![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
141 Cards in this Set
- Front
- Back
|
Xanthelasma
|

-Slightly raised irregular flat yellow lesions
-Secondary to abnormality in lipid metabolism -Localizes to upper/lower eyelids and around canthus |
|
|
Periorbital edema
|

-Swelling around eye
-Always abnormal -Causes include: allergic rxns, thyroid disease, mono, conjunctivitis, renal disease, insect bites, trauma, cellulitis |
|
|
Preseptal cellulitis (periorbiral cellulitis)
|

-Infection of anterior soft tissues of eye
-Usually staph or strep -No fever or leukocytosis -No restriction in eye motility -No pupillary defect -Tx w/ oral antibiotics |
|
|
Orbital cellulitis
|

-Infection of deep soft tissues of eye
-Usually staph or strep -Fever, leukocytosis, proptosis -Dec EOM -Afferent pupillary defect -Tx w/ admission and IV antibiotics |
|
|
Orbital ecchymosis
|

-AKA raccoon eyes
-Periorbital edema -Indicates basilar skull fracture from trauma -If no trauma has occurred, suspect bleeding disorder |
|
|
Fracture of orbit
|

-Direct blow to eye
-Impaired ocular movement due to inferior rectus entrapment -Periorbital edema, diplopia, epistaxis |
|
|
Proptosis
|

-Fwd displacement of globe that implies orbital soft tissues are distended by inflammation or tumor
-In peds, rapid onset may indicate rhabdomyosarcoma |
|
|
Exophthalmos
|

-Represents a bilateral protrusion of eyeballs
-Think hyperthyroid |
|
|
Eyebrow irregularities
|
-Scaling and redness = seborrheic dermatitis
-Loss = chemo, plucking, burns, alopecia -Coarse or do NOT extend past temporal canthus = hypothyroid |
|
|
Rosenback sign
|
-Tremors of lids
-Suspect hyperthyroidism |
|
|
Lid lag (Von Graefe sign)
|
-Strip of sclera above upper lid visible during superior/inferior eye tracking
-Indicates spasm and/or hyperthyroidism |
|
|
Blepharitis
|

-Present: red eyes
-Chronic irritation of lids and lashes -Telangectatic lid margins w/ greasy flakes on lashes -Irritation, blurring, itching -Causes include inflammatory, infectious, autoimmune -Tx w/ antibiotic eye ointment, eyelid scrubs, warm compresses |
|
|
Ptosis
|
-When superior eyelid covers more of iris than other or extends over pupil in primary gaze
-Can be congenital or acquired -Weakness of levator muscle or palsy of CN III -Other causes: MG, trauma, edema of lids, old age, DM |
|
|
Ectropion
|

-Present when lower lid is turned away from eye
-May result in excessive tearing -Causes: congenital, scarring, surgery, trauma, aging, Bell's palsy |
|
|
Entropion
|

-Present when lid is turned inward toward the globe
-More threatening to sight -May cause corneal and conjunctival irritation |
|
|
Acute hordeolum of upper eyelid
|

-AKA sty
-Caused by inflamed meibomian gland resulting in pustule -Position is ON lash margin -PAINFUL, red -Tx w/ warm packs, antibiotic eye ointment |
|
|
Chalazion
|

-Chronic cyst of a sebaceous gland
-Localized swelling or protrusion ABOVE lid margin -NONTENDER and enlarges slowly -Tx w/ hot packs and massage |
|
|
Dacryocystitis
|

-Infection of lacrimal sac usually due to congenital or acquired obstruction of nasolacrimal system
-Due to staph aureus or hemolytic strep in acute and S epidermdis, anaerobic strep, or Candida albicans in chronic -Pain, swelling, redness in tear sac area w/ possible purulence -Tx w/ antibiotics or surgery |
|
|
Allergic conjunctivitis
|

-Non painful eye irritation that does NOT affect vision or pupils
-Bilateral, pruritic, cobblestone appearance w/ clear d/c as well as chemosis or edema of conjunctiva |
|
|
Subconjuctival hemorrhage
|

