![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
86 Cards in this Set
- Front
- Back
|
Define the following terms:
1) Caries 2) Calculus 3) Sialadenitis 4) Sialolithiasis |
1) Tooth decay (Streptococcus mutans - produces acid from sucrose fermentation - acid erodes enamel).
2) Mineralized bacterial plaque that deposits around the teeth. 3) Inflammation of salivary gland - traumatic, viral, bacterial, or autoimmune origin. Normally secondary to calculus which obstructs salivary duct. 4) Salivary duct obstruction. |
|
|
Child presents with a gray pseudomembrane on the posterior pharynx. Why would it be dangerous to scrape the lesion?
|
This presentation is characteristic of diphtheria (Corynebacterium diphtheriae) a gram positive rod. It releases an exotoxin which has a an A unit which inhibits mRNA and a B unit which helps the bacteria penetrate myocardial (A-V block) and neuronal tissue (nerve palsies).
|
|
|
Patient presents with red, swollen tonsils and pharynx, purulent exudates on tonsils, a fever, and swollen lymph nodes. Culture reveals a gram positive bacteria and further test reveal its catalase negative. What is the most probably bacteria?
|
Streptococcus pyogenes.
|
|
|
What is the most common cause of sialadenitis?
|
Staphylococcus aureus.
|
|
|
A patient has the following findings: saddle nose, saber shins, Hutchinson’s teeth, and Mulberry molars. What caused these late-onset findings?
|
Congential syphilis.
Saber shin - malformation of the tibia. Hutchinson's teeth - small, wide spaced incisors. Saddle nose - destruction of cartilage. Mulberry molars - molars resemble mulberries. |
|
|
What are the oral manifestations of AIDS?
|
Candidiasis - most common.
Apthous ulcer (canker sour) - painful ulcers covered by shaggy gray membrane. Hairy leukoplakia - glossitis due to EBV. Kaposi sarcoma - on hard palate, due to HHV8. |
|
|
Patient presents with bilateral parotiditis and increased serum amylase. You discover the child was never vaccinated as a child. What are some complications of this virus?
|
Paramyxo family: mumps.
Complications include: meningoencephalitis, unilateral orchitis, pancreatitis. |
|

|
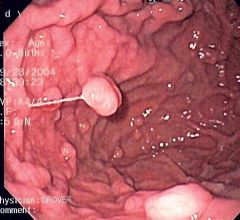
Actinomyces israelii (gram positive). This picture shows a draining sinus tract. These lesions are normally preceded by an abscessed tooth.
|
|

|
Herpangina (Coxsackie A).
|
|
|
What causes herpangina and how does it present?
|
Coxsackievirus A. Occurs in children and manifests as multiple vesicles or ulcers on soft palate and pharynx surrounded by erythema. + Fever and soar throat.
|
|
|
What is Behcet's syndrome?
|
Autoimmune disease with recurrent aphthous ulcer (canker sore), genital ulceration, uveitis, and conjuctivitis.
|
|
|
What percentage of exudative tonsilitis is group A beta hemolytic strep and what percentage are viral?
|
Group A beta hemolytic: 30%
Virus (adenovirus, EBV, etc): 70% |
|

What is the first step in management of this patient?
|
This is leukoplakia (doesn't scrape off). Do a biopsy to rule out squamous dysplasia or cancer.
|
|
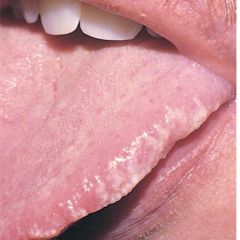
What causes this lesion? Is it an AIDS defining lesion?
|
Hairy leukoplakia is caused by EBV. It is a pre-AIDS-defining lesion.
|
|

What are the risk factors for this lesion?
|
Squamous cell carcinoma (invasive) - color changes and shift in the midline. RF: male, smoking, tobacco, EtOH, HPV.
|
|
|
Name the causes of macroglossia.
Name the causes of glossitis (inflammation). |
1) Primary hypothyroidism, Down syndrome, acromegaly, amyloidosis, multiple endocrine neoplasia syndrome.
