![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
79 Cards in this Set
- Front
- Back
What is the name of the capsule on the liver?
What is the porta hepatis? How big is the liver? |
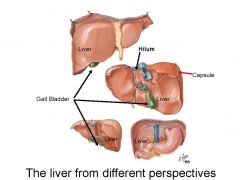
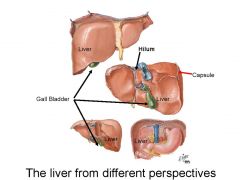
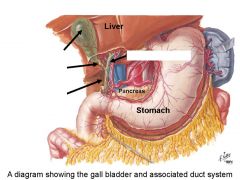
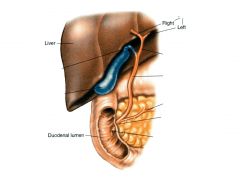
1. Location - the liver is a large, reddish, lobed structure located in the upper abdominal quadrants just beneath the diaphragm. Note the gallbladder and pancreas too.
2. It is the largest gland in the body (1.5 kg). 3. Description o right and left lobes. 4 LOBES TOTAL o The porta hepatis (hilum) is the site for the entry or exit of hepatic portal vein, hepatic artery, bile duct, lymphatic vessels & nodes, and autonomic nerves. 4. Surface is covered by a thin connective tissue capsule (Glisson’s capsule). |
|
Describe the blood supply to the liver.
What % of cardiac output does it get? |
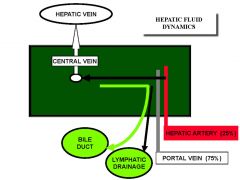
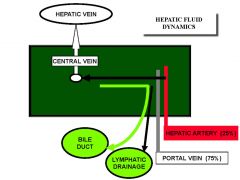
1. BLOOD SUPPLY. The liver has a dual blood supply (i.e. systemic and portal). The liver is a highly perfused organ, receiving about 25% of the total cardiac output.
a). Portal Vein (75% of hepatic blood) supply) - oxygen-poor blood; rich in digestive products from the intestines (but not chylomicrons which bypass the liver via intestinal lymphatics!) via the Superior Mesenteric Vein, and hemoglobin breakdown products from the spleen via the Splenic Vein and from the pancreas (the venous blood in the Pancreatic Vein contains endocrine hormones). (PORTAL BLOOD means its going from one capillary plexus to another (the 2nd being in the liver). Most of the blood going to the liver is coming from the GI tract. The products of digestion are being back from the GI to the liver to be processed. Also blood from the pancreas and the spleen coming here.) The Portal Vein divides into left and right hepatic branches that enter the hepatic sinusoids. There are abundant vascular intercommunications at the sinusoidal level. b). Hepatic Artery (supplies about 25% of the hepatic blood supply). Oxygen rich blood. -The portal and well oxygenated blood are all mixed together and go into the liver itself and drain through the parencyma cells into the central vein and out from the liver. c). Hepatic Vein – Central Vein. Most of the hepatic venous blood drains to the three major hepatic veins – the right, middle and left. Each has short extrahepatic segment before joining the inferior vena cava. Note: -The liver is also producing a lot of lymphatic material that is rich in plasma protein -Also produces bile (stored in gallbladder) |
|
What the the major components of this unit?
How much bile does the liver produce? Recycle? |
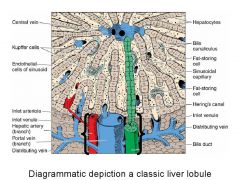
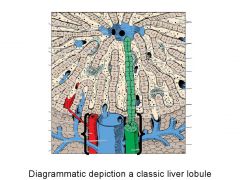
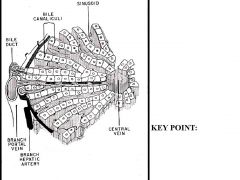
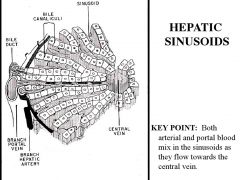
***IMPORTANT***
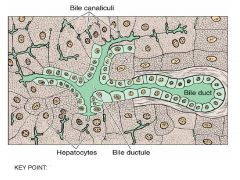
• MAJOR COMPONENTS (Figure 4): 1. Portal Triad (hepatic artery, portal vein, bile duct. At periphery of lobule) 2. Central Vein 3. Hepatic Plates 4. Sinusoids Blue is branch of hepatic portal vein - bringing everything back from GI and spleen etc -blood goes through sinusoids (capillaries, lets things go through) -goes through sinusoids to central vein liver is producing bile which goes through canaliculi (green). 10% made 90% recycled. the 10% made goes opposite blood flow out to periphery. Kupffer cells: phagocytic cells arising from monocytes in the blood and only become obvious when they're active Have fat storing cells as well Red branch of hepatic portal artery |
|
|
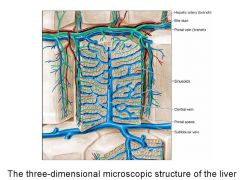
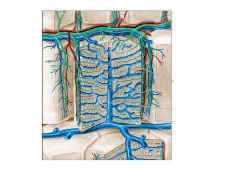
Schematic
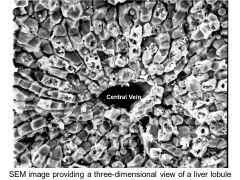
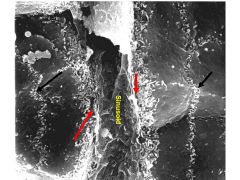
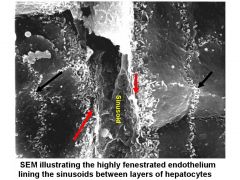
3d microscopic structure of the liver Note portal vein coming in, the branch of hepatic artery, bile duct leaving, they all go through and drain through TRUE SINUSOIDS (true sinusoids - highly fenestrated) and then drain through plates that are 1-2 cells thick - plates of liver cells. Liver cells are called hepatocytes. Then it goes to the central vein and drains by the sublobular vein. This is a liver lobule. Liver composed of 4 lobes but then broken down by connective tissue sepate into lobules |
|

|

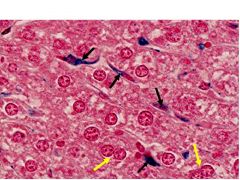
LOBULES are the basic functional unit of the liver **
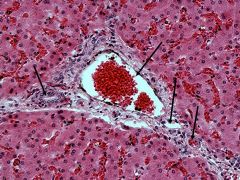
-In center is a lobule. Cells have hexagonal shape At corners of lobule is where you find the tirad (black arrow) The dark red material is the blood from the sinusoids Yellow points to central vein -arteries demarcated by connective tissue septae |
|
When does the liver produce bile?
