bodies
The amount of reduced glutathione becomes insufficient to neutralize intracellular oxidants. This results in globin denaturation and precipitation as aggregates (Heinz bodies). |
|
|
The majority of senescent RBC’s are removed from the body by______ hemolysis (catabolism).
|
Extravascular hemolysis
|
|
|
The growth factor responsible for regulation of RBC production is?
|
Erythropoietin
|
|
|
The RBC precursor that is most plentiful in an aspiration from the normal adult marrow is the:
|
Rubricyte
|
|
|
Reticulocytes may be seen in Wright’s stained smears as:
|
Reticulocytes appear blue-gray on the Wright. They are referred to as polychromatophic.
|
|
|
The normal mature RBC is a:
|
round, biconcave disc-shaped, anuclear cells measuring approximately 7-8 microns in diameter with an internal volume of 80-100 fL.
|
|
|
Iron found in the bone marrow stores is in the form of:
|
Hemosedrin
|
|
|
The packed cell volume is also known as the:
|
Hematocrit
|
|
|
The normal hemoglobin level for people living at high altitudes would be:
|
Higher than the normal given range
|
|
|
Approximately ____ percent of RBC’s are replaced daily in the adult
|
1%
|
|
|
The “rule of three” suggests that:
|
RBC x 3 = HgB x 3 = Hct
|
|
|
The anemia of a patient who’s MCV=65.1 fL, MHC=22.2 pg, and MCHC=0.295 g/L is termed:
|
Microcytic hypochromic
|
|
|
recommended method for hemoglobin measurement is spectrophotometric absorbance reading of:
|
540 nm wave length
|
|
|
Reticulocytes are:
|
Are immature red blood cells, typically composing about 1% of the red cells in the human body. Reticulocytes develop and mature in the red bone marrow and then circulate for about a day in the blood stream before developing into mature red blood cells. Like mature red blood cells, reticulocytes do not have a cell nucleus. They are called reticulocytes because of a reticular network of ribosomal RNA that becomes visible under a microscope with certain stains such as new methylene blue.
|
|
|
Body stores of iron are most closely paralleled by serum levels of:
|
Ferritin
|
|
|
Porphyrias are disorders of:
|
That involve a block in porphyrin synthesis that is due to a defect in the enzymes in the pathway of heme synthesis.
|
|
|
The hematologic parameter that is most sensitive to macrocytosis is:
|
Hematocrit
|
|
|
When reticulocytes are stained with supravital stains, the substance that stains is:
|
RNA
|
|
|
Hemoglobin in the ferric (Fe 3+) state is called:
|
Methemoglobin
globin + heme (Fe3+) = methemoglobin Methemoglobin, which is inactive -Because this form is useless to the body, an enzyme, called diaphorase is used to reduce the methemoglobin back to normal ferrous (Fe2+) hemoglobin that can carry O2.The Fe2+ version of heme is called ferroheme; ferroheme is the active, O2 binding form of the heme group toward oxygen transfer. globin + heme (Fe2+) = hemoglobin (ferroheme) |
|
|
The most common adult hemoglobin is:
|
Hgb A
|
|
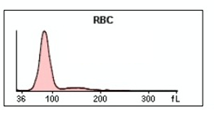
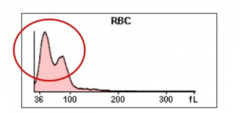
The RBC histogram below is indicative of:
|
Normal
|
|
|
A variation in size of RBCs is termed:
|
Anisocytosis
|
|
|
A variation of shape of RBCs is termed;
|
Poikilocytosis
|
|
|
Macrocytes can be defined as RBC’s with a:
|
MCV>100fL
The term macrocytosis refers to a blood condition in which red blood cells (RBC) are larger than normal. Macrocytosis is reported in terms of mean corpuscular volume (MCV) larger than 100fL |
|
|
Macrocytosis can be caused by:
|
• Megaloblastic anemias
• Shift reticulocytes (Hemolysis) • Anemia of Liver Disease |
|
|
Microcytes can be caused by:
|
• Iron-related disorders
• Sideroblastic anemias • Anemia of Chronic Disorders • Thalassemias o Beta-Thalassemia Major o Beta-Thalassemia Minor o Alpha Thalassemia (Hemoglobin H Disease) o Alpha Thalassemia (Hydrops Fetalis) • Lead poisoning |
|
|
Any RBC having an increased central area of pallor is said to have:
|
Hypochromia/hypochromic as Central pallor > 1/3
|
|
|
A Wright’s stained smear of a patient with an elevated reticulocyte count will show:
|
• With Wright’s stain, reticulocytes stain a slight blue-purple.