2) Iron deficiency (Plummer-Vincent syndrome), B12 or folate deficiency, scurvy, scarlet fever, EBV. |
|
|
What is the most common tumor in the oral cavity (not from salivary gland origin)?
|
Squamous papilloma - exophytic growth (outward) with fibrovascular core.
Other tumor: ameloblastoma - arise from enamel organ epithelium or dentigerous cyst. |
|
|
Hyperpigmentation of the buccal mucosa could be due to what?
|
Peutz-Jeghers, Addison's disease (ACTH stimulates melanocytes), Pb poisoning.
|
|
|
Name three salivary gland tumors. Which one is the most invasive?
|
1) Pleomorphic adenoma (mixed tumor): two different types of tissue from the same cell layer. Most common salivary tumor. F > M. Parotid - most common site. Painless, moveable mass at the angle of the jaw.
2) Warthin's tumor - benign parotid gland tumor. M > F. Heterotropic salivary gland tissue in lymph node. 3) Mucoepidermoid carcinoma - most common malignant salivary gland tumor. |
|
|
What is the clinical significance of dysphagia for solids, dysphagia for liquids/solids, and odynophagia?
|
For solids: symptoms of obstruction - cancer, esophageal web (Plummer-Vincent), stricture.
For solids/liquids: motility disorder. Upper esophagus (striated muscle) - dermatomyositis, myasthenia gravis, stroke. Lower esophagus (smooth muscle) - systemic sclerosis, CREST, achalasia. Odynophagia: painful swallowing - Candida esophagitis (AIDS defining). |
|
|
Pregnant mother has polyhydramnios (excess amniotic fluid). What is the differential diagnosis?
|
Tracheoesophageal (TE) fistula - blindly ending esophagus. Distal esophagus arises from the trachea.
Down's syndrome: duodenal atresia. |
|
|
What is VATER syndrome?
|
Vertebral abnormalities.
Anal atresia. TE fistula. Renal disease and absent radius. |
|
What muscle is weakened, causing this presentation?
|
Zenker's diverticulum: cricopharyngeus muscle. Painful swallowing, halitosis (entrapped food), diverticulitis.
|
|
|
Describe the difference between a true and false diverticulum.
|
True: outpouching lined by mucosa, submucosa, muscularis propria, and adventitia.
False: weakness in underlying muscle wall; outpouching of mucosa and submucosa. |
|
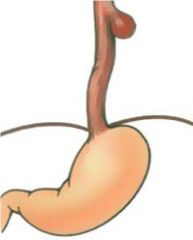
What are the clinical manifestations of this condition?
|
Sliding hernia (95% of hiatus hernias). Herniation of proximal stomach. Heartburn, nocturnal epigastric reflux, hematemesis, ulceration, stricture.
|
|
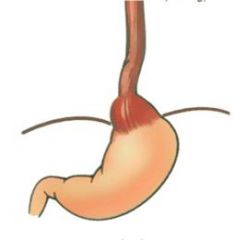
What hormone is reduced in this condition?
|
This is achalasia. Pathogenesis: incomplete relaxation of LES due to absent ganglion cells in myenteric plexus - decreased contraction and loss of vasoactive peptide (VIP) which relaxes the LES. Acquired cause: Chaga's (trypanosoma cruzi).
|
|

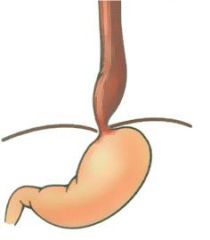
What is this?
|
Paraesophageal hernia.
|
|
|
What is the histological changes in Barret's esophagus?
|
This is a complication of GERD. Glandular metaplasia in distal esophagus due to acid injury: gastric-type columnar cells and small intestine-type cells (goblet cells) replace squamous cell. Glandular dysplasia is associated with an increase in adenocarcinoma.
|
|
|
What is the difference between Mallory-Weiss syndrome and Boerhaave's syndrome?
|
MW: mucosal tear in the proximal stomach and distal esophagus due to retching (EtOH or bulimmia).