How much does it produce per day? Where does the biliary system begin? How does the bile get to its final destination? What is the function of bile? |
BILIARY SYSTEM. The liver produces bile continuously (600-1200ml per day) and is carried by
the biliary tract system to the duodenum. • The biliary system begins at the hepatocyte parenchymal cell level. Portions of the plasmalemmma (cell membrane) of the hepatocyte are indented to form small channels called bile canaliculi between hepatocytes. Tight junctions produce impermeable seals. The intralobular bile canaliculi carry bile to the periphery of the lobule. • At the periphery of the lobule the canaliculi converge to form canals of Hering at the periphery of the lobules. They traverse the limiting plate and enter small terminal ductules. These terminal ductules are lined by cuboidal epithelium. The ductules enter larger ducts in the interlobular septum. • This duct system follows the segmental anatomy of the vascular supply (in the reverse direction) to enter the bile ducts in the portal triad, then to larger ducts which supply the gall bladder. • Bile functions: bile salts secreted into the intestine emulsify dietary fats in the intestines and facilitate digestion. Certain metabolic products (e.g. the hemoglobin breakdown product called bilirubin which gives bile a yellow color) and excess cholesterol. |
|
|
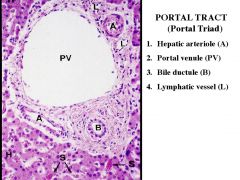
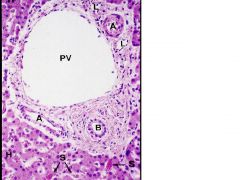
If you were to look at triad at high magnification:
Triad means 3 structures: 1. hepatic arteriole 2. Portal venule 3. bile duct 4. Lymphatic vessel -->liver is making lots of lymph PV = portal vein A=arteriole (note muscle) B=Bile duct Vessels are lined by thin squameous epithelium, but BD is lined by cuboidal cells. L=Lymphatic. How do you tell? There are no RBCs, only lymphocytes Connective tissue all around |
|
|

Another example of portal triad
Branch of hepatic portal vein --> thin lining epithelium RBCs in lumen Note branch of hepatic arteriole with RBCs in lumen. Also endothelium around and smooth muscle around that Lymphatics are thin walled structure Bile duct lined by CUBODIAL CELLS Hepatocytes are the light pink with RBCs in it (red) in the sinusoids Some hepatocytes have 1 nuclus some have 2. Liver has great ability to regenerate |
|
|
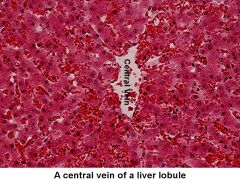
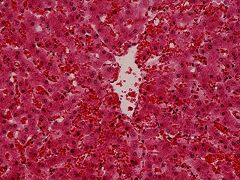
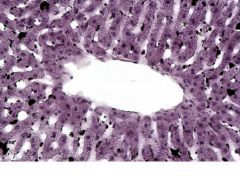
This is the center of a lobule
Note central vein The larger cells w/ purple nuclei are hepatocytes |
|
|
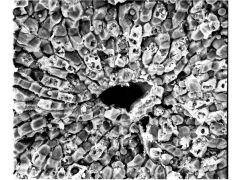
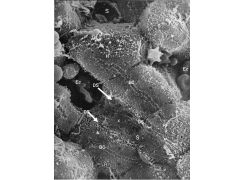
Can see all the liver cells and the spaces between
|
|
|
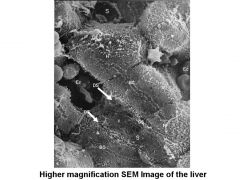
"classic image"
Sinusoid on other side RBC looks like star Can see how fenestrated the sinusoid is. Hepatocytes on bottom? Reticular fibers NOTE bile cannulucus between adjacent liver cells (BC) Bile is coming OUT while blood is going in. THe space between the lining endothelium and hepatocyte = DS = space of Disse. This is where exchange takes place between blood and hepatocyte Hepatic sinusoids include: (a). Sinusoidal capillaries lined with discontinuous endothelium (no basal lamina, just reticular fiber support); carries blood towards central vein (see Figure 10A) (b) The space of Disse – subsinusoidal. bathes hepatocytes with sinusoidal plasma and initiates lymph formation). See Figure 10B. (c). Cells within sinusoids: |
|
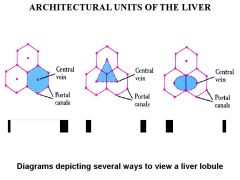
What the the different ways to look at a liver lobule?