-Present: red eye, no pain
-Caused by straining, mild trauma, bleeding disorder -Painless -No tx needed |
|
|
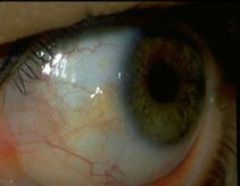
Pterygium
|

-Benign fleshy, triangular encroachment of bulbar conjunctiva OVER cornea at 3 or 9 o'clock
-Usually bilateral and caused by excessive wind, sun and dust exposure -Irritation, redness, tearing -Tx w/ eye lubricants, steriods, possibly surgery |
|
|
Pinguecula
|
-Benign raised yellow/white lipid deposit on bulbar conjunctiva extending TO cornea at 3 and 9 o'clock
-Thought to be due to sun, dirt and dryness over long period of time -No tx required |
|
|
Scleral icterus
|
-May be apparent when sclera is yellow
-Usually indicates liver disease |
|
|
Episcleritis
|

-Localized inflammation of episcleral vessels
-Self limiting and idiopathic; little discomfort -In some cases associated w/ collagen vascular disease |
|
|
Scleritis
|

-Markedly dilated vessels that do not extend onto underside of lower lid
-May appear purplish w/ deep pain and photophobia that can threaten vision -Often in women w/ associated connective tissue disease |
|
|
Miosis
|
-Pupillary constriction to less than 2mm
-Pupil fails to dilate in dark |
|
|
Mydriasis
|
-Pupillary dilation of more than 6 mm
-Pupil fails to constrict w/ light -Associated w/ state of coma |
|
|
Anisocoria
|

-Inequality between diameters of pupils
-Up to 1 mm difference is ok -Can be normal variant from drops, iritis, 3rd nerve palsy, glaucoma, intracranial mass, artificial eye, etc |
|
|
Ciliary flush (injection)
|

-Indicated inflammation of iris and ciliary body
-Produces pink band surrounding corneal limbus -NOT seen in conjunctivitis -Commonly seen in acute glaucoma, iritis |
|
|
Acute narrow angle glaucoma
|
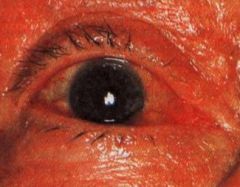
-Present: red, painful eye, dec vision, N/V
-Acute increase in IOP -Severe, aching deep pain -Dec vision -Dilated, fixed pupil -Steamy, cloudy cornea -Widespread injection -Tx w/ IV acetazolamide |
|
|
Acute iritis or anterior uveitis
|

-Mod, aching deep pain from iris spasms
-Dec vision and photophobia -Small, irregular pupil -Cornea clear or slightly clouded -Injection confined to corneal limbus -Sarcoidosis, RA, Reiters, ankylosing spondyltis |
|
|
Arcus senilis
|
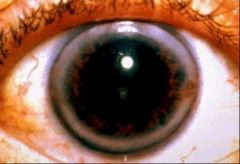
-Hazy ring at edge of cornea where meets iris
-Composed of lipids deposited in periphery of cornea -Common after 60, lipid disorder before 40 |
|
|
Corneal abrasion
|

-May be secondary to infection, contacts, UV light, drugs, or blepharitis
-PAIN, photophobia, FB sensation, lacrimation, injection, possible dec vision -Dx w/ fluorescein staining -Tx / antibiotics (controversial), artificial tears |
|
|
Corneal ulcer
|
-Red eye w/ predominantly circumcorneal injection
-May be purulent or watery d/c -Pain, photophobia, tearing, reduced vision -Tx w/ antibiotic eye drops, steroids if NOT bacterial |
|
|
Herpes keratosis
|
-Viral infection of eye caused by herpes simplex virus
-Dendritic (branching) ulcer most characteristic manifestation -Tx w/ debridement, patch, topic antivirals |
|
|
Herpes zoster ophthalmicus
|

-Occurs when varicella-zoster virus reactivated in ophthalmic division of trigeminal nerve
-Malaise, fever, HA and periorbital burning and itching -Tip of nose involvement predicts involvement of eye -Tx w/ high dose acyclovir, valcyclovir w/in 72 hrs of appearance |
|
|
Kayser-Fleischer ring
|
-Circular band of brown pigment near limbus
-Associated w/ Wilson's disease, a disorder of copper metabolism |
|
|
Hyphema
|

