![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
28 Cards in this Set
- Front
- Back

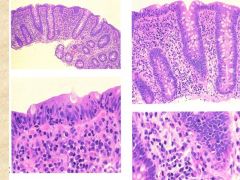
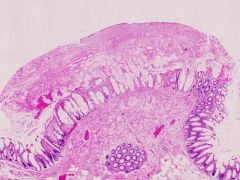
What are the histologic features of normal small intestine?
How do you distinguish different parts of the SI? |
- Long vili (facing lumen) with crypts at base
- Lined by goblet cells (mucous) Duodenum--> brunner's glands Terminal ileum --> peyer's patches Otherwise, the jejunum and ileum look identical |
|

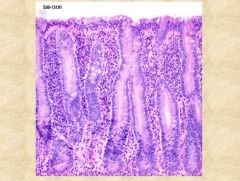
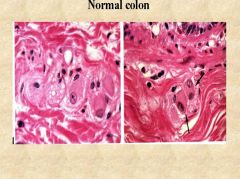
What are the histologic features of normal colon?
|
- Crypts (no vili) lined by goblet cells
- test tube like architecture - small amount of mononuclear cells within lamina propria |
|
|
What is the central problem in IBD (Inflammatory Bowel Disease)?
|
Patients have unregulated, exaggerated response to commensal organism in gut. They have epithelial barrier defects (allow bacteria to get in)
|
|
|
What is the role of NOD2 in Crohn's disease?
|
NOD2= intracellular receptor for microorganisms (triggers NF-kB pathway to kill bacteria). Defective NOD2 in CD, so persistent intracellular microbes --> body reacts with continuous inflammation.
|
|
|
What is the age distribution of Crohn's Disease? What region of the GI tract is affected most commonly?
What are some typical presenting clinical features in these patients? |
Bimodal- 20s/30s and 60s/70s (F>M, Jews > no-jews)
Terminal ileum = most commonly affected (rectal sparing) Features = abdominal cramping, diarrhea, weight loss, fatigue, joint pain, etc. |
|

What gross morphologic characteristics of Crohn's is seen here?
|
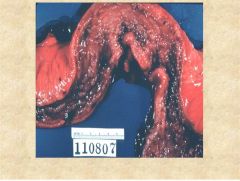
Left = Hyperemic (inflammation of walls)
Right = Cobblestone appearance (sharp demarcation between fissuring ulcer and normal mucosa). *above image shows cobblestoning and stricture formation (from thickening fibrosis) |
|

What characteristic finding in the right panel helps indicate what type of GI pathology this is?
|
Skipped lesions (there are aphethous ulcers on the surface of the mucosa, amidst normal gut mucosa). This is what causes the "cobble stone" appearance.
|
|
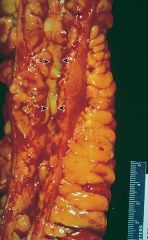
What pathognomonic finding is shown here?
|
Creeping fat, seen in Crohn's disease. You can see that lumen is narrowing (because bowel wall is thickening), and mesenteric fat is extending into bowel surface.
*typically fat just hangs off the side of the colon |
|
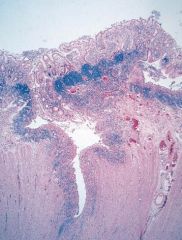
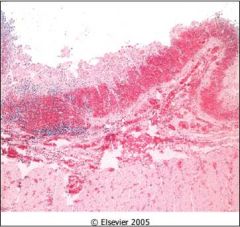
This is a gross histologic image of what Inflammatory Bowel disease? How can you tell? What is a complication of this condition?
|
Fissuring ulcer (going into submucosa and muscularis propria). Transmural involvement (characteristic of CROHN'S DISEASE), with preservation of intervening mucosa.
Complication = adhesion with adjacent bowel loop and fistula formation |
|
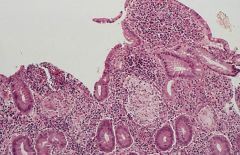
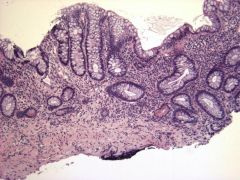
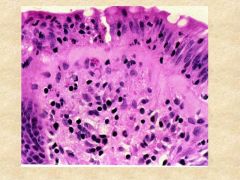
What characteristic lesion is shown in this image? What inflammatory bowel disease is it associated with?
|
Non-caseating granuloma. Associated with CROHN'S disease.
Note the epitheliod histiocytes (aggregations of macrophages)- Th1 mediated. |
|
|
What is the age distribution of UC?
What is the typical clinical presentation of the disease? |
Peaks in 20s (but affects any age)
Clinical presentation = chronic, relapsing disorder. Attacks of bloody mucoid diarrhea. Lower abdominal pain, cramping, weight loss. |
|