|
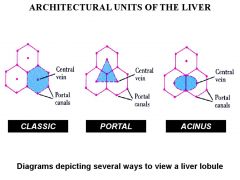
1. Classic Hepatic Lobule - the point of focus is the central vein (blood flow perspective). Corners are formed by each of the portal triads. The outer boundary is set by a limiting plate of hepatocytes
*this is the way we've been looking at it 2. Portal Lobule - the point of focus is the portal triad (bile/lymph flow perspective) 3. Hepatic Acinus (important concept from a PATHOLOGIST’s perspective). The points of focus are the distribution of branches of blood vessels in the portal along the connective tissue framework of the interlobular septum (especially terminal branches of hepatic artery and portal vein). Follows the blood flow along sinusoids to the central veins and the bile flow from hepatocytes to the bile duct. The variable proximity of hepatocytes to the vascular backbone results in hepatocellular heterogeneity and the identification of three zones. Note: many hepatic injuries, and hepatocellular function exhibit zonal distribution patterns |
|
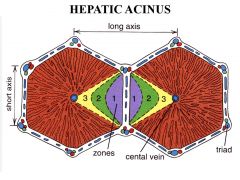
Describe the 3 zones
|
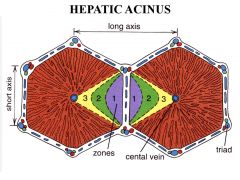
Three zones of the Rappaport Acinus Live Lobule:
Zone 1 (periportal) - closest to distributing vessels; maximum availability of oxygen and nutrients; will survive insults better and regenerate faster. Zone 2 (midzonal) - intermediate. Zone 3 (centrilobular) - furthermost from distributing vessels (i.e. closest to central vein); lowest availability of oxygen and nutrients; often the first to die. *These zones respond differently to different insults. Zone 3 is most responsive to ISCHEMIC insults and Zone 1 is most responsive to TOXIC insults (think about it in terms of blood flow and exposure) |
|
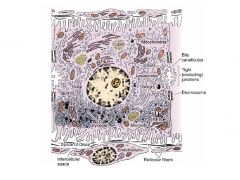
Describe the microscopic structure of hepatocytes (nuclus, cytoplasm, plasma membrane, RER, SER, Golgi, Peroxisomes).
How big are hepatocytes? |
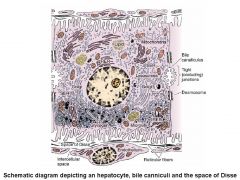
-This is the 2nd most important slide..
- This is a liver cell/hepatocyte! -If there is one cell that has everything in it, it's liver. RER, SER, perioxisomes, etc. -The lumen of the sinusoid is at the bottom lined by endothelial cells -NO basal lamina -On the right is where the synthesized bile goes --> canaliculi. They are bounded on either side by tight junctions Hepatocytes are Large polyhedral parenchymal cells. Size: 20-30 microns. Nuclei – one or two nucleoli. Some of the nuclei are larger with polyploid chromosome numbers. Cytoplasm - eosinophilic cytoplasm with abundant mitochondria) which may appear foamy (glycogen or fat storage). Plasma membrane – o the sinusoidal face has numerous microvilli extending into the space of Disse – increases surface area X6. **this is where exchange takes place o between hepatocytes there are tight and gap junctions between neighboring cells. Bile canaliculi are formed by indentations of plasma membrane. They are sealed by tight junctions of the membrane. o Desmosomes hold the cells together Rough Endoplasmic Reticulum produces plasma proteins such as albumin, clotting factors, lipoproteins. Smooth endoplasmic Reticulum ER - bilirubin conjugation, bile salt synthesis, detoxification. Golgi - packages proteins for release into space of Disse. Peroxisomes – contain oxidases & catalases. Microvilli extend into space of Disse and increase absorptive surface markedly |
|

|
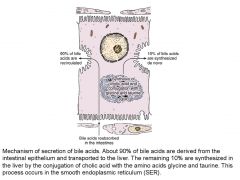
-This summarizes the mechanism of bile secretion
-Read slide -You have bile being made, going into bile cannaculi |
|

|
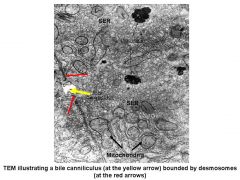
-This is TEM of bile cannaculus
Have desmosomes (red) on either side Yellow is cannacului HAD ANOTHER IMAGE OF HEPATOCYTE. |
|

|
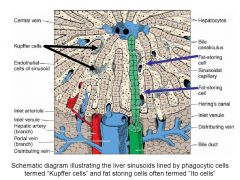
-Kupffer cells: phagocytic cells derived from monocytes in blood line the sinusoids of liver
Fat storing cells (another name) |
|
|

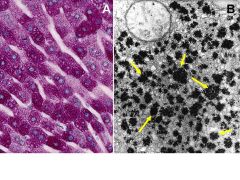
-Looking at glycogen in the liver.