-Layer of BLOOD visible in anterior chamber
-Caused by blunt trauma -Refer immediately |
|
|
Hypopyon
|

-PUS in anterior chamber
-May accompany corneal ulcer -Refer immediately |
|
|
Astigmatism
|
-Type of refractive error of eye
-Front surface of cornea is curved more in one direction than other causing blurred vision -Corrected by toric lens |
|
|
Cataracts
|

-Gradually progressive blurred vision
-Clear lens becomes thicker, yellow and cloudy -May see slight haze or blur over visual field w/ glare, halo or starburst -Risks include aging, DM, HTN, sun, smokers, steroids -Tx w/ removal using ultrasound device |
|
|
Strabismus
|

-Disorder in which eyes do not line up in same direction when focusing
-Involves lack of coordination between extraocular muscles -Prevents bringing gaze of each eye to same point in space which affects binocular vision and depth perception |
|
|
Esotropia
|
-Excessively convergent or medially deviated
-Most common type -Tx w/ glasses, amblyopia tx, and sometimes surgery |
|
|
Exotropia
|
-Excessively divergent or lateral deviation
-Tx w/ surgery, patch, glasses |
|
|
Amblyopia
|
-Unilateral or bilateral impairment in visual acuity
-Affected during development and uncorrected by optics -Leads to damage in visual pathway and visual loss -Leading cause of monocular vision loss in people between 20-70 -Tx w/ patch |
|
|
Presbyopia
|
-Farsightedness (impaired near vision)
-Defect in advancing years involving loss of accomodatio or recession of near point -Due to loss of elasticity of lens |
|
|
Myopia
|
-Nearsightedness (impaired far vision)
-Defect in vision in which parallel rays come to focus in front of retina -Objects can only be seen distinctly when very close to eyes |
|
|
Refractive error
|
-One corrected by glasses/lenses
|
|
|
Extraocular movements
|
-Controlled by integrated functions of CN III (oculomotor), IV (trochlear), VI (abducens)
-LR6SO4 |
|
|
Nystagmus
|
-Fast, uncontrollable movements of eyes
-May be side to side, up and down, or rotary -Causes of acquired include MS, stroke, head trauma, Meniere's dz, labyrinthitis, brain tumor, drugs, etc |
|
|
Hemianopia
|
-Decreased vision or blindness in half the visual field of one or both eyes
-Damage can result from acquired brain injuries caused by stroke, tumor, or trauma -Occurs b/c of direct insult to eye via trauma or disease, damage to optic nerve, or damage to brain itself |
|
|
Bitemporal hemianopia
|
-Visual loss involving temporal half of both fields
-Defect at optic chiasm (pituitary tumor) |
|
|
Homonymous hemianopia
|
-Visual loss on same side of both eyes
-From tumor or stroke in occipital lobe |
|
|
Glaucoma
|

-Third leading cause of blindness
-Optic nerve damage due to increased IOP - Pathologic cupping of optic disc -Insidious progressive bilateral loss of peripheral vision, resulting in tunnel vision but preserved visual acuities -Tx w/ prostaglandin analogs, laser therapy and surgery |
|
|
Crescents
|
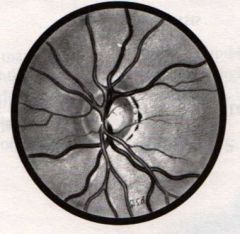
-Often seen around optic disc
-Normal developmental variations that appear as either white sclera, black retinal pigment, or both, especially along temporal border of disc -Not part of disc itself and should not be included in estimate of disc diameter |
|
|
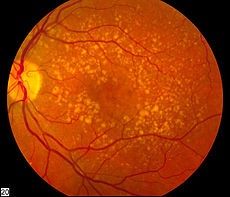
Retinal drusen
|