• Higher amounts of retics will be presented (equal or greater than 4% of the Total RBC Count) due to attempted compensation for anemias. |
|
|
Cells that are more often artifactual than a true result of a disease process are:
|
• Infected with parasites that are outside the norm of a normal histological examination. These artifacts interfere with the normal histological processes of the body and can change tissue appearances/structures.
• Examples are: o Malaria (Ringed forms, Schizonts & Gametocytes) Plasmodium vivax P. falciparum¬ P. ovale P. malariae o Babesiosis (Multiple ringed forms) Blue, ring-shaped parasite with a dark-straining minute chromatin dot. o Bartonellosis Organism adheres to RBCs and are gram-negative rods (acute phase) and as cocci in recovery phase o Clostridium perfringens Refer to PowerPoint, will provide a better answer soon. |
|
|
Cells that occur as a result of a decreased oxygen environment are:
|
Reticulocytes
• Anemic - A reduction in the hemoglobin of red blood cells with consequent deficiency of oxygen in the blood, leading to weakness and pallor. (Actual answer I believe) • Hypoxic – Sudden change in attitude (High to low, mountain to sea levels, reversed scenarios as well). Examples include Altitude sickness, Chronic Mountain Sickness, Polycythemia, Polycythemia Vera. • Proliferated – Stimulated by EPO in respond to the body’s need for new RBCs leading to increased erythropoiesis. |
|
|
The morphologic difference between acanthocytes and burr cell is evident in the:
a. b. |
a.Echinocyte
NL Size NL MCHC Oval shape Even projections b.Acanthocyte Small Size Increase MCHC Spheroid Uneven spicules |
|
|
An aid for dealing with RBC agglutination in a laboratory specimen is to:
|
Heat up the specimen to body temperature
|
|
|
An aid for dealing with rouleaux in a laboratory specimen is to:
|
Change the plasma for saline to get rid of the rouleaux
|
|
|
A stain used to confirm the presence of precipitated iron in the RBCs is:
|
Prussian Blue- Siderotic Granules
|
|
|
A patient with lead intoxication typically has numerous RBCs with:
|
Basophilic Stippling
|
|
|
Cells that have decreased tolerance to swelling and are less deformable than normal are:
|
Spherocytes
|
|
|
The RBC with a slit like central pallor is called a
|
stomatocyte
|
|
|
Heinz bodies are:
|
Hgb
|
|
|
Heinz bodies can be seen only with which stain
|
Crystal violet
|
|
|
Disorders involving any component of hemoglobin synthesis usually result in RBCs that are:
|
normocytic, normochromic. There is microcytosis and hypochromia in some variants (HbE).Abnormal red cell morphology may or may not be seen in the blood smear and reticulocytes often are elevated.
|
|
|
In the body, iron primarily acts as a(n):
|
of oxygen and carbon dioxide and their transport to and from tissues of the body.
|
|
|
The majority of iron in the body is found in the:
|
the hemoglobin iron (2/3), rest is found as tissue iron.
|
|
|
Eating food high in vitamin C along with iron-rich foods will cause iron absorption to be:
|
Enhanced.
|
|
|
Pappenheimer bodies are also known as:
|
Iron-containing or siderotic granules.
|
|
|
The most common cause of iron deficiency in America women of childbearing years is:
|
Menstrual bleeding.
|
|
|
The most common cause of iron deficiency in adult men is:
|
GI bleeding.
|
|
|
During treatment for iron deficiency anemia, recovery is fist seen in peripheral blood as:
|
Sudden increase of RDW
|
|
|
The clinical manifestation that distinguishes pernicious anemia from folic acid deficiency is:
|
Neuropathies in pernicious anemia.
