![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
131 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Most common cause of pseudocirrhosis (mimics cirrhosis) on CT?
a. Treated breast cancer b. Metastatic colon cancer c. liver transplant rejection d. pyogenic abscess e. candidiasis f. primary sclerosing cholangitis |
Treated breast cancer
In patients with cancer metastases to the liver, treatment with chemotherapy can result in areas of retracted tumor tissue and scarring. Lung or breast primary may simulate cirrhosis |
-between areas of scarring, the liver parenchyma is regenerative.
-referred to as pseudocirrhosis because it resembles macronodular cirrhosis -observed within a few weeks or months after therapy -unlike cirrhosis, at pathology patients do not have bridging portal fibrosis |
|
|
Which is NOT an US feature of cirrhosis:
a. Caudate atrophy b. Left lobe hypertrophy c. Increased echogenicity d. Lobulated contour, capsule nodularity e. Enlarged hepatic artery |

Caudate atrophy (FALSE)
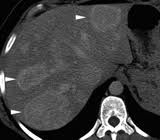
-asymmetric shrinkage of the right hepatic lobe (and medial segment of left lobe) with relative hypertrophy of the lateral left lobe and caudate Sagittal sonogram showing enlargement of the caudate lobe (C) in a patient with cirrhosis. Arrows, fissure for the ligamentum venosum. |
-increased echogenicity indicates fatty infiltration
-hepatic echotexture appear heterogenous, nodular, grainy or coarse -hepatic arterial flow is increased in the setting of portal hypertension to compensate for decreased portal flow |
|
|
Which is the most potent stimulator of pancreatic secretions?
a. secretin b. gastrin c. CCK d. somatostatin e. trypsin |
Secretin
-main stimulator of pancreatic secretions -inhibits gastrin -released when pH < 4.5 |
Gastrin
-strongest gastric acid stimulator Cholecystokinin -potent stimulator of GB contraction Somatostatin -prolongs gastric emptying time, decreases gastric acid & secretions, diminishes pancreatic exocrine secretion |
|
|
Role of MR in Crohns w perianal fistula:
a. Evaluate for occult abscesses and tracts not visible under anesthesia examination b. Evaluate for occult malignancy c. Evaluate healing |
Evaluate for occult abscesses and tracts not visible under anesthesia examination
|
|
|
|
Which is the function of gastrin?
a. Increase bicarbonate secretion of pancreas b. Increase polypeptide secretion of pancreas c. Increase gastric acid secretion |
Increase gastric acid secretion
|
|
|
|
Several non-circular, irregular shaped regions of low attenuation within liver. Normal branching vessels are seen coursing through these lesions. Diagnosis:
a. focal fat b. HCC c. hemangioma d. mets |

Focal fat
-doesn't have rounded convex margins like a mass -no displacement of normal vasculature, indicating that there is no mass effect -low attenuation (usually 0-30HU not true fat attenuation as this is microscopic fat) |
|
|
|
LEAST likely liver lesion to demonstrate increased through transmission?
a Metastasis b Focal fatty infiltration c HCC d Hemangioma e Abscess |

Focal fatty infiltration
-causes increased attenuation of the ultrasound beam, not increased through transmission |
-in hemangiomas, increased through transmission is often (but not always) present
-abscesses can have cystic components which will demonstrate increased through transmission -metastases can resemble anything |
|
|
MRI finding most specific for HCC:
a. early enhancement with delayed central washout b. array of T1 and T2 findings c. fat within the lesion (per UF) |
Fat within the lesion
Fat in HCC is very common Heterogeneous hypervascular mass with "washout" of contrast enhancement and portal vein invasion T2W1: hyperintense |
-If the patient is a young woman, keep in mind that adenomas can also have macroscopic fat.
"flash-filling" hemangiomas can have delayed washout |
|
|
TRUE regarding MR of liver with HCC:
a. Early arterial enhancement with early washout b. Isointense T1 and T2 signal c. Decreased T1 and increased T2 signal |

Early arterial enhancement with early washout
|
|
|
|
TRUE about GI stromal tumor?
a. large mucosal exophytic mass b. may display central region of low homogenous attenuation on CT c. spread by lymphatics d. treated by radiation |

May display large central area of low attenuation
(NOTE: if just exophytic, then true; if mucosal, then false) |
-ulceration and necrosis common on CECT
-PET superior to CT in predicting early response to Gleevec -Hypermetabolic foci for both primary tumor and metastases -Best diagnostic clue: Well-circumscribed, submucosal mass extending exophytically from GI tract -Best imaging tool: CECT, PET -Nonenhancing necrotic or hemorrhagic areas |
|
|
In a patient with glycogen storage disease, what are you likely to see in the liver?
a. hepatic cysts b. regenerative nodules c. hepatic adenomas d. FNH |
Hepatic adenomas
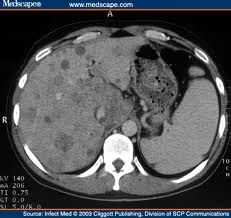
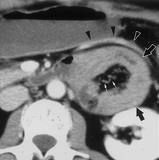
well-known complication of glycogen storage dz Type 1A, Von Giergke's disease Pic: Hepatic adenomas in a patient with type IA glycogen storage disease (von Gierke disease). Axial unenhanced computed tomographic (CT) image shows multiple relatively hyperattenuating lesions (arrowheads), findings consistent with adenomas. Note the abnormally low attenuation of the surrounding liver parenchyma secondary to diffuse fatty infiltration. |
-smaller than adenomas than those seen with contraceptive use and are less likely to hemorrhage.
-more likely to be multiple and undergo malignant degeneration into HCC although this is rare |
|
|
Which of the following is NOT associated with intestinal malrotation?
A. gastroschisis. B. omphalocele C. situs inversus totalis D. congenital diaphragmatic hernia E. asplenia |

Situs inversus totalis (NOT associated)
-On UGIS, spiraling “corkscrew” of small bowel as it twists around the SMA -On CT, SMA to right of SMV, spiraling of small bowel around the SMA -Radiography: "Double bubble" sign: Distended stomach and duodenum; little gas in remainder of SB |
Associations:
-Omphalocele, gastroschisis, diaphragmatic hernia -Asplenia and polysplenia syndrome, duodenal stenosis or atresia, annular pancreas, agenesis of dorsal pancreas, Hirschsprung disease |
|
|
A female patient has polycythemia rubra vera and suffers acute onset of right upper quadrant pain, hepatomegaly, and ascites. Liver biopsy demonstrates hepatic necrosis. What is the etiology?
a. Budd-chiari syndrome b. autoimmune hepatitis |
Autoimmune hepatitis
Polycythemia rubra is associated with both Budd Chiari and autoimmune hepatitis Autoimmune hepatitis biopsy -piecemeal necrosis, bridging necrosis, and fibrosis Budd Chiari liver biopsy -high-grade venous congestion and centrilobular liver cell atrophy -thrombi within the terminal hepatic venules |
|
|
|
Budd Chiari is NOT associated with:
a. chronic hepatitis b. polycythemia vera c. transplant liver d. myelodysplasia |
Transplant liver (NOT associated)
Budd Chiari: -Polycythemia vera is the most common underlying disease -Global or segmental hepatic venous outflow obstruction -"Bicolored" hepatic veins (due to intrahepatic collateral pathways) on color Doppler ultrasound CECT -Nonvisualization of IVC and hepatic veins -Hypertrophy of caudate lobe -Nodular regenerative hyperplasia in dysmorphic liver |
|
|
|
More common complication s/p lap gastric bypass surgery vs open bypass?
a. internal hernia b. wound infection c. adhesion d. incisional hernia e. iatrogenic splenectomy |
Internal hernia
Lap GBP decrease in: -iatrogenic splenectomy -wound infection -incisional hernia -mortality Lap GBP increase in: -early and late bowel obstruction (?internal hernia) -gastrointestinal tract hemorrhage -stomal stenosis |
|
|
|
FALSE about familial adenomatous polyposis coli (FAP)?
a. Associated with gastric adenomatous polyps in 80% b. Occurs with abdominal desmoid tumors c. Associated with cancer of duodenal papilla (ampullary tumor) d. Autosomal dominant e. 100% colon CA is left untreated |