-Small, yellowish deposits that form w/in layers of retina
-Represents breakdown of photoreceptors -May concentrate at posterior pole between optic disc and macula -Increase in size or number raises risk of developing AMD |
|
|
Diabetic retinopathy
|
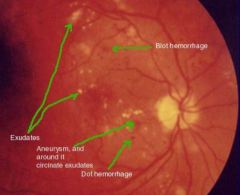
-Microaneurysms, hemorrhages, exudates, and edema of retina
-Types include background, maculopathy, proliferative -Tx w/ lasers to block development of new vessels and stop leaking vessels -Tight glucose control is best |
|
|
AV nicking
|

-Tapering of edges of vein as approaches artery
-Due to compression of vein at arteriovenous crossing -Think HTN!! |
|
|
Papilledema
|
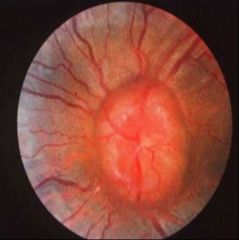
-Condition in which increased pressure in or around brain causes optic nerve to swell where enters eye
-Disc is swollen and margins blurred -Caused by brain tumor or abscess, head injury, bleeding in brain, severe HTN, infection of brain |
|
|
Cotton wool spots
|

-White or grayish, ovoid lesions w/ irregular "soft" borders
-Moderate in size but usually smaller than disc -Result from infarcted nerve fibers -Seen in HTN, DM, AIDS |
|
|
Hard exudates
|

-Creamy or yellowish, often bright, lesions w/ well-defined "hard" borders
-Small and round but may coalesce into larger irregular spots -Often occur in clusters or in circular, linear, or star-shaped patterns -Causes include DM and HTN |
|
|
Central retinal vein occlusion
|

-Caused by hardening of vessels
-Blood and thunder fundus |
|
|
Central retinal artery occlusion
|
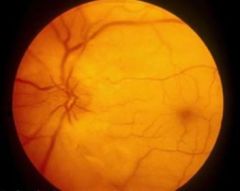
-Caused by embolisms
-Cherry red fovea |
|
|
Retinal detachment
|

-Separation of light-sensitive membrane in back of eye (retina) from supporting layers
-PAINLESS, sudden loss of vision -Flashing lights and new floaters may be sign of impending detachment |
|
|
Macular degeneration
|
-Leading cause of blindness over age 60
-Progressive disease of retina wherein light-sensing cells in central area of vision (macula) stop working and eventually die -Loss of detail vision, contrast sensitivity, relative/absolute scotoma -Two types: -Neovascular or "wet": more severe, some treatment -Atrophic or "dry": most common, no treatment -Tx w/ vitamins, drugs (AVEGF), surgery, rehab |
|
|
Viral conjunctivitis
|

-Present: red, itchy eye w/ FBS x 1 week
-Adenovirus is the most common cause - Bilateral infection with copious watery d/c often with marked FBS and a follicular conjunctivitis -There may be pharyngitis, fever, malaise, and preauricular adenopathy -May also be due to herpes simplex virus (HSV) – Usually unilateral infection – May be associated with lid vesicles, and enterovirus 70 or coxsackievirus A24 -Tx w/ artificial tears |
|
|
Bacterial (gonococcal) conjunctivitis
|

-Present: acute onset swollen eye, copious drainage
-Rapid onset of purulent drainage -Tx w/ antibiotics such as topical fluoroquinolone or IM Ancef and poazithromycin |
|
|
Traumatic iritis
|

-Present: eye pain, photophobia after bumping eye
-Ciliary flush, pupil asymmerty, pain, photophobia after trauma -Tx w/ topical corticosteroic |
|
|
Caput succedaneum
|
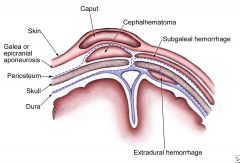
-Condition involving subcutaneous, extraperiosteal fluid collection w/ poorly defined margins
-Between scalp and periosteum -Caused by pressure of presenting part of scalp against dilating cervix during delivery |
|
|
Cephalohematoma
|
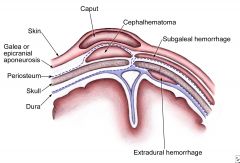
-Hemorrhage of blood between skull and periosteum of newborn
-Between periosteum and skull bones -Secondary to rupture of blood vessels crossing periosteum |
|
|
Acute otitis media
|