Although neuropathy is mainly characteristic of vitamin B12 deficiency, several cases of neurologic abnormalities associated with folic acid deficiency have been reported. |
|
|
When the maturation rates of nuclear and cytoplasmic development of hematopoietic cells differ, it is called:
|
Nuclear-cytoplasmic asynchrony
|
|
|
In megaloblastic anemias, the M:E ratio of the bone marrow is often:
|
Low – May be as low as 1:1 to 1:3
|
|
|
A major cause of non-megaloblastic macrocytosis is:
|
Alcoholism and chronic liver disease
|
|
|
A chemistry test that is often elevated in patients with megaloblastic anemia is:
|
Type of Megaloblastic Anemia-Chemistry Test
B12 Deficiency-Elevated Homocysteine and Methylmalonic Acid (MMA) Folate Deficiency-Elevated Homocysteine Pernicious Anemia-Elevated Homocysteine and Methylmalonic Acid (MMA) |
|
|
Following correct diagnosis and treatment of a megaloblastic anemia, the patient’s complete blood count (CBC) returns to normal in approximately:
|
3 to 6 weeks based on severity of the disease
|
|
|
Aplastic anemia manisfets as a decreased production of:
|
Erythrocytes, leukocytes, and platelets.
Characterized by cellular depletion in hematopoietic precursors with fatty replacement of the bone marrow |
|
|
One of the more common causes of aplastic anemia is:
|
Idiopathic
|
|
|
A drug that frequently causes aplastic anemia is:
|
Chloramphenicol or phenylbutazone (benzene)
|
|
|
An infectious state that is occasionally associated with bone marrow suppression is:
|
Hepatitis
|
|
|
Clinical manifestations of aplastic anemia are the result of:
|
Insidious process owing to the gradual decrease in bone marrow production of all cells (erythrocytes, leukocytes, and platelets)
|
|
|
Peripheral blood cell morphology in aplastic anemia is most often:
|
Normochromic, normocytic anemia with little or no evidence of regeneration such as polychromatophillic cells, basophilic stippling, or nucleated red cells seen.
|
|
|
The reticulocyte count of a patient with aplastic anemia is usually:
|
Decreased (pancytopenia)
A reticulocyte percentage of 0.5 percent to zero is strongly indicative of aplastic anemia, reflecting the lack of bone marrow regenerative activity |
|
|
In aplastic anemia, an abnormality that may be noted in the WBC differential is:
|
A WBC differential usually shows a relative lymphocytosis of 70 – 90%, reflecting decreased numbers of myeloid and monocytic cells.
• Total leukocyte count ≤ 1.5 x 109/L • Leads to pancytopenia |
|
|
In aplastic anemia, a bone marrow biopsy commonly reveals a marrow that is:
|
Hypocellular in nature. Most of the blood stem cells are gone and replaced by fat (yellow marrow).
|
|
|
In left untreated, most patients with aplastic anemia will:
|
Patients will undergo progressive decreases in blood counts and subsequent lethal infection or bleeding.
|
|
|
For children and young adults with severe aplastic anemia, the preferred treatment is:
|
Allogeneic bone marrow marrow or peripheral stem transplantation.
|
|
|
Anemia of chronic disease (inflammation) is usually:
|
Normocytic, Normochromic- but as the condition progresses, it becomes hypochromic and microcytic. (This is all I could find, I’m not sure what the choices may be)
|
|
|
Anemia of chronic disease (inflammation) may be confused initially with iron deficiency anemia because both disorder exhibit
|
Low serum iron levels
|
|
|
In inflammation, the erythrocyte sedimentation rate is often:
|
Increased, due to c-reactive proteins increase
|
|
|
The primary cause of anemia of chronic renal disease is:
|
Deficiency of erythropoietin by damage to the kidneys leading to decrease of erythrocytes.