Associated with gastric adenomatous polyps in 80% (FALSE)
FAP -autosomal dominant -If left untreated, all patients with this syndrome develop colon cancer by age 35-40 years -Colon > stomach > duodenum > small bowel -2 varied expressions of FAPS: FAP coli and Gardner syndrome -Associated with ↑ incidence: Malignant CNS tumors |
Extraintestinal manifestations: Gardner syndrome
-epidermoid cyst, lipoma, fibroma, desmoid tumors -osteomas -thyroid cancer |
|
|
10 sub-centimeter polyps are present in the fundus and body of the stomach. What is the likely etiology?
a. Hyperplastic polyps b. Peutz-Jeger c. Polyps in familial autosomal polyposis d. Adenomas in FAP |

Polyps in familial autosomal polyposis (FAP)
-40% of patients with familial polyposis coli also have multiple small, sessile fundic gland polyps in the upper body and fundus of the stomach – so-called fundic gland polyposis -no malignant potential |
|
|
|
Increased risk of all of the following with hereditary non-polyposis colorectal cancer syndrome EXCEPT:
(a) cholangiocarcinoma (b) endometrial cancer (c) breast cancer (d) ovarian cancer (e) gastric cancer |
Breast cancer (NO increased risk)
HNPCC (Lynch syndrome I and II): -early age of onset -predominant involvement of the right colon -tumors evolve from colorectal adenomas -villous (flat) -70 percent of first lesions arise proximal to the splenic flexure |
Lynch syndrome II
-high risk of extracolonic tumors -most common of which is endometrial carcinoma |
|
|
What mesentery attaches to the anterior surface of the pancreas?
a. lesser omentum b. gastocolic ligament c. transverse mesocolon d. faliform ligment e. greater omentum f. lesser omentum |
Tranverse mesocolon
|
|
|
|
SBFT (shows asymmetric involvement of TI) with 3 cm linear ulcerations on mesenteric border and pseudosacculation on anti-mesenteric border:
a. Crohn’s disease b. Scleroderma c. TB d. Yersinia e. UC |
Crohn's disease
Classic SBFT: ulceration on mesenteric border with pseudosacculation of anti-mesenteric border |
|
|
|
Patient with hypovolemia (hypoperfusion syndrome). all are seen EXCEPT:
a. Small aorta b. Flat IVC c. Periportal edema (tracking) d. Hyperenhancing bowel e. Pancreas hypodensity |
Periportal edema (tracking)
Hypoperfusion syndrome -shock bowel -diminished caliber and increased enhancement of the IVC and aorta -intense contrast enhancement of the kidneys and mesentery -hypodense spleen and pancreas due to vasoconstriction -intense adrenal enhancment |
|
|
|
10 yo child presents with hypoperfusion syndrome after hemorrhage. Which is NOT seen on CT of the abdomen?
A. dilated fluid filled bowel B. decreased enhancement of bowel wall C. small abdominal aorta D. slit-like inferior vena cava E. multiple abdominal fluid collections F. persistent nephrograms |
Decreased enhancement of bowel wall (NOT seen)
Hypoperfusion syndrome -shock bowel -diminished caliber and increased enhancement of the IVC and aorta -intense contrast enhancement of the kidneys and mesentery -hypodense spleen and pancreas due to vasoconstriction -intense adrenal enhancment |
|
|
|
Hypoperfusion syndrome, increased enhancement in all EXCEPT:
a liver b pancreas c adrenals d IVC e Small bowel wall |
Pancreas
Hypoperfusion syndrome -shock bowel -diminished caliber and increased enhancement of the IVC and aorta -intense contrast enhancement of the kidneys and mesentery -hypodense spleen and pancreas due to vasoconstriction -intense adrenal enhancment |
|
|
|
What is a characteristic on IPMT on CT?
a) diffuse pancreatic ductal dilatation b) unilocular mass c) multilocular mass d) hypodense mass |

Diffuse pancreatic ductal dilatation
Intraductal Papillary Mucinous Tumor -"Multicystic" lesion in uncinate process or pancreatic head contiguous with dilated MPD on CECT/MRCP BPD lesion: Uncinate process & head (branch panc duct) MPD lesion: Usually body &/or tail (main panc duct) -Main duct IPMT, ↑ chance of malignant degeneration |
|
|
|
TRUE regarding pancreatic adenocarcinoma on T1 pre and post contrast compared to normal pancreas:
a. Hypo pre, hypo post b. Hyper pre, hypo post c. Hyper pre, hyper post d. Hypo pre, hyper post |
T1 hypo pre, T1 hypo post
poor or no enhancement of adenocarcinoma |
|
|
|
TRUE regarding pancreatic adenocarcinoma:
A. Adenocarcinoma is associated with duct dilatation and atrophy of tail B. Displaces vessels C. Hyperechoic on ultrasound D. Well encapsulated E. Isointense enhancement on arterial phase F. Hypervascular |
Adenocarcinoma is associated with duct dilatation and atrophy of the tail
-Encases vessels. Infiltrates vessels rather than displacing them. -Hypoechoic on US. -No capsule. Musinous cystic neoplasm is encapsulated. -Nonenhancing, fibrotic, hypovascular adenocarcinoma |
|
|
|
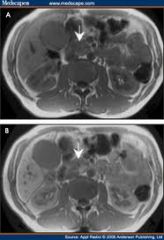
Most common type of choledochal cyst:
a. fusiform dilatation of CBD (fusiform dilatation of extrahepatic duct) (type I) b. saccular dilatation of CBD (type I) b. extrahepatic duct diverticulum c. Caroli’s disease d. intra/extra hepatic biliary duct dilatation e. choledococele |
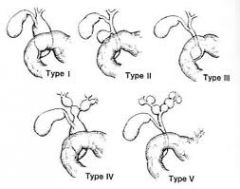
Fusiform dilatation of the CBD
Type II: diverticulum of the common bile duct (rare) Type III: intrapancreatic diverticulum or choledococele (rare) Type IV: extra and intrahepatic ductal dilation (2nd most common) Type V: intrahepatic duct dilation (Caroli's disease) |
|
|
|
LEAST likely to cause cavitary small bowel lesion:
a. melanoma metastasis b. lymphoma c. adenocarcinoma d. GIST |
Melanoma metastasis (LEAST likely)
Classically, a cavitary small bowel lesion is lymphoma. |
Cavitary Small Bowel Lesions DDx includes:
1. Lymphoma 2. Leiomyosarcoma ie GISTs 3. Primary adenocarcinoma - duodenum 4. Metastases (especially malignant melanoma) |
|
|
MOST likely to cause cavitary small bowel lesion:
A. Melanoma B. Leiomyosarcoma C. NHL D. Adenocarcinoma |
Answer: 1. Lymphoma. 2. Leiomyosarcoma.
Classically, a cavitary small bowel lesion is lymphoma. |
Cavitary Small Bowel Lesions DDx includes:
1. Lymphoma 2. Leiomyosarcoma, ie GISTs 3. Primary adenocarcinoma - duodenum 4. Metastases (especially malignant melanoma) |
|
|
Asymptomatic 60 yo with a 3cm mobile non-obstructing excavating mass in the distal ileum. Most likely diagnosis?
A Carcinoid B Lymphoma C Adenocarcinoma D Melanoma E Crohn's disease |

