![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
157 Cards in this Set
- Front
- Back
|
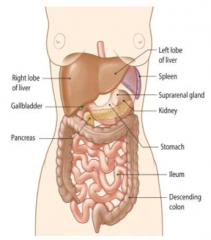
What is the largest glandular tissue in the body? Size? |
Liver |
|
|
What are the lobes of the liver? Which are the biggest? |
- Right |
|
|
What blood does the liver receive? Origin? |
Receives mainly venous blood, arriving directly from the spleen, pancreas, and intestine |
|
|
What are the implications of the liver receiving venous blood from the spleen, pancreas, and intestine? |
It is the first organ to encounter any ingested toxic substances as well as nutrients |
|
|
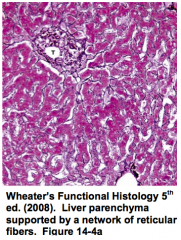
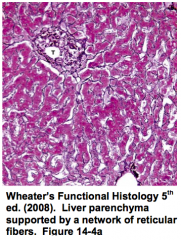
What kind of tissue makes up the liver? |
- Bulk is uniform parenchymal cells = hepatocytes |
|
|
What are the functions of the liver? |
- Detox metabolic waste products |
|
|
What are the two types of properties of the liver? How do they differ? |
Endocrine |
|
|
What happens to endocrine secretions from the hepatocytes? Which ones? |
- Directly enter the hepatic blood |
|
|
What compound is produced by hepatocytes to be released for exocrine function? |
Bile |
|
|
What are the four functional groups of liver components? |
- Connective tissue |
|
|
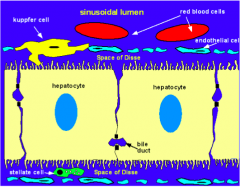
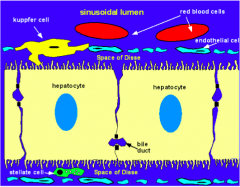
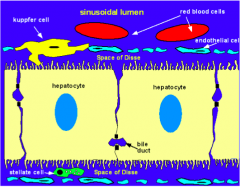
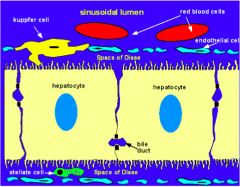
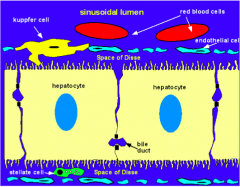
What surrounds the hepatocytes and sinusoids in the liver? |
Reticular fibers composed of Collagen Type III |
|
|
What is the only connective tissue in the lobules of the liver? Organization? Functions? |
Reticular Fibers made of Collagen Type III |
|
|
What is the origin of the reticular fibers (collagen type III) that surround hepatocytes and sinusoids? |
Stellate / Ito cells found in the Space of Disse |
|
|
Where are Stellate / Ito cells found? Function? |
- Space of Disse |
|
|
What can disrupt the reticular fiber network surrounding hepatocytes and sinusoids? How can you assess this? |
- Liver disease can cause disruption of this network |
|
|
What are the fiver major vessel systems in the liver? |
- Hepatic artery |
|
|
What is the function of the hepatic artery? Origin? |
- Carries oxygenated arterial blood into the liver |
|
|
What is the function of the hepatic portal vein? |
- Carries venous blood into the liver (high in nutrients) |
|
|
What is the function of the central veins? |
Carries blood away from the liver toward the hepatic veins and eventually into the IVC |
|
|
What is the function of the bile ducts? |
Transports bile from the liver |
|
|
What is the function of the lymphatic vessels in the liver? |
Carries lymph away from the liver |
|
|
What are the contents of the hepatic portal vein blood from the intestine? |
Nutrients and toxic substances |
|
|
What are the contents of the hepatic portal vein blood from the pancreas? |
Endocrine secretions like insulin and gluagon |
|
|
What are the contents of the hepatic portal vein blood from the spleen? |