Boerhaave's: rupture of the distal esophagus due to endoscopy, retching, bulimia. Air enters pleural cavity - crunching sound on physical exam (Hamman's crunch). |
|

What causes this esophageal pathology?
|
Cirrhosis leading to portal hypertension. Dilated left gastric vein.
|
|
|
Black American, male, smoker, and chronic alcoholic has dysphagia for solids. Most likely diagnosis?
|
Squamous cell carcinoma.
|
|
|
4 week old presents with projectile vomiting of non-bile stained fluid. On exam, you can palpate a mass in the epigastrium. Diagnosis?
|
Congenital pyloric stenosis.
|
|
|
Newborn presents with bile-stained vomit and double bubble sign: air trapped in the stomach and proximal duodenum.
|
Duodenal atresia in Down.
|
|
|
What are some differences between acute gastritis and chronic gastritis?
|
Acute gastritis: multiple erosions (mucosal layer only); most often due to NSAIDS (other: CMV, alcohol, smoking); hematemesis, melena, iron deficiency
Chronic gastritis: pernicious anemia, H. pylori, or autoimmune; chronic inflammatory infiltrate in LP; metaplasia from glandular to columnar; risk for adenocarcinoma |
|
|
Where does type A chronic atrophic gastritis occur?
Where does type B chronic atrophic gastritis occur? |
1) Involves the body and fundus; most commonly due to pernicious anemia.
2) Involves the antrum and pylorus; most commonly due to Helicobacter pylori. |
|
|
What are the diseases associated with H. pylori?
What does H. pylori secrete that damages the mucosa? |
1) Duodenal (90%) and gastric (80%) ulcers, type B chronic atrophic gastritis, gastric adenocarcinoma, and low grade B-cell malignant lymphoma.
2) Urease (AA to ammonia), proteases, cytotoxins |
|
|
Stressed out businessman has severe epigastric pain that radiates to the shoulder. Play odds, diagnosis?
|
Perforation of a duodenal ulcer allows air to collect under diaphragm. Irritated (phrenic) fourth nerve, referred pain to the shoulder.
|
|
|
What are the four layers of a histologic section of an ulcer in PUD? Are the ulcers in PUD malignant?
|
PUD is caused by H. pylori. Ulcers are clean and sharply demarcated. Layers: necrotic debris, inflammation with PMN, granulation tissue, fibrosis. A small percentage of gastric ulcers are malignant, duodenal ulcers are never malignant.
|
|
|
What is Zollinger-Ellison syndrome? How will the BAO, MAO, and BAO/MAO ratio change? Why does a patient with this syndrome have malabsorption?
|
Malignant islet cell tumor secreting gastrin producing hyperacidity. MEN I association in 20-30%.
BAO, MAO, and BAO/MAO increase. High gastrin levels interfere with pancreatic enzyme activity causing malabsorption. |
|
Patient is on omeprazole. What is this lesion?
|
Gastric polyp. Causes: chronic gastritis and achlorhydria. Types: hyperplastic polyp (hamaratoma - not malignant) and adenomatous polyp (neoplastic).
|
|
|
What is the most common benign tumor in the gastrointestinal tract?
What is the most common gastric carcinoma and what are the risk factors? |
Leiomyoma.
Intestinal gastric adenocarcinoma. RF: H. pylori, nitrosamines, smoked foods (Japan), diets lacking fruits/vegetables, type A chronic atrophic gastricis, Menetrier's disease (hyperplasia of mucus secreting cells). Other carcinoma: diffuse type adenocarcinoma, primary gastric malignant lymphoma. |
|
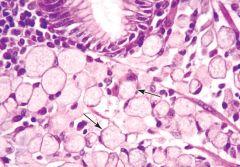
What is shown in this section form the stomach wall?
|
Diffuse type of gastric adenocarcinoma. The arrow shows signet-ring cells. This cancer produces Krukenberg tumors of the ovaries (via hematogenous spread).
|
|
|
Female presents with weight loss and epigastric pain with vomiting. Examination reveals an enlarged left supraclavicular node and acanthosis nigricans. What other paraneoplastic syndrome may be present with the cancer your patient has? What is Sister Mary Joseph sign?
|
Leser-Trelat sign: multiple outcropping of seborrheic keratoses.
