![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
146 Cards in this Set
- Front
- Back
|
What are some congenital abnormalities of the small and large intestine?
|
- duplications
- malrotation - omphalocele - gastroschisis - imperforate anus - congeital aganglionic megacolon (Hirschsprung disease) - atresia - stenosis - diverticula - Meckel's diverticulum - heterotopias: gastric and pancreatic tissue most often seen in duodenum |
|
|
What is this congenital disease?
- diverticulum about 2 ft from ileocecal valve - about 2 inches long - symptoms similar to appendicitis |
Meckel's diverticula
- omphalomesenteric duct |
|
|
What is this congenital disease?
- absence of ganglion cells (auerbach and meissner) in the large intestine |
Hirschsprung disease
- constriction of the distal aganglionic segment with proximal dilation -> risk of rupture of intestine - ret gene involved |
|
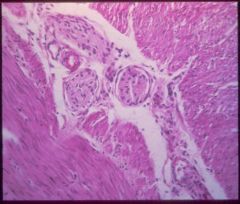
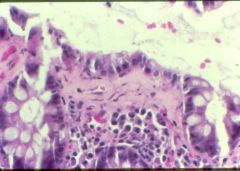
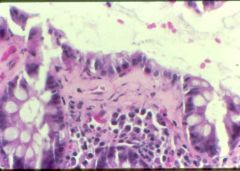
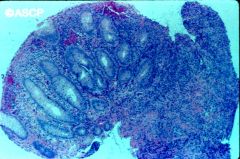
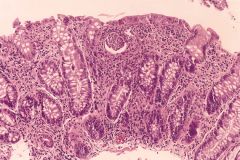
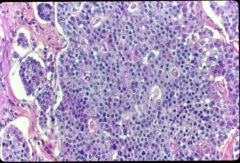
What is this disease? (hint: what is missing in this biopsy?)
|

Hirschsprung disease
- absence of ganglion cells in the large intestine: auerbach (muscular wall), meissner (submucosa) - RET oncogene involved |
|
|
What are some causes of acquired megacolon?
|
- chagas disease
- organic obstruction: tumor or inflammation - toxic megacolon: ulcerative colitis or Crohn's - functional psychosomatic |
|
|
What kind of toxin does C. diff have?
|
- A/B exotoxin
- cause psudomembrane colitis: firin, inflammatory cells, cellular debris |
|
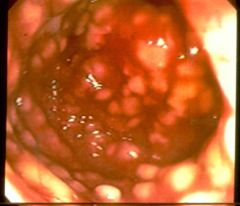
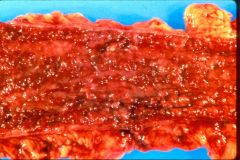
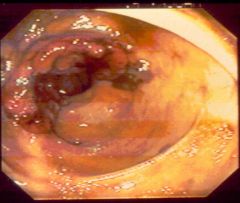
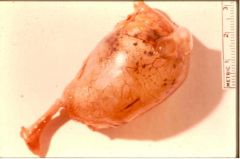
What is this disease?
- redness - yellow/white plaques |

pseudomembranous colitis (c. diff)
- fibrin - inflammatory cells - cellular debris |
|
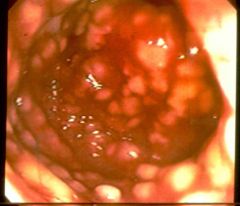
What is this disease?
- redness - yellow/white plaques |

