![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
43 Cards in this Set
- Front
- Back
|
best indicator of hemolytic anemia is...
|
high retic count
|
|
|
when does hemolytic anemia occur?
|
when RBC survival is shortened to <30 days (nl= 120 days)
|
|
|
what happens when your direct bilirubin is low and you mostly have elevated indirect/unconjugated bilirubin?
|
If direct bilirubin is low and mostly indirect/unconjugated bilirubin, then you can deduce that you have hemolytic anemia. This unconjugated bilirubin will not be excreted and you’ll have jaundice and icteric sclera (yellow eye). You’ll have only have icteric sclera without yellow pee (it’ll be clear instead).
|
|
|
name some causes of indirect (unconjugated) hyperbilirubinemia
|
-hemolytic anemia
-ineffective erythropoiesis -resorption of hematomas -liver dz (bc damaged hepatocytes can't conjugate bilirubin anymore) |
|
|
name some causes of direct (conjugated) hyperbilirubinemia
|
-biliary obstruction/stasis
- hepatocellular dz |
|
|
what is the key question in differential dx of bilirubinemia?
|
is the direct or indirect elevated? this will tell you what the etiology of the problem may be.
for example, hemolysis causes INDIRECT hyperbilirubinemia, while hepatocellular dz causes DIRECT hyperbilirubinemia |
|
|
tell me about the difference b/w intrinsic (intracorpuscular) vs. extrinsic (extracorpuscular) abnormaliites as a form of classifying hemolytic anemias
|
intrinsic = usually hereditary (except for PNH, which is acquired intrinsic abnormality), where defect causing HA is in the RBCs themselves (transfused red cells typically have nl life span)
extrinsic = acquired, where RBCs are being destroyed by something outside of themselves (transfused RBCs even have shortened life span bc there's something in the blood or vascular environment that's causing destruction) |
|
|
tell me about the difference b/w intravascular vs extravascular classification of hemolytic anemias
|
intra: rbcs perish in blood stream
extra: rbcs perish in the reticuloendothelial system (lymph nodes/spleen) |
|
|
RBCs leaving bone marrow stain as reticulocytes for about __ hours. normal retic count is about __%.
|
24; 1
|
|
|
what would you expect for the routine lab tests for a pt with hemolysis?
|
CBC, especially hgb/hct (down)
Including smear review! Reticulocyte count (↑) Indirect bilirubin (↑) |
|
|
What would these lab results indicate?
-LDH (↑) -Haptoglobin (dec) -Plasma hemoglobin -Urine hemoglobin and hemosiderin (iron in tubular cells shed into the urine) |
tests show intravascular hemolysis
haptoglobin=a protein in plasma that binds free hemoglobin and removes it |
|
|
name 3 congenital causes of hemolytic anemia (and give examples!)
|
1. membrane abnormalities (hereditary spherocytosis/elliptocytosis)
2. enzyme defects (G6PD deficiency) 3. Hb defects (sickle cell, thalassemias) |
|
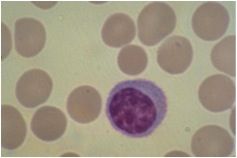
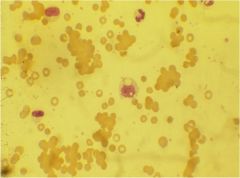
what is this?
|
hereditary spherocytosis
|
|
|
name the acquired causes of hemolytic anemia
|
1) Immunologic
Warm antibody, cold agglutinin, allo-immune 2) Fragmentation -TTP, HUS, DIC, valve hemolysis 3) Infections -Malaria, Clostridia, Babesiosis 4) Metabolic/osmotic/chemical or physical agents -Hypophosphatemia, Wilson’s disease, fresh water near drowning, burns 5) Membrane abnormalities - Paroxysmal nocturnal hemoglobinuria, spur cell anemia 6) Hypersplenism |
|
|
most common cause of ACUTE intravascular hemolytic anemia
|
ABO incompatible transfusion (someone gets wrong blood during transfusion and Ab's kill transfused blood cells)
|
|
|
what are some other causes of acute intravascular hemolysis?
what are the sx's? |
clostridial sepsis; PNH crisis
sx's: chills/fever, dark or red urine, back and/or abdominal pain |
|
|
how can parvovirus complicate chronic hemolytic anemias?
|
cause aplastic crisis
|
|
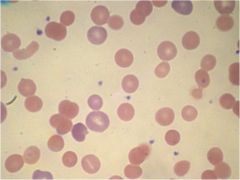
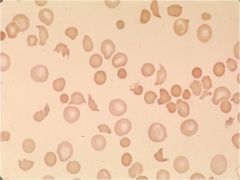
what is shown here?
|
microspherocytes where rbcs have no central pallor. normally 1/3 of diameter should have central pallor -- these cells have become spherical. don't know if this is hereditary or acquired problem.
|
|
what is shown here?
|
microspherocytes where rbcs have no central pallor. normally 1/3 of diameter should have central pallor -- these cells have become spherical. don't know if this is hereditary or acquired problem.
|
|
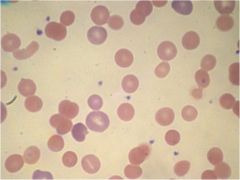
what is shown here?
|
microspherocytes as well as spherocytes. bigger ones are reticulocytes.
|
|
|
pathophysiology of AIHA (IgG). why is it called warm antibody hemolytic anemia
|
pt produces Ab's to self RBCs. Ab's damage rbcs and these rbcs are removed by macrophages (particualrly in the spleen).
