![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
43 Cards in this Set
- Front
- Back
|
what cell type lines the pericardium?
|
mesothelial cells
|
|
|
What are the two types of pericarditis, which is more common?
|
Most common pericarditis is a secondary phenomenon.
Primary Pericarditis is almost always viral |
|
|
What are the 5 types of acute pericarditis
|
1. serous
2. fibrinous/serofibrinous 3. purulent/suppurative 4. hemorrhagic 5. caseous |
|
|
how much fluid is normally contained in the pericardium/what type?
|
Normally 15-50mL clear serous fluide (transudate of plasma)
|
|
|
Describe acute serous pericarditis
how much fluid & causes |
50-200mL of fluid of exudates slowly accumulates
often idiopathic, but may be related to non bacterial causes (SLE, turmor, uremia, viruses) or Rheumatic fever |
|
|
what is the most common clinical form of acute pericarditis
|
fibrinous/serofibrinous
|
|
|
describe acute fibrinous/serofibrinous pericarditis
|
serous fluid mixed with fibrinous exudate
see with MI and assoc with pericardial FRICTION RUB (Dressler's syndrome) Can resolve or leave adhesions (adhesive pericarditis) or plaque like thickenings |
|
|
what is dressler's syndrome
|
autoimmune condition several weeks post MI
|
|
|
describe purlent/suppurative pericarditis
|
exudate of pus -->400-500mL
due to infectious organisms in pericardial space red granular appearance organization leads to constrictive pericarditis -->can lead to heart failure |
|
|
how do infectious organisms get into the pericardial space
|
direct extension
seeding of blood lymphatic extension direct introduction during cardiotomy |
|

describe the pathology
|
The epicardial surface of the heart shows a shaggy fibrinous exudate. This is another example of fibrinous pericarditis. This appearance has often been called a "bread and butter" pericarditis, but you would have to drop your buttered bread on the carpet to really get this effect. The fibrin often results in the the finding on physical examination of a "friction rub" as the strands of fibrin on epicardium and pericardium rub against each other.
|
|
|
what are the causes listed in our notes of hemorrhagic pericarditis (4)
|
malignancy
TB clotting disorders surgery ( ie Coronary artery bypass) |
|
|
what infection causes caseous pericarditis
|
TB
|
|
|
describe chronic pericarditis
|
When pericarditis heals or gets organized it might simply produce fibrous thickenings of the serosal membranes (soldier's plaque), or thin, delicate adhesions of obscure origin. In other cases, organization results in complete obliteration of pericardial sac.
(notes say; thick pearly nonadherent epicardial plaque often found with resolved pericarditis-->the above description helped me more) |
|
|
what are the two types of chronic pericarditis
|
a) Adhesive Mediastinopericarditis - this may follow a suppurative or caseous pericarditis, previous cardiac surgery or irradiation to mediastinum.
b) Constrictive Pericarditis - heart is enclosed in a dense, fibrous or fibrocalcific scar that limits diastolic expansion and seriously restricts cardiac output, resembling restrictive cardiomyopathy. |
|
|
Describe Adhesive Mediastinopericarditis
|
Pericardial sac is obliterated, and adherence to the external surfaces of the parietal layer (tethered to mediastinum)produces great strain on cardiac function. The increased workload causes cardiac hypertrophy and dilation, mimicking DCM (Dilated Cardiomyopathy).
|
|
|
Describe Constrictive pericarditis
|
Pericardial space is obliterated and heart surrounded by dense, adherent layer of scar that can resemble a plaster mold in extreme cases (concretio cordis = dec CO).