pseudomembranous colitis (c. diff)
- fibrin - inflammatory cells - cellular debris |
|
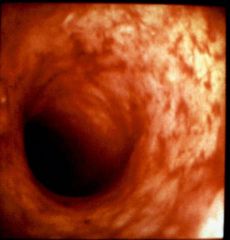
What is this disease?
- exploding crypt: fibrin, inflammatory cells, cellular debris |
pseudomembranous colitis (c. diff)
- after use of antibiotics (clindamycin) |
|
|
Abornalities in the following result in what condition?
- intraluminal digestion: brushborder of small intestine - terminal digestion - transepithelial transport |
malabsorption
|
|
|
Name two malabsorptive diseases.
|
- celiac disease
- Crohn's disease |
|
|
Conditions in intestine that promote bacterial overgrowth. (3)
|
- stasis
- hypochlothydria - immune deficiencies |
|
|
What is this disease?
- skin: itchy rash made of bumps and blisters - anti-endomysial and anti-gliadin antibody |
celiac disease
- cutaneous dematitis herpetiformis - cell mediated immunity (CD8 T cells) - HLA DQ2/8 - villous atrophy with crypt hyperplasia, increased intraepithelial lymphocytes - risk for carcinoma and lymphoma |
|
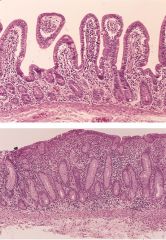
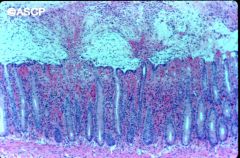
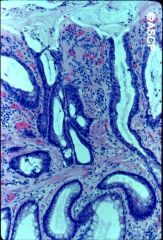
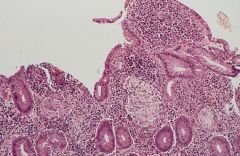
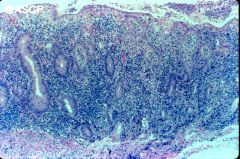
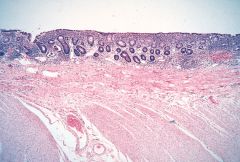
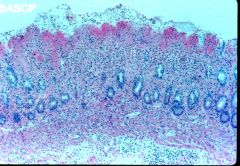
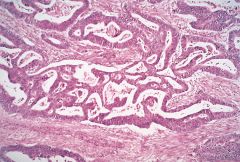
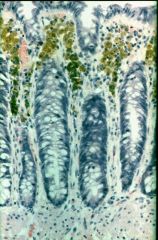
What is this disease?
- low serum level of iron, fat soluble vitamins - H&E: top (normal), bottom(villous atrophy with crypt hyperplasia, increased intraepithelial lymphocytes |
celiac disease
- flattened mucosa - thickened crypt - serum antibodies: anti-endomysial, anti-gliadin |
|
|
What is the genetic predisposition of celiac disease?
|
- HLA DQ2/8
|
|
|
What is this disease?
- multisystem disease - shaggy appearance to intestinal mucosa: enlarged villi - lymphadenopathy - etiology: PAS positive inclusions in macrophages |
Whipple's disease
- tropheryma whippelii |
|
What is this disease?
- Weight loss, diarrhea, joint pain, and arthritis - white male on 30s/40s - PAS stain as above |
Whipples disease
- tropheryma whippelii - multisystem disease - malabsorption - treatable by antibiotics |
|
|
How to treat pseudomembranous colitis?
|
oral vancomycin or metronidazole
|
|
|
What is the malabsorptive disease?
- watery osmotic diarrhea - bloating, flatulence - hypoglycemia with lactose dose |
lactase deficiency- enzyme at brushboder in the small intestine
|
|
|
What can cause acquired lactase deficiency?
|
- oral antibiotics
- viral gastroenteritis |
|
|
T/F: Unlike celiac sprue whixh affect proximal small intestine, tropical sprue affect the entire small intestine.
|
T.
|
|
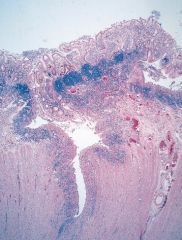
What is this disease?
- no gross abnormality - collagen deposition in submucosa |
collagenous colitis
- |
|
|
In order to diagnose idiopathic IBD, what DDXs need to be ruled out?
|
- collagenous colitis
- HUS - Bechet - infections - radiation colitis - solitary rectal ulcer syndrome - ulcer of the colon - necrotizing enterocolitis - small bowel bypass colitis - eosinophilic colitis |
|
What is this disease?
- smooth muscle band in lamina propria - mucosal prolapse - DDX of IBD |
solitary rectal ulcer
- mucosal prolapse due to pulling if mucosa |
|
|
Genetic predisposition of Crohn's disease.
|
HLA-DR1
HLA-DQw5 |
|
|
Genetic predisposition of ulcerative colitis.
|
HLA-DR2
|
|
|
Genetic predisposition of IBD with ankylosing spondylitis.
|
HLA-B27
|
|
|
How ia IBD diagnosed?
|
colonoscopy
|
|
|
Epidemiology of Crohn's disease.
|
- white > non-whites
- Jewish > non-Jewish - adolescents and young - female > male |
|
|
What part of intestine do you see Crohn's disease.
|
all
- 30% small intestine only - 30% both - 30% colon only |
|

