![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
41 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Which hand tendon can rupture as a result of distal radius fracture? What is the first line treatment? |
Extensor pollicis longus (EPL) rupture is most commonly caused by late effects of distal radius fractures. Devascularization is the most likely cause leading to attritional rupture. Rupture can present 2 weeks to 11 months after fracture; the average is 7 weeks. This patient may extend her thumb when it is adducted because of connections of the intrinsics with the dorsal apparatus. Tendon transfer of the extensor indicis proprius to distal EPL stump is the first-line treatment. |
Distal radius = Colles fracture |
|
|
Recommended treatment for boutonnière deformity? What ruptures? |
The most appropriate position for splint immobilization of an injury leading to a boutonnière deformity is with the distal interphalangeal (DIP) joint free and the proximal interphalangeal (PIP) joint extended. Central slip disruption. |
|
|
|
Which condition does this treatment describe? The most appropriate treatment is relative motion extension splint immobilization for 6 weeks. |
Extensor tendon laceration. |
What is cut & what's intact? |
|
|
A 42-year-old woman comes to the ED after sustaining a deep laceration to the dorsal aspect of the right forearm with broken glass. She reports pain on attempted extension of the middle and ring fingers of the right hand & she cannot extend her fingers beyond the neutral position with her right hand held flat on a table. She is able to extend all digits completely at the interphalangeal joints in all positions of the hand. What is the most likely cause of these findings? |
Extrinsic extensor tendons are cut completely with intact intrinsic muscles. Extension of the interphalangeal joints (IP) and extension of the metacarpophalangeal joints (MCP) to the neutral position after an injury to the forearm extensor tendons is possible through the action of the lumbricals and dorsal interossei (intrinsic hand muscles). The extrinsic extensor tendons alone are responsible for extending the MCP joints beyond neutral. |
|
|
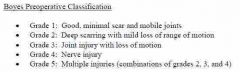
What type of tendon repair for a delayed presentation of grade 1 injury? |
Several conditions must be met for single-stage tendon grafting to be successful. These include a hand and finger that have good passive motion, a well-healed wound with minimal scarring, and a digit that has intact nerves and arteries. If the grade of injury is greater than 1, two-stage grafting should be considered with implantation of a silicone rod and additional treatment to manage the other conditions to increase motion and function, such as joint release or reconstruction for loss of motion, nerve repair/reconstruction, and pulley reconstruction. |
|
|
|
Dorsal dislocation of the thumb at the MCP joint typically occurs with forced hyperextension. Which 2 things can get stuck in the joint? |
Volar plate/collateral ligament & sesamoid bone, which can make it irreducible. |
This is for a grade 1 injury, no bone involved. |
|
|
Rupture of the flexor digitorum profundus (FDP) tendon from its distal attachment is commonly known as X finger. When & how should it be treated? |
Jersey. Type I injuries involve retraction of the profundus tendon all the way to the palm, with associated injuries to the vincula longus and vinculum brevis. Injuries to the vincula disrupt the blood supply to the tendon, necessitating surgical repair within 7 days to avoid necrosis of the tendon and a permanent contracture deformity. |
|
|
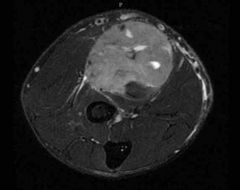
A 45-year-old man has a mass in the left volar forearm. An MRI is shown. Oncologic resection will involve removing all muscles of the anterior forearm compartment. Which of the following techniques is most appropriate to reconstruct finger flexion postoperatively?