Sister Mary Joseph: metastasis to umbilicus. |
|
|
Give a differential for hematemesis due to an esophagus pathology?
|
Cancer, esophageal varices, Mallory-Weis, hiatal hernia.
|
|
|
What are the four types of stimuli for abdominal pain?
What are the three categories of abdominal pain? |
Stretching/tension, inflammation, ischemia, or neoplasm.
Visceral pain: dull and poorly localized (begins at midline). Parietal pain: intense and localized more precisely to the site of the lesion. Referred pain: remotes site of pain is supplied by the same neurosegment as the involved organ. |
|
|
What abdominal pathologies lead to the follow degrees of pain:
1) Explosive and excruciating (immediate) 2) Rapid, severe, and constant (minutes) 3) Gradual and steady pain (hours) 4) Intermittent and colicky |
1) Perforated ulcer, biliary or renal colic, ruptured aneurysm, MI
2) Acute pancreatitis, complete bowel obstruction, mesenteric thrombus 3) Acute cholecystitis, diverticulitis, acute appendicitis 4) Early subacute pancreatitis, mechanical small bowel obstruction |
|
|
Name the categories of diarrhea (diarrhea).
|
Goljan: invasive, secretory, osmotic, and malabsorptive.
UQ/Robins: malabsorptive, osmotic, dismotility, exudative/inflammatory, secretory |
|
|
Invasive diarrhea is characterized by low-volume, blood and leukocytes (dysentery). Name all the pathogens that cause dysentery.
|
US bacteria (most-least common): Campylobacter jejuni, Salmonella typhi, Shigella dysenteriae, enterohemorrhagic Escherichia coli, Yersinia enterocolita.
Amebiasis (Entomeba histolytica). |
|
|
What two test are used to determine if diarrhea is invasive, secretory, or osmotic?
|
Fecal smear for leukocytes: positive = invasive.
Stool osmotic gap: 300 mOsm/kg (represents normal plasma Osm) - 2 x (random stool Na + random stool K). Less than 50 = secretory, greater than 100 = osmotic. |
|
|
What organism(s) have a heat-stable toxin that causes a secretory diarrhea? What is the mechanism?
|
ETEC and Vibrio Chlorea: neither are invasive.
HS toxin (an exotoxin) activates the Gs-protein which stimulates adenylate cyclase and increases cAMP which inhibits reabsorption of Na/Cl and stimulates the secretion of Cl and HCO3. |
|
|
What type of diarrhea is caused by the carcinoid syndrome?
|
Carcinoid syndrome is caused by carcinoid tumors of the GI tract that are neuroendocrine in origin and release 5-HT (serotonin). Serotonin increases gut motility and causes a secretory diarrhea.
|
|
|
What type of diarrhea does lactose deficiency cause?
|
Osmotic. Lack of the disaccharidase (lactase) leaves lactose, an osmotically active substance in the gut. Anaerobes in the colon also degrade the lactose into lactic acid and H2 gas leading to abdominal distention with explosive diarrhea.
|
|
|
Several members of a family develop nausea, emesis, and water diarrhea hours after a picnic. They ate rice and ham. What type of bacteria could cause this?
|
Enterotoxin-producing bacteria is considered because the symptoms began soon after ingestion.
Staph. aureus: food poisoning with performed toxin. Bacillus cereus: food poisoning (rice, tacos) with performed toxin |
|
|
Name the bacteria associated with these scenarios that caused diarrhea:
1) S-shaped gram - rod, produces ulcers resembling UC, pt ate chicken 2) Patient ate honey and has mydriasis 3) Undercooked beer, Shiga-like toxin 4) Pt has a pet turtle, triad: bradycardia, neutropenia, splenomegaly |
1) Campylobacter jejuni
2) Clostridium botulinum 3) EHEC 4) Salmonella |
|
|
Your on your honeymoon cruise when 25% of the boat (300) people) are afflicted with acute gastroenteritis, but not everyone ate the same food. What is the causative agent?
|
Most likely the Norwalk-like virus (Calici, ssRNA). High attack rate rules out bacteria (unless everyone ate the same thing).
|
|
|
What diarrhea causing virus infects children? Adults? AIDS pt?
|
Rotavirus - children. Infects and destroys enterocytes.