-On left is light microscope. Round blue dots are nuclei. -If you were to starve someone glycogen would be gone in a day or so |
|
|
|
|
|
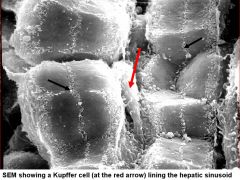
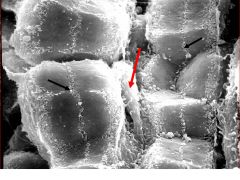
-Can see kupffer cells at red arrow
on either side are the hepatocytes. Black arrow = bile canalaculi Kupffer Cells. -->Resident macrophages. Derived from monocytes. -->Usually located between endothelial cells (incorporated into the lining by the sinusoid ) -->Function - phagocytic, motile for surveillance and response. |
|
|
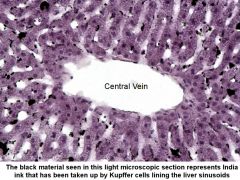
-Ink was taken up especially by Kupffer cells
|
|
|
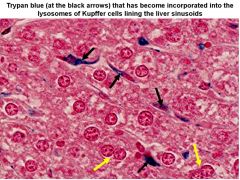
Kupffer cells have taken up dye
Note at yellow arrows that some hepatocytes are binucleated Kupffer cells at black arrow. The dye is in the cell's lysosomes |
|
|
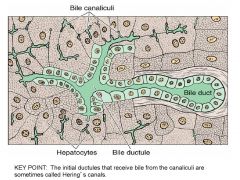
-Bile canaliculi:
as you go to periphery of lobule, they become lined by cubodial cells that are continuous with the cells that line the bile duct. These regions are called the canals of Hering |
|
|
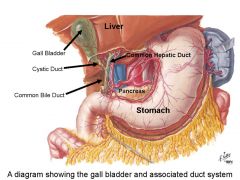
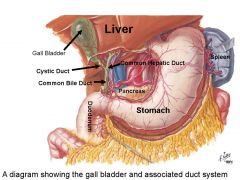
-The liver produces a lot of bile
-Have R and L heptatic duct -Bile is stored in gall bladder -Bile goes both up and down the cystic duct -Exits via common bile duct |
|
|
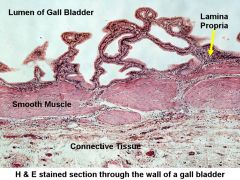
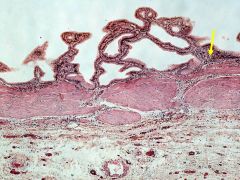
-Lining mucosa is HIGHLY FOLDED *characteristic
-Has smooth muscle that can contract -Connective tissue -- side that is embedded in liver -Gall bladder can hold ~50ml of bile -stores and concentrates |
|
|
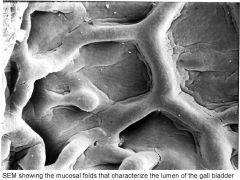
Folds in gallbladder
|
|
|

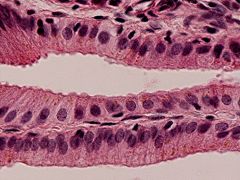
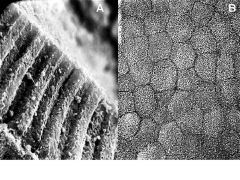
Simple columnar epithelium lining gall bladder
|
|
|
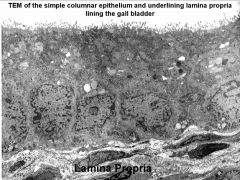
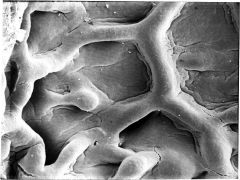
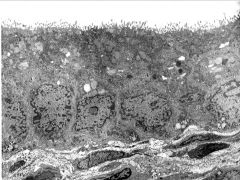
Surface has microvilli associated with fact that these cells concentrate the bile up to FIVE TIMES. Reabsorption of water takes place here.
|
|
|
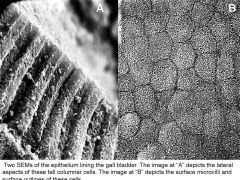
On left are cells lining the gall bladder
On right can see cells, note hexagonal/pentagonal pattern. Remember that this is how lobules are shaped as well |
|
|
|
|
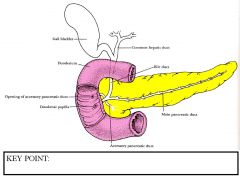
Describe the main pancreatic duct.
|
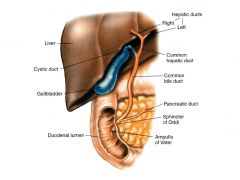
R/L hepatic duct coming down from common hepatic duct into 1st portion of duodenum after merging with pancreatic duct
There is sphincter (of Oddi) that opens in response to CCK. 1. Main Pancreatic Duct: duct of Wirsung (Figure 7). - composed of fused ducts from the dorsal and ventral anlage. - begins in the tail and continues throughout the length of the organ. - fuses with the common bile duct to form ampulla of Vater at entry to the duodenum. - lined by simple columnar epithelium with goblet cells. |
|
Describe the two components of the pancreas.
|
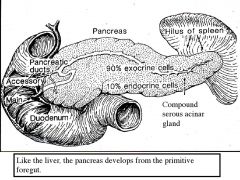
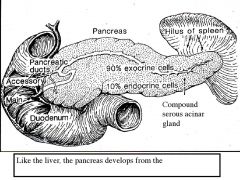
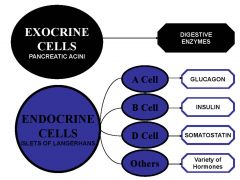
Pancreas is both endocrine (10%) and exocrine (90%)
1. Exocrine component (90%) - synthesis and secretion of digestive enzymes (“pancreatic juices”). The glands produce 2 - 2.5 liters of pancreatic fluid each day. Released into the intestine. 2. Endocrine (10%) - Islets of Langerhans scattered throughout the gland. Secretes hormones into the circulation via the pancreatic vein. Regulate multiple organs. |
|
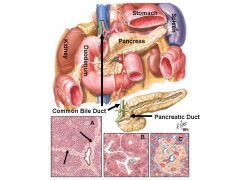
Describe the location of the pancreas
Of the images on the bottom, which one shows the exocrine portion? The endocrine? |
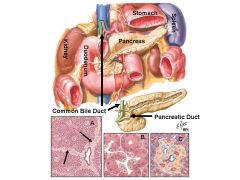
- A long, flat, lobulated organ (pinkish white) with three anatomical regions: head, body and tail.