Breakdown products of the blood cells |
|
|
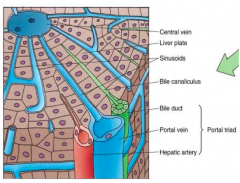
How does blood gain access to the hepatocytes? |
Arterial capillaries and inlet venules carry blood from the hepatic artery and portal veins into a network of sinusoidal capillaries (sinusoids) |
|
|
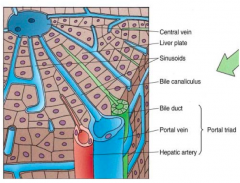
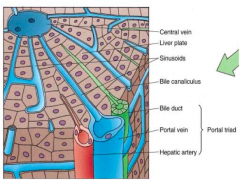
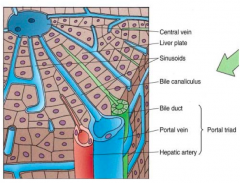
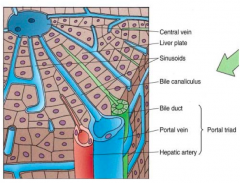
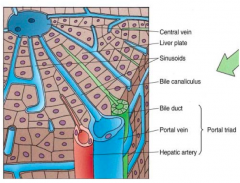
What is the portal triad? How much blood is contributed by these components? |
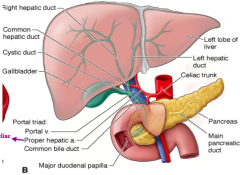
Combination of branches of: |
|
|
What is the flow of blood through the portal triad and the hepatocytes? |
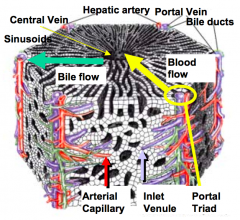
- Blood from hepatic arteries and portal veins flows through the sinusoids toward the central vein |
|
|
What kind of capillaries are in the hepatocytes? Function? |
Sinusoidal (type III) - allows the exchange of substances between the blood and hepatocytes |
|
|
What are the types of cells in the sinusoids of the liver? |
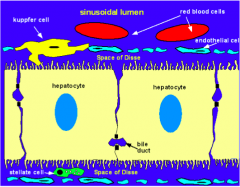
- Endothelial cells (sometimes called sinusoidal cells) |
|
|
What are Kupffer cells derivatives of? Function? |
- Monocytes (they are aka sinusoidal MACROPHAGES) |
|
|
Which cells are possibly involved in the breakdown of senile RBCs? |
Kupffer cells (aka sinusoidal macrophages) |
|
|
What are the characteristics of the endothelium lining the sinusoids? |
- Discontinuous to |
|
|
What is found within the sinusoidal lining? |
Large numbers of fenestrae that are arranged as sieve plates |
|
|
Where does exchange of substances between blood and hepatocytes take place? |
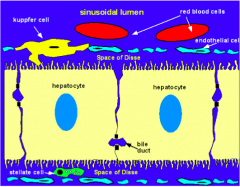
Peri-sinusoidal Space of Disse |
|
|
Where is the peri-sinusoidal Space of Disse? |
Lies between the basal surface of the hepatocyte and the sinusoid |
|
|
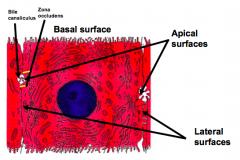
What special feature is found on hepatocytes? Function? |
Microvilli on basal surface which increases the surface area available for substance exchange |
|
|
Why do hepatocytes have microvilli? |
To increase the surface area available for substance exchange |
|
|
What is commonly found in the peri-sinusoidal Space of Disse? |
Stellate cells (Ito cells / adipose / lipocytes) |
|
|
What is the structure and function of Stellate cells (Ito cells / adipose / lipocytes)? |
- Commonly found in peri-sinusoidal Space of Disse |
|
|
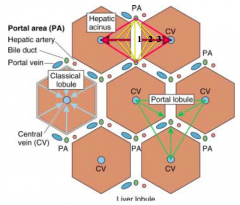
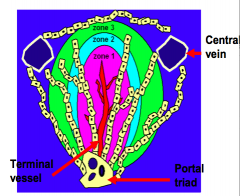
What is the term for the "functional units" of the liver? What are the types? |
Lobules: |
|
|
What is the shape of the Classic Lobule? Organization? |
- Hexagonal block of tissue |
|
|
How do you identify the classic lobule in pig livers? Human livers? |
- Pigs: presence of CT surrounding each lobule |
|
|
What is at the center of a classic lobule? |
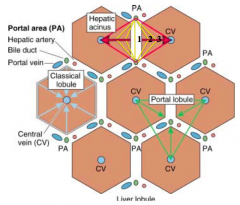
Single central vein |
|
|
What is at the corners of the hexagonal classic lobule? |
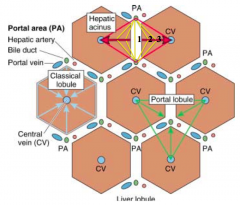