A) Flexor digitorum profundus to superficialis transfer B) Flexor pronator slide C) Free gracilis innervated by a median nerve branch D) Oberlin-Mackinnon nerve transfer E) Pedicled latissimus dorsi muscle flap transfer |
Free gracilis |
|
|
|
A Boutonnière deformity occurs with injury to the X tendon and injury or attenuation of the Y ligament. |
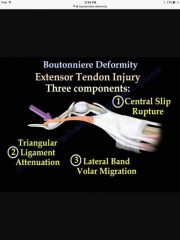
A Boutonnière deformity occurs with injury to the central tendon and injury or attenuation of the triangular ligament. The lateral bands migrate volarly to become proximal interphalangeal (PIP) joint flexors, and their action is on the distal interphalangeal (DIP) joint, extending it. The triangular ligaments are bound by the lateral bands, central slip, and terminal tendon. |
|
|
|
What type of passive ROM is needed for flexor tenolysis to be successful? |
flexor tenolysis; however, the indications are clear that the patient must have minimal soft-tissue edema, minimal scarring, and full or near-full passive range of motion. |
|
|
|
A 42-year-old right-hand–dominant construction worker is evaluated for an 8-week history of pain with wrist motion. Physical examination shows swelling 4 cm proximal to the Lister tubercle. There is tenderness to palpation and crepitation over the muscle bellies of the abductor pollicis longus and extensor pollicis brevis. The remainder of the examination shows no abnormalities. Which of the following is the most likely diagnosis? A) Basal joint synovitis B) de Quervain synovitis C) Extensor pollicis longus tendinitis D) Intersection syndrome E) Wartenberg syndrome |
Intersection syndrome is synovitis of the second dorsal compartment. It is located where the abductor pollicis longus and extensor pollicis brevis cross the extensor carpi radialis longus and extensor carpi radialis brevis. The syndrome often occurs in athletes with repetitive forceful extension. The swelling is located 4 to 6 cm proximal to Lister tubercle. |
|
|
|
How does Wartenberg syndrome present? |
Wartenberg syndrome is radial sensory nerve compression where the nerve exits the supinator muscle. Symptoms would be paresthesia over the radial nerve distribution and a Tinel sign |
|
|
|
What is de Quervain synovitis? Which physical exam test would be positive? |
De Quervain is synovitis of the first dorsal compartment, which would be located over the radial styloid and have a positive Finkelstein sign. |
|
|
|
Ideal time frame to perform nerve grafting with brachial plexus injuries? |
Ideally, nerve transfers are performed within 6 months of the injury. Studies have shown greater than 70% will achieve M3 function for elbow flexion and shoulder abduction. Common donor nerves include the spinal accessory, intercostals, anterior interosseous, and triceps branch. |
|
|
|
A 30-year-old woman comes to the office because of a laceration of the dorsal long finger extensor tendon. Physical examination shows extension of all fingers to zero degrees at the metacarpophalangeal joint. Which structure provides extension force that explains this exam finding? |
Juncturae tendinum are tendon-like bands that connect the long, ring, and little finger extensor digitorum communis tendons. If the long finger extensor tendon is lacerated proximal to the attachment of the juncturae tendinum between the long and ring fingers, the ring finger extensor digitorum communis tendon will apply extension force to the distal long finger extensor tendon via the juncturae tendinum and produce metacarpophalangeal (MCP) extension. |
|
|
|
Swan neck vs Boutonnière deformity: What is the deformity? Mechanism of injury? What is always injured in each? |
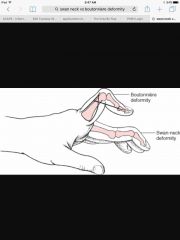
Swan-neck deformity can occur in the post-traumatic setting as well as in the rheumatoid arthritis population. The PIP joint hyperextends, and the DIP joint flexes. Unlike boutonnière deformity, which is always initiated by a rupture of the central slip of the extensor mechanism, the origin of a swan-neck deformity can be at the DIP, PIP, or MCP joint. Regardless of the initiating problem, a swan-neck deformity can only occur if there is laxity of the volar plate of the PIP joint to allow hyperextension. |
|
|
|
A 32-year-old man comes to the office because of a "mallet" deformity of the distal joint of the long finger of the dominant hand sustained 12 years ago while he was playing baseball. He has not sought medical treatment until now. On examination, which of the following deformities is most likely? A) Boutonnière B) Camptodactyly C) Clinodactyly D) Hook-nail E) Swan-neck |
Swan Neck. Flexion deformity of the distal joint seen in mallet finger will lead to secondary hyperextension of the proximal joint. This occurs in a zigzag fashion because of the imbalance of forces. If the terminal tendon is displaced proximally, the conjoined tendons will slide proximally and become extensors to the proximal joint. |
|
|
|
Difference between mallet finger and swan neck deformity? |
Mallet finger can lead to swan neck through rupture of the terminal extensor mechanism. |
|
|
|