- Located in the upper abdomen – retroperitoneal. - The head of the pancreas is located in the duodenal concavity and the body and tail of pancreas extend to the hilum of the spleen. Exocrine portion in middle endocrine on right |
|
|
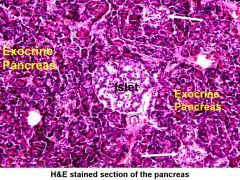
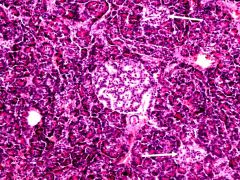
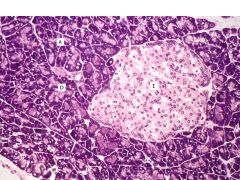
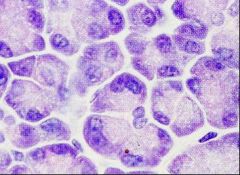
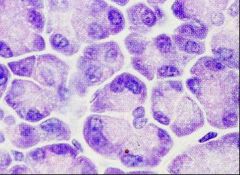
Endocrine -- Islets of langerhan
|
|
|
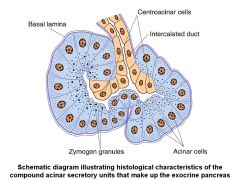
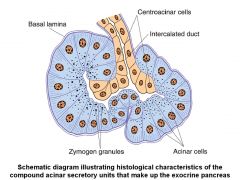
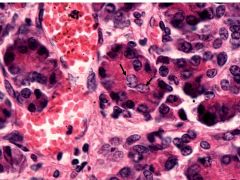
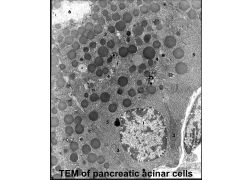
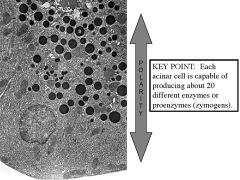
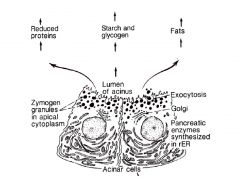
Exocrine pancreas
-These cells are making enzymes that break down fats, carbs and proteins -These cells are really active, full of RER -Apical portion full of zymogen granules, products secreted into lumen -Whole structure is called an acinus -Product exits by way of intercalated ducts -Unique to acini of pancreas is fact that these cells of ducts protrude into lumen of the acinus. the cells that protrude in are the central acinar cells. **characteristic of exocrine pancreas Acini - Composed of a compound acinar glands – serous. - The acini are formed by several pyramidal serous cells. - The serous cells are highly polarized – they exhibit strongly basophilic staining in the base (because of abundant RER) and an acidophilic apex (filled with zymogen granules). - Acinar cells produce, store, and release several proenzymes and enzymes. - Contents secretory granules are secreted by exoytosis. |
|
What are lobules separated by?
How much of the pancreas needs to be damaged before signs of maldigestion occur? |
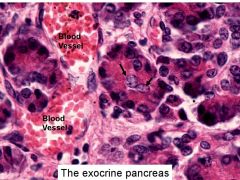
H&H Of acinus
Central acinar cell at black arrow - The lobules separated by fine connective tissue septa. Groups of acini within lobules. Intralobular ducts. Larger ducts in the septa. - There is a very large reserve of exocrine pancreas function; more than 90% of these cells must be damaged before signs of maldigestion occur. |
|
|
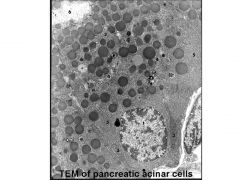
TEM showing lumen of acinus and zymogen granules filled with pancreatic enzymes
Nucleus at bottom surrounded by RER |
|
|
S = storage granules
RER Nucleus |
|
|
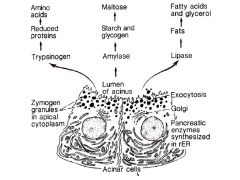
Different kinds of products these cells are producing
|
|
Describe the pancreatic duct(s).
|
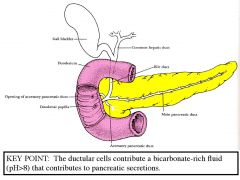
This shows you that what comes from exocrine pancreas goes to pancreatic duct which merges with common bile duct and then goes to duodenum
. Ducts - Begin in acini - The duct system for the pancreas is similar to other lobulated glands. The system includesintercalated, lobular and lobar that supply the major ducts. (a) Centroclinal cells - These are intra-canard ducts – the origin of the intercalated ducts; unique to the pancreas. They appear as pale cells within acini. (b) Intercalated Ducts - lining cells secrete water and bicarbonate ions. Note: the ducts in the pancreas are not striated (vs. salivary gland). The duct lining cells secrete a watery, bicarbonate rich fluid. Stimulated by secretin. |
|
|

Endocrine pancreas is about 10% of this gland. It is composed of islets of langerhans, surrounded by thin connective tissue.