Portal triad: branches of the portal vein, hepatic artery, and bile duct |
|
|
What radiates from the central vein to the portal triad at each corner of the hexagonal classic lobule? |
Sinusoids and hepatic plates |
|
|
What is the shape of the liver acinus? Organization? |
- Lozenge shaped |
|
|
What does the liver acinus correlate with? |
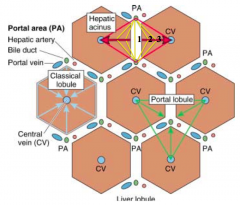
- Liver acinus closely correlates with blood perfusion, metabolic activity, and liver pathology |
|
|
What is the flow of oxygenated nutrient / toxin rich blood through the classic lobule? |
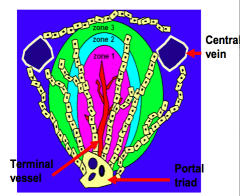
- Blood perfuses from the terminal vessel toward the central vein |
|
|
What is the organization of the zones in the acinus? |
Three concentric zones surrounding a terminal vessel |
|
|
How do the three zones of the acinus differ? |
Differ with respect to metabolic activity, glycogen storage, and presence of organelles |
|
|
Acetaminophen toxicity damages which part of the acinus? |
Zone 3 |
|
|
What is the principal functional cell of the liver? |
Hepatocyte |
|
|
How are hepatocytes organized? |
- Makes up the liver parenchyma |
|
|
What shape are hepatocytes? Size? |
- Large polyhedral cells |
|
|
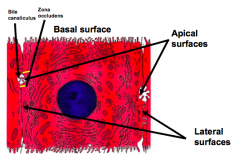
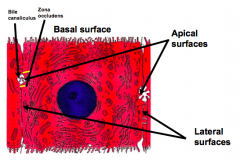
What do the peri-sinusoidal surfaces of hepatocytes face? |
They represent the basal aspect of the cell |
|
|
What sides of the hepatocytes face other hepatocytes? |
Lateral surfaces |
|
|
What sides of the hepatocytes face bile canaliculi? |
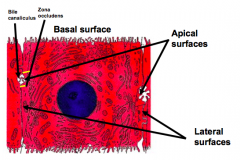
Apical surfaces |
|
|
Where does transfer of substances between sinusoids and hepatocytes occur? |
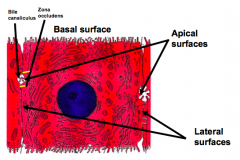
Across the basal surface (peri-sinusoidal surface) |
|
|
What is the shape/organization of the nuclei in hepatocytes? |
- Large spherical nucleus located in the center of the cell |
|
|
What are the features of the organelles in hepatocytes? |
- Extremely rich in organelles |
|
|
How can we prove that liver regeneration occurs? |
Partial hepatectomy (in rodents): |
|
|
What cells regenerate after a partial hepatectomy? |
All liver cell types: |
|
|
How long does the regeneration process from a partial hepatectomy take in rats? |
5-7 days |
|
|
How does liver regeneration occur in humans? |
- During regeneration, normal liver function is maintained |
|
|
What are the problems with hepatocyte transplantation? |
- Recovering enough normal donor hepatocytes that are acceptable by the host |
|
|
What would be the ideal way to transplant hepatocytes? |
- Isolate hepatic stem cells from an afflicted individual |
|
|
Where are oval cells found? Characteristics? |
- Rare population of cells present in the biliary epithelium |
|
|
What can oval cells become? Why? |
They can differentiate to form both biliary epithelial cells and hepatocytes because they are bipotential |
|
|
What happens during chronic liver damage when hepatocyte function and replication is severely compromised? |
Oval cells proliferate and differentiate |
|
|