-Bacterial infection of the mucosally lined air-containing spaces of the temporal bone
-Usually precipitated by a viral URI that causes eustachian tube obstruction, resulting in accumulation of fluid and mucus, which become secondarily infected by bacteria -Bacteriology: S pneumo, H flu, M catarrhalis -Most commonly occurs 6 mths - 5 yrs -Sx include fever, otalgia, irritability, otorrhea, red/bulging TM, cervical adenopathy -Complications of TM perforation, mastoiditis, facial paralysis, hearing loss, impaired speech development -Tx w/ high dose Amoxicillin, Amoxicillin/Clavulanate |
|
|
Chronic otitis media
|

-Chronic infection of middle ear and mastoid as a consequence of recurrent acute otitis media
-Bacteriology: P aeruginosa, Proteus species, mixed anaerobes -Purulent d/c with or without otalgia -TM perforation with conductive hearing loss -Tx w/ debridement and topical antibiotic drops |
|
|
Recurrent acute OME
|
-Repeted episodes of AOME w/ disease free intervals
-Tx w/ BMT |
|
|
Chronic nonsuppurative OME
|
-Persistent non-infected middle ear fluid w/ hearing loss
-Tx w/ BMT |
|
|
Acute otitis media w/ tympanostomy tubes
|

-Infection of inner ear in children w/ BMT tubes
-Risk factors include URI, EAC contamination, retained tubes -Bacteriology: S aureus, P aeruginosa, a-hemolytic strep -Sx include purulent otorrhea (no pus = no infection) -Tx w/ ototopical antibiotics such as fluoroquinolones (Ciprodex) |
|
|
Acute otitis externa
|

-Inflammation of EAC
-Often hx of recent water exposure ("swimmer's ear") or mechanical trauma (eg, scratching, cotton applicators) -Bacteriology: staph, gram-negative rods (eg, Pseudomonas, Proteus) or fungi (eg, Aspergillus), which grow in the presence of excessive moisture -Painful erythema and edema of ear canal skin often with a purulent exudate -Tx w/ removal of debris, reacidification, antibiotics, ototopicals |
|
|
Chronic eczematoid otitis externa
|
-Flackey, itchy, weepy/moist EAC
-Usually related to eczema/psoriasis, too frequent q-tipping, astringents -Tx w/ steroid containing ointment, lotion, or emollient |
|
|
Fungal otitis externa
|

-White cheesy debris in EAC
-Often result of overuse of ototopical drops -Tx w/ debridement, antifungals such as Lotrimin or Lotrisone |
|
|
Malignant otitis externa
|

-Skull base osteomyelitis seen in immunocompromised pts
- Persistent foul aural discharge, granulations in the ear canal, deep otalgia -Tx w/ prolonged antipseudomonal antibiotic administration |
|
|
Herpes zoster oticus
|

-Shingles of the ear
-If associated w/ facial nerve paralysis called Ramsey Hunt Syndrome -Tx w/ antivirals or corticosteroids |
|
|
Acute rhinosinusitis
|
-Defined as up to 4 weeks of purulent nasal drainage accompanied by nasal obstruction, facial pain, facial pressure, or fullness
-Bacteriology: S pneumo, H flu, M catarrhalis -Must then distinguish between viral rhinosinusitis (VRS) and acute bacterial rhinosinusitis (ABRS) -Viral Rhinosinusitis -Sx present less than 10 days -Sx are not worsening -Acute Bacterial Rhinosinusitis -Sx present 10 days or more beyond onset of upper respiratory symptoms -Sx worsen within 10 days after an initial improvement -Tx w/ decongestants/mucolytic, humidification/saline irrigation, antibiotic (AM/CL, cefuroxime 1 wk course) |
|
|
Chronic rhinosinusitis
|
-Inflammatory condition of nasal cavity and paranasal sinuses lasting for longer than 12 weeks
-Believed to be multifactorial, resulting from interactions between host anatomy, genetics, and the environment -Bacteriology: S aureus, gram negs, anaerobic, polymicrobial, fungal -Sx include nasal obstruction, facial congestion-pressure-fullness, discolored nasal d/c, fatigue and myalgias -Tx w/ antibiotics (4-6 wks) + nasal steroid, humidification/mucolytic |
|
|
Pediatric sinusitis
|
-Sx include coryza, congestion, LGFs, poor sleep
-Usually an acute nasopharyngitis (adenoiditis) or URI -Tx w/ nasal suctioning and irrigation, decongestants, mucolytics, surgery if failure to improve |
|
|
Darwin's tubercle
|