The endocrine pancreas makes lot of endocrine hormones. 1. There are approximately 1 million islets in the human pancreas (most numerous in the tail region). 2. Each islet is a multihormonal endocrine gland and represents a collection of several hundred cells that form cords or clusters around fenestrated capillaries. 3. Because the cells have less RER, islets stand out against the background of the serous exocrine pancreas. 4. Only a delicate reticular capsule separates islets from the surrounding exocrine pancreas. The different cell types in the islets cannot be distinguished using routine H&E staining. Identified by immunofluorescent staining procedures are used to identify them. The relative quantities of the different cell types may vary between islets. Secretory granules are distinctive by EM. |
|
|
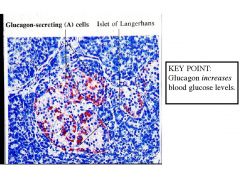
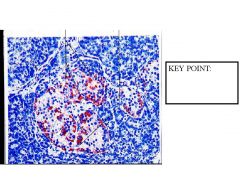
Glucagon is from alpha cells.
~20% produce glucagon Found in periphery of islet |
|
|
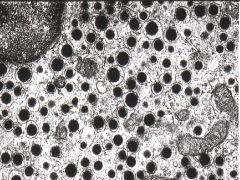
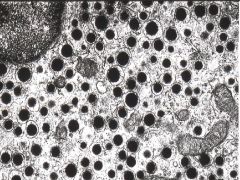
TEM of islet -- storage of glucagon in black dots
|
|

|
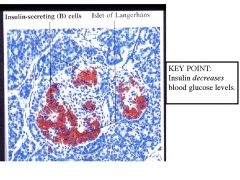
Insulin producing B cells
insulin decreases blood glucose levels while glucagon increases __% are made of B cells |
|
|
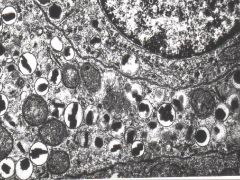
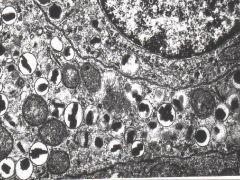
Like alpha cells that have characteristic morphology at EM level, so do B cells
|
|
|
Delta cells -- secrete somatostatin
|
|

|
Other cells make pancreatic polypeptide, which may inhibit the exocrine pancreas
|
|
|
What do the Exocrine cells of pancreas produce?
What do the A, B, C, and D cells (endocrine) of the pancreas produce? |
|
|
|
What does the liver develop from? How does it develop?
|
• The liver, like the pancreas, develops as a glandular outgrowth of the primitive gut endoderm. The floor of the future duodenum gives rise to a sacculation named the hepatic diverticulum. The cranial part becomes the liver parenchyma and bile ducts. The caudal part becomes the gall bladder and cystic duct.
|
|
|
How much lymph does the liver produce ?
Is hepatic lymph the same as lymph made in different sites? How does the lymph produced in the liver get to the lymphatics? |
• The liver produces a large volume of lymph. More lymph than any other organ in the body. Approximately 25-50% of lymph in the thoracic duct comes from the liver. Hepatic lymph is different from lymph from other sites because it is rich in plasma proteins (made in the liver e.g. albumin)
• Plasma escaping from the fenestrations in the sinusoidal endothelium into the space of Disse move in a direction counter to the blood flow in the sinusoids. • At the periphery of the lobules the lymph enters lymphatics that accompany the blood vessels and bile duct in the interlobular septa and portal triads. |
|
|
What is the liver innervated by?
|
INNERVATION. The liver is innervated by mainly autonomic nerves. Present in connective tissue around portal triads, throughout the lobules and apposed to hepatocytes in the space of Disse.
|
|
|
What is an Ito cell?
|
Lipocytes (Ito cell or stellate cell).
• store lipid and vitamin A. |
|

How are hepatocytes arranged?
What is this image of? What % of the liver cell population are hepatocytes? What is the function of hepatocytes? |

(a). Organization – hepatocytes are arranged in Hepatocellular Plates.
They form continuous interconnecting/anastomosing cords of hepatic cells (1 or 2 cells thick), interspersed by the sinusoids. (b). Limiting plate – (image above). Located at th periphery of the lobule. The hepatic cells surround the circumference of the lobule forming a nearly continuous wall of hepatocytes against the interlobular septum. Only tiny branches of the hepatic artery, portal vein, and bile ducts penetrate through via fenestrations in the limiting plate (c). The hepatocytes comprise 80% of the liver cell population. (d). Functions of the hepatocyte: (i). Protein synthesis (ii). Metabolism – lipids and glucose/glycogen for storage and intermediary biochemical pathways e.g. converts ammonia to urea, conjugates bilirubin (iii). Bile secretion (iv). Detoxification including drugs, e.g. cytochrome P450 |
|
|
Can the liver regenerate?
To what extent can it do this? When might this occur? |
G. LIVER REGENERATION.
• The liver has almost unlimited capacity to regenerate. • There is enormous functional reserve of the liver such that failure may not be exhibited until 80-90% of hepatic tissue is lost. 1. Liver regeneration in acute liver injury. In mammals, hepatocytes can rapidly proliferate after acute liver injury to repair liver damage. Hepatocytes have a significant capacity for regeneration in response to liver injury. |
|
|
Liver Cirrhosis
|
- This condition usually results from repeated toxic insults to the liver (e.g. alcoholism, viral hepatitis). It is characterized by hepatocellular necrosis, hepatocellular regeneration (nodularity), and fibrosis (lipocyte activation). Clinical consequences include liver failure, portal hypertension, and even cancer.
|
|
|
Liver Cancer
|
- Primary liver cancer (i.e. hepatocellular carcinoma) is one of the most common neoplasms world-wide (often associated with viral hepatitis). Because of its extensive blood supply, the liver is also a common site for metastatic cancer (e.g. hepatic metastasis is found in 30-50% of autopsies on patients dying from malignant disease).