How does bone marrow relate to oval cells? |
- Transplanted BM has been shown to give rise to oval cells |
|
|
More recently, what have pluripotent stem cells been derived from? How can this be used for liver regeneration? |
- Pluripotent stem cells have been derived from human fibroblasts |
|
|
What is the main exocrine function of the liver? |
Production of bile |
|
|
What are the functions of bile salts? |
- Emulsification - decreases surface tension and breaks fat globules into smaller size particles |
|
|
Where is bile produced? How is it excreted? |
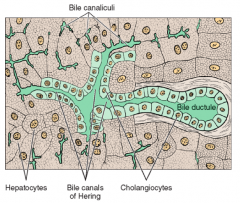
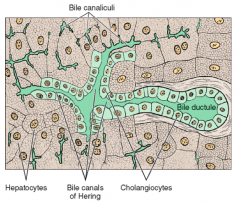
- Hepatocytes produce bile |
|
|
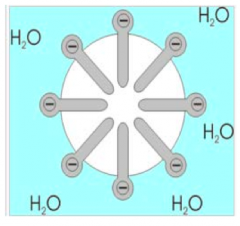
What is found in the bile canaliculi (where bile is excreted after being produced by hepatocytes)? |
ATPases - which means that bile secretion is an active process |
|
|
What is the organization of bile canaliculi? |
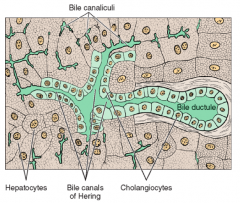
The canaliculi join together to form small terminal ductules called Canals of Herring |
|
|
What are bile ducts made of? |
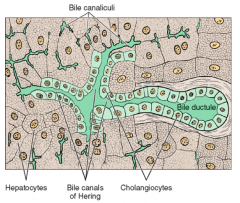
- Biliary epithelial cells |
|
|
How does bile flow compare to blood flow? |
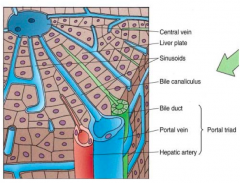
Bile flows in the opposite direction of the blood, i.e., away from the central vein toward the portal triad |
|
|
Where do bile ducts lead? |
Lead from the portal triad to join the hepatic duct that carries the bile to the gallbladder |
|
|
How much bile is secreted by the liver per day? |
1 L |
|
|
What is the function of the gallbladder? |
- Concentrates the dilute bile that comes from the liver 5-10x |
|
|
What stimulates gallbladder contraction and release of bile into the duodenum? |
- The presence of lipid in the duodenum induces secretion of the hormone CCK |
|
|
What is the function of CCK? |
Cholecystokinin-pancreozymin stimulates gallbladder contraction and forces concentrated bile out |
|
|
What is the shape/structure of the gallbladder? |
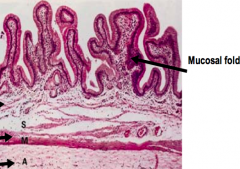
- Muscular sac |
|
|
What type of epithelium lines the gallbladder? Characteristics? |
- Mucosa made of simple columnar epithelial cells |
|
|
How are the cells of the epithelium in the gallbladder connected? |
Junctional complexes to produce a barrier between the luminal and intercellular compartments |
|
|
What is the function of the epithelium of the gallbladder? |
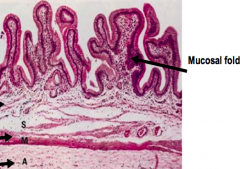
- Concentrate bile by actively absorbing water into a capillary rich network in the lamina |
|
|
How big is the adult pancreas? |
- 100-150 g |
|
|
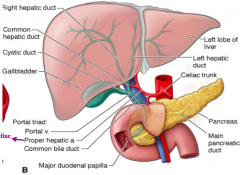
What are the parts of the pancreas? Location? |
- Head: nestles within the concavity of the duodenum, which is C-shaped |
|
|
What is the pancreas made of? |
- Highly lobular |
|
|
What is the path of the main pancreatic duct? |
Transverses the length of the pancreas and joins the common bile duct before entering the duodenum |
|
|
What are the functions of the pancreas? |
Exocrine (blue): |
|
|