Ab shows max reactivity with rbcs at 37 degrees (body temp). |
|
|
differentiate b/w direct and indirect coomb's tests
|
- direct Coombs test is used to detect these antibodies or complement proteins that are bound to the surface of red blood cells; a blood sample is taken and the RBCs are washed (removing the patient's own plasma) and then incubated with antihuman globulin (also known as "Coombs reagent"). If this produces agglutination of RBCs, the direct Coombs test is positive, a visual indication that antibodies (and/or complement proteins) are bound to the surface of red blood cells. ==> shows that there is presence of auto-antibodies on rbcs themselves!!
The indirect Coombs test is used in prenatal testing of pregnant women, and in testing blood prior to a blood transfusion. It detects antibodies against RBCs that are present unbound in the patient's serum. In this case, serum is extracted from the blood, and the serum is incubated with RBCs of known antigenicity. If agglutination occurs, the indirect Coombs test is positive. ==> detects presence of Ab's in serum |
|
|
pt has pos DAT and pos IgG, pos C3
|
warm autoimmune hemolytic anemia (IgG) aka. AIHA
|
|
|
pt has pos DAT, neg IgG, pos C3
|
cold agglutinin dz (IgM)
|
|
|
pt has pos IAT, neg DAT
|
caused by prior transfusion
|
|
|
causes of AIHA
|
- idiopathic (unknown cause) in 1/3; in children often triggered by viral infeciton
- lymphoproliferative disoders (CLL, lymphomas) - systemic lupus erythematosus (or other autoimmune dz) |
|
|
tx of warm-Ab AIHA
|
corticosteroids, splenectomy, immunosuppression, transfusion (with caution)
|
|
what is shown here? what's the pathophysiology?
|
cold agglutin dz (IgM)
- IgM antibodies that are maximally active in colder parts of body are directed towards self-rbcs. IgM avidly fixes complement for rbc destruction. hemolysis is both intravscular (c9 fixation - MAC complex) and extravsasulr (c3 promotes phagocytosis) |
|
|
what are the signs/sx's of cold agglutinin HA?
|
anemia, ischemia of fingers, earlobes
|
|
|
causes of cold agglutinin dz
|
- idiopathic
- infections (mycoplasma pneumonia, etc) - systemic lupus - lymphoproliferative disorders |
|
|
tx of cold agglutinin dz
|
-infectious: keep warm, gloves, earmuffs
-NOT corticosteroids/splenectomy - immunomodulatory drugs - rbc transfusions |
|
|
define: red cell fragmentation syndromes
|
hemolytic anemias where hemolysis is caused by physical forces on flowing blood.
|
|
|
should you treat cold agglutinin dz with corticosteroids and splenectomy?
|
no
|
|
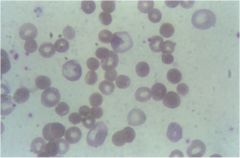
what is shown here?
|
Fragmentation syndromes – smear shows fragmented red cells; presence of spherocytes, but mostly see bizarre, triangular shaped cells. Notice there are no platelets here.
|
|
|
define: microangiopathic hemolytic anemias
|
these are disorders of small blood vessels (via fibrin depositions) that induce red cell fragmentation (schistocytes). ie. TTP and HUS.
|
|
|
tell me the big differences between TTP and HUS
|
TTP affects adults more than children, more likely to present with cns symptoms, fever.
HUS occurs mainly in children!! less likely to have cns symptoms, more likely to have renal problems! lose a lot more platelets (even though both have thrombocytopenia) |
|
|
pathophys of TTP
|
acquired cases: antibody to ADAMTS13, which allows unusually large vWF to circulate in plasma --> leads to platelet clots, microvascular occlusion
Red blood cells passing the microscopic clots are subjected to shear stress which damages their membranes, leading to intravascular hemolysis and schistocyte formation. Reduced blood flow due to thrombosis and cellular injury results in end organ damage. |
|
|
what is the proper tx of TTP?
|
plasma exchange (for acquired TTP)
PLATELET TRANSFUSIONS ARE CONTRAINDICATED!!!!! |
|
|
pathophys of PNH (paroxysmal nocturnal hemoglobinuria)
|
-mutation in PIG-A gene which impairs ability to form membrane bridges
there are 20 proteins hanging on the surface of the RBC hanging with inositol bridge. Without this bridge, these proteins won’t be there. 2 of those proteins inhibit complement (CD 55 and CD 59). Therefore, complement will kill RBCs abnormally. And you get intravascular hemolysis. |
|
|
dx and tx of PNH
|
dx: flow cytometry
tx: Eculizumab, a monoclonal Ab that binds C5 component of complement to inhibit complement activation (results in less hemolysis) |
|
|
features of hypersplenism
|
-splenomegaly
-reduction in one or more of the blood cell lines leading to anemia, leukopenia, thrombocytopenia, or combination of these -no morpholgical changes of blood cells on smear |
|
|
what can correct blood cytopenia(s)?
|
splenectomy
|
|
|
causes of hypersplenism
|
- portal hypertension
- infectious dz (mono, CMV) - infiltrative dz of spleen (Gaucher's) - neoplastic dz (leukemias, lymphomas) - hemoglobinopathies (SCD, thalassemia) |