|
|
|
Neonatal Jaundice
|
- This common condition is due to an underdevelopment of the hepatocyte’s smooth endoplasmic reticulum. As a result, the hepatocytes cannot conjugate bilirubin which then builds-up in the body causing a yellow color (jaundice).
|
|
|
What is the function of bile?
|
Bile has two key functions:
1. Digestion - emulsification of dietary fats in the intestines – bile acids and salts. Help in absorption of fatty acids, monoglycerides, cholesterol and other lipids from the intestine. by detergent action. 2. Waste excretion: a. bilirubin - end product of hemoglobin breakdown b. cholesterol- by product c. metabolites |
|
|
What transports bile from the hepatocytes to the duodenum? Trace the path it takes.
|
The biliary tract system transports bile from the hepatocytes to the duodenum. It consists of the bile canaliculi, bile ductules at perimeter of lobules, which enter bile ducts in the portal triads and join to larger ducts.
A. Intrahepatic - bile canaliculi, enter bile ductules via the canals of Hering (which penetrate the limiting plate). Join larger bile ducts in the Portal Triads. These are lined by a simple cuboidal epithelium. B. Extrahepatic - lined by simple columnar epithelium 1. Hepatic duct. The right and left hepatic ducts leave the liver at the porta hepaticus and join to form the common hepatic duct. 2. Gallbladder & cystic duct - the gallbladder is drained by the cystic duct; the cystic duct joins with the common hepatic duct to form the common bile duct. 3. Common bile duct - joins with the main pancreatic duct to form the ampulla of Vater which angles obliquely through the wall of the duodenum (this probably helps prevent reflux of duodenal contents). 4. Sphincter of Oddi - smooth muscle complex which controls the opening of the ampulla of Vater; between meals this sphincter remains closed and prevents bile from passing through and prevents reflux from the intestine. When closed bile backs up through the cystic duct to collect in the gallbladder for storage. |
|
|
What is bile composed of?
pH? |
Bile Constituents. Hepatic bile is a pigmented
fluid. It is isotonic, alkaline (pH = 8.6), and contains: 1. Water (82%) 2. Bile acids (12%) (e.g. cholic and chenodeoxycholic acids) - act as detergents which emulsify lipid via micelle formation (produced from cholesterol by hepatocyte SER) a. emulsify cholesterol in bile b. emulsify intestinal fats which facilitates actions of pancreatic lipases & absorption 3. Bilirubin (conjugated or water-soluble) 4. Cholesterol 5. Other components - electrolytes |
|
|
What are the functions of the gall bladder?
What is the maximum volume of the gall bladder? How much bile does the liver produce per day? How much of the bile excreted into the intestine is reabsorbed? |
The gallbladder serves as the structure which stores,
concentrates, and releases bile. 1. Storage - normally can store 30 - 75 ml of concentrated bile (about 12 hours worth of bile produced by liver) 2. Concentration - originally hepatic bile is isotonic; However, in the gallbladder resorption of water concentrates bile up to 5X. 3. Release - upon demand, the gallbladder can contract and release bile into the duodenum. Maximum volume 40-70 ml. The liver continuously produces bile at about 600-1200 ml of bile per day. 90% of bile acids excreted into the intestine is reabsorbed (esp. ileum) and returned via the portal vein to the hepatocytes (“enterohepatic circulation”). |
|
|
Describe the gross and microscopic structure of the gall bladder.
|

1. Gross
- the gallbladder is pear-shaped structure (fundus, body, neck) - located on visceral surface of liver; is retroperitoneal (exposed surface covered by peritoneum; hepatic surface by adventitia) - connects to common hepatic duct via the cystic duct - spiral fold (spiral valve) keeps lumen of cystic duct open which allows bidirectional flow of bile 2. Microscopic - simple columnar epithelium (lacking in goblet cells). - surface microvilli, tight junctions, and basolateral active Na+ pumps (H2O follows osmotically). - mucosa is thrown into numerous folds or plicae when contracted. Branched. Loose connective tissue stroma. - thin layer of smooth muscle in wall – muscularis externae. - adventitia outside the smooth muscle – loose connective tissue. |
|
|
Describe how CCK affects bile secretion.
|
Cholecystokinin (CCK)
- hormone secreted by enteroendocrine cells (I cells) in duodenal epithelium. - stimulated by the presence of ingested fats and amino acids. - causes gallbladder smooth muscle to contract. - causes the sphincter of Oddi to relax. |
|
|
- The serous cells are highly polarized – they exhibit strongly basophilic staining in the base (because of abundant RER) and an acidophilic apex (filled with zymogen granules).
|
|
|
What is the pH of the digestive fluid secreted by the exocrine pancreas?
What are the main components of the pancreatic exocrine secretions? |
Synthesis and secretion from acinar cells and function of pancreatic enzymes and other secretions.