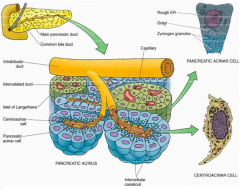
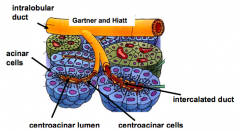
What is the organization of the exocrine pancreas? |
- Consists of densely packed Acini (blue) |
|
|
What is the organization of the endocrine pancreas? |
Consists of randomly distributed Islets of Langerhans (green) throughout the exocrine tissue (blue) |
|
|
What does the exocrine pancreas release? |
Enzymes involved in digestion in small intestine: |
|
|
What hormones are released when the duodenum contains food? Function? |
- Secretin |
|
|
How are digestive enzymes stored in the exocrine pancreas? |
Zymogen granules within the cytoplasm of acinar cells |
|
|
How are the zymogen forms of digestive enzymes activated? |
Proteolytic cleavage in the intestine |
|
|
How does the pancreas ensure there is no auto-digestion of its tissues? |
- Digestive enzymes exist in their proenzyme state (inactive) that only are activated in the intestine by proteolytic cleavage |
|
|
What is the functional unit of the exocrine pancreas? Shape? |
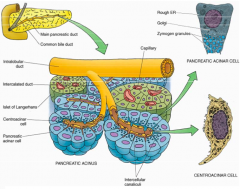
Acinus - roughly spherical containing 40-50 pancreatic acinar cells surrounding the lumen of a small ductule |
|
|
What induces acinar cells to secrete pancreatic enzymes into the lumen? |
Cholecystokinin, stimulated by fatty foods in the duodenum |
|
|
What is the organization and function of centroacinar cells? |
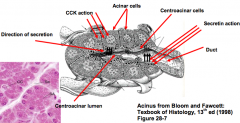
- Extend from the end of the duct into the acinus as a discontinuous epithelium |
|
|
What induces centroacinar cells to secrete the alkaline fluid component of pancreatic juice? |
Secretin |
|
|
What is the function of Cholecystokinin? |
- Results in gallbladder contraction and emptying in under 1 hour |
|
|
What is the function of Secretin? |
- Stimulates secretion of alkaline fluid, rich in sodium bicarbonate, from the centroacinar cells |
|
|
What is the importance of the alkaline fluid released from centroacinar cells? |
- Solubilization of zymogen granules |
|
|
What is the shape and organization of the acinar cells of the pancreas? |

- Pyramidal shape |
|
|
How are the zymogen granules released into the lumen? |
Exocytosis at the apical surface of the acinar cell |
|
|
How is pancreatic juice transported to the duodenum? |
Network of pancreatic ducts: |
|
|
What is the organization of the bile ducts in the liver and gallbladder? |
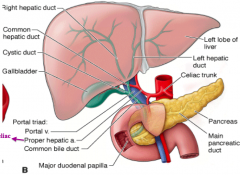
- R hepatic duct drains R lobe and L hepatic duct drains L lobe |
|
|
What does the round ligament separate? What is it a remnant of? |
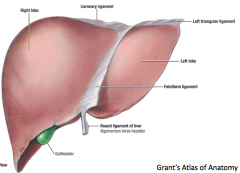
- Anatomically, the round ligament divides the left part of the liver into medial and lateral sections. |
|
|
What does the coronary ligament of the liver do? |
The coronary ligament of the liver refers to parts of the peritoneal reflections that hold the liver to the inferior surface of the diaphragm |
|
|
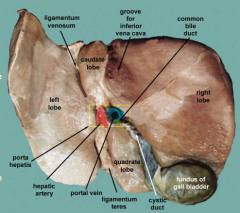
What is the porta hepatis? |
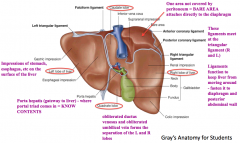
Gateway to the liver - where the portal triad enters the liver (portal vein, hepatic artery, and common bile duct) |