What is this lesion of Crohn's?
|
crohn's disease
- linear ulcers |
|

What is this lesion of crohn's?
|
- serositis: fat wrapping, adehsions
- thick walls - linear ulcers |
|
What is this lesion of Crohn's?
|
cobblestone mucosa
- ulcers underline the mucosa |
|
What is this lesion of Crohn's?
|
fistula
|
|

What is this lesion of Crohn's?
|
stenosis
- need to rule out ischemia and carcinoma |
|
|
What are some gross pathology of Crohn's disease?
|
- thickened wall
- ulcers that skip areas: linear, aphthous - cobblestone mucosa: ulcers underlining mucosa - stricture - fistula - serositis: fat wrapping, adhesions - mucosal edema - anal involvement - lymphadenopathy |
|
|
What are some microscopic features of Crohn's that differ from ulcerative colitis?
|
- granulomas
- transmural inflammation - fissuring ulcerations, focal - vasculitis - sharp transition from inflammed mucosa to normal mucosa - submucosal edema |
|
|
What are some gross pathology of Crohn's disease?
|
- thickened wall
- ulcers that skip areas: linear, aphthous - cobblestone mucosa: ulcers underlining mucosa - stricture - fistula - serositis: fat wrapping, adhesions - mucosal edema - anal involvement - lymphadenopathy |
|
|
What are some microscopic features of Crohn's that differ from ulcerative colitis?
|
- granulomas
- transmural inflammation - fissuring ulcerations, focal - vasculitis - sharp transition from inflammed mucosa to normal mucosa - submucosal edema |
|
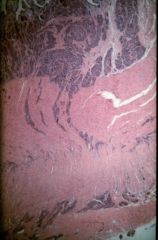
Crohn's or ulcerative colitis?
|
Crohn's
- this is a focal lesion - transmural inflammation |
|
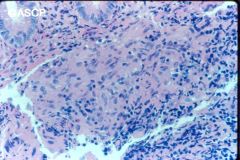
Crohn's or ulcerative colitis?
|
Crohn's
- granulomas |
|
Crohn's or ulcerative colitis?
|
Crohn's
- fissuring ulcers |
|
|
In order to make a diagnosis of Crohn's disease, what biopsy features should you aim for?
|
- segmental transmural inflammation
- noncaseating granulomas - fissuring ulcerations with fistula formation - aphthous ulcers - preserved goblet cells, intact crypts - mucosal/submucosal edema - patchy mucosal inflammation - lymphoid aggregates around blood vessels (vasculitis) - normal rectum |
|
|
What diseases can cause granulomas in the colon?
|
- Crohn's
- TB, fungal, bacterial infection - UC with foreign body reaction - sarcoid |
|
|
What is this disease?
- diarrhea with fever and pain - bloody stool with anemia - obstruction - fistula - malabsorptive symptoms |
Crohn's disease
|
|
|
How to treat Crohn's disease?
|
- anti-inflammatory
- surgery |
|
|
Why do people with Crohn's disease present with malabsorption?
|
- affect small intestine: chunked out (shorter)
- fibrosis of mucosa |
|
|
Which is more common, Crohn's or UC?
|
UC is slightly more common
|
|
|
Crohn or UC?
- intact serosa - normal wall thickness - continuous spread of inflammation (pancolitis): left to right - mild enlargement of lymph nodes - mucosal atrophy |