|
|
|
When RBCs from a healthy donor are transfused into a patient with an extracoupuscular RBC defect, the life span of the donor cells will be:
|
Destroyed
|
|
|
Hemoglobinenia, hemoglobinuria, and hemosiderinuria are good indicators of:
|
Chronic intravascular hemolysis
|
|
|
Cells that have a decreased osmotic fragility and are less deformable than normal are:
|
Xerocytosis
|
|
|
Hereditary spherocytosis is considered a disorder of the:
|
Membrane, due to deficiency in spectrin
|
|
|
A common treatment for hereditary spherocytosis is:
|
Splenectomy is funtionally curative in the majority of patients with this disease
|
|
|
The osmotic fragility in most patients with hereditary elliptocytosis is:
|
Normal
|
|
|
The disorder in which RBCs exhibit thermal instability in hereditary;
|
Hereditary pyropoikilicytosis leads to thermal instability and extreme morphologic abnormalities
|
|
|
The most commonly encountered anemia is the congenital non-spherocytic hemolytic anemia is caused by a deficiency of:
|
G6PD, PK, enzyme deficiency in the ebden myerhof pathway
|
|
|
G6PD is found in the:
|
X chromosome (Xq28)
|
|
|
The hemolytic episodes in G6PD deficient patients are self-limiting because:
|
RBCs fail to maintain adequate levels of GSH
|
|
|
An osmotic fragility performed on fresh blood from a patient with PK deficiency will be:
|
Osmotic fragility test is normal
|
|
|
Favism may be associated with:
|
G6PD deficiency
|
|
|
PNH is a disorder that is:
|
-Acquired hemolytic anemia associated with cellular membrane abnormalities
-Lack of GPI-anchored proteins on the erythrocyte membrane |
|
|
The classic presentation of a patient with PNH includes:
|
The classic description of the manifestations of PNH is the presence of dark urine during the night with partial clearing during the day; however, hemoglobinuria may occur every day in severe cases, more frequently in episodes lasting 3-10 days, or, in some cases, not at all. Thrombosis of the veins usually manifests as a sudden catastrophic complication, with severe abdominal pain and rapidly enlarging liver and ascites (Budd-Chiari syndrome). This thrombosis is secondary to a lack of CD59 on platelet membranes that induces platelet aggregation and is highly thrombogenic, particularly in the venous system. Deficient hematopoiesis may occur due to diminished blood cell production with a hypoplastic bone marrow; thus, patients have a 10-20% chance of developing aplastic anemia in their course, and patients known to have aplastic anemia eventually develop PNH in 5% of cases. The nature of the pathogenetic link between these two diseases still is unknown.
|
|
|
A disorder that may be confused with PNH because both produce positive acidified serum lysis (Ham’s) result is:
|
CDA
|
|
|
Polychromasia may be seen on the Wright’s stained smear of a patient with PNH due to an elevation of:
|
Reticulocytes
|
|
|
The RBC enzyme whose level corresponds to the acuity of PNH is:
|
phosphatidylinositol glycan A (PIGA)
|
|
|
A screening test for PNH is the:
|
sugar water test (sucrose hemolysis)
|
|
|
The confirmatory test for PNH is the:
|
Hams test (acidified serum lysis test)
|
|
|
Fresh normal serum is required for the acidified serum lysis (Ham’s) test to ensure the presence of:
|
Hemolysis
|
|
|
A valuable test for evaluating suspected hemogobinopathies is:
|
CBC with manual morphology
|
|
|
Hemoglobinopathy may be defined as:
|
Group of diseases caused by or associated with the presence of one or several forms of abnormal hemoglobins in the blood
|
|
|
The hemoglobin of sickle cell disease may be designated as:
|
-The abnormal form of hemoglobin that creates sickle cell disease is Hemoglobin S. It is formed by a genetic mutation in which one amino acid replaces another (valine replaces glutamic acid)
|
|
|
When the bone marrow temporarily ceases to produce cells in a sickle cell patient, a (n) _________ crisis has occurred.
|
-Aplastic
|
|
|
The most severe anemia results from which of the following hemoglobinopahies?