|
|
What separates the right and left lobes of the liver? |
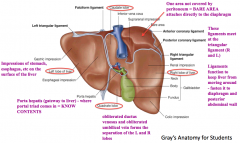
Obliterated ductus venosus and and obliterated umbilical vein |
|
|
What area of the liver is not covered in peritoneum? What does this part attach to? |
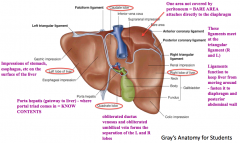
- The superior bare area on the right lobe |
|
|
What are the functions of the ligaments on the liver? |
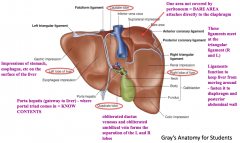
- Keeps the liver from moving around |
|
|
What is the function of the Left Triangular Ligament? |
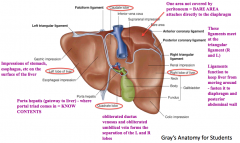
- Fold that connects the posterior part of the upper surface of the left lobe of the liver to the diaphragm |
|
|
What is the location and function of the Right Triangular Ligament? |
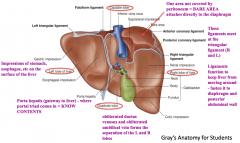
- Situated at the right extremity of the bare area |
|
|
If planning to resect part of the liver, how do you approach the task? |
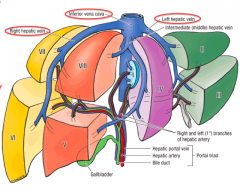
Hepatic Segments: based on arterial, venous, and biliary supply, in addition to the drainage of the liver |
|
|
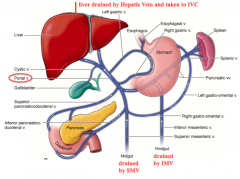
What drains the liver? |
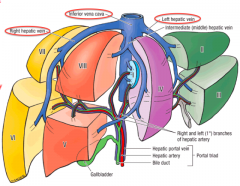
Hepatic veins (right, middle, and left) that empty into the IVC |
|
|
What separates the L and R lobes clinically? |
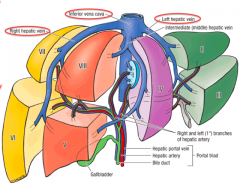
Middle hepatic vein |
|
|
What do the segments of the liver represent? |
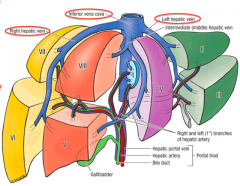
- Caudate lobe: segment 1 |
|
|
What is special about segment 1 of the liver? |
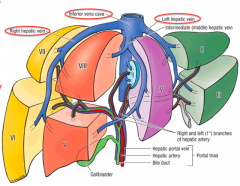
- Represents the caudate lobe |
|
|
If you are transplanting a liver, which segments do you take? |
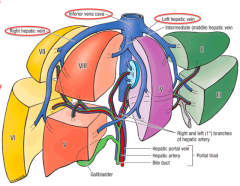
- Adult: R lobe (segments 5, 6, 7 and 8) |
|
|
What is the route of bile from the gallbladder to the small intestine? |
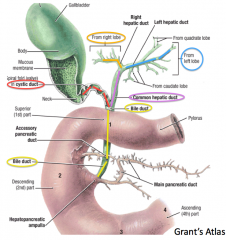
- Cystic duct drains gallbladder |
|
|
What is the flow of blood leaving the midgut? |
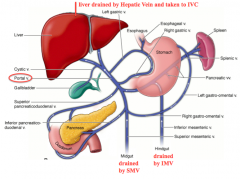
- Branches of Superior Mesenteric Vein |
|
|
What is the flow of blood leaving the hindgut? |
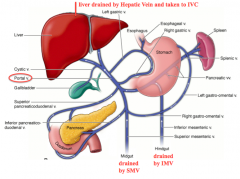
- Branches of Inferior Mesenteric Vein |
|
|
What can happen to the portal circulation if there is liver disease? |
Liver disease can cause blood flow to back up and reverse direction to the spleen, causing the spleen to enlarge |
|
|
How does fresh blood get to the liver? What percent of the blood comes via this route? |
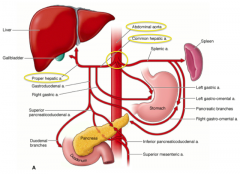
- Abdominal aorta supplies the Celiac Trunk |
|
|
Once blood enters the liver via the hepatic artery or the portal vein, how does it flow through the liver? |
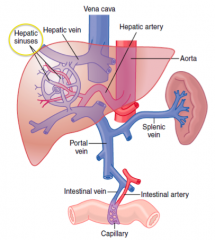
- The blood flows through the hepatic sinuses / sinusoids |
|
|
What kinds of cells line the bile canaliculi? |
Liver cell plates |
|
|
Where is the space of Disse? |
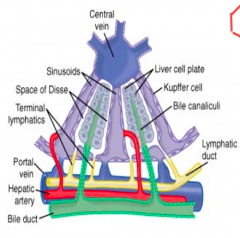
Located between the sinusoids and the liver cell plates that line the bile canaliculi |