Lymphoma
Excavating mass of the TI is a buzzword for lymphoma -Most common malignant SB tumor -Mets most common in melanoma and carcinoid |
|
|
|
Asymptomatic 30 yo with 3 cm pedunculated mass lesion in the terminal ileum. No mention of obstruction or excavation. Most likely diagnosis?
A. lymphoma B. adenocarcinoma C. carcinoid D. adenoma E. inflammatory fibroid polyp |
Carcinoid
-Most common primary small bowel tumor beyond ligament of Treitz -Appendix > ileum > duodenum > other sites -90% of small bowel carcinoids arise in distal ileum -Duodenal and jejunal carcinoids have ↑ prevalence in MEN1 (multiple endocrine neoplasia) -Carcinoid syndrome = metastatic spread to liver -Spectrum of symptoms (flushing, diarrhea, asthma, pain, right heart failure) -In-111 octreotide or somatostatin receptor scintigraphy |
|
|
|
MOST associated with Whipple’s disease?
a. Calcific densities in the liver b. High density large spleen c. Low attenuation periaortic lymph nodes d. Low attenuation densities in the colon e. Scattered, isodense areas in the pancreas |
Low attenuation paraaortic lymph nodes
Whipple Disease -Rare systemic bacterial disease leading to chronic diarrhea and malabsorption -Thickened proximal small bowel folds and low-density mesenteric adenopathy -Low-density (near fat), large mesenteric and retroperitoneal nodes |
|
|
|
Patient p/w hypotension and hematemesis. First line of management?
A. Tagged RBC scan B. Upper endoscopy C. Angiography D. CT abdomen E. UGI |
Upper endoscopy
Angiography may be useful if bleeding persists and endoscopy fails to identify a bleeding site. |
|
|
|
Definitive treatment for recurrent GI bleeds due to gastric varices in a young women with isolated splenic vein thrombosis (secondary to pancreatitis)?
a. Splenectomy b. Splenorenal shunt c. Portocaval shunt d. Mesocaval shunt e. TIPS f. Anticoagulate g. Partial gastrectomy |
Splenectomy
Symptomatic sinistral portal hypertension is best treated by splenectomy |
|
|
|
% maliancy risk of 15mm colon polyp?
a. 2% b. 10% c. 35% d. 50% |
10%
< 1cm: 1%. 1-2 cm: 25%. >2 cm: > 40% recommend polypectomy at colonoscopy if > 1cm |
|
|
|
LEAST likely liver lesion to be echogenic:
a. Lymphoma b. Hemangioma c. Focal fat |
Lymphoma
Lymphoma is typically hypoechoic and can mimic a cyst on US. |
|
|
|
Barium swallow shows a 1.5 cm sac anterolaterally and inferior to the cricopharyngeus muscle (anterolateral outpouching filled with barium). Most likely etiology?
a. Killian Jamieson diverticulum b. Zenkers diverticulum c. Lateral pharyngeal diverticulum |

Killian-Jamieson diverticulum
-originates at anterolateral wall of proximal cervical esophagus off midline -below the cricopharyngeus -lateral to the longitudinal tendon of the esophagus |
Zenker’s diverticulum
between the fibers of the circopharyngeus muscle (at anatomical weak point) Lateral pharyngeal diverticula: -protrusions of pharyngeal mucosa through weaknesses in the pharyngeal wall -above the cricopharyngeus; seen in horn players |
|
|
TRUE regarding Zenkers diverticulum:
a. Occurs inferior to the cricopharyngeus b. Is a traction diverticulum c. Has a 5% risk of malignancy d. Posterior midline in the distal pharynx e. Empties with mild smooth muscular contraction |

Posterior midline in the distal pharynx
-occurs through the cricopharyngeal muscle -pulsion diverticulum |
Killian-Jamison diverticula are lateral and below the cricopharangeus muscle
|
|
|
MOST important when determining stage of (prognosis of) rectal cancer?
a. depth of invasion and nodal status b. depth of invastion, mets, and nodal status c. proximity to anus, nodal status, and depth of invasion d. size of tumor and nodal status |
Depth of invasion and regional LNs OR Depth, mets, and nodal status
-local extent of disease (i.e., depth of tumor penetration) independently influences survival -Regional lymph node involvement is one of the strongest predictors of outcome following surgical resection of rectal cancer, second only to distant metastasis |
|
|
|
MELD score includes which of following?
a. Serum albumin b. ALT c. Serum creatinine d. Ascites e. Hepatic encephalopathy |
Serum creatinine
MELD (Model ESLD) Score -INR -total bilirubin -serum creatinine |
After elective TIPS creation, patients with a MELD score of 18 or more have a significantly lower 3-month survival rate than do those with a MELD score of 17 or less.
|
|
|
MOST common location of gastric diverticula?
(a) proximal greater curvature (b) cardia (c) fundus |

Fundus
no treatment is usually needed probably congenital |
|
|
|
Which does NOT involve TI/cecum?
(a) Giardia (b) Yersinia (c) TB (d) Amebiasis (e) Lymphoma |
Giardia
Giardia affects the duodenum and jejunum |
Yersinia, TB, and amebiasis can cause an acute ileitis indistinguishable clinically from acute Crohn's ileitis.
|
|
|
Which is TRUE regarding giardiasis?
a. chronic bloody diarrhea b. may develop chronic malabsorption (in duodenum) c. most commonly gastroduodenal d. negative stool exam rules it out e. small bowel series shows abnormal ileum |
May develop chronic malabsorption
-an acute self-limited diarrhea (non-bloody) -chronic state of diarrhea, malabsorption and weight loss -involves duodenum and jejunum and spares ileum |
|
|
|
Most common location of GI lymphoma:
(a) esophagus (b) stomach (c) small bowel (d) colon (e) rectum |
Stomach
1. Stomach (75%). 2. Small bowel (including duodenum). 3. Ileocecal region. |
|
|
|
Endometriosis involving small bowel appears similar to which of the
following on barium studies? (a) metastatic melanoma (b) peritoneal metastases (c) pseudomyxoma peritonii |
Peritoneal metastases
Endometrial implants -rectosigmoid colon >appendix > cecum > distal ileum -puckering or a crenulated appearance of the affected wall |
|
|
|
Patient with enlarged spleen, signal dropout in liver and pancreas on T2 (hypointensity on T2). Patient has skin changes. Diagnosis?
a) primary hemochromatosis b) secondary hemochromatosis c) amyloidosis d) Wilson’s disease e) Gaucher’s disease |

Primary hemochromatosis
-in primary, liver has low signal due to iron overload of parenchymal cells -in severe cases, pancreas also has decreased signal -in secondary, the liver, spleen, and bone marrow are low due to iron overload in the RES (hemosiderosis) |
|
|
|
Patient presents with hyperglycemia, unusual skin pigmentation, esophageal varices. Most likely diagnosis:
A. Cirrhosis and pancreatitis B. Wilson’s Disease C. Hemochromatosis D. Alcoholic cirrhosis E. Waldenstrom macroglobulinemia |

