![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
32 Cards in this Set
- Front
- Back
|
Which organisms produce Shiga
toxin or Shiga-like toxin? 1. Vibrio cholerae 2. Salmonella typhi 3. Shigella dystenteriae 4. Shigella sonnei 5. Enterohemorrhagic E. coli |
Shigella dystenteriae
Enterohemorrhagic E. coli |
|
|
In what way(s) is EIEC like Shigella?
1. Type III secretionsystem to invade mucosal epithelial cells 2. Assemble actin tails to propel laterally through the epithelium 3. Escape the phagosome and multiply in cytosol 4. All of the above |
All of the above
|
|
|
Clinical symptoms:
hemorrhagic colitis (bloody stool; cranberry sauce-like) Transmission: foods (unpasteurized apple cider, milk, fresh vegetables), petting zoos and dairy farms (organism found in cattle feces) • Most severe in young children (can also result in high mortality in the elderly) |
Enterohemorrhagic E. coli
(EHEC) |
|
|
When you hear news reports about
outbreaks of “E. coli” infections, they are usually talking about : |
E. coli O157
|
|
|
In what way(s) is EHEC similar to
EPEC? 1. Non-invasive 2. Invasive 3. Forms an actin pedestal 4. Does not cause bacteremia 5. Causes attaching and effacing lesions 6. Produces Shiga toxin 7. Produces fever |
Non-invasive
Forms an actin pedestal Does not cause bacteremia Causes attaching and effacing lesions |
|
|
A major sequelae of infection with
Shiga-like toxin producing E. coli (STEC) and Shigella dysenteriae is development of: |
hemolytic uremic syndrome
(HUS) |
|
|
How does Shiga toxin cause
disease? 1. ADP-ribosylates Gsa 2. ADP-ribosylates elongation factor 2 3. Inactivates the 60S ribosome to inhibit protein synthesis 4. Induces calcium release inside the cell |
Inactivates the 60S ribosome to inhibit protein synthesis
|
|
|
Pathogenesis:
thought that Shiga toxin is absorbed across the intestine and gains access to the blood |
HUS caused by STEC (shiga-toxin E. coli)
|
|
|
____ is the leading cause of acute renal failure in children
|
Diarrhea-associated HUS
|
|
|
What is a hallmark finding of HUS?
|
Microangiopathic hemolytic anemia
- Endothelial dysfunction is the triggering event in the development of microangiopathic processes, mainly affecting endothelial cells located in the renal microvasculature |
|
|
Why would you see Thrombotic thrombocytopenic purpura in HUS?
|
Platelet consumption as a
result of thrombi in the microvasculature |
|
|
A 6-year-old boy presents to the ER with a 2-day history of
diarrhea. His condition was worsening with about a dozen bowel movements that day that had become bloody. He also complained of pain on defecation. He had vomited once and is afebrile He attended a cookout 6 days earlier and claims his mother made him eat a hamburger that was “pink inside”. His physical exam was benign except for dehydration. His white blood count was 13,100/mm3 (normal is 3,200-9,800/mm3) with 87% PMNs (normal is 54-62%) Gram stain of the stool showed many PMNs and was positive for quaiac. He was admitted to the hospital and treated with IV fluids. No antibiotics were given. He quickly improved and was discharged the next day Diagnosis? 1. EIEC 2. EHEC 3. ETEC |
EHEC
|
|
|
Salmonella = motile/nonmotile
Shigella= motile/nonmotile Yersinia= motile/nonmotile |
Salmonella = motile
Shigella= nonmotile Yersinia= nonmotile |
|
|
- More common in Northern Europe and Canada due to non-pasteurization of certain dairy products, eg. cheese
• Acute diarrhea and vomiting in young children (pseudoappendicitis) • Causes an invasive infection • Can cause liver and spleen abscesses and an inflammatory colitis • Reactive polyarthritis occurs as a complication in approximately 15% of patients |
Yersinia enterocolitica
|
|
|
Your patient is a 45-year-old woman who returned from a visit to Japan with watery diarrhea, abdominal pain, nausea, vomiting, headache and chills.