UC
|
|
|
Acute or chronic UC?
Gross - granular - ulcerated - inflammatory polyps (pseudopolyp) |
acute phase
|
|
|
Acute or chronic UC?
Microscopic - diffuse colitis - mucin depletion - crypt abscess and cryptitis - crypt distortion - basal palsmacytosis |
acute phase
|
|
|
Acute or chronic UC?
Gross - atrophic mucosa - shortened colon |
chronic phase
|
|
|
Acute or chronic UC?
Microscopic - crypt distortion and shortening - basal plasmacytosis and inflammation - preserved mucin - thickened muscularis mucosae - paneth cell metaplasia |
chronic phase
|
|
|
How to differentiate acute UC from chronic UC by gross exam?
|
acute
- granular - inflammatory polyp - ulcerated chronic - atrophic mucosa - shortened colon |
|
|
How to differentiate acute UC from chronic UC by microscopic exam?
|
acute
- mucin depletion - crypt abscess chronic - crypt distortion and shortening - preserved mucin - thickened muscularis mucosae - paneth cell metaplasia |
|
|
Acute or chronic UC?
Microscopic - crypt distortion and shortening - basal plasmacytosis and inflammation - preserved mucin - thickened muscularis mucosae - paneth cell metaplasia |
chronic phase
|
|
|
How to differentiate acute UC from chronic UC by gross exam?
|
acute
- granular - inflammatory polyp - ulcerated chronic - atrophic mucosa - shortened colon |
|
|
How to differentiate acute UC from chronic UC by microscopic exam?
|
acute
- mucin depletion - crypt abscess chronic - crypt distortion and shortening - preserved mucin - thickened muscularis mucosae - paneth cell metaplasia |
|
|
Acute or chronic UC?
Microscopic - crypt distortion and shortening - basal plasmacytosis and inflammation - preserved mucin - thickened muscularis mucosae - paneth cell metaplasia |
chronic phase
|
|
|
How to differentiate acute UC from chronic UC by gross exam?
|
acute
- granular - inflammatory polyp - ulcerated chronic - atrophic mucosa - shortened colon |
|
|
How to differentiate acute UC from chronic UC by microscopic exam?
|
acute
- mucin depletion - crypt abscess chronic - crypt distortion and shortening - preserved mucin - thickened muscularis mucosae - paneth cell metaplasia |
|
Crohn's or UC?
|
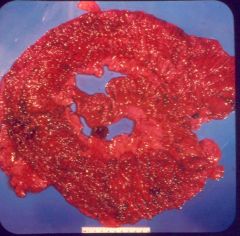
UC (acute)
- pancolitis - normal wall thickness - granular - inflammatory polyps |
|
Crohn's or UC?
|

UC (chronic)
- mucosal atrophy |
|
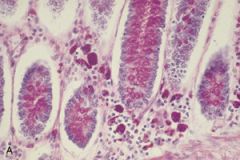
Crohn's or UC?
|
UC (acute)
- crypt abscess - mucin depleted - no granuloma - no fissuring ulcers |
|
Crohn's or UC?
|
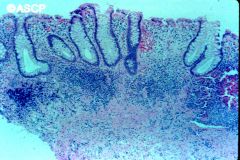
UC (chronic)
- thickened muscularis mucosae - preserved mucin - no granuloma - no fissuring ulcers |
|

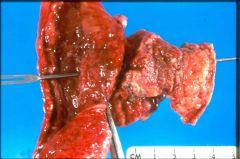
Crohn's or UC?
|
UC- toxic megacolon
- dilated, ulcerated, black, pus on the outside - thinned wall - transmural inflammation - fissuring ulcers |
|