Hemochromatosis
Primary -hyperpigmentation, -hepatomegaly (with cirrhosis later), -diabetes mellitus, -CHF, -arrythmia Secondary -arises from multiple blood transfusions |
|
|
|
Most reliable measurement (closest estimate) of the portal venous pressure:
(a) hepatic venous wedge pressure (b) hepatic venous free pressure (c) a+b (wedge + free) (d) a-b (e) b-a |
(d) Hepatic venous wedge pressure – hepatic venous free pressure
Hepatic venous-pressure gradient (HVPG) -accurate estimate of portal venous pressure -> 5 mm Hg is diagnostic of portal HTN -Splenomegaly and thrombocytopenia develop when HVPG > 5 mm Hg -Esophageal varices develops when HVPG > 12 mm Hg |
|
|
|
TRUE regarding appendiceal carcinoid?
(a) appendiceal carcinoid is mostly benign (b) results in left-sided fibroelastosis (c) few with carcinoid syndrome will have metastasis |
Appendiceal carcinoid is mostly benign
Tumors < 2 cm (95% of patients) are unlikely to have metastasized |
|
|
|
Which does NOT mimic achalasia?
(a) Chagas' disease (b) Severe diabetes (c) Dermatomyositis (d) Gastric tumor (e) Lung cancer |
Lung cancer (NOT achalasia mimic)
|
|
|
|
FALSE about enteric duplication cysts:
A. Muscular layer of bowel is more echogenic than mucosal layer on US B. Most common in terminal ileum C. May not communicate with bowel D. cysts containing ectopic gastric mucosa are more likely to be symptomatic than those without E. neurenteric cysts are associated with vertebral defects |
Muscular layer of bowel is more echogenic than mucosal layer on US (FALSE)
Enteric duplication cyst: -thin echogenic mucosa with thinner hypoechoic muscular layer -most common in jejunum and ileum -75% cystic with no communication with bowel Muscular layer of bowel is more echogenic than mucosal layer on US (FALSE) |
|
|
|
Low density in RLQ with calcifications:
a) mucocele of the appendix b) pseudomyxoma peritonei c) chronic appendicitis d) teratoma e) meconium peritonitis |

Mucocele of the appendix
|
|
|
|
NOT a post-BMT complication:
a) adrenal hemorrhage b) graft versus host disease c) hepatic veno-occlusive disease d) CMV e) splenic abscess |
Adrenal hemorrhage (NOT associated)
|
|
|
|
Pt with VHL has a lesion in the pancreas. What is the most likely pathology?
a) microcystic adenoma b) islet cell tumor c) pancreatic cyst d) pancreatic adenocarcinoma |

Microcystic adenoma
Von-Hippel Lindau -hemangioblastomas of cerebellum, spinal cord, retina, kidney -associated with RCC and pheochromocytomas |
|
|
|
NOT characteristic of microcystic adenoma of the pancreas:
A. Elderly women B. Heterogeneous mass with central stellate calcification C. High malignant potential D. Large low attenuation mass with numerous small cysts |

High malignant potential (NOT associated)
|
|
|
|
70 year old woman has a 5 cm mass in the pancreatic head that is hypovascular and contains central calcifications. This finding was present on a previous study five years ago. Most likely diagnosis?
A Pseudocyst B Microcystic adenoma C Pancreatic adenocarcinoma D Papillary pancreatic carcinoma E Mucinous cystadenoma/adenocarcinoma |

Microcystic adenoma
-benign neoplasm -of innumerable small cysts containing proteinaceous fluid -over age 60 -females |
|
|
|
Which syndromes has highest risk of malignancy?
a) Gardner’s syndrome b) Peutz-Jeugers c) Menetrier’s d) Juvenile polyposis |

Gardner’s syndrome
GI polyps progress to malignancy in almost 100% of patients in Gardner’s -osteomas -thyroid cancer -epidermoid cyst -fibromas -sebaceous cyst |
Juvenile polyposis does not have malignant potential
-bengin, hamartomatous GI tract polyps Peutz--Jeugers -benign hamartomatous polyps in the gastrointestinal tract -hyperpigmented macules on the lips and oral mucosao Menetrier's Disease -enlarged gastric mucosal folds -secretes massive mucus -most common after virus (CMV) or H. pylori |
|
|
Multiple segmental strictures of intra- and extra- hepatic biliary system (papillary stenosis). Most likely diagnosis:
a) AIDS cholangitis b) Primary sclerosing cholangitis c) Ascending cholangitis d) Recurrent pyogenic cholangitis |
Primary sclerosing cholangitis
-Autoimmune -ulcerative colitis, cirrhosis/ chronic hepatitis, pancreatitis, RP fibrosis -US: brightly echogenic portal triads - “String of beads” |
AIDS cholangitis
-looks like PSC but also shows papillary stenosis -If old recall states papillary stenosis, then AIDS cholangitis is in differential! |
|
|
Primary sclerosing cholangitis is associated with what disease?
A. ulcerative colitis B. sprue C. amyloidosis D. irritable bowel syndrome E. insulinoma |
Ulcerative colitis
|
|
|
|
In which would obtaining a CT with arterial and PV imaging be useful?
a. Metastatic transitional cell carcinoma b. HCC c. FNH d. Lymphoma |

HCC
early arterial enhancement and rapid washout |
|
|
|
On CT, small bowel protrudes lateral to rectus abdominus muscle. What hernia?
a. Spigelian hernia b. Richer’s hernia c. Obturator hernia |

Spigelian hernia
-an acquired ventral hernia through the linea semilunaris -through the internal oblique muscle, beneath the external oblique |
|
|
|
Match each of the following hernias:
1. Spigelian 2. Richter 3. Obturator 4. Paraduodenal A. Involves part, but not all of the bowel B. Semilunar line (lateral margin of rectus sheath) C. Congenital and diaphragmatic D. Associated with leg pain on hip flexion E. Inferior mesenteric vein |
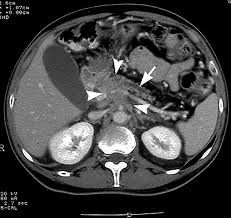
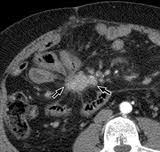
1-B, 2-A, 3-D, 4-E
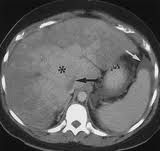
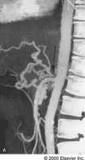
Paraduodenal hernias -Most occur on the left -dilated small bowel loops in LUQ lateral to ascending duodenum, indenting posterior gastric wall and distal transverse colon -IMV and ascending left colic artery lie in anteromedial border of a left paraduodenal hernia CT scans show an encapsulated bowel loop (black arrows) in the left paraduodenal fossa. The inferior mesenteric vein (arrowheads) is displaced anterolaterally by the bowel loop and joins the SMV through the root of the SBM. |
Richter’s
-entraps the antimesenteric border of the bowel, classically in older women with femoral hernias |
|
|
30 yo F with nonbloody diarrhea, abdominal pain, serum protein of 4.5. UGI+SBFT shows dilated loops, hyperseccretion, thickened folds, and intussusception appearance. Diagnosis?:
a. Sprue b. Yersinia infection c. Scleroderma d. Crohn’s disease e. Whipple’s disease |