-Thickening along upper ridge of helix
-A normal variation |
|
|
TOPHI
|

-Small whitish uric acid crystals along peripheral margins of auricles
-Associated w/ gout |
|
|
Keloid
|

-Progressive enlargement of scar by xs collagen formation during healing
-Deformations of ear have high correlation to renal anomalies |
|
|
Cauliflower ear (perichondral hematoma)
|

-Initially caused by blunt trauma to ear and left untreated, turns to scar tissue and calcifies
-Starts as hematoma--if not drained, necrose then scar |
|
|
Seborrheic dermatitis
|

-Dry scales and underlying erythema behind ear
-Caused by pityrosporum ovale -Tx w/ shampoos containing salicylic acid, coal tar, zinc, resorcin, ketoconazole, or selenium |
|
|
Mastoiditis
|

-Postauricular pain, fever and outwardly displaced pinna
-Mastoid often appears swollen and red -Consequence of middle ear infection -Tx w/ myringotomy and IV antibiotics |
|
|
Battle's sign
|

-Periauricular ecchymoses
-Seen several days after basilar skull fracture |
|
|
TM perforations
|

-Small holes in TM membrane
-Caused by direct trauma, infection, loud noise, flying, diving -Never irrigate and avoid swimming and getting water in ears |
|
|
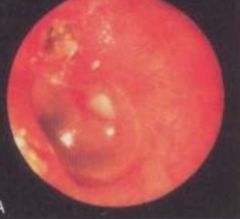
Bullous myringitis
|

-Painful hemorrhagic vesicles on TM, canal, or both
-Associated earache, blood tinged d/c, and conductive hearing loss -Caused by mycobacterium pneumonia -Tx is primarily pain control |
|
|
Serous effusion
|

-Air bubbles in middle ear w/ or w/o hearing impairment, pain
-Caused by Eustachian tube dysfunction, resolving bacterial OM, allergies, large adenoids -Tx w/ antibiotics, antihistamines, decongestants |
|
|
Cholesteatoma
|
-Squamous epithelium in middle ear or mastoid
-Most often result of untreated OM -Purulent otorrhea, conductive hearing loss, tinnitus, mild vertigo -Retraction of TM with a squamous debris collection or a whitish mass behind an intact TM -Tx w/ debridement and ototopical antibiotics |
|
|
Conductive hearing loss
|
-Results from dysfunction of external or middle ear
-Loss of air conduction -There are four mechanisms, each resulting in impairment of the passage of sound vibrations to inner ear: (1) obstruction (eg, cerumen impaction, foreign body) (2) mass loading (eg, middle ear effusion, OM) (3) stiffness effect (eg, otosclerosis) (4) discontinuity (eg, ossicular disruption, TM perforation) -Weber test: sound lateralizes to impaired ear -Tx w/ cleaning, myringotomy w/ tubes, bone conduction hearing aid |
|
|
Sensorineural hearing loss
|
-Results from deterioration of cochlea, usually due to loss of hair cells from organ of Corti
-Loss of bone AND air conduction -Loss may be congenital (present at birth) or acquired -In both congenital and acquired categories, hearing loss may be either hereditary (due to a genetic mutation) or nonhereditary -Most common form is a gradually progressive, predominantly high-frequency loss with advancing age (presbyacusis) -Additional common causes include Connexin 24 & 26, meningitis, aminoglycosides -Weber test: sound lateralizes to unaffected ear -Tx w/ amplification, cochlear implant (direct stim of cochlea) |
|
|
Rhinophyma
|
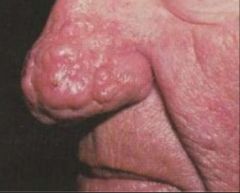
-Hypertrophy of nose w/ follicular dilation
-Results from hyperplasia of sebaceous glands w/ fibrosis and increased vascularity -End stage of roscea |
|
|
Nasal hematoma
|