|
|
|
list the 6 causes in our notes of Immune mediated pericarditis
|
dressler's syndrome
post cardiotomy acute rheumatic fever SLE/RA/Scleroderma drug hypersensativity inflammatory bowel dz |
|
|
describe the natural history of pericarditis
|
usually self limiting, may be relapsing
small % pts dev signs/sx of RHF can lead to fibrosis/constriction several cases tx with pericardiectomy (if needed) |
|
|
see if you can describe the 4 things that differentiate MI from pericarditis
|
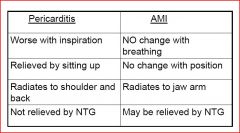
see chart
|
|
|
How much fluid is in a pericardial effusion? what are the consequences
|
>50 mL -->causes intrapleural pressure in the pericardial space, as it rises diastolic filling impaired
|
|
|
describe slow developing effusion
|
can be large (>1000cc) and not cause symptoms
he has myxedema in the slide in parentheses-->if you know what it is let me know |
|
|
describe a rapidly developing effusion
|
trauma - can be small and fatal (<200cc)
|
|
|
When pericardial pressure is rising and diastolic filling is imparied which is affected more, left or right
|
R >>:L
|
|
|
Define pericardial tamponade
|
hemodynamic compromise resulting from a rapid increase in pericardial pressure
|
|
|
what are the causes of pericardial tamponade
|
rapidly developing effusion with significant volume = trauma, aortic dissection, AMI with rupture, iatrogenic
|
|
|
What are the exam findings
|
Echo: diastolic filling impaired with RA and RV collapse
falling CO |
|
|
SIGNS AND SYMPTOMS of Pericardial Tamponade
|
Pulses Paradoxus - greater than 10mmHg drop in systolic BP between inspiration and expiration (dec during inspiration)
|
|
|
what are the 3 causes of special forms of pericardial effusion
|
Chylous effusion
Cholesterol effusion Hemorrhagic effusion |
|
|
what causes a chylous effusion
|
obstruction of the thoracic duct
|
|
|
what causes a cholestrerol effusion
|
Myxedema, RA, TB
|
|
|
what causes a hemorhagic effusion
|
TB, tumor, infection, bleeding disorder, surgery
|
|
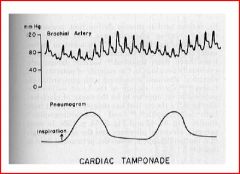
what does this demonstrate
|
pulsus paradoxus
|
|

describe the patholgoy
|
Hemorrhagic pericarditis: (he noted the red nodules in lecture) The surface of the heart with hemorrhagic pericarditis demonstrates a roughened and red appearance. Hemorrhagic pericarditis is most likely to occur with metastatic tumor and with tuberculosis (TB). TB can also lead to a granulomatous pericarditis that may calcify and produce a "constrictive" pericarditis.
|
|
|
what is the most common cuase of constrictive pericarditis worldwide
|
tuberculous pericarditis
|
|
|
List the pathology associated with the mediastinum
|
Chronic Mediastinitis
Cysts (Anterior compartment) THymomoa (Anterior compartment) lymphoma soft tissue neoplasm (neuroma) germ cell tumors |
|
|
What usually causes Chronic Mediastinitis?
|
Usually infectious
fungus = histoplasmosis |
|
|
List the pathology associated with the Thymus
|
aplasia (DiGeorge Syndrome: parathy)
cysts thymoma |
|
|
how does a thymoma typically present
|
it may present as an incidental finding
40% present because of pressure symptoms 40% present as myasthenia gravis it is a tumor of adults can also present as many other paraneoplastic syndromes |
|
|
what size are thymomas,
|
may attain large size (15cm to 20 cm)
|
|
|
what type of histology are thymomas
|
may be cystic, necrotic, or calcified
|
|
|
What percentage are invasive, what is their prognosis
|
20-25% are invasive (locally) and < 50% 5yrs if invasive
|
|
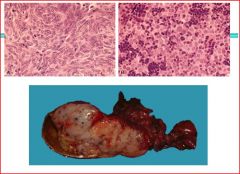
describe the pathology
|
lymphocytes and thymocytes
grossly lobulated -Ask surgeon if came otu easily &/or if had clean margins -->IF NOT think invasive thymoma |