The digestive fluid secreted by the exocrine pancreas is isotonic and alkaline (pH > 8.0). 1. Pancreatic Enzymes (produced by acinar cells). a. amyolytic enzymes (e.g. amylase) - hydrolytic breakdown of carbohydrates. b. lipolytic enzymes (e.g. lipase) - hydrolytic breakdown of fats. c. proteolytic enzymes (e.g. trypsinogen) - hydrolytic breakdown proteins. - Proteolytic enzymes are produced, stored, and released as inactive proenzymes (zymogens). 2. Water & Electrolytes (produced by ductular cells) - alkaline fluid, rich in -HCO3 - helps to neutralize acidic chime from the stomach. - all pancreatic enzymes function best at neutral pH. |
|
|
What controls exocrine pancreas secretions?
|
Hormones secreted by enteroendocrine cells of duodenal & jejunal mucosa - hormones are secreted in response to ingested food and pH of gastric chyme
a. fat rich food -> Cholecystokinin ( CCK) stimulates enzyme-rich secretions by acinar cells. b. acidic chyme -> secretin -> watery, bicarbonate-rich secretions by ductal cells. 2. Vagus nerve - parasympathetic exerts significant control over pancreatic secretions. |
|
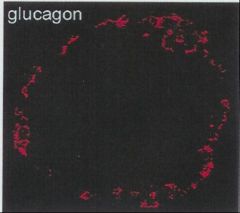
What cells are stained in this image?
|
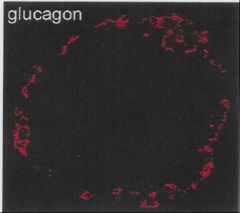
A (alpha) cells – Glucagon. Increases blood glucose levels.
- 20% of islet cells. - more peripherally located in islet (see Figure 10). - dense core granules are round, uniform, and have a clear halo. ***pancreatic islet of langerhan |
|
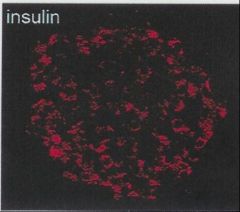
What cells are stained in this image?
|
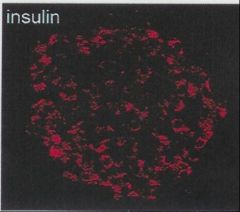
B (beta) cells - insulin -> decreases blood glucose levels.
- 70% of islet cells; are centrally located throughout he islets - The granules have irregular crysalline cores (packaged by Golgi) - Production process includes preproinsulin, proinsulin. - The proinsulin is cleaved into insulin and C peptide (both are secreted into the blood). ***pancreatic islet of langerhan |
|
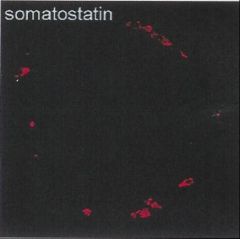
What cells are stained in this image?
|
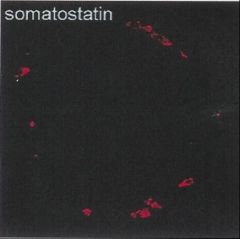
D (delta) cells – somatostatin.
- 5% of islet cells (Figure 12). - Function: inhibits other islet cells (paracrine effect) and slows motility of intestinal tract - this extends the time for digestion and uptake of nutrients. ***pancreatic islet of langerhan |
|
What cells are stained in this image?
|
F cells - pancreatic polypeptide
- rare cell ***pancreatic islet of langerhan |
|
|
Cholecystectomy
|
- the surgical removal of the gallbladder is a very common procedure (e.g. for gall stones) and indicates that it is not essential for life (although certain dietary modifications may be necessary). Certain mammals (e.g. horse, deer, rats) do not have a gallbladder at all.
|
|
|
Acute Pancreatitis
|
- although uncommon (5,000 cases per year in the US), this is a serious condition associated with a 10% mortality rate; regardless of the inciting cause, autodigestion by activated proteolytic enzymes is the pathogenesis; blood tests for increased levels of certain enzymes (amylase and lipase) which “leak” into the blood are helpful in making the diagnosis
|
|
|
Primary sclerosing cholangitis
|
- this is a disease of uncertain cause that involves ongoing inflammation, destruction, and fibrosis (“onionskin” appearance) of intrahepatic and extrahepatic bile ducts. It leads to cirrhosis, portal hypertension, and liver failure.
|
|
|
Jaundice
|
- a syndrome characterized by hyperbilirubinemia and deposition of bile pigments in the skin, mucous membranes, and other tissues resulting in the yellow appearance of the patient (icterus is a synonym for jaundice); the causes of jaundice or icterus may be prehepatic (e.g. hemolysis), hepatic (e.g. hepatitis), or posthepatic (e.g. biliary tract obstruction)
|
|
|
Cholelithiasis
|
- gallstones (i.e. stones or calculi in the gallbladder or biliary tract) form when solid concretions of cholesterol lipid acts as a nidus for calcium salt deposition. At least 10-15% of adults may have gallstones; small gallstones are asymptomatic while larger gallstones can cause obstructive jaundice, cholecystitis, pancreatitis or other problems.
|
|
|
Cystic Fibrosis
|
- about 90% of CF patients depend upon pancreatic enzyme supplements to relieve the symptoms of exocrine pancreatic insufficiency d/t chronic pancreatitis. The progressive pancreatic damage is thought to be due to ductal inspissation since the CFTR chloride channel cannot dilute (and alkalinize) the pancreatic juices. This results in dilated (cystic) ducts with surrounding fibrosis (thus, “cystic fibrosis”).
|
|
|
Diabetes Mellitus
|
- a metabolic disorder characterized by increased blood glucose levels; there are two types of diabetes mellitus: Type 1 is usually d/t autoimmune destruction of the islets with a resulting loss of beta cells (and insulin production), whereas Type 2 usually involves a decreased sensitivity of tissues to insulin which is called insulin resistance (i.e. levels of insulin may be normal or even increased!).
|
|
|
Insulinoma
|
- a form of cancer involving the B (beta) cells of the islets; these tumors may be functional which results in unregulated insulin hypersecretion and symptoms of hypoglycemia.
|
|
|
Pancreatic Carcinoma
|
- the close association of the pancreas with large blood vessels, extensive drainage to lymph nodes, and frequent spread to the liver via the portal venous system are factors contributing to the ineffectiveness of surgical removal (or cure) of pancreatic tumors.
|