Norwalk - adults. Cytomegalovirus - AIDS. |
|
|
Your patient has colonic ulcers and bloody diarrhea. Fecal leukocytes are present. You've ruled out all bacterial, viral, and helminth causes. You cannot find any trophozoites with ingested RBCs. What infective pathogen could cause this?
|
Balantidium coli - produces colonic ulcers.
|
|
|
Patient recently camped up in the Taos mountains and developed diarrhea. What should you treat him with?
|
Metronidazole. Most common protozoal cause of diarrhea in the US - Giardia lamblia.
|
|
|
What is the most common cause of hospital-acquired diarrhea?
|
Clostridium difficile infection.
|
|
|
Seth comes down with a fever, bloody diarrhea, and abdominal pain (whats new). He ate tofu last night which was stored in his refrigerator. What infections diarrhea does he have?
|
Yersinia enterocolitis - can survive refrigeration.
|
|
|
What are the causes of malabsorption?
|
Pancreatic insufficiency: pancreatitis (EtOH, CF)
Bile salt deficiency: inadequate production (cirrhosis), bile duct blockage, bacterial overgrowth in small bowel with destruction of bile salts, excess binding of bile salts, terminal ileal disease preventing recycling of bile. Small bowel disease: destruction of villi (e.g. celiac, whipples), lymphatic obstruction (abetalipoproteinemia). |
|
|
What is a D-Xylose screening test?
|
Xylose does not require pancreatic enzymes for adsorption. Lack of reabsorption of oral xylose indicates small bowel disease.
|
|
|
How does celiacs cause malabsorption?
|
Autoimmune disease: Abs against gliadin (a fraction of gluten; gluten is from wheat, rye). Autoimmune (T-cell mediated) destruction of villi in duodenum and jejunum. Glands will be hypertrophied and LP will show chronic inflammation.
|
|
|
What bacteria can cause malabsorption and symptoms including fever, polyarthritis, lymphadenopathy, and increased skin pigmentation?
|
Whipple's disease: Tropheryma whippelii bacilli. Causes villi destruction. PAS-positive macrophages in LP obstruct lymphatics.
|
|
|
What are the two most common causes of small bowel obstruction?
What are the clinical findings in SMO? |
Adhesions: previous surgery
Indirect inguinal hernia: bowel becomes trapped in inguinal canal. Colicky pain, bowel distention. Radiographic finding: air/fluid levels with a step-ladder appearance. |
|
|
How does a gallstone ileus cause bowel obstruction?
|
Occurs in elderly woman with chronic cholecystitis and cholelithiasis. Fistula develops between gallbladder and small bowel.
|
|
|
What is missing in Hirschsprung disease? What portion of the bowel is most affected?
|
Absense of ganglion cell in the submucosal and myenteric plexus due to defective neural crest cell migration. Involves distal sigmoid and rectum.
|
|
|
Patient presents with bloody diarrhea and abdominal pain. Examination reveals an oblong mass palpated in midepigastrium. Diagnosis?
|
Intussusception.
|
|
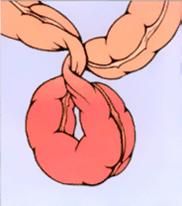
Where does this usually occur in the bowel?
|
Volvulus - producing obstruction and strangulation.
Young adult: cecum. Elderly: sigmoid colon. Risk factors: chronic constipation, pregnancy, laxative abuse. |
|
|
What is the area of weakness in the following hernias? Is obstruction associated?
1) Direct 2) Femoral 3) Indirect 4) Umbilical 5) Ventral |
1) Transversalis in the floor of the triangle of Hesselbach. No obstruction occurs.