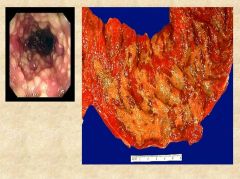
What features of UC (shown in the left panel) differ from Crohn's disease?
What is the most common site of UC? |
UC= well formed granulomas are absent. No skip lesions (hyperemia of entire surface). Ulcers do not extend full length of wall.
Most commonly seen in end of colon (starts in rectum). There is no mucosal thickening like Crohn's (not much fibrosis). Much higher risk of carcinoma. |
|

What are characteristic features of ulcerative colitis shown here?
|
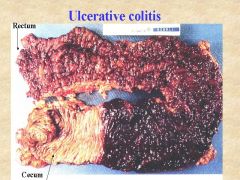
Left= frank ulceration, with loss of normal mucosa (full surface affected, no intervening normal mucosa).
Right = Friable psuedopolyp (should be biopsied). *above: see the Colonic involvement without skip lesions (sparing of cecum of terminal ileum) |
|
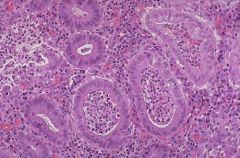
What are these lesions called and which type of Inflammatory Bowel disease are they more representative of?
|
Crypt abscesses- these are neutrophils within center of crypts. Seen in UC (but can also be found in Crohn's). Sign of active disease.
*note above: UC showing limited mucosal involvement and architectural distortion of colonic crypts. |
|
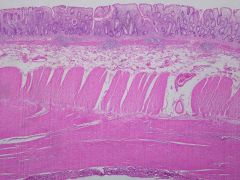
This is an image of a person treated with infliximab for ulcerative colitis. What changes can you see in the colon?
What is the most dangerous long term complication of Inflammatory bowel disease? |
This is Chronic inactive colitis. Treated patients show some normal test tube crypt formation. But there are also PANETH cells (seen in proximal colon) which indicate metaplasia.
Complication = dysplasia (risk increases 1% per year after diagnosis). Need to do colonoscopy to follow up and biopsies every 10cm. |
|
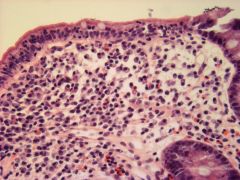
What are two types of Microscopic colitis?
Which is shown above? What demographic does it tend to affect? |
Lymphocytic and Collagenous colitis
Lymphocytic shown here (note intraepithelial lymphocytes). On gross inspection, the colon looks normal (thus MICROSCOPIC colitis). Tends to be associated with Celiac sprue. Vs. Collagenous which affects middle aged women |
|
What type of microscopic colitis is shown here? What stain would better help identify this?
|
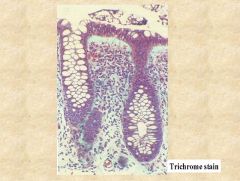
Collagenous colitis (note the thickened basement membrane full of collagen)
Trichrome stain for collagen helps identify it. Unknown etiology (may be autoimmune). |
|
Describe the etiology of the condition shown here.
What is the typical clinical scenario for this? |
Pseudomembranous colitis- from exotoxin A & B damage (typically C. dif, a normal gut flora). Occurs 6-8 wks after a course of antibiotics that clear out normal, protective gut flora.
Often seen in hospital/nursing homes. Presentation with abdominal pain, PROFUSE DIARRHEA, and low grade fever. |
|
What does this biopsy show?
What would be an appropriate treatment for the patient? |
Fibrinopurulent membrane is shown (doesn't form epithelium, just sticks to existing colon, thus pseudomembrane).
Treat with metronidazole, vancomycin. Give supportive care. *for recurrent infections, fecal transplant helps! |
|
What are some characteristic histologic features of Celiac Sprue (i.e Gluten Sensitive Enteropathy)?
What area is most affected? |
There is crypt hyperplasia and villous atrophy (affects the ileum).
Proximal area of small intestine (duodenum) is most affected (shows most atrophy and flattening, good place to do a biopsy) |
|
Describe the pathogenesis of Celiac Sprue. What is shown in the above image?
|
Sensitivity to gliadin (found in wheat). Gliadin is deaminated by TTG (tissue transglutaminase) and it binds to MHC molecules (DQ2 and DQ8). --> CD4 recognize these particles and cause damage to epithelium. CD8 activation cause further damage.
Above = diffuse flatening of vili. Note the intraepithelial lymphocytes (CD8+). |
|
|
How can you diagnose Celiac Sprue? What are long term complications of this condition that you want to be aware of?
Are there any treatments? |
Diagnose via history, Test for Gliadin or TTG antibodies. HLA typing (associated with HLA-DQ2 and DQ8). Almost 90% of patients with Celiac disease have these. Biopsy (esp of duodenum, or proximal SI).
T-cell lymphoma and epithelial malignancy (adenocarcinoma), can result. Remove gliadin from diet. |
|
|
What age group is Celiac sprue typically diagnosed in? Does it show a predominance to a certain population?
What dermatologic condition is it associated with? |
wide range (from infancy to adulthood). Predominant in Northern European/Caucasian.
Associated with Dermatitis Herpetiformis (vesicles that are itchy). |
|

