![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
60 Cards in this Set
- Front
- Back
|
what is hematochezia?
Melana ? |
Bright red blood in poo
Melana- Black blood in stool (blood has been digested, iron is oxidized) |
|
|
what is an anorectal malformation?
|
Opening to the anus absent or structurally obstructed
Rectum may end in blind sac or connect to urethra, urinary bladder, vagina, scrotum |
|
|
What is Hirschsprungs disease? Associated genetics?
|
Absence of parasympathetic neuronal cell bodies (ganglion cells) of the enteric ganglia
Neurons of the submucosal (Meissner’s) and myenteric (Auerbach’s) plexus Failure of normal caudal migration of enteric neurons produces “aganglionic segment” Familial and sporadic cases related to RET gene loss-of-function mutations |
|
|
a pt is unable to relax the anus and thus develops a congenital form of megacolon. What genetic problem would you likely see? What type of pt would you likely see this in?
** |
This is Hirschsprung's disease, in which you have absence of parasympathetic neuronal cell bodies in the enteric ganglia
so you would see a RET gene loss-of-function mutation Seen in Down Syndrome (Trisomy 21) |
|
|
symptoms of Hirschsprungs Disease?
|
Stenosis and constipation: newborns with failure to pass meconium and vomiting
Dilation of proximal (“upstream”) uninvolved segment of bowel (megacolon) |
|
|
Most common CONGENITAL cause of intestinal obstruction?
Most common functional GI tract disorder ? |
Hirschsprungs
IBS |
|
|
where do diverticuli occur within the wall of the bowel?
|
btw the taenia coli (outer longitudinal layer of muscularis propria)
|
|
|
although the majority are asymptomatic, some pts may present with flatulence or inflammation from retained fecal material with bacterial build-up. What does this describe?
|
Diverticular Disease
|
|
|
Sx’s and signs: abdominal pain, ∆ in bowel habits, dysuria, fever, blood per rectum; leukocytosis, palpable mass, + FOB
describes? (just read this card probably) |
A diverticuli
Abscess Perforation → peritonitis and possibly sepsis Fistulas between colon and adjacent structures(e.g., urinary bladder, segment of bowel, vagina, skin) |
|
|
pt presents with inflammation of the colon that has a "paper-like" plaque that presents after prolonged antibioitic therapy...what is the pathogenesis?
|
Clostridium Difficile
(this is Pseudomembranous colitis due to prolonged ABX use) |
|
|
what is the key problem in IBD?
|
INFLAMMATION
we don't really know why (infection, ischemia, drug rxn) |
|
|
Mouth to anus, skip lesions.....
* |
Chron's Disease
(Human Centipede) |
|
|
Ulcertive Colitis affects where?
* |
anus to colon
|
|
|
is resection going to be helpful for a person with ulcerative colitis or Chron's disease?
|
UC- only affects colon and anus, so you could surgically take them out
whereas in CD, it affects ass to mouth |
|
|
Cobblestoning and Creeping fat are going to be buzz words for what?
** |
Chron's Disease
|
|
|
noncaseating granulomas with multinucleated giant cells is pathognomonic for what?
* |
Chron's Disease
note: Transmural inflammation (full-thickness |
|
|
Ulcerative Colitis vs. Chrons
Continuous lesions |
UC
(Chron's are spot lesions) |
|
|
Ulcerative Colitis vs. Chrons
full thickness affected |
Chrons
(UC is NOT full thickness, only mucosa and submucosa) |
|
|
radiographic lead pipe appearance?
* |
Ulcerative colitis
note: With prolonged inflammation, develop inflammatory pseudopolyps; crypt abscesses |
|
|
With prolonged inflammation, develop inflammatory pseudopolyps; crypt abscesses
what does this occur in? * |
Ulcerative colitis
|
|
|
What is indeterminate colitis?
|
Cannot distinguish btw CD and UC
|
|
|
a polyp that is an abnormal proliferations/arrangements of normal tissue constituents is what kind of polyp?
|
Hamartomatous
|
|
|
what is polyposis syndrome?
|
multiple hamartomatous polyps
|
|
|
Mucocutaneous lesions sucha as tricholemmomas, oral mucosal papillomas, acral keratoses are associated with what?
|
Cowden’s syndrome
|
|
|
Mucosal pigmentation of the buccal mucosa and lips are associated with what?
|
Peutz-Jeghers polyposis
|
|
|
Peutz-Jeghers polyposis and Cowden's syndrome have increased risk of what?
|
Malignancy (the polyps themselves do not give rise to the neoplasm)
Peutz-Jeghers polyposis: gastric, small bowel, colorectal, pancreas, breast, lung, ovary Cowden's syndrome: thyroid, breast), but not likely in colorectal polyps (these are considered benign) |
|
|
doing an ophthalmologic exam on a child you see dark spots on the retina, what might you think
|
Familial adenomatous polyposis (FAP)
|
|
|
upon scope and biopsy you find a pt with hyperplastic polyps. What should you do next?
|
nothing!
they don't normally enlarge, they are asymptomatic, and have minimal malignant potential you don't even need to watch them more closely |
|
|
what type of adenoma is more likely to become an invasive carcinoma?
|
Villous (as opposed to Tubular)
|
|
|
genetics associated with Familial adenomatous Polyposis (FAP)
*** |
inactivation of adenomatous polyposis coli (APC) tumor suppressor gene
|
|
|
what are Gardner's syndrome and Turcot's syndrome?
|
Gardner’s syndrome (AD) polyposis with osteomas and desmoid tumors
Turcot’s syndrome (AR) polyposis with CNS tumors |
|
|
how do you get from adenoma polyp to Colorectal carcinoma
** |
in general you just get a sequence of gene changes
APC → RAS → p53 |
|
|
What are the mismatch repair genes that malfunction in Hereditary Nonpolyposis Colon Cancer (HNPCC)?
