![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
23 Cards in this Set
- Front
- Back
|
What is the function of a stellate cell in the normal liver? What about in a state of injury (virus, alcohol, etc.)?
What are the "true" liver function markers? |
Normally, stellate cell= fat storage (vit A storage). In pathologic state, it produces collagen and is fibrogenic.
True = Bilirubin, Albumin, PT time/ coagulation factors (these all give an indication that liver is failing). AST, ALT are just markers of injury to cells. |
|
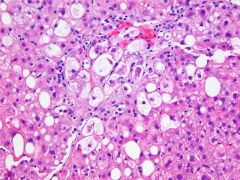
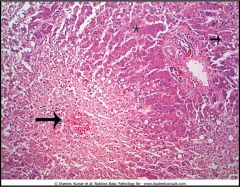
What histological finding is shown here? Is it specific to any condition?
|
Ballooning Degeneration- swelling of hepatocytes with cytoplasmic pallor and irregularly clumped cytoplasmic organelles.
Non-specific--> Can be seen in alcoholic hepatitis, NASH, Wilson's disease, viral hepatitis. |
|
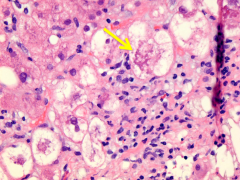
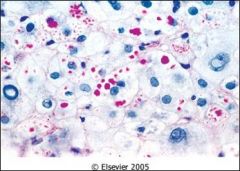
What is shown within the swollen cells? What condition is it most commonly associated with?
|
Ballooned hepatocytes with MALLORY HYALINE (eosinophilic aggregates of keratin). These are intermediate filaments that resist degradation.
Associated with Alcoholic Hyaline (also seen in PBC, Wilson, chronic cholestasis, tumor, etc.) |
|
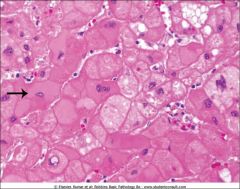
What type of liver change is seen here? What conditions is it seen in?
|
Feather degeneration (swelling of individual hepatocytes). Looks similar to ballon degeneration but there is yellow discoloration.
Seen in cholestatic liver disease (retained biliary material) |
|
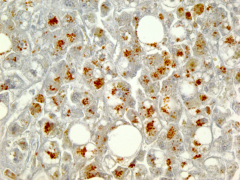
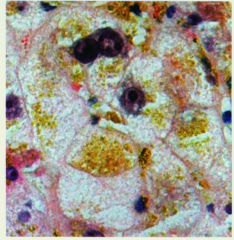
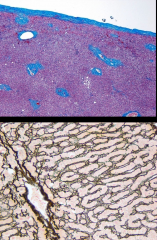
What type of stain would you use to diagnose Wilson's disease on a biopsy (shown above) ?
What about alpha1 antitrypsin deficiency? |
Wilson's disease --> Cu2+ deposits --> Rhodanine stain
a1AT deficiency --> PAS stain (for glycogen and glycoproteins). (shown above) |
|
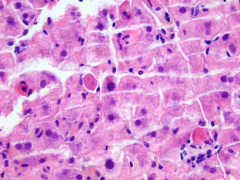
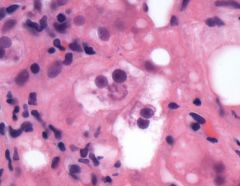
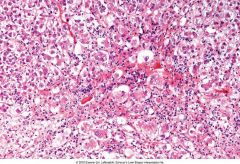
What are the eosinophilic cells in this image called? What
|
Counsilman Body (Acidophil Body) - they are apoptotic hepatocytes.
|
|
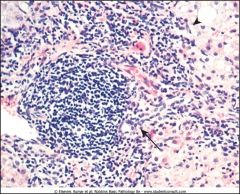
What is another name for the type of necrosis shown above?
|
Piecemeal necrosis = periportal inflammation = interface hepatitis
This is necrosis of limiting plate. Replacement of hepatocytes by inflammatory cells/fibrosis. |
|