High or low grade UC?
|
high grade
|
|
High or low grade UC? rexommendation?
|
high garde dysplasia
- dark nuclei - consider colectomy |
|
|
Risk factors for colon cancer in UC.
|
- duration of disease
- severity of disease - extent of disease |
|
|
High or low risk for colon cancer?
UC: pancolitis for 10 years |
highest risk
- 20-30x increase |
|
|
UC vs. Crohn's
- diffuse - left to right - continuous - mucosal - high risk for cancer |
UC
|
|
|
UC vs. Crohn's
- focal - right to left - skip areas - transmural - low risk for cancer |
Crohn's
|
|
|
IBD diagnosus is composed of what 3 items.
|
- clinical history
- adequate tissue biopsy: multiple sites, multiple pieces - always biopsy the rectum |
|
|
Stages of intestinal necrosis.
|
From mucosal surface to wall
- epithelial slough, mucosal congestion and hemorrhage - mucosal necrosis with mucosal congestion and hemorrhage - deeper hemorrhagic necrosis - full thickness hemorrhagic mural necrosis - wall rupture -> peritonitis |
|
What stage of ischemia is this?
|
mucosal
- dead surface - residual preserved crypts |
|
|
What are some causes of ischemic injury?
|
- arterial thrombosis
- arterial embolism - venous thrombosis: less distinct demarcation between dead and preserved portion - nonocclusive ischemia |
|

What are some causes of this?
|
transmural ischemia
- SMA: vasospasm, emboli, atherosclerosis - SMV: hypercoagulable state, stasis, CHF - decreased flow in hypotensive episodes - torsion - strangulated hernias |
|
|
What type of symptoms do elderly present with transmural intestinal ischemia?
|
vague symptoms
|
|
|
Causes of intestinal mucosal ischemia.
|
- hypoperfusion
- shock/sepsis - radiation |
|
|
What portion of the colon is more susceptible to chronic ischemia?
|
SMA and IMA watershed area
|
|
|
Chronic intestinal ischemia may lead to ____.
|
stricture
|
|
|
What is this disease?
- tortuous submucosal collapsed vessels - usually in cecum and right colon - often diagnosed by radiologist |
angiodysplasia
- 20% of significant lower GI bleeds |
|
|
What is the most common site for acquired intestinal diverticula?
|
sigmoid colon
- highest luminal pressure |
|
|
Pathogenesis of acquired diverticula.
|
- wall weakness
- increased intraluminal pressure |
|
|
Complications of diverticula.
|
- abscess
- perforation - fistula - bleeding |
|

What is this disease?
|

diverticula
|
|

What complication of diverticula is this?
|
perforation
|
|
|
Name 6 major areas of intestinal obstructive lesions.
|
- intussusception: telescopic intestine
- meconium ileus: premature infants, CF infants - tumors and infarcts - hernias - adnesions - vovulus |
|

What is this called? What can this lead to?
|

intussusception
- compromise vascular supply -> ischemia |
|
|
2 types of hernia.
|
incarcerated vs strangulated
- incarcerated: trapped colon that can not be pulled out - strangualted: vascular supply compromised -> ischemia |
|
|
Areas of hernias.
|
- inguinal and femoral canals
- abdominal wall - retroperitoneal |
|
|
Is it common to see tumors in small intestine? What types of tumors would you see?
|
Very rare to see.
- adenomatous polyps at ampula of vater - adenocarcinoma |
|
|
What are some non-neoplastic polyps of colon and rectum? 3
|
- hyperplastic polyps
- juvenile polys - peutz-jeghers |
|

What is this lesion? risk for cancer?
|
hyperplastic polyp
- no/low cancer risk |
|