20-year-old man comes to the office 2 months after "jamming" the long finger of the right hand in a rugby game. On examination, the patient has a boutonnière deformity. The distal interphalangeal (DIP) joint has 20 degrees of hyperextension and active flexion to 85 degrees. X-ray study shows no fracture. What is the most appropriate initial treatment? |
Splinting of the PIP in extension and active DIP flexion |
|
|
|
A 35-year-old, right-hand-dominant man comes to the office 3 months after he completely severed both the flexor digitorum superficialis and profundus tendons in Zone II of the right long finger. He did not seek medical attention at the time of the injury. Physical examination shows inability to flex actively at the proximal interphalangeal (PIP) joint and distal interphalangeal (DIP) joint. He has passive range of motion. Which of the following is the most appropriate management? A) One-stage tendon grafting B) Primary repair C) Tendon transfer D) Two-stage tendon reconstruction E) Observation only |
When patients present with zone II flexor injuries, it is optimal to repair both flexors within 10 days after the injury before the tendons retract excessively preventing primary approximation of the tendon ends. Late flexor injuries (after 2 weeks) in zones I, III, IV, and V can be managed with single-stage tendon grafting. However, when the injury is in zone II, the sheath has collapsed and tendon grafts cannot be easily pulled under intact pulleys, necessitating pulley reconstruction over a silicone rod in the first stage. Then, in a second stage, the tendon rod is replaced with the tendon graft pulled into the sheath in the proximal to distal direction after suturing the graft to the rod. The tendon is repaired first distally to bone, and then the appropriate tension is set on the proximal juncture repair of the graft to the motor tendon (usually the flexor digitorum superficialis to avoid quadriga and lumbrical plus posture). Two-stage tendon grafting in general is recommended for zone II flexor repairs that present late, require simultaneous critical pulley reconstruction (A2, A4), or if volar finger soft-tissue reconstruction is required. |
|
|
|
For 2-4 strand tendon repair, what is the ideal purchase length? |
For both two-strand and four-strand locking core repair methods, the length of core suture purchase significantly influences both resistance to gapping and also ultimate strength to breaking. The optimal length of purchase is between 0.7 and 1.0 cm. Increased length of purchase from 0.7 to 1.2 cm does not increase the repair strength. Purchase length of 0.4 or less greatly reduces repair strength. |
|
|
|
What treatment should be done for mallet finger in the acute setting? Open vs closed? |
The majority of closed mallet injuries (Type I) in Zone I of the extensor tendon can be treated by continuous extension splinting for 6 to 8 weeks. It is important that the finger not be allowed to flex at the DIP joint during this time period to avoid disruption of healing. Exploration and suture of the tendon is used to treat Type II (open) mallet injuries. |
|
|
|
21-year-old man is brought to the emergency department after sustaining injuries to the right volar wrist when he punched a glass window. Surgical exploration shows a complete laceration through the palmaris longus tendon. Based on the proximity of the patient's injury, which additional structure is most likely injured? |

Median nerve |
|
|
|
What is a Fowler tenotomy? Which finger deformity does it treat? |
The Fowler central slip tenotomy is well known, but seldom used. The central slip or tendon inserts on the base of the middle phalanx and acts on the proximal interphalangeal (PIP) joint. A central slip tenotomy will rebalance the extensor mechanism such that the terminal tendon will be able to extend the distal interphalangeal (DIP) joint in patients with a chronic mallet finger. However, many clinical and anatomical studies have shown that the central slip tenotomy may not restore full extension in patients with a preexisting lag of approximately 36 degrees. Used to treat chronic mallet deformity. |
|
|
|
What causes Jersey finger? Treatments for types I-III including timing? |
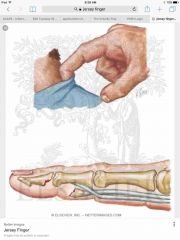
Jersey injury occurs when a player grabs the opposing player’s jersey. The DIP joint is in a flexed position and when the tackle is broken, there is a forced extension. Flexor digitorum profundus (FDP) avulsion occurs 75% of the time in the ring finger. In Type I, the tendon only retracts into the palm and requires urgent repair and reinsertion within 7 to 10 days. In Type II, the tendon retracts to the PIP joint level being tethered by the long vinculum. Repair can be delayed 6 to 12 weeks. In Type III, a large bony fragment blocks the tendon from entering the A4 pulley and can be repaired at any time. The FDP insertion is avulsed from the distal phalanx with or without bone fragments. |
|
|
|
Scaphoid fracture malunion or scaphoid arthritic spurs can result in ruptures to the X tendon. |
Scaphoid fracture malunion or scaphoid arthritic spurs can result in ruptures to the flexor pollicis longus tendon. |
|
|
|
Radial nerve block at the wrist should be performed superficial to which landmark? |
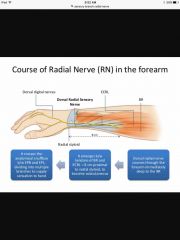