* |
MLH1
MSH2 |
|
|
what sided Colorectal cancer is associated with the following?
Change in bowel habits occur earlier, can have dark blood |
Left-sided
this is because the bowel diameter is smaller |
|
|
what sided Colorectal cancer is associated with the following?
iron deficiency anemia |
Right-sided CRC
DUE TO MORE SUBSTANTIAL BLEEDING |
|
|
what sided Colorectal cancer is associated with the following?
Larger tumors |
Right-sided CRC
(larger diameter bowel) |
|
|
Colorectal cancer tends to spread to where?
|
Liver most often
|
|
|
3 most common anorectal neoplasms?
|
Basaloid carcinoma
Adenocarcimona squamous cell carcinoma |
|
|
why are mucoceles important when found in the appendix (2)
|
Non-neoplastic, obstructed appendix (just fills with mucous)
Mucinous cystadenoma or cystadenocarcinoma |
|
|
what is a Pseudomyxoma peritonei
|
Mucinous neoplasm erodes through the appendiceal wall and mucinous tumor implants throughout peritoneum – e.g., on ovaries
Confused with primary ovarian mucinous neoplasm |
|
|
receptor tyrosine kinase, plays crucial role in neural crest development
Loss of function mutation in Hirschsprung Dz |
RET gene
|
|
|
Newborn patient presents with a chronically contracted muscularis causing constipation
Intestinal biopsy reveals: Absence of submucosal enteric ganglion cells with compensatory hypertrophy of non-enteric parasympathetic nerve fibers that normally innervate the enteric ganglion cells |
Hirschsprung Dz
|
|
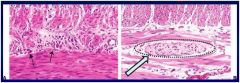
What's happening in Panel B?
|
Hirschsprung Dz
Biopsy shows a [hypertrophied] nerve in the mesenteric plexus (arrow) and an absence of ganglion cells |
|
|
**Pathogenesis:**
– Prolonged increased intraluminal pressure • Lack of adequate fiber • Most often affects sigmoid colon **Symptoms** – Asymptomatic in majority of cases (~ 80%) – Flatulence – Inflammation from retained fecal material (~ 10-20%) |
Diverticular Dz
|
|
|
• Located between taenia coli (outer longitudinal layer of muscularis propria)
– At sites of penetrating nutrient blood vessels surrounded by collagen, less wall integrity • Surrounding muscular wall is hypertrophied |
Diverticuli
|
|
|
CD vs UC
Radiography: “string sign” from narrowed lumen |
Crohn's Dz
|
|
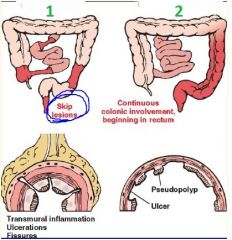
CD vs UC
|
1: Crohn's DZ
2: Ulcerative Colitis |
|
|
CD vs. UC
Extraintestinal Features: -nephrolithiasis |
Crohn's Dz
|
|
|
CD vs. UC
Extraintestinal Features: -Primary sclerosing cholangitis (PSC) |
Ulcerative Colitis
|
|
|
CD vs. UC
Clinical Presentation: -RLQ colicky pain; BPR (blood per rectum); aphthous ulcers (mouth) |
Crohn's Dz
|
|
|
CD vs. UC
Clinical Presentation: - Left-sided abdominal pain, bloody diarrhea w/ mucus |
Ulcerative Colitis
|
|
|
CD vs. UC
Laboratory: - p-ANCA neg. & ASCA pos. |
Crohn's Dz
|
|
|
CD vs. UC
Laboratory: - p-ANCA pos. & ASCA neg. |
Ulcerative Colitis
|
|
|
CD vs. UC
Which one is more likely to cause: Epithelial dysplasia and adenocarcinoma *** |
UC
**Most likely to cause cancer!!** |
|
|
T/F
• All adenomas, by definition, exhibit at least lowgrade dysplasia and are neoplastic ***EXAM*** |
True!!
Note: -Adenomas are common and typically asymptomatic -Prevalence increases with age |
|
|
What is the initial proliferative abnormality of the colonic mucosa that
leads to the accumulation of mucosal cells --> adenocarcinoma |
the extension of the mitotic zone in the crypts
|
|
|
Internal/External Hemorrhoids
–superior plexus, above pectinate line • Bleeding, “painless” |
Internal
|
|
|
Internal/External Hemorrhoids:
– inferior plexus, below pectinate line • Painful thrombosis |
External
|
|
|
FAP vs HNPCC
Hundreds of adenomas, with malignant transformation in 30’s or 40’s |
FAP
(There aren't tons of polyps present in HNPCC) |
|
|
What is seen in almost all cases of HNPCC but only ~ 15% of
sporadic cases? |
Micro Satellite Instability (MSI)
(If cancer arises with abscense of polyps; look for MLH1 and MSH2 gene mutations to Dx HNPCC!) |