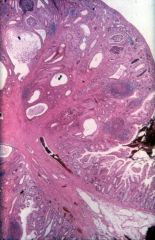
What are these lesions?
|
- left: hyperplastic polyp
- right: Peutz-jegher polyp (arborizing) |
|
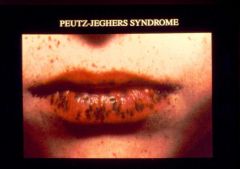
What is this person's condition? risk of cancer?
|

Peutz-Jehger syndrome
- polyps (hamartoma) throughout GI mucosa - mucosal hyperpigmentation - increased cancer risk |
|

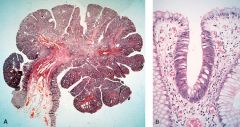
What is this lesion? risk of caner?
|
juvenile polyp
- usually in rectum of children - lamina propria expansion - low cancer risk |
|
|
What are the three patterns of adenomatous polyps?
|
- tubular
- villous - tubulovillous |
|

What is this? What is the histologic feature? cancer risk?
|
tubular adenomatous polyp- increased risk for cancer
- pedunculated - nuclear crowding - loss of goblet cell |
|
|
What is this? What is the histologic feature? cancer risk?
|
villous adenomatous polyp
- increased risk for cancer - finger like growth - adenomatous type epithelium: nuclear crowding, loss of goblet cells |
|

What is this? cancer risk?
|
sessile villous adenoma
- high risk for cancer |
|
|
What features of adenomatous polyp confer higher risk?
|
- larger size
- sessile villous type - severe dysplasia |
|
|
Genetic mechanism of FAP.
|
AD, chromosome 5
- APC(tumor suppressor) bind B-catenin and E-cadherin -> B-catenin bind to transcription of T cell factor or lymphoif enhacer factors (TCF-LEF) -> inhibition of apoptosis and increased proliferation |
|
|
Genetic mechanism of HNPCC.
|
4 gene mutations
- MSH2: missmatch repair gene - MLH1 - PMS1 - microsatellite instability - PMS2 |
|
|
Name some genes other than those in FAP and HNPCC that participate in colon cancer pathogenesis.
|
- K-ras
- DCC at chromosome 18 - p53 |
|
|
Risk factors for colon carcinoma.
|
- lower fiber
- red meat - decreased micronutrients - refined carbs - excess calories |
|
|
What age group has the peak incidence of colon cancer?
|
60-79
|
|
|
Rank the following sites of colon cancer from most common to least common.
- ascending colon - transverse colon - sigmoid colon |
- ascending
- sigmoid - transverse |
|
|
Is this more likely to be in the right or left side of the colon?
- polypoid, exophytic - rarely obstruct - pol |
right
- more fluid |
|
|
Is this more likely to be in the right or left side of the colon?
- annular obstructive lesions |
left
|
|
|
T/F: Mucin producing colonic adenicarcinomas have better prognosis.
|
F. They have poorer prognosis
|
|
|
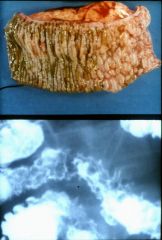
What does this person have?
- Fe deficiency - older male - "apple core" sign on barium xray |
GI carcinoma until proven otherwise
|
|
What is this disease?
- bloody stool - bowel obstruction - fe deficiency |
colonic adenocarcinoma
|
|
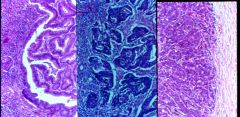
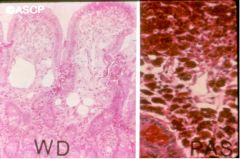
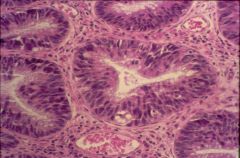
Describe the different degrees of differentiation of adenocarcinoma of colon.
|
- left: well differentiated
- middle: moderately differentiated - right: high grade solid growth |
|
|
TNM staging:
N1 |
1-3 regional lymph node
|
|
|
TNM staging:
M1 |
distant metastases
|
|
|
TNM staging:
T3 |
through muscular wall
|
|
|
TNM staging:
T4 |
invades other organs
|
|
|
TNM staging:
T2 |
into muscular wall
|
|
|
TNM staging:
T1 |
submucosa
|
|
|
Foregut, midgut or hindgut?
- esophagus - stomach - duodenum |
foregut
|
|
|
Foregut, midgut or hindgut?
- mid-duodenum to splenic flexure |
midgut
|
|
|
Foregut, midgut or hindgut?
- splenic flexure to anus |
hindgut
|
|
|
Rank the following from high to low incidence of carcinoid tumor.
- stomach - ileum - appendix - colon - rectum |
appendix
ileum rectum stomach colon |
|
|
What disease is this?
- intact mucosa - desmoplasia (buckled wall) - cause obstruction - secrete gastrin |
carconoid tumor
- Zollinger-Ellison syndrome |
|
|
What disease is this?
- intact mucosa - desmoplasia (buckled wall) - cause obstruction - secrete ACTH |
carcinoid tumor
- cushing syndrome |
|
|
What disease is this?
- intact mucosa - desmoplasia (buckled wall) - cause obstruction - secrete VIP |
carcinoid tumor
- VIPomas |
|