Sprue
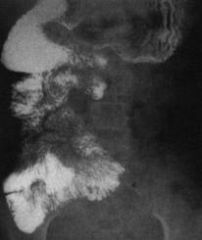
-Most common small bowel disease producing malabsorption syndrome -Reversal of jejunoileal fold pattern (blunted jejunal folds) CT -Circumferential wall thickening of jejunum -possible intussusception -"bubbly" duodenum Celiac disease with a bubbly bulb. There are multiple hexagonal filling defects in the duodenal bulb and thickened, irregular folds in the descending duodenum as a result of associated duodenitis. |
Whipples Disease
-does not have SB dilation -reversal of the jejunoileal fold pattern Scleroderma -flaccid, dilated bowel, no fold thickeining -"hidebound" appearance of SB - thinned folds are tethered together |
|
|
Which is NOT typically seen with sprue?
A Hypersecretion B Folds greater than 4mm C Villous atrophy on biopsy D Asymptomatic intussusceptions E Moulage pattern on barium study |

Folds > 4 mm (NOT associated)
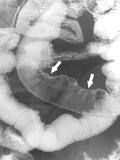
Fluoroscopic-guided enteroclysis -More accurate than SBFT in diagnosing celiac disease Jejunal folds -Decreased number of proximal jejunal folds (< 3/inch; normal: ≥ 5/inch) -Increased separation and absence of folds; "ileal" appearance Ileal folds - Increased number of folds in distal ileum (4-6/inch; normal: 2-4 /inch) - Increased fold thickness ≥ 1 mm: "Jejunization" of ileum in 78% of cases - Mosaic pattern: Due to total villous atrophy -1-2 mm islands of mucosa surrounded by barium-filled grooves Duodenal changes -Decreased number and irregular folds, especially in distal duodenum -"Bubbly" duodenum: Nodular pattern in mucosa CT -Circumferential wall thickening of jejunum -+/- intussecption Right posterior oblique spot image from enteroclysis in patient with celiac disease shows markedly decreased number of folds per inch of jejunum (black arrows) with increased number of ileal folds (white arrows), producing a “flip-flop” pattern. |
|
|
|
Characteristics of a hepatic hydrothorax?
a. Occurs more commonly on the left b. Can occur even with minimal ascites c. The presence of cirrhosis is not necessary |
Can occur even with minimal ascites
-Seen with continuous peritoneal dialysis -pleural effusion in cirrhotic patients in the absence of primary cardiac or pulmonary disease is most likely a hepatic hydrothorax -majority right-sided -transudative |
|
|
|
Bowel LEAST likely to become ischemic?
a. Rectum b. Hepatic flexure c. Splenic flexure d. Cecum |
Rectum
Dual blood supply |
|
|
|
MRI of liver shows a lesion isointense to spleen on T1 and T2. What is it?
a) Hemangioma b) Adenoma c) Metastasis d) HCC e) FNH |
Metastasis
|
|
|
|
During ERCP, the pancreatic acini are dilated/filled. Which is TRUE?
a. The patient has chronic pancreatitis b. The patient has an IPMT c. The patient has ductal stones d. Acinar dilatation is a complication of ERCP that will result in pancreatitis |
Acinar dilatation is a complication of ERCP that will result in pancreatitis
Overdistention of the pancreatic duct during ERCP causes acinarization of the pancreas, which leads to ERCP induced pancreatitis. |
|
|
|
Most common complication from ERCP:
a. duodenal perforation b. pancreatitis c. bile duct perforation d. hemorrhage |
Pancreatitis (if cholangitis is not an answer choice)
-most common complication is cholangitis (not a choice) -second more common is pancreatitis |
|
|
|
Which liver metastases is NOT typically hypervascular?
a) Melanoma b) Islet cell c) Bronchogenic carcinoma d) Thyroid e) Renal |
Bronchogenic carcinoma (NOT hypervascular)
Hypervascular mets: -RCC -thyroid -carcinoid -breast -melanoma -islet cell -choriocarcinoma -ovarian cystadenocarcinoma -sarcoma -pheochromocytoma |
|
|
|
What happens in Boorhave’s syndrome?
a) pneumomediastinum is early CXR findin b) use barium to diagnose |
Pneumomediastinum is early CXR finding
|
|
|
|
Linitis plastica most likely secondary to:
a) breast cancer b) lung cancer c) prostate cancer |

Breast cancer
Linitis plastica -Refers to a rigid, nondistensible, "leather bottle" stomach Usually due to one of 3 etiologies * Gastric carcinoma * Metastases to stomach (especially breast cancer) * Caustic gastric injury |
|
|
|
Most specific/characteristic of bowel malrotation on a barium enema:
a. Duodenal-jejunal junction inferior and medial (inferior medial displacement of the duodenal-jejunal junction) b. Cecum elevated and medial to its normal position c. Jejunum within the right abdomen d. Twisted fundus e. Sigmoid volvulus |
Duodenal-jejunal junction inferior and medial (inferior medial displacement of D-J junction)
-SMA is to the right of SMV, -large intestine is on the left, -small intestine is on the right |
|
|
|
Woman w/ abd pain; scan shows hepatic artery filling from collaterals from gastroduodenal artery. Diagnosis?
a. congenital anomaly/normal variant b. FMD of celiac artery c. Atherosclerosis of celiac artery d. Median arcuate ligament compression e. Portal hypertension |
Median arcuate ligament compression
-celiac artery compression from the median arcuate ligament of the diaphragm |
|
|
|
20 minute delayed abdomen CT is most useful for which of the following?
a. Cholangiocarcinoma b. Neuroendocrine tumor of pancreas c. Hypervascular liver metastasis d. RCC |

Cholangiocarcinoma
Most lesions show tumor enhancement 8 to 15 minutes after contrast medium injection. |
|
|
|
More common proximally versus distally:
a. Lymphoma b. Adenocarcinoma c. Meckel’s diverticulum d. Carcinoid e. Crohn’s disease |
Adenocarcinoma
Lymphoma is most common in the distal ileum |
|
|
|
15 year old Asian male presents with bleeding esophageal and gastric varices and normal LFT’s. Most likely underlying disease:
a) Schistosomiasis b) Hepatoblastoma obstructing portal vein c) Congenital hepatic fibrosis d) Budd-Chiari syndrome |
Schistosomiasis
CT: -"Tortoise shell" or "turtle back" appearance -Periportal fibrotic bands and widened fissures -Capsular calcification (parallel or perpendicular to liver surface) -Portal hypertension in advanced disease |
|
|
|
Patient with isolated gastric varices (no esophageal varices). Most likely cause?
A. portal vein thrombosis B. splenic vein thrombosis C. superior mesenteric vein thrombosis |
Splenic vein thrombosis
Portal vein thrombosis gives both gastic and esophageal varices |
|
|
|
TRUE regarding plain film findings of suspected appendicitis:
a) an appendicolith is more likely to be associated with perforation b) loss of properitoneal fat strip is specific c) appendicoliths are visulized>30% of time d) visualization of an air-filled appendix is specific for appendicitis |
An appendicolith is more likely to be associated with perforation
because it is more likely to obstruct the lumen |
|
|
|
The ligamentum teres represents the:
a. Obliterated umbilical vein b. Falciform ligament c. Obliterated ligamentum venosum |