|
-Both Alpha Thalassemia major (this autosomal recessive trait results in fetal death) and Beta Thalassemia major (Cooley’s anemia)
|
|
|
The presence of HbF causes the severity of sickling in sickle cell disease to:
|
Decrease
|
|
|
Hemoglobins that denature and precipitate within RBCs as Heinz bodies are:
|
-Intracellular inclusions called Hemoglobin Köln and Hemoglobin Zurich.
|
|
|
The majority of hemoglobinopathies are caused by?
|
-The majority of hemoglobinopathies result from B chain abnormalities. Although they may arise from a single amino acid substitution.
|
|
|
Alpha-thalassemia is usually manisfested:
|
Fatigue, Weakness, Shortness of breath, Pale appearance, Irritability, Yellow discoloration of skin (jaundice), Facial bone deformities, Slow growth, Abdominal swelling, Dark urine
|
|
|
Alpha- thalassemia are characterizes by increases in hemoglobins:
|
Decreased or absent alpha chain production will result in excess gamma chains during fetal life and at birth and in excess of beta chains later on. This causes formation of stable tetramers such as:
• Hgb H & Hemoglobin Barts |
|
|
After incubation with brilliant cresyl blue, RBCs containing hemoglobin H will:
|
• Hemoglobin H Inclusions - alpha thalassemia, greenish-blue inclusion bodies appear in many erythrocytes after four drops of blood is incubated with 0.5mL of Brilliant cresyl blue for 20 minutes at 37°C.
|
|
|
The characteristic that allows hemoglobin F to be studied is its:
|
• Fetal Hemoglobin is more resistant than adult hemoglobin to elution at acid pH and can be demonstrated on a peripheral smear by the acid elution test Klehauer and Betke.( Im not sure about this answer I couldn’t find better info than this, please let me know if you guys find anything more accurate than this answer)
|
|
|
The thalassemia syndromes are morphologically described as:
|
• Microcytic, Hypochromic
|
|
|
In general, thalassemias are characterized by a (n):
|
• decreased rate of globin synthesis
|
|
|
The Kleihauer-Betke acid elution test demonstrates hemoglobin:
|
the most appropriate screening test for detecting hemoglobin F.
|
|
|
A2 2%, F Even, Sickle solubility Negative
|
B-thalassemia
|
|
|
A2 1%, F Negative, Sickle solubility Positive
|
Sickle cell trait
|
|
|
A2 1.5%, F Negative, Sickle solubility Negative
|
Normal
|
|
|
A positive direct antiglobulin test is one indication of:
|
C. Acquired hemolytic anemia (positive DAT)
|
|
|
A delayed hemolytic transfusion reaction occurs within_______ post transfusion.
|
3-7 days
|
|
|
The system most commonly associated with immediate hemolytic transfusion reaction is:
|
ABO
|
|
|
The fetomaternal incompatibility most commonly associated with HDN is:
|
fetomaternal alloimmune thromocytopenia
|
|
|
In hemolytic disease of the newborn, if intervention therapy is necessary and the fetus is too premature for delivery, the therapy of choice is:
|
if delivery is planned prior to 34 weeks' gestation, maternal steroid administration to enhance fetal lung maturity is indicated.
|
|
|
The specificity of the antibody most commonly found in warm autoimmune hemolytic anemia is:
|
IgG
|
|
|
The antibody screen of a patient with warm autoimmune hemolytic anemia (AIHA) will reveal positive results only in the phase associated with:
Hemolytic Transfusion Reaction: acute and delayed |
• Hemolytic Disease of the Newborn
• Lab results: IgG antibody increase Bili decrease Haptoglobin DAT + |
|
|
Cold antibodies are usually:
|
IgM
so they do NOT cross the placenta and do NOT cause HDFN; can be non-red cell stimulated; usually only clinically significant if it fixes complement or causes hemolysis; reacts optimally at 4C but can and frequently does react at room temperature. |
|
|
The most common antibody specificity in cold AIHA is:
|
IgM/ Anti-I, Anti-H, Anti-IH specificity
|
|
|
The antibody specificity is paroxysmal cold hemoglobinuria is:
|
IgG antibody, Anti-P specificity
|
|
|
The Donath-Landsteiner antibody is associated with:
|
Paroxysmal cold hemoglobinuria
|
|
|
The most common protozoal infestation that results in anemia is:
|
Malaria
|
|
|
A common finding in the peripheral blood of patients with intravascular hemolysis due to mechanical trauma is:
|
schistocytes and other poikilocytes
|
|
|
Which of the following factors will result in an immediate increase in oxygen delivery to the tissue?
