![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
74 Cards in this Set
- Front
- Back
|
What GI disease causes 1/3rd of all cases of dyspepsia?
|
Peptic Ulcer Disease
|
|
|
Peptic ulcer disease includes both _____ and ____ ulcers
|
gastric and duodenal
90% are duodenal ulcers located in the first portion of duodenum |
|
|
Peptic ulcers are primarily associated with ______ and ________
|
NSAIDS and H PYLORI
although it can occur with or without h pylori infections |
|
|
Gastric ulcer: Definition
|
chronic ulceration in the lining of the stomach, frequently in the lesser curvature of the antrum near the pre-pyloric area
|
|
|
What is the peak age range for PUD?
|
Peak ages: 55-65 years, rare before age 40
|
|
|
PUD: Etiology
|
Familial tendency for gastric ulcer
Causes of gastric ulcer are multifactoral >60% have positive H. pylori Whereas >80% of pts with duodenal ulcers have H. pylori NSAIDs – ulcerogenic drugs Cocaine use: may increase stomach imbalance Imbalance between aggressive factors Gastric acid, pepsin ..and protective factors Mucous, blood flow, cell turnover |
|
|
H pylori and cancer risk
|
2 – 6 x higher risk for gastric cancer in presence of H. pylori
90% adenocarcinoma of stomach have pos H. pylori |
|
|
H pylori and ulcer formation
|
More than 50% of adults have chronic H pylori infection, but only 5-10% develop ulcers (Peters, 2010)
|
|
|
People at higher risk for H pylori infection
|
Hispanic
African American Older adults Lower socioeconomic level of income |
|
|
PUD: PRIMARY PREVENTION
|
Avoid/decrease use NSAIDs
Quit cigarette smoking Associated with corticosteroid use – minimize overuse if possible Stress reduction (questionable if effective) May not be related to etoh, caffeine, dietary spices, Tylenol If anything irritates stomach, best to avoid but … bland diet DOES NOT promote healing! |
|
|
PUD and bland diet
|
If anything irritates stomach, best to avoid but … bland diet DOES NOT promote healing!
|
|
|
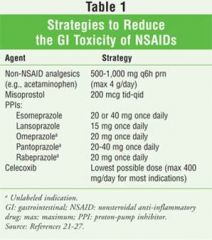
Primary prevention if caused by NSAIDs
|
|
|
|
Secondary Prevention: PUD
|
NONE!
Early diagnosis facilitated by high level of suspicion in: 1. pts taking NSAIDs to facilitate early diagnosis 2. H pylori levels in symptomatic pts (some resources suggest only doing in face of positive ulcer finding e.g. positive fecal blood) 3. Fecal blood – requires follow-up studies to determine site of bleed NB: Hg may be normal unless hemorrhage |
|
|
***GASTRIC ULCERS AND EFFECT ON HEMOGLOBIN
|
NB: Hg may be normal unless hemorrhage!
|
|
|
What are classic symptoms (relieving and exacerbating factors) of gastric ulcers?
|
Pain decreased or absent with fasting (CLASSIC)
Pain occurs almost immediately after eating (CLASSIC) Food avoidance, weight loss common |
|
|
Duodenal Ulcer Symptoms
|
Gnawing or burning epigastric pain 1-3 hours after meals
Nocturnal pain causing early morning awakening Pains relieved by: food, antacids, antisecretory agents |
|
|
NSAID INDUCED ULCERS: SYMPTOMS
|
NSAID induced ulcers may be asymptomatic – perforation may be first overt sign of disease (medical emergency!)
|
|
|
PUD: DIFFERENTIAL DIAGNOSIS
|
Non-ulcer dyspepsia
Zollinger-Ellison syndrome (gastrinoma) Usually tumors in head of pancreas or sm intestine are cause – they secrete gastrin that increases gaastric acid. About ½ of these are malignant, and many of the patients have MENS (Multiple Endocrine Neoplasia), which also effects the pitutitary and parathyroid. NB: Gastric carcinoma – symptoms of this are vague and it is rare to diagnose this in early stage! H pylori induced gastritis GERD Cholecystitis Crohn’s disease (gastroduodenal) Variant angina pectoris |
|
|
****GASTRIC CARCINOMA: SYMPTOMS
|
NB: Gastric carcinoma – symptoms of this are vague and it is rare to diagnose this in early stage!