What is the most common congential anomaly of the GI tract?
|
Meckel's diverticulum- true diverticulum- pouch composed of all layers of SI. It is ~20 cm from ileocecal valve. Can contain ectopic gastric secreting or pancreatic rests.
Results from failure to involute the vitelline duct or yolk stalk. Complications = duodenal atresia, stenosis. Imperforate anus. All can lead to intestinal obstruction. |
|
This is the biopsy of a baby who failed to pass meconium and had a distended abdomen. What is shown here?
What is the diagnosis and what might be some clinical presentations? |
Hirschsprung disease- failure of ganglion cells (of auerbach and meissner's plexus) to migrate to colon wall. There is a "functional obstruction" (no peristalsis), so fecal material backs up and causes megacolon.
Tends to present as babies, with pseudomembranous colitis (from bacterial overgrowth), or diarrhea *in biopsy, only nerves can be seen, not the normal pale pink ganglion cells shown above |
|
|
What are four major causes of ischemic bowel disease (can be acute or chronic)?
|
1. Arterial occlusion (atherosclerosis, emboli, aneurysm, vasculitis)
2. Venous thrombosis (hypercoagulable, post-op, peritonitis) 3. Hypoperfusion (shock, cardiac failure, dehydration) 4. Strangulation, volvulus |
|

What is the difference in clinical presentation between mucosal/mural, transmural, and chronic ischemic colitis?
|
Mucosal/mural (only surface is lost)- non-specific abdominal complaints, intermittent bloody diarrhea.
Transmural- older pts, severe abdominal pain, bloody diarrhea. Can perforate and get peritonitis & sepsis. Chronic Ischemic colitis- intermittent bloody diarrhea (confused with Inflammatory bowel disease!) |
|
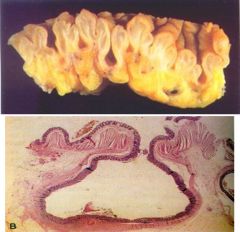
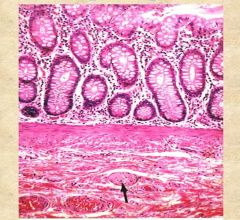
Is this a true diverticula?
What is the pathogenesis of diverticulosis? What age is most commonly affected? |
No. True = all layers of wall. This only has mucosa & submucosa, but no muscularis propria.
Low fiber diet --> low stool bulk --> ↑ peristalsis (contraction) --> ↑ intraluminal pressure --> outpouching into subserosa. *complications if fecal matter gets stuck --> causes inflammation and LLQ pain. Rx. surgery |