Obliterated umbilical vein
|
|
|
|
Most common metastasis to the spleen is:
a) Breast b) Lung c) Colon |
Lung
|
|
|
|
Immunocompromised with odynophagia and numerous ulcers present in mid-esophagus. Likely etiology?
a. CMV b. HIV c. Candida d. Herpes |

Herpes
-discrete, superficial ulcers -mid to distal eso -Immunocompromised Candida - ulcers associated with diffuse plaque, "shaggy" eso -Immunocompromised Drug-induced -Discrete, superficial ulcers; occasional giant, flat ulcers -Mid-esophagus near aortic arch, L bronchus CMV,HIV -One or more giant, flat ulcers Radiation -Superficial or deep ulcers Double-contrast esophagram shows small, discrete ulcers (arrows) in the midesophagus |
|
|
|
NOT associated with large (>3cm) esophageal ulcers?
A. Esophageal CA B. Herpes C. CMV D. HIV E. Melanoma metastasis |

Herpes (NOT associated)
Herpes -discrete, superficial ulcers -mid to distal eso -Immunocompromised Candida - ulcers associated with diffuse plaque, "shaggy" eso -Immunocompromised Drug-induced -Discrete, superficial ulcers; occasional giant, flat ulcers -Mid-esophagus near aortic arch, L bronchus CMV,HIV -One or more giant, flat ulcers Radiation -Superficial or deep ulcers |
|
|
|
Regarding esophageal ulcers:
A More likely in the immunocompromised B Herpes more common than Candida C Long segment strictures |
More likely in the immunocompromised
Candida esophagitis is the most common cause of infectious esophagitis. |
|
|
|
TRUE regarding pancreatic divisum?
a. rare congenital anomaly b. dorsal part drains at major papilla c. most common cause of pancreatitis d. pancreatitis associated with it is due to stenosis of minor papilla |
Pancreatitis associated with it is due to stenosis of minor papilla
most common congenital anomaly small ventral duct, or duct of Wirsung, drains via the major papilla large dorsal duct, or duct of Santorini, drains via minor papilla recurrent pancreatitis |
|
|
|
Which of the following is associated with Cronkhite-Canada syndrome?
a. dysplastic nails b. buccal and oral lesions c. osteomas d. intussusception |
Dysplastic nails
Cronkite-Canada syndrome is a generalized polyposis syndrome associated with characteristic ectodermal changes. The small, sessile hamartomatous polyps are found in the stomach, small bowel, and colon. brown macules or confluent areas of hyperpigmentation are seen on the skin, particularly involving the hands and feet dystrophic changes in the nails Gardner's syndrome is associated with osteomas of the calvarium and mandible, as well as ampullary carcinoma. Peutz-Jeughers syndrome is associated with mucocutaneous lesions of the buccal mucosa, palms and soles. |
|
|
|
TRUE regarding epidermoid cysts within the spleen:
A. Due to trauma B. Echinococcal origin C. Contains trabeculations D. Hyperdense on CT E. Congenital |
Contains trabeculations
Cyst wall trabeculation or peripheral septa were found in 86% |
|
|
|
Associated w/ gastric MALT lymphoma?
a. Zollinger-Ellison syndrome b. H. pylori c. Menetrier’s disease d. Eosinophilic gastritis e. Lymphoid hyperplasia |
H. pylori
MALT lymphomas arise in areas of gastritis associated with H. pylori infection. |
|
|
|
FALSE regarding gallbladder cancer:
a) intraluminal polypoid lesion is the most common finding b) gallstones are commonly found at the time of surgery c) direct invasion into the surrounding liver is possible d) is usually seen in older (female) patients |
Intraluminal polypoid lesion is the most common finding (FALSE)
The most common sonographic appearance for gallbladder cancer is a soft tissue mass centered in the gallbladder fossa that completely or partially obliterates the lumen. The least common form of gallbladder cancer is a polypoid intraluminal mass. |
|
|
|
50 year old man with LLQ pain. CT shows a fatty mass next to the descending colon with surrounding fatty infiltration:
a) appendigitis epiploica b) retroperitoneal lipoma c) retroperitoneal lipomasarcoma d) mesenteric infarction |
Appendigitis epiploica
|
|
|
|
TRUE regarding gastric leiomyosarcoma:
A Large necrotic mass with ulceration (frequently contains areas of necrosis and calcification) B Worse prognosis than gastric adenoCA C Broad based exophytic mucosal mass D Metastasizes by lymphatics |
Large necrotic mass with ulceration (Frequently contains areas of necrosis and calcification)
Leiomyosarcomas are uncommon neoplasms, constituting only 1-3% of all malignant tumors in the stomach. These smooth muscle tumors are often confined to the wall of the stomach for prolonged periods before invading adjacent structures, so they have a better prognosis than gastric adenocarcinomas. They often contain large cystic cavities or ulcers because of hemorrhage or necrosis of the tumor. They metastasize hematogenously. |
|
|
|
NOT associated with reflux esophagitis?
A. mucosal granularity B. small ulcerations C. pseudodiverticulosis D. raised plaque-like lesions E. strictures F. motility disturbance |
Raised plaque-like lesions (NOT associated)
Thickened folds, limited distensibility, abnormal motility, mucosal plaques & nodules, erosions & ulceration, localized strictures, & intramural pseudodiverticulosis. |
|
|
|
TRUE regarding splenic aneurysms?
A. never presents as a pulsatile mass B. more common in males C. rarely calcify D. can be secondary to PAN |
Can be secondary to PAN
Known association between PAN and splenic artery aneurysms. also associated with FMD. Splenic aneurysm 2/3 of the time calcify, M: F 1:2 commonly present as pulsatile mass but usually asymptomatic Most likely to rupture in pregnancy |
|
|
|
TRUE about splenic aneurysm:
a. Rarely calcify b. Male > female c. Usually present w pulsatile mass d. Most likely to rupture in pregnancy e. Commonly result from PAN |
Most likely to rupture in pregnancy
associated with PAN and FMD Most likely to rupture in pregnancy Splenic aneurysm 2/3 of the time calcify M: F 1:2 commonly present as pulsatile mass but usually asymptomatic |
|
|
|
Patient with HIV has target lesions in the spleen. What is the most likely cause?
A. fungal infection B. lymphoma C. MAI D. NHL |
Fungal infection
|
|
|
|
TRUE regarding acute pancreatitis:
A. Fluid collections are common B. Focal form is more common than diffuse C. Hereditary form is recessive D. Chronic pancreatitis is associated with gallstones E. Acute interstitial pancreatitis commonly leads to chronic pancreatitis F. The pancreas becomes atrophic proximal to obstructing stone |
Fluid collections are common with acute pancreatitis
Fluid collections and gallstones associated with acute pancreatitis, not chronic. Diffuse 52%, focal 48%. Head/Tail ratio of 3:2. Hereditary form is AD. |
|
|
|
LEAST associated with colon cancer?
A. breast cancer B. prostate cancer C. previous polyp D. family history of colon cancer E. inflammatory bowel disease F. ovarian cancer |
Prostate cancer (LEAST associated)
All the others are mentioned in Dahnert as risk factors |
|
|
|
TRUE regarding bile salt resorption?
A. undergoes active reabsorption in TI B. undergoes passive reabsorption in TI C. undergoes active reabsorption in jejenum D. undergoes passive reabsorption in jejenum E. undergoes passive resorption in colon |
Undergoes active reabsorption in the terminal ileum
Conjugated bile salts are reabsorbed in the ileum via active transport. |