|
|
|
PUD: Assessment: GENERAL
|
Overall appearance including Weight and Affect
Skin: including Hydration Abd exam: esp. epigastric tenderness |
|
|
PUD: ASSESSMENT: IMAGING
|
Endoscopy more accurate than radiology, and Endoscopy is considered less expensive
|
|
|
PUD: ASSESSMENT: LABS
|
H. pylori (Peters, 2010)
Serum antibody – cheapest non-invasive test-remains positive for years after eradication Only useful if negative as a positive needs to be confirmed with one of other two tests Stool antigen – highest sensitivity and specificity – can test for resolution Carbon-labeled urea breath testing – most accurate non-invasive test and resolution Accurate 4 weeks after treatment for eradication Fecal occult blood Would you draw a Hg? Consider serum gastrin (seen in Zollinger-Ellison syndrome) |
|
|
H Pylori Serum Antibody
|
cheapest non-invasive test-remains positive for years
after eradication Only useful if negative as a positive needs to be confirmed with one of other two tests |
|
|
What h pylori test has the highest sensitivity and specificity?
|
Stool antigen – highest sensitivity and specificity – can test for resolution
|
|
|
most accurate non-invasive test and resolution for h pylori
|
Carbon-labeled urea breath testing – most accurate non-invasive test and resolution
Accurate 4 weeks after treatment for eradication |
|
|
Zollinger-Ellison syndrome: Definition
|
Extensive ulcerations in stomach and duodenum due to excess secretion of acids
|
|
|
PUD: Management: Guidelines
|
In young, healthy, person with dyspepsia and without weight loss, or persistent vomiting; AND <45 years (American College Gastroenterology, 2010; Chey, 2007)
Empiric treatment initially is considered reasonable All others: Endoscopy Emergency endoscopy and hospitalization if suspected ulcer bleeding |
|
|
IF NEGATIVE FOR H pylori treat: RULE OF THUMB
|
just with acid suppression:
|
|
|
If negative for H PYLORI how long do you treat a gastric ulcer
|
12 weeks
|
|
|
If negative for H PYLORI how long do you treat a duodenal ulcer
|
8 weeks
|
|
|
PUD therapy: H2 receptor antagonists (H2RA)
|
No longer considered first line, but much cheaper and otc when compared to PPIs
Examples: Ranitidine or Nizatidine 150 bid or 300 mg HS Cimetidine 400 bid or 800 HS (very inexpensive) |
|
|
PUD Therapy: Proton pump inhibitor
|
Treat for 4 – 8 weeks e.g.
First line drug choice usually Promote healing of ulcer Examples: Omeprazole 20 mg qd (may be curative of PUD in 8 weeks) |
|
|
What is the first line treatment for PUD?
|
PPI
treat for 4-8 weeks (may be curative in 8 weeks) promotes healing of ulcer |
|
|
H pylori eradication protocols
|
Multiple “triple therapy” regimen
Example for two weeks (first line treatment 2013) Omeprazole 20 mg bid Clarithromycin 500 bid Amoxicillin 1 gm bid |
|
|
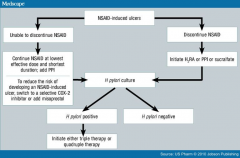
PUD from NSAIDS
|
|
|
|
PUD: Follow up
|
Return visit in 2 weeks (or sooner) to evaluate
Weight Symptom relief Adherence to plan Ensure quit smoking plan If no improvement or if any high suspicion symptoms occur, refer to gastroenterologist for endoscopy |
|
|
PUD: Economic, ethical, legal psychosocial, cultural, and family considerations
|
During treatment, symptoms usually mild enough to allow essentially normal activities for work/school/family/social
Dietary restrictions no longer required within reason. |
|
|
PUD: Health policy implications
|
There have been proposals to increase health insurance in those who smoke – this is another example, including those of respiratory origin, indicating an increased health risk and subsequent health care cost from those who smoke. Should insurance costs be based on risks?
|
|
|
GERD: definition
|
the reflux of stomach contents into the esophagus – a ‘mobility disorder’
|
|
|
GERD: causes
|
usually related to dysfunctional relaxation of the lower esophageal sphincter
Other causes: pregnancy, scleroderma, delayed gastric emptying, acid hypersecretion, some surgeries e.g. colon resection |
|
|
GERD: Primary Prevention
|
Avoid smoke, ETOH, and caffeine – coffee
Weight management Avoid meds that lower esophageal sphincter tone: Theophylline, anticholinergics, progesterone, calcium channel blockers, alpha adrenergic agents, diazepam, meperidine Avoid foods that lower esophageal sphincter tone: High-fat foods, yellow onions, chocolate, peppermint Avoid foods that irritate esophagus: Citric fruits and juices, spicy food and drinks |
|
|
GERD: SECONDARY PREVENTION
|
NONE!