She consumed a lot of seafood during her stay, especially her favorite seafood: mussels What is your diagnosis? 1. Salmonella typhi 2. Vibrio cholerae 3. Shigella dysenteriae 4. EHEC 5. Vibrio parahaemolyticus |
Vibrio parahaemolyticus
|
|
|
• Halophilic (salt-loving; lives in brackish salt water)
• Non-invasive in the GI tract (can invade wounds) • Gastroenteritis from ingesting contaminated raw seafood (shellfish) - Leading cause of human gastroenteritis associated with seafood consumption in the United States • Clinical symptoms include diarrhea, abdominal cramps, nausea, vomiting, headache, fever and chills • Highest incidence in Japan (~35% of all food poisoning outbreaks) |
Vibrio parahaemolyticus
|
|
|
Has Two toxins that cause hemolysis:
-thermostable direct hemolysin (TDH) -TDH-related hemolysin (TRH) Damages erythrocytes by forming a pore (2nm) in the membrane resulting in osmotic lysis |
Vibrio parahaemolyticus
|
|
|
A 18-year-old man presents to your clinic with abdominal pain and diarrhea. He reports that he had consumed some undercooked “pink” chicken at a BBQ he attended about 4 days ago
3 days after the BBQ he reports passing 10 stools per day. On the third day of his symptoms he observed blood in his stool and decided to book an appointment to see you A day before the stools started he reports feeling dizzy, delirious and had general aches that lasted about 24h |
Campylobacter jejuni
|
|
|
Vibrio and Campylobacter both have:
|
POLAR FLAGELLA
|
|
|
What is the most common cause of
inflammatory enteritis in US? |
Viruses (e.g., adenovirus, rotavirus,
Norwalk virus) are the most common cause of diarrhea in the United States |
|
|
• Curved, Gram-negative bacilli
• Motile: polar flagella • Incidence is slightly less than Salmonella • Wet mount = gull-winged organisms with darting motility |
Campylobacter
|
|
|
- Ingest organisms from contaminated food (chicken) or water (often in contact with infected animals)
• Organisms multiply in small intestine and invade mucosal layer • Organisms may spread to mesenteric lymph nodes • Bacteremia and septic arthritis in susceptible populations |
Campylobacter
|
|
|
**EXAM**
Infections of C. jejuni often precede _________ and is associated with axonal degredation, slow recovery, and severe residual disability |
Guillan-Barre Syndrome
|
|
|
G+ Spore Former
Anaerobe Motile |
Clostridium difficile
|
|
|
What is another Gram + rod that is
spore-forming, motile but aerobic and which causes diarrhea? Hint:food poisoning and not C. diff 1. Staphylococcus aureus 2. Streptococcus mutans 3. Candida albicans 4. Bacillus cereus 5. EHEC |
Bacillus cereus
|
|
|
G+ Rod
spore former AEROBE Motile |
Bacillus cereus
|
|
|
This bug is associated with Antibiotic Associated Pseudomembranous Colitis
|
C. diff
|
|
|
How can you detect C. diff toxin in stool?
|
latex agglutination or EIA procedure
|
|
|
• Gram-positive bacillus
• Obligate anaerobes • Spore forming: large oval subterminal spores • Leading cause of hospitalassociated diarrhea (nosocomial diarrhea) in the US and Europe • Toxins: toxin A (enterotoxin causing fluid accumulation in the intestine) and toxin B (cytopathic agent) |
Clostridium difficile
|
|
|
How do the A and B toxins of C. diff work?
|
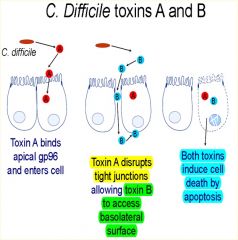
|
|
|
**Clostridium difficile**
Where does Toxin A bind? How does this effect Toxin B? |
binds gp96 (a heat shock protein) on the apical surface of colonocytes and enters the cell.
The toxin disrupts tight junctions allowing toxin B access the basolateral surface of colonocytes |
|
|
How do A & B toxins of C. diff compare to Cholera Toxin and LT toxin (ETEC)?
|
CT and LT trigger fluid secretion
WITHOUT intestinal inflammation |