|
|
|
NOT associated with peptic ulcers?
A. Rheumatoid arthritis B. aspirin C. H. pylori D. Menetrier's E. steroids F. Zollinger-Ellison syndrome |
Menetrier's
Menetrier’s disease is hypertrophic gastritis characterized by giant mucosal hypertrophy,hypoproteinemia,& hypochlorydia RA patients do get peptic ulcer disease but it is secondary to steroids or NSAIDS |
|
|
|
What does NOT abut liver caudate lobe?
A. left lobe B. right lobe C. ligamentum teres D. fissure for the ligamentum venosum E. inferior vena cava |
Ligamentum teres
Adjacent structures of the caudate lobe of liver include IVC(posterior aspect), fissure for ligamentum venosum (separates left lobe and caudate), left and right lobe. Fissure for ligamentum teres divides left hepatic lobe into medial and lateral segments. |
|
|
|
LEAST common metastasis to esophagus:
A. carcinosarcoma B. melanoma C. breast |
Carcinosarcoma
|
|
|
|
Elderly male patient with diabetes, acute colicky abdominal pain, and tarry stools. Plain film shows single dilated loop of bowel assoc w/ segment of straightened, thick-walled bowel. Diagnosis?
A. short segment ischemia B. generalized ischemic colitis C. Crohn's/regional enteritis D. C. difficile colitis E. Yersinia colitis F. Strangulated internal hernia |
Short segment ischemia
Focal segmental ischemia is nongangrenous ischemic bowel disease caused by hypoperfusion of the gut wall microcirculation. It is different from mesenteric ischemia in that it is not in a specific distribution of a major mesenteric vessel. Makes sense in a guy with diabetes who has vascular disease. |
|
|
|
50yo man presents with bloody stools after acute onset of abdominal pain. Films shows thickened folds of the transverse colon. Diagnosis?
A Ischemic colitis B Pseudomembranous colitis C Ulcerative colitis D Granulomatous colitis |
Ischemic colitis
Mesenteric ischemia classically presents with abdominal pain, rectal bleeding, and thumbprinting (thickened folds). |
|
|
|
Regarding esophageal leiomyomas:
a. most common in mid- to distal-esophagus b. most common esophageal tumor c. commonly produce obstructive symptoms d. frequently transform into leiomyosarcoma e. frequently ulcerate |
Most common in mid- to distal- esophagus
Benign neoplasms of the esophagus are rare. Leiomyomas are the most common benign tumors of the esophagus. Leiomyomas are most often found in the mid to distal esophagus. They infrequently transform into leiomyosarcomas. |
|
|
|
Clonorchis is most associated with:
a. Caroli’s disease b. Cholangiocarcinoma c. Gallbladder carcinoma d. Primary sclerosing cholangitis |
Cholangiocarcinoma
The Clonorchis sinensis worm is acquired by ingesting raw fish, mostly in Southest Asia. The worms develop in the bile ducts, where they can cause Oriental cholangiohepatitis/recurrent pyogenic cholangitis. There is also an increased risk of cholangiocarcinoma. |
|
|
|
TRUE concerning colonic lipomas:
A. More common in obese women B. More common in the distal colon C. Most common nonepithelial colon tumor D. Commonly associated with ulceration and hemorrhage |
Most common nonepithelial tumor of the colon
Lipomas are the most common benign nonepithelial tumors of the colon and rectum. They are multiple in up to 20% of cases, and are primarily seen in women and the elderly. no malignant potential, and they are usually asymptomatic Intussusception can occur |
|
|
|
Atrophy of liver lobe in porta hepatis cholangiocarcinoma is secondary to:
A. portal vein branch obstruction B. hepatic artery brach obstruction C. hepatic vein obstruction D. bilary duct obstruction |
Portal vein branch obstruction
Cholangiocarcinoma can cause atrophy of the involved hepatic lobe due to compression of the portal vein and biliary system. |
|
|
|
Which is characteristic of a 3 cm hepatic (cavernous) hemangioma? (two answers)
a. Demonstrates increased Doppler flow centrally (internally) b. Hyperechoic, well-defined lesion (variant states ill-defined, shaggy borders) c. Increased uptake on sulfur colloid d. Most commonly occur in left lobe of liver e. Slight acoustic enhancement (increased through transmission) |
Hyperechoic, well-defined lesion; increased through transmission
usually do not show internal flow have decreased uptake on sulfur colloid scan 75% of hemangiomas also have posterior acoustic enhancement that is correlated with hypervascularity In large hemangiomas, heterogeneous areas are interspersed within the hyperechoic mass. Enhanced through transmission in a hyperechoic lesion is virtually diagnostic and seen in 80%. Usually NO Doppler signal |
|
|
|
Most likely to mimic a liver cyst:
a. Lymphoma |
Lymphoma
Most common pattern of lymphoma in the liver is infiltrative diffuse without distortion of the architecture. It could also be mistaken for a cyst. |
|
|
|
Most likely to mimic a liver cyst:
a. Lymphoma |
Lymphoma
Most common pattern of lymphoma in the liver is infiltrative diffuse without distortion of the architecture. It could also be mistaken for a cyst. |
|
|
|
MOST hypoechoic liver lesion on US?
A. Lymphoma B. Hemangioma C. Colonic adenocarcinoma metastasis D. Melanoma E. Adenoma |
Lymphoma
Lymphoma is hypoechoic and homogeneous. FNH is iso or slightly hypoechoic, homogeneous. Adenomas are hyper (30%), hypo (20-40%), or mixed. Hemangioma – hyperechoic. Colon adeno ca – GI mets echogenic especially in fatty liver. Melanoma – a hypervascular met, which are echogenic. |
|
|
|
MOST likely to cause hypovascular metastasis to the liver?
a. carcinoid b. renal cell c. colon d. thyroid |
Colon
Adenocarcinoma metastases are hypovascular. Liver metastases: colon>stomach> pancreas> breast>lung. |
|
|
|
Waveform in the hepatic veins?
a. Biphasic b. Triphasic c. Irregular d. Monophasic |
Triphasic
Normal hepatic vein waveform is essentially triphasic with antegrade systolic and diastolic waves and a retrograde A-wave. |
|
|
|
Hepatomegaly, enlargement of the portal vein, and pulsatile flow in the portal vein:
A. Cirrhosis B. Hepatitis C. Budd-Chiari D. Heart failure |
Heart failure
Congestive heart failure can cause postsinusoidal portal hypertension and hepatomegaly. Pulsation in the portal vein flow is seen in tricuspid regurgitation. In cirrhosis the liver is usually small (the liver may be enlarged initially with nodular cirrhosis). Cirrhosis is the most common cause of sinusoidal portal hypertension. In Budd-Chiari, the liver can be enlarged. Flow in portal vessels may be reversed or diminished. |
|
|
|
Causes of delayed gastric emptying include all of the following EXCEPT?
A. post vagotomy B. hyperglycemia C. hypothyroidism D. Zollinger-Ellison syndrome |
Zollinger-Ellison syndrome
Delayed gastric emptying: diabetic gastroparesis, hypothyroidism, gastric ulcer, gastritis, connective tissue disorder (scleroderma, SLE), amyloidosis, post-surgical gastroparesis, pyloric stenosis/obstruction. Increased gastric emptying: dumping syndrome, hyperthyroidism, gastrinoma (Zollinger-Ellison), gastric motility medications. |
|
|
|
NOT characteristic of hepatic adenoma:
A. Propensity to hemorrhage B. Usually present with pain and a mass C. Can be differentiated from hepatocellular carcinoma on core biopsy D. Usually photopenic on Tc sulfur colloid scintigraphy E. Increased incidence with oral contraceptives |
Can be differentiated from HCC on core biopsy