Testing for H pylori in high risk population is controversial. Use if no improvement with treatments – then is diagnostic NOT screener. |
|
|
GERD: Tertiary prevention
|
Step therapy:
Elevate HOB, avoid laying supine after meals, avoid valsalva maneuver, low fat diet, smaller more freq meals Wt loss if needed OTC antacids or H2 antagonists Stool antigen test for H pylori eradication following treatment Vitamin B 12 levels in patients with atrophic gastritis Hct |
|
|
GERD: Symptomatology and assessment
|
Heartburn (most pts have esophageal mucosal pathology, though not usually ulcers are present)
Regurgitation – almost all patients have heartburn and regurg – other symptoms are less often (Fisichella, 2010) Dysphagia Angina CP Bronchospasms Laryngitis Chronic cough Globus sensation Loss of dental enamel |
|
|
GERD: ASSESSMENT: DIAGNOSTICS
|
Consider
Barium swallow (finds ulcers and strictures, but not mucosal injury) – INSENSITIVE TO GASTRITIS Useful if patient also has dysphagia Esophagoscopy with biopsy ( preferred choice for outcome, cost, finding of Barrett’s esophagus, and pt preference) Esophageal pH monitoring and/or gastric analysis (use if atypical GERD) Esophageal manometry if surgery considered |
|
|
What is the preferred choice for GERD DIAGNOSTICS?
|
Esophagoscopy with biopsy ( preferred choice for outcome, cost, finding of Barrett’s esophagus, and pt preference)
|
|
|
Barrett’s esophagus
|
Strong links between prolonged unresolved GERD, Barrett’s esophagus, and esophageal cancer (Ferri, 2013)
|
|
|
GERD: Differential diagnosis
|
Infectious esophagitis candida, herpes, HIV, CMV
Chemical esophagitis Radiation injury Chron’s disease of esophagus Angina pectoris Esophageal/gastric carcinoma Medication related Achalasia PUD |
|
|
GERD: Management and Interventions
|
Step therapy includes dietary/lifestyle changes listed earlier for all individuals
Step treatment Mild symptoms: OTC H2 receptor antagonists (H2RA), antacids American Gastroenterology Assn most recent guidelines at guidelines.gov (2008): “Antisecretory drugs for the treatment of patients with esophageal GERD syndromes (healing esophagitis and symptomatic relief). In these uses, proton pump inhibitors (PPIs) are more effective than histamine2 receptor antagonists (H2RAs). ….Twice-daily PPI therapy for patients with an esophageal syndrome with an inadequate symptom response to once-daily PPI therapy.” Moderate - severe symptoms: proton pump inhibitors (PPIs) or prescription strength H2RAs Ulcerated esophagus: surgery H2RAs: Cimetidine (Tagamet) 800mg bid is least expensive option Many patients may have tried this otc already Heartburn history has a positive predictive value >80% warranting empiric initial care in absence of worrisome symptoms Empiric trial of proton pump inhibitor compares well to pH monitoring as diagnostic tool for GERD NB: Complications more likely in elderly |
|
|
GERD: National protocols
|
Agency for Healthcare Research and Quality (AHRQ)
PPIs are superior to histamine H2-receptor antagonists for the resolution of GERD symptoms at 4 weeks and healing of esophagitis at 8 weeks. Typical GERD symptoms treatable with acid suppression therapy for 6-8 weeks If cont symptoms, or if not typical from onset, endoscopy Risk factors exist for stricture and Barrett’s esophagus – evaluation needed if unresolved GERD |
|
|
GERD: Resistant cases
|
Patients who do not respond to usual treatment after 4-8 weeks acid suppression therapy, should:
undergo is upper endoscopy to exclude a diagnosis of peptic ulcer disease or cancer and identify the presence of esophagitis (Richter, 2007) Refractory reflux syndromes associated with normal endoscopy findings are more problematic testing may include 48 h pH testing, impedance measurements (for nonacid reflux), esophageal manometry and gastric function tests. May need fundoplication surgery if not resolved with medications (90% effective; Cooper, 2007) |
|
|
Nissen fundoplication
|
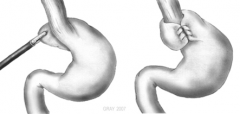
|
|
|
GERD: Case management: economic, psychologic considerations
|
Common disorder in adults
May limit socializing due to regurgitation, pain, cough, food limitation OTC medications ease access to treatment but don’t assist in identification of those with serious underlying disease |
|
|
Cholecystitis: definition
|
acute or chronic inflammation of the gallbladder, usually related to previously asymptomatic gallstones
|
|
|
Cholecystitis: what race is at higher risk?
|
Native Americans (Pima) and Scandanavian descent with greatest incidence
|
|
|
Cholecystitis: Risk factors
|
Women
Older adults (>40 years) Obese Fasting Low LDL, Elevated triglycerides Pregnancy Hyperalimentation Oral contraceptive pills Cirrhosis |
|
|
Cholecystitis: Primary prevention
|
Most risk factors not malleable
Avoid obesity Avoid rapid weight loss Consider alternate BC than OCP in Native Americans Low fat diet? Adequate fluid intake? Exercise may increase bile duct motility |
|
|
What ever happened to the undergraduate neumonic: fair, female, fat, forty, fertile?