-Potentially serous complication of nasal fracture
-Can cause necrosis of septum secondary to pressure and low vascularity of septum -Tx w/ immediate drainage by ENT and antibiotics to prevent septal abscess -Untreated can lead to saddle nose deformity |
|
|
Nasal fracture
|
-Most common facial fracture
-Sx include deformity, tenderness, hemorrhage, edema (can mask underlying deformity, crepitation, instability) -Untreated can lead to cosmetic deformity and impaired nasal function |
|
|
Sudden onset HL
|
-Unilateral sensorineural HL of greater than 30 dB over 3 contiguous pure tone frequencies
-Caused by labyrinthine viral infection, labyrinthine vascular compromise, intracochlear membrane rupture, idiopathic -No standart treatment; spontaneous recovery in 47-63% |
|
|
Noise induced HL
|
-Most common preventable cause of hearing loss
-Occurs when 25-30% of hair cells are lost -Can be caused by one time event or continued/repetitive exposure |
|
|
Presbycusis
|
-Most common type of sensorineural hearing loss
-Progressive bilateral symmetrical age-related sensorineural hearing loss -Tends to affect high frequencies more -Tx w/ hearing aids, cochlear implants, portable amplifiers, etc |
|
|
Vestibular deficits
|
-Associated condition of hearing loss
-Low muscle tone, "snuggly" baby, arching of back, delayed disappearance of newborn reflexes |
|
|
Angioedema
|

-Swelling of lips
-Allergic rxn, meds, etc |
|
|
Cheilitis
|

-Dry, cracked lips
-Due to dehydration, dentures/braces, excessive lip licking, sun/wind exposure -Angular (only on corners) or perl'eche (fungal or vitamin deficiency) |
|
|
Chelosis
|

-Deep fissures at corners of mouth
-Can be seen w/ poorly fitting dentures, lip licking, rarely Riboflavin deficiency |
|
|
Herpes labialis
|

-Painful recurrent vesicular and ulcerative lesions of mouth and tongue
-Caused by herpes virus, usually type 1 -Tx w/ acyclovir or valcyclovir |
|
|
Peutz Jegher syndrome
|

-Melanin spots on lip
-Associated w/ multiple polyps of intestine -High risk for colon and small bowel cancer |
|
|
Pyogenic granuloma
|

-Frequently appear following injury, during prego, while taking OCPs
-Can bleed easily -Tx w/ electrocautery, lasers, freezing, excision |
|
|
Strawberry hemangioma
|

-Swelling or growth of endothelial cells lining blood vessels
-Children are born with -May resorb or can be excised |
|
|
Cleft lip
|
-Congenital deformity caused by abnormal facial development
-Can affect muscles in nasopharynx and Eustachian tube -Multifactorial inheritance |
|
|
Squamous cell cancer
|

-Most common form of oral cancer
-Thickened plaque, ulcer, or warty growth usually involving lower lip |
|
|
Mucocele
|

-Painless, thin sac on the inner surface of the lips containing clear fluid
-Caused by traumatic rupture of mucous gland -Tx w/ laser ablation or total excision |
|
|
Aphthous ulcer
|

-AKA canker sore
-Most common oral mucosa lesion -Shallow, recurrent white, round or oval ulcerative lesion w/ red halo and pseudomembrane -Tx w/ tetracycline rinse, kenalog, lidocaine, zine lozenges |
|
|
Salivary gland tumor
|

-80% involve parotid and are benign (pleomorphic adeomas)
-Slow growing, painless masses -Malignant masses most commonly Mucoepidermoid carcinomas |
|
|
Candidiasis
|

-Creamy white, curdlike patches which rub/scrape off w/ friable base
-Caused by Candida albicans -More common after antibiotic use, immunosuppresses, infants, DM, chronic steriods -Tx w/ nystatin oral suspension or chlotrimazole troches |
|
|
Lichen planus
|

-White, reticulated or lacelike lesions
-Can be painful, bilateral -Autoimmune -Tx w/ steroids |
|
|
Koplik spots
|