Hepatic adenoma occurs almost exclusively in young women taking oral contraceptive pills. men who use anabolic steroids or in patients with glycogen storage disease Patients present with hepatomegaly or acute onset RUQ pain due to intratumoral hemorrhage. can regress after discontinuation of OCPS. Due to risk of rupture or malignant transformation, hepatic adenomas are surgically removed. Technetium-99m sulfur colloid scanning: hepatic adenomas tend to be cold because they do not contain Kupffer cells (the main functional cell of the reticular endothelial system that takes up colloid). Adenomas are not biopsied but excised due to similar histology to HCC. |
|
|
|
FALSE concerning colonic polyps?
a. Hyperplastic polyps rarely premalignant b. Colonic neoplasia follows adenoma to carcinoma hypothesis c. Villous adenomas arise from epithelium d. Tubular adenomas arise from mucus cells e. Tubulo-villous polyps are the least likely polyps to become malignant |
Tubulo-villous polyps are the least likely polyps to be malignant (FALSE)
the risk of carcinoma within a polyp is related to proportion of villous change. Thus, tubulovillous adenomas are intermediate between tubular and villous polyps in their risk of invasive carcinoma. |
|
|
|
Colorectal screening starts at age 50 in:
A. Ulcerative colitis patients B. Strong family history C. Normal asymptomatic people with no known risk factors D. Positive occult stool |
Normal asymptomatic people with no known risk factors
|
|
|
|
Drug most likely to be associated w/ large benign greater curvature antral ulcer?
a. Morphine b. Prednisone c. Aspirin d. Potassium chloride |
Aspirin
NSAIDS and aspirin are associated with gastritis, usually located in the antrum and body, and can result in benign ulcerations. NSAID induced ulcers commonly occur on the greater curvature because of gravity. |
|
|
|
TRUE regarding hepatic fluid collections:
a. Amebic abscesses are not amenable to surgical or percutaneous drainage b. Hepatic abscesses are cryptogenic in 80% c. Echinococcus granulosus is the causative organism of cystic hydatid disease d. Multilocular collections cannot be treated percutaneously |
Echinoccus granulosus is the causative organism of cystic hydatid disease
Echinococcus granulosus is the organism responsible for producing hydatid cysts. Hepatic abscesses are cryptogenic 45% of the time. Multilocular collections are less likely to be successfully drained percutaneously than non-septated collections but they can still be treated with drainage. While metronidazole is first line of treatment for amebic abscesses, they are amenable to surgical or abscess drainage. |
|
|
|
Does NOT commonly involve the small bowel in patients with AIDS?
A Cryptosporidium B MAI C Candida albicans D CMV |
Candida albicans (NOT associated)
Candida typically infects the oral cavity and the esophagus. Mycobacterium avium complex infection is most commonly jejunal. CMV locations: Colon > small bowel (terminal ileum) > esophagus > stomach. Cryptosporidiosis locations: Jejunum > the rest of the small bowel > stomach > colon. |
|
|
|
What are areae gastricae?
A Normal gastric folds B Response to hypertrophic gastritis C Parietal cells D Precursor to malignancy E Reaction to peptic ulcer disease |
Normal gastric folds
The area gastricae are 1-5 mm tufts of gastric mucosa separated by a reticular network of shallow grooves thus creating a detailed pattern of the gastric mucosal folds as demonstrated on double-contrast examination of stomach. This is a normal pattern. These may become thickened secondary to H. pylori gastritis. |
|
|
|
20 y/o black man with hepatomegaly, diarrhea and peripheral edema. Dense bones on plain film. Most likely diagnosis:
A Lymphoma B Mastocytosis C Carcinoid D Gardner syndrome E Scleroderma |
Mastocytosis
hepatosplenomegaly, diarrhea, steatorrhea, and sclerotic bone lesions Urticaria pigmentosa is the classic skin finding. clinical features relate to histamine release with local urticaria, flushing, shocklike episodes, diarrhea, and vomiting In the GI track, mastocytosis usually causes thickened small bowel folds with nodules, episodic diarrhea, and peptic ulcer disease. |
|
|
|
Specific finding in portal hypertension?
A Enlarged portal vein B Enlarged hepatic vein C Portosystemic collaterals D Ascites E Splenomegaly |
Portosystemic collaterals
|
|
|
|
MOST characteristic of Crohn’s disease?
A Asymmetrical mural wall involvement B Continuous involvement of colon and SB C Involves SB and colon >50% D Frequently involves duodenum E Jejunal involvement > ileal involvement |
Asymmetric mural wall involvement
classic description of Crohn’s disease are skip areas of asymmetric bowel wall thickening preferentially involving the mesenteric side involves the colon and TI 50-55% only small bowel 30% only colon 15% |
|
|
|
Hepatic lesions which are near-water density w/ central area of higher density that enhances brightly. Diagnosis?
A Caroli's disease B AVM C HCC |
Caroli’s disease
The “central dot” sign of Caroli’s disease: the dilated segment of bile duct surrounds the adjacent hepatic artery and portal vein so that these vascular structures produce a small enhancing focus in the middle of a cystic attenuated dilated duct |
|
|
|
Enterocutaneous fistula from rectum and enterovaginal fistula. Diagnosis?
A Crohn's disease B Diverticulitis |
Crohn’s disease
Multiple fistulas likely represents Crohn’s. |
|
|
|
What divides right and left hepatic lobes?
A. RHV B. LHV C. MHV D. Falciform ligament |
Middle hepatic vein (divides right and left hepatic lobes)
Right and left lobes are separated by the major lobar fissure, defined by MHV. Right hepatic lobe divided into anterior and posterior segments by right intersegmental fissure, defined by RHV. Left hepatic lobe divided medial and lateral segments by left intersegmental fissure, defined by LHV, falciform ligament. Variant: The middle hepatic vein divides which structures? Answer: Right and left hepatic lobes |
|
|
|
High-density liver on CT likely due to:
A. Steatosis B. Chronic steroid use C. Amyloidosis D. Amiodarone E. Chemotherapy |
Amiodarone
DDX for high liver attenuation: amiodarone, hemachromatosis, glycogen storage disease, Wilson's disease, cisplatin, increased relative density in anemic patients. |
|
|
|
True of solid and papillary pancreatic carcinoma appearance?
A. Displacement of vessels B. Well circumscribed mass C. Hypoechoic to rest of the pancreas D. Involving primarily pancreatic head E. Pancreatic atrophy prox to ductal obstr |
Well circumscribed mass
low grade, non-endocrine malignant tumor of pancreas that usually arises in the tail large well-encapsulated heterogeneous mass with considerable cystic degeneration and hemorrhagic necrosis calcification in 33%; lesion is hypovascular, poor enhancement in solid components |
|
|
|
Which does NOT relax following glucagon administration:
A. Esophagus B. Stomach C. Duodenum D. Jejunum/ileum E. Colon |
Esophagus (NOT affected)
Glucagon is produced in alpha cells of pancreas and released by low blood glucose levels hypotonic affect on the duodenum>jejunum>stomach> colon releases catecholamines from the adrenal that paralyze intestinal smooth muscles It increases bile flow and relaxes gallbladder and sphinctor of Oddi. |
|