|
Only partly correct
|
|
|
Cholecystitis: secondary prevention
|
NONE
|
|
|
Cholecystitis: Symptomatology
|
Intermittent pain, typically RUQ immediately following classically a meal of high fats
Pain is intense with radiation to epigastrum, R shoulder or back Classic ‘biliary colic’ is pain rising over 2-3 minutes to plateau of intensity maintained for >20 minutes Any suspicion that pain origin is cardiac warrants an emergent referral for cardiac workup Usual symptoms Anorexia, Abd bloating, Belching Nausea , Vomiting |
|
|
Cholecystitis: acute presentation
|
Acute presentation – emergent surgical referral:
May appear acutely ill Temp may be mildly to moderately elevated Abdominal distension Local epigastric/RUQ tenderness – rarely diffuse Jaundice Loose, light-colored stools Physical assessment special tests: Inspiratory arrest when palpating RUQ and pt taking deep inspiration (also with tenderness) Ortner’s sign: tenderness when hand taps the R edge of costal arch. Georgievskiy - Myussi's sign (phrenic nerve sign) - pain when press between edges of sternocleidomastoid muscle Boas' sign – Tenderness inferior to R scapula (also can be seen with phrenic nerve irritation) |
|
|
Murphy's sign
|
Inspiratory arrest when palpating RUQ and pt taking deep inspiration (also with tenderness)
|
|
|
Ortner’s sign
|
tenderness when hand taps the R edge of costal arch.
|
|
|
Georgievskiy - Myussi's sign
|
(phrenic nerve sign) - pain when press between edges of sternocleidomastoid muscle
|
|
|
Boas' sign
|
Tenderness inferior to R scapula (also can be seen with phrenic nerve irritation)
|
|
|
Cholecystitis: Symptomatology and assessment - chronic
|
Chronic presentation –
Usually only pain and nausea as with acute presentation, other symptoms absent Consider laparoscopic cholecystectomy as outcomes poorer if acute presentation for surgery (Ferri, 2007) Consider referral to gastroenterologist for dissolution agent, shock-wave lithotripsy or possible removal by endoscopic retrograde cholangiopancretography (ERCP) |
|
|
Diagnose acute cholecystitis: The diagnosis of acute cholecystitis is based on the presence of at least two of three factors;
|
• acute right upper quadrant tenderness
• fever higher than 99-5° F (37.5° C) or leukocytosis greater than 10,000/mm- • ultrasound evidence such as a thickened and edematous gallbladder wall, the presence of maximal tenderness elicited over the gallbladder, and pericholecystic fluid collection. |
|
|
Cholecystitis: differential diagnosis
|
PUD
Hepatitis Diverticulitis Dypsepsia Neoplasms Pancreatitis Perforated duodenal ulcer MI Pneumonia Nephroliasis |
|
|
Cholecystitis: Diagnostics: Labs
|
HCG in women of childbearing age
Amylase – if elevated >500U – consider pancreatitis ALT/AST (elevated) Alkaline phosphatase (elevated) Bilirubin (elevated) U/A CBC – expect leukocytosis in >70% patients |
|
|
GBUS: Cholecystitis
|
Highly sensitive and specific for GB disease – before ordering if symptoms suggest PUD, or gastritis would consider trial of PPIs for 2 weeks
Ultrasound can accurately detect cholecystitis in 95% of patients. |
|
|
Cholecystitis: management and interventions
|
Referral to surgeon if require narcotics
Acute cases remain NPO while transport to hospital Chronic presentations advise on low fat diets Consider watchful waiting in cases without biliary colic But in those cases with biliary colic (constant acute pain R shoulder or abd, with onset and resolution sudden, typically at HS, often with N/V), incidence of recurrence 50% annually and pt may likely benefit from surgery. |
|
|
When do you use non surgical options for cholecystitis?
|
Used for patients who are asymptomatic or poor surgical candidates
|
|
|
What are the non surgical options for cholecystitis?
|
Oral medications:
Drugs made from bile acid—including ursodiol (Actigall) (8-10mg/kg/day po divided qd-tid) used to dissolve the stones. These drugs work best on small (less than 20mm) cholesterol stones, and months or years of treatment may be necessary before all the stones are dissolved. Extracorporeal shockwave lithotripsy (ESWL): This treatment uses shock waves to break up stones into smaller pieces that can pass more easily through bile ducts and avoid blockages. However, intense pain can follow treatment, and the long-term success rate is not known. |
|
|
Cholecystitis: Economic, ethical, legal psychosocial, cultural, and family considerations
|
Post op course may limit family/social/work/school responsibilities for several weeks
|