-White specks w/ redbase opposite 1st/2nd molars
-Associated w/ measles (ribeola) |
|
|
Torus palatinus
|

-Bony protuberance at midline
-No clinical significance unless not midline |
|
|
Palatal lesions
|

-Adenocarcinoma of palate
-Palatal cyst |
|
|
Kaposi sarcoma
|

-Red to purple nodules, macules or papules
-Type of CA -Increased incidence secondary to AIDS |
|
|
Strep pharyngitis
|

-Abrupt onset of sore throat, fever, malaise, nausea, and headache
-Throat red and edematous, with or without exudate; cervical nodes tender -Caused by group A beta-hemolytic strep -Tx w/ penicillin, macrolide, cephalosporin |
|
|
Peritonsillar abscess
|

-Infection of tissue between tonsils and pharynx
-Trismus and "hot potato" voice -Red swollen tonsils, tonsillar pillars and soft tissue adjacent to soft palate -Tx w/ I&D or tonsillectomy |
|
|
Mononucleosis
|

-Fever, sore throat, exudative pharyngitis, uvular edema, tonsillitis, or gingivitis may occur and soft palatal petechiae may be noted
-Caused by EBV -Tx is symptomatic |
|
|
Epstein pearls
|

-Retention cysts
-Small whitish, yellow masses on alveolar gingiva or junction of hard/soft palates -Found in infants and disappear w/in few weeks after birth |
|
|
Gingivitis/periodontitis
|

-Erythematous, bleeding, bulbous, edematous
-Most common cause is plaque -Also phenytoin, OCs, calcium channel blockers |
|
|
Gingival hyperplasia
|

-Enlargement of gingiva
-Can be due to leukemia, dilantin therapy |
|
|
Caries
|

-Discoloration or erosion of crown or base of teeth
-Often painful to percussion |
|
|
Notched teeth
|
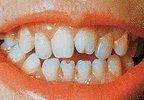
-Hutchinson's teeth from congenital syphilis
|
|
|
Dental abscess
|

-Red, fluctuant tender swelling of gingiva
-Starts w/ infection of pulp that can occur in one of three ways: (1) Defect in enamel and dentin (2) Periodontal pocket (3) Hematogenous seeding of pulp that has been irritated mechanically -Tx w/ antibiotics to fight infection |
|
|
Meth mouth
|

-Characterized by broken, discolored and rotting teeth
-Drug causes salivary glands to dry out, which allows mouth's acids to eat away to tooth enamel -Vasoconstriction and tissue necrosis in moutn |
|
|
Geographic tongue/benign migratory glossitis
|

-Scattered smooth red areas that are denuded papillae
-Condition is benign |
|
|
Leukoplakia
|

-Painless, white plaques that will NOT rub off
-Pre-cancerous |
|
|
Varicosities
|

-Usually seen on ventral surface of tongue
-Blanche w/ pressure |
|
|
Glossitis
|

-Tongue swelling.
-Smooth appearance to the tongue due to pernicious anemia (Vitamin B12 Deficiency). -Tongue color changes (usually dark "beefy" red). -Sore and tender tongue. -Difficulty with chewing, swallowing, or speaking |
|
|
Condyloma
|

-Oral lesion (wart) on tongue
-HPV virus |
|
|
Hairy tongue
|

-Yellow-brown to black elongated filliform papillae on dorsum
-Overgrowth of yeast of bacteria -Can be associated w/ antibiotic therapy, malnutrition, Pepto bismol, smoking, excess coffee |
|
|
Oral hairy leukoplakia
|

-Corrugated or hairy raised nonpainful white lesions on lateral sides of tongue
-Associated w/ EBV |
|
|
Strawberry tongue
|

-Enlarged red papillae on tongue
-Associated w/ Scarlet fever |
|
|
Fissured (scrotal) tongue
|

-Benign condition characterized by deep grooves (fissures) in the dorsum of the tongue
-Appears w/ advanced age, benign |
|
|
Macroglossia
|

-Enlargement, hypertrophy of tongue
-Associated w/ hypothyroidism, Down syndrome |