2) Femoral canal. Bulge located below inguinal ligament. High rate of incarceration. 3) Failure of a peritoneum to form between inguinal canal and tunica vaginalis. Incarceration or strangulation. 4) Fascial defect. Incarceration is possible. 5) Old surgical incision. |
|
|
What makes up the borders of the triangle of Hesselbach? Femoral triangle?
|
Hesselbach: medial - rectus abdominis, lateral - inferior epigastric artery, inferior - inguinal ligament.
Femoral: superior - inguinal lig, medial - adductur longus, lateral - sartorius. |
|
|
What is the most common cause of mural and mucosal infarcts of the small bowel?
What is the most common cause of transmural (full-thickness hemorrhagic) infarction of the small bowel? |
1) Hypoperfusion states, e.g. shock.
2) Occlusion of SMA - thrombosis or embolism (from atrial fibrillation). |
|
|
Where does ischemic colitis occur?
|
At the splenic flexure of the large bowel which is a watershed area. Atherosclerotic narrowing of SMA or IMA causes mesenteric angina: severe pain.
|
|
|
What is angiodysplasia?
|
Dilation of mucosal and submucosal venules in the cecum and right colon. Occurs in elderly individuals and leads to hematochezia.
|
|

From what does this small bowel malformation arise?
|
Meckel diverticulum is a remnant of the vitelline duct (omphalomesenteric). It is a true diverticulum (all layers of the mucosal wall are dilated). Mnemonic: 2 inches long, 2 feet from the ileocecal valve, 2% of population, and 2% symptomatic.
|
|
|
Where do large bowel diverticulum most often occur and what are the causative factors?
|
Pulsion diverticulum are due to a low-fiber diet with increased constipation. They most often occur in the sigmoid colon. Two factors contribute to their formation: (1) area of weakness in taenia coli where vessels penetrate the muscular propria, (2) Increased intraluminal pressure.
|
|
|
What is the pathogenesis of the pain in irritable bowel syndrome?
|
Intrinsic colonic motility disorder. Clinical features mimic UC, but sigmoidoscopy is normal.
|
|
|
Are these features more common in UC or Crohn's:
1) More common in women 2) Mainly rectum 3) Inflammatory pseudopolyps 4) Mucosal and submucosal (not transmural) inflammation 5) Granulomas in 60% of cases 6) Dysplasia/cancer |
1) Crohn's (also Jews > non-Jews)
2) Ulcerative colitis 3) UC 4) UC 5) Crohn's 6) UC |
|

This picture shows creeping fat and the arrows point to linear ulcers. What is this characteristic of?
|
Crohn's. Linear (aphthous ulcers) have a cobblestone appearance.
|
|
|
What is the most common small bowel malignancy and where does it normally occurs?
|
Carcinoid tumor (neuroendocrine tumor) - metastatic potential correlates with size and depth. Locations: appendix and terminal ileum. Terminal ileum commonly metastasizes to liver.
|
|
|
Explain when a carcinoid tumor would create a carcinoid syndrome.
|
The tumor must metastasize to the liver, else the serotonin secretions (5-HIAA) will be delivered to the liver, metabolized, and excreted in the urine.
|
|
|
What are the clinical findings due to serotonin?
|
Flushing of the skin, secretory diarrhea, tricuspid regurgitation and pulmonary stenosis.
|
|
|
Non-neoplastic (hamartomatous) polyps have no malignant potential. Name all the types of non-neoplastic polyps.
|
Hyperplastic polyp: adults, sigmoid colon.
Juvenile: children, rectum Peutz-Jeghers polyposis: AD, small bowel. |
|
|
Neoplastic polyps (adenomas) increase with age. Name the three types.
|
Tubular adenoma: most common, stalked
Tubulovillous adenoma: Villous adenoma: greatest risk for cancer |
|
|
What are the risk factors for malignancy potential of adenoma?
|
Larger than 2 cm.
Multiple polyps. Increased villous component. |
|
|
Patient has a condition that has almost a 100% chance of developing colon cancer. What is the inheritance of this condition?
|
Familial polyposis: AD.
|