What is this disease? What would you see microscopically?
|
carcinoid - kink
- invading muscularis propria - monomorphic nuclei "salt and pepper" look |
|
What is this disease?
- intact mucosa - desmplasia |
carcinoid tumor
- monomorphic nuclei "salt and pepper" look |
|
|
What is this disease?
- vasomotor symptoms - intestinal hypermotility - bronchoconstriction |
carcinoid syndrome
- sx due to 5HT - fibrosis: heart valves, endocardium, retroperitoneum, pelvis |
|
|
How does GI carcinoid tumor produce carcinoid syndrome?
|
has to mestastaize to the liver
|
|
|
What is this disease?
- fibrosis in heart valves, retroperitoneum - intestinal hypermotility |
carcinoid syndrome
|
|
|
What is the cause of western type GI lymphoma?
|
t (11,18)
- stomach > small intestine > proximal colon |
|
|
What type of GI lymphoma is common in mediterranean population?
|
IPSID (immunoproliferative small-intestinal disease)
|
|
|
What type of GI lymphoma does sprue cause?
|
EATL (enteropathy-associated T cell lymphoma)
|
|
|
Name a mesenchymal tumor of the intestines.
|
GIST (gastrointestinal stromal tumor)
- c-kit (CD117) expression for therapy |
|
|
What gene expression is helpful in therapy for GIST?
|
c-kit (CD117) expression
|
|
|
What are some carcinomas of the anal canal?
|
- adenocarcinoma: rectal extension
- squamous cell carcinoma: HPV |
|
|
What is this disease?
- periumbilical/RUQ pain - nasea, vomit - abdominal tenderness - fever - leukocytosis: lymphocytes in muscularis |
acute appendicitis
|
|
What is this disease?
|
mucocele of the appendix
- hyperplasia - mucinous cystadenomas - mucinous cystadenocarcinoma |
|
|
What is this disease?
- gelly belly: mucin accumulation in abdominal cavity |
pseudomyxoma peritonei
|
|

What is this disease?
- brown bowel |
melanosis coli
- laxative abuser |
|
|
What is this disease?
- mucin producing tumor - omentum is also involved - women often also have ovarian cancer |
appendiceal carcinoma
|
|
|
Which is more common, primary or secondary peritoneal tumor?
|
secondary
- penetration of primary tumor - peritoneal seeding: primary carcinomas of ovary |
|
|
What are some primary peritoneal tumors?
|
- mesotheliomas (asbestos)
- surface serous carcinoma (similar to ovarian cancer) - desmoplastic small round cell tumor |
|
|
What is this disease of the peritoneum?
- dense fibrous overgrowth - inflammatory origin - encases normal structures |
sclerosing retroperitonitis
|