What does the finding of "nutmeg liver" represent (shown above on gross image)?
If a patient had left sided heart failure, what zone would be most ischemic? Which zone would be most congested if the patient had right sided heart failure? |
Nutmeg liver = gross appearance of liver that has areas of hemorrhage and centrilobular necrosis
Left sided --> hypoperfusion --> Zone 3 most ischemic Right sided --> retrograde congestion --> blood accumulates in Zone 3 |
|
This person has overdosed on Acetaminophen and damaged their liver. What zone is most susceptible to necrosis?
|
Centrilobular necrosis - from acetaminophen overdose. Tylenol is broken down by CYP450 enzymes and it's metabolites are released (causing damage).
CYP450 enzymes are most abundant in zone 3 (Note: usually toxins affect zone 1 because they are highest in concentration there). |
|
|
What is the predominant cell that comprises the mononuclear infiltrate seen in Acute Hepatitis?
What about in Autoimmune hepatitis? Alcoholic hepatitis? Drug induced hepatitis? |
Lymphocytes! Though acute, lymphocytes respond to the virus causing damage to hepatocytes.
Autoimmune --> Plasma cells Alcoholic --> Neutrophils Drug-induced --> Eosinophils |
|
|
What is the difference between liver regeneration after partial hepatectomy vs. submassive/massive hepatic necrosis?
What are the stem cells of the liver called? |
Partial hepatectomy --> compensatory hyperplasia and hepatocyte replication
Massive hepatic necrosis --> stem cell = oval cells (in the canal of Herring) , differentiate in hepatocytes and cholangiocytes |
|
T or F
Collagen Type IV is found in liver sinusoidal cells. What stain is shown on the bottom image? |
False- they don't have basement membrane (no Col Type IV). Instead they have Col type 3 (stain positive with Reticulin).
|
|
|
What are the most common causes of cirrhosis?
What are some characteristics of cirrhosis? |
1. Chronic alcoholism, 2. Hepatitis (B&C)
Characteristics = - diffuse process (involves entire parenchyma) - bridging fibrous septa - parenchymal nodules that are encircled by fibrosis |
|
Does acute viral hepatitis cause portal or lobular inflammation? What about chronic viral hepatitis?
What are changes seen in Acute viral hepatitis (shown here)? |

ACUTE causes LOBULAR inflammation (chronic causes portal)
- ballooning degeneration -acidophil bodies (apoptosis) - lymphocyte predominance - kupffer cell aggregates (phagocytosis of hepatocellular debris) - LOBULAR disarray |
|
|
What is the definition of Chronic hepatitis? How does the distribution of inflammation in the liver differ from Acute hepatitis?
If someone is tested for Hep B and comes back with positive Anti-HBs, what does this indicate? |
Chronic - continuing/relapsing disease for > 6 months. Unlike acute, there is PORTAL/PERIPORTAL inflammation (with Interface hepatitis).
Anti-HBs --> either the person recovered from HBV infection (in which case, check Anti-HBc to check if positive), OR they were vaccinated (in which case HBsAg and HBc will be negative) |
|
What are the two major pathologic features of Chronic Hepatitis B, shown here?
|
1. Ground glass hepatocytes (HBsAg in the cytoplasm)
2. Sanded nuclei (contain HBcAg- core antigen) |
|
|
What is the greatest risk factor for HCV infection? If someone is Anti-HCV positive, what does that mean about their immune status?
What are two ways in which a person can acquire hepatitis D virus? |
#1= IV drug abuse, #2= multiple sex partners
Presence of Antibodies DO NOT confer immunity (unlike HBV) Hepatitis D: 1) via co-infection (with both hep C and hep B) 2) via superinfection (an HBV carrier can get superinfected with Hep D). |
|
What is the triad of findings you would see in CHRONIC hepatitis?
|

1. Lymphoid aggregates in portal tracts
2. Mild steatosis of iver 3. Bile duct injury |
|
What cell type do you see in this predominate in this type of Hepatitis (hint: it is indistinguishable from chronic viral hepatitis)?
What type of labs would it be appropriate to check in these patients? |
Autoimmune Hepatitis: Prominent PLASMA cell and lymphocyte infiltrate. Otherwise, indistinguishable from chronic viral hepatitis.
Check autoantibodies (positive in 80% of cases) - ANA, Anti-smooth muscle, anti-liver kidney microsome) *more predominant in females |
|

What is the causative agent of the abscess that you see in either image?
|
Left= amebic abscess ("anchovy paste")
Right= ecchinococcus (can cause hydatid cyst that if it ruptures --> anaphylaxis) |
|
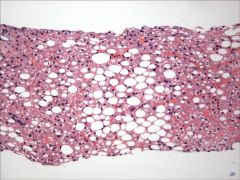
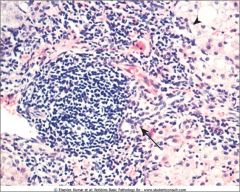
What are three forms of alcoholic liver disease? Which is shown above?
Which one(s) are(is) reversible? |
1. Hepatic steatosis (fatty liver)- reversible (shown in picture)
2. Alcoholic hepatitis- reversible 3. Cirrhosis --> IRREVERSIBLE |
|
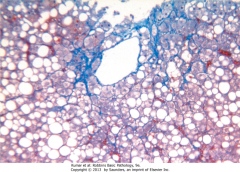
What is this type of fibrosis (associated with alcoholic hepatitis) called?
|
Chicken wire fence fibrosis (i.e. sinusoidal or pericellular fibrosis). From stellate cell activation and deposition of collagen.
|
|
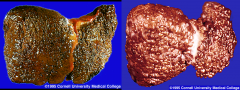
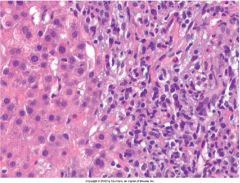
What condition is most commonly associated with the change seen on the left? What about the right?
|
Left= Micronodular < 3 mm --> secondary to ETOH (can also be seen in Wilson's disease, hemochromatosis, PBC)
Right= Macronodular >3 mm--> most common cause is VIRAL hepatitis |