The sensory branch of the radial nerve arises between the brachioradialis and extensor carpi radialis brevis approximately 8 cm proximal to the styloid process of the radius. It pierces the fascia approximately 5 cm (3 fingerbreadths) proximal to the radial styloid. The nerve then fans out proximal to the wrist and passes superficially to the radial styloid and first dorsal compartment. |
|
|
|
The X tendons to the long, ring, and little fingers share a common muscle belly. Thus, holding the long and little fingers in extension will prevent the X to the long, ring, and little fingers from firing. Any flexion of the PIP joint of the ring finger must then be caused by the X tendon. |
The FDP tendons to the long, ring, and little fingers share a common muscle belly. Thus, holding the long and little fingers in extension will prevent the FDP to the long, ring, and little fingers from firing. Any flexion of the PIP joint of the ring finger must then be caused by the FDS tendon. |
|
|
|
Why do zone II flexor transactions need to be repaired right away? |
The tendon sheath will scar down quickly after the tendon retracts. |
|
|
|
Which pulley is most important in the thumb? Which muscle does it attach to? |
Oblique, which comes off adductor pollicus |
|
|
|
Which flexor zone involves carpal tunnel? |
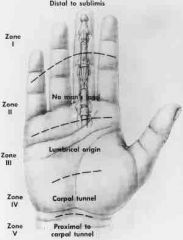
Zone IV |
|
|
|
Flexor tendon repairs: minimum of x strands for early active motion protocol. What size suture? Recommended length from proximal and distal laceration site? |
4 strand 3-0 or 4-0 1 cm |
|
|
|
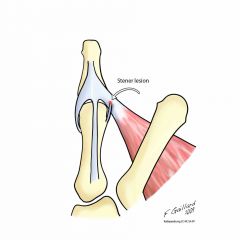
Skiers or gamekeepers thumb where the adductor pollicis is preventing the ulnar collateral ligament from going back where it belongs. Requires OR because this is a complete tear. |
Back (Definition) |
|
|
|
First thing to do when called with skiers or gamekeeper thumb? |
Get an X-ray, because if there's a bone fragment & it's close to where it should be, within 1-2 mm of bone, just thumb spica & don't stress it. |
|
|
|
Which flexor tendon pulleys arise from volar plates? |
A1, 3, 5 |
|
|
|
First line treatment for full, acute collateral ligament tear of the PIP joint? How many degrees of angulation is typical for full tear? |
Repair the collateral ligament, consider it for >20 degrees. |
|
|
|
What is intersecting in intersection syndrome? Where is the pain relative to Lister tubercle? |
Intersection syndrome is synovitis of the second dorsal compartment. It is located where the abductor pollicis longus and extensor pollicis brevis cross the extensor carpi radialis longus and extensor carpi radialis brevis. The syndrome often occurs in athletes with repetitive forceful extension. The swelling is located 4 to 6 cm proximal to Lister tubercle.
|
|
|
|
53-year-old woman comes to the office after undergoing fixation of a humerus fracture 17 months ago. Physical examination shows inability to extend the wrist, fingers, and thumb. Tendon transfers are planned. Transfer of which muscle is most appropriate for restoration of wrist extension? Which muscle is it transferred to? |
Pronator teres: median nerve–innervated muscle that has adequate power and excursion to provide wrist extension. It is typically transferred to the extensor carpi radialis brevis (as opposed to the extensor carpi radialis longus) in these cases to provide for more centrally oriented wrist extension.
|
|
|
|
39-year-old man is referred to the office 4 months after repair of a zone II flexor tendon involving both the flexor digitorum superficialis and flexor digitorum profundus tendons to the right long finger. He still has poor range of motion of his long finger. Physical examination shows 45 degrees of active range of motion at the proximal interphalangeal (PIP) joint and 25 degrees of active range of motion at the distal interphalangeal (DIP) joint. Active and passive ranges of motion are equal. Which of the following is the most appropriate next step in management? A) Continued hand therapy to improve passive range of motion B) Flexor tenolysis C) PIP arthrodesis D) Two-stage flexor tendon reconstruction E) Observation to allow for scar remodeling |
this scenario, the recommended course of action is to continue hand therapy to improve passive range of motion. A successful functional outcome following tendon injury depends on supple joints with full passive range of motion and tendon gliding. The ultimate goal would be to perform flexor tenolysis; however, the indications are clear that the patient must have minimal soft-tissue edema, minimal scarring, and full or near-full passive range of motion. |
|
|
|
A 50-year-old woman comes to the emergency department after sustaining an avulsion injury of the right ring finger proximal interphalangeal (PIP) joint. A photograph is shown. Examination shows the central slip is disrupted, and the inside of the PIP joint is visible through the dorsal wound. The patient is able to actively extend the PIP joint. Which anatomical structure allows the patient to extend the PIP joint? |
Interosseus muscle |
|
|
|
Zone II four-strand flexor tendon repair configurations are strongest when dorsal or volar? |
Dorsal |
|