|
|
How does the concentration of bile in the liver compare to that in the gallbladder? How does this change occur? |
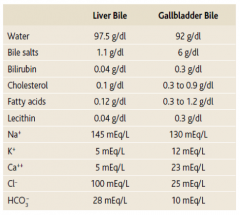
- Liver bile is more dilute than gallbladder bile |
|
|
What happens to the volume of bile that leaves the liver to that which is stored in the gallbladder? |
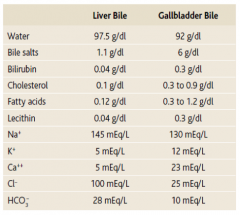
Volume goes from 500 mL to 50 mL via absorption of water, Na+, and Cl- |
|
|
What happens to cholesterol and lecithin in the gallbladder? |
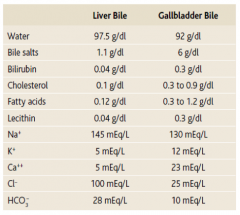
They are solubilized by bile salts |
|
|
Where are bile acids reabsorbed? |
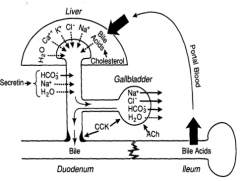
Ileum where they are taken via the portal blood back to the liver |
|
|
What enzymes are released by the pancreas to digest proteins? |
- Trypsinogen |
|
|
How are the enzymes released from the pancreas to digest proteins activated? |
- Trypsinogen is activated to Trypsin by Enterokinase |
|
|
What activates Trypsinogen to Trypsin? |
- Enterokinase |
|
|
What activates Chymotrypsinogen to chymorypsin? |
Trypsin |
|
|
What activates Procarboxypeptidase to Carboxypeptidase? |
Trypsin |
|
|
What prevents activation of the pancreatic enzymes? |
Trypsin inhibitor prevents activation until secretions reach the small intestine |
|
|
What are the three forms of carbohydrates in our diet? |
- Starches |
|
|
How do you digest starches? |
Starch → Maltose and 3-9 glucose polymers |
|
|
How do you digest lactose? |
Lactase from the intestine breaks Lactose down into Galactose and Glucose |
|
|
How do you digest Sucrose? |
Sucrase from the intestine breaks down Sucrose into Fructose and Glucose |
|
|
What is the form of the dietary fats? |
- Majority are Triglycerides (TG): glycerol nucleus + 3 FA side chains |
|
|
What digests Triglycerides? |
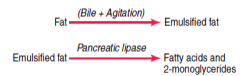
Pancreatic Lipase - can digest all TG it can reach within 1 minutes (requires emulsification by bile salts) |
|
|
What is the function of Pancreatic Lipase? |
Digests Triglycerides into Free Fatty Acids and 2-Monoglycerides |
|
|
How do you digest Phospholipids? |
Phospholipase |
|
|
How do you digest Cholester esters? |
Cholesterol Esterase |
|
|
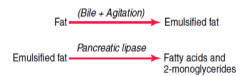
What happens to the digested fat remnants? |
Bile salts form micelles and remove monoglycerides and fatty acids and transports them to the brush border for absorption |
|
|
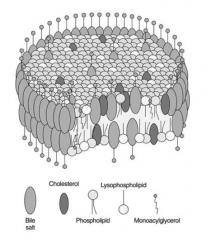
Where is bicarbonate secreted from? |
Bile ducts and pancreatic ducts |
|
|
How does bicarbonate get formed? |
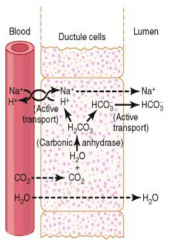
- CO2 diffuses in and combines with H2O to form H2CO3 |
|
|
Which hormone has the greatest effect on Sphincter of Oddi relaxation? |
Cholecystokinin |
|
|
In a 40-yo male with Hepatitis C, which hepatic acinus zone would be exposed to the greatest number of viral particles? |
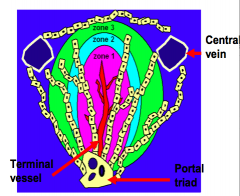
Zone 1 (this receives the greatest amount of blood flow) |
|
|
Which zone of the hepatic acinus would be affected most by ischemia? |
Zone 3 |