|
Hypoxia
|
|
|
The fish tapeworm Diphyllobothrium latum is associated with the development of
|
vitamin B12 deficiency, pernicious anemia
|
|
|
A moderately anemic patient with suspected pernicious anemia (PA) shows intrinsic factor antibodies and a low cobalamin level. Which of the following would NOT support the diagnosis of PA?
|
decrease serum B12 and the presence of the ab to IF are indicative of pernicious anemia
|
|
|
The major mechanism responsible for the anemia of chronic disease is
|
chronic states block the transfer of storage iron to maturing erythroid precursors within the bone marrow
|
|
|
A “shift to the left”, when used to describe a cell population, refers to
|
Increase in immature blood cells following release of bone marrow pools
|
|
|
In children, the most important effect of lead poisoning is on the
|
Neurologic system
|
|
|
Which of the following values can be used to indicate the presence of a hemolytic anemia?
|
Reticulocyte count
|
|
|
Which of the following does NOT characterize beta-thalassemia major?
|
Decreased alpha chains result in excess beta chains
|
|
|
A patient with normocytic normochromic anemia secondary to small cell carcinoma may be exhibiting an anemia designated as
|
Myelophthisic (Anemia in which there is bone marrow failure. Seen in patients who are experiencing bone marrow replacement of normal hematopoietic tissue by metastatic cancer, cell fibrosis or leukemia.
|
|
|
Which of the following is a true red blood cell aplasia?
|
Diamond-Blackfan anemia
|
|
|
The classic presentation of a patient with PNH includes:
|
Hepatomegaly and ascites in Budd-Chiari syndrome
Splenomegaly if there is splenic vein thrombosis Absent bowel sounds in bowel necrosis Papilledema in cerebral vein thrombosis Skin nodules that are red and painful in dermal vein thrombosis |
|
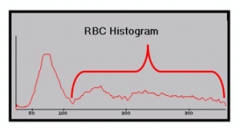
The RBC histogram below is indicative of:
|
Agglutination
|
|
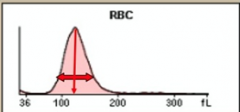
The RBC histogram below is indicative of:
|
Macrocytic, Elevated RDW
|
|
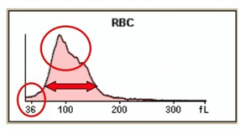
The RBC histogram below is indicative of:
|
RBC fragments, Elevated RDW
|
|
The RBC histogram below is indicative of:
|
Dimorphic population, Elevated RDW
|
|
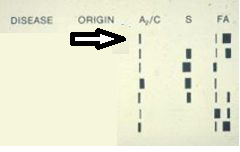
Interpret the electrophoresis the arrow is pointing at
|
Normal
|
|
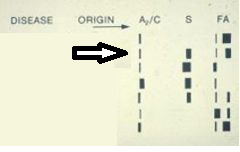
Interpret the electrophoresis the arrow is pointing at
|
Sickle Cell Trait
|
|
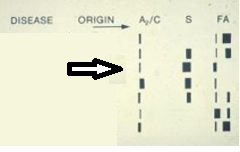
Interpret the electrophoresis the arrow is pointing at
|
Sickle Cell Disease
|
|
Interpret the electrophoresis the arrow is pointing at
|
Sickle C
|
|
Interpret the electrophoresis the arrow is pointing at
|
Sickle -Thalassemia
|
|
Interpret the electrophoresis the arrow is pointing at
|
Thalasemia Major
|
|
Interpret the electrophoresis the arrow is pointing at
|
Thalassemia Minor
|
|

Refer to the following scatterplot, histograms and automated values on a 52-year old woman. What follow up verification procedure is indicated before releasing these results?
|
Warm up at 37 for 15 min
Falsely Elevated MCV, MCH, MCHC Falsely Decreased RBC count |

