![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
38 Cards in this Set
- Front
- Back
|
What is the significance of premature membrane rupture during pregnancy?
|
Already infected with pathogen or provides a clear pathway for infection (transcervical/ascending infection)
|
|
|
What is an Apgar score?
5 parameters? What does the one-min score predict? 5-min score? |
A clinically useful method of evaluating the physiolgic condition and responsiveness of a newborn infant, and hence her/his chances of survival.
Apperance (color) Pulse (HR) Grimace (response to nasal catheter) Activity (muscle tone) Respiratory effort 1min score - immediate action to be taken 5min score - one month mortality |
|
|
What are 4 risk factors for PPROM (preterm premature rupture of plancental membranes)?
Complications of PPROM? |
1. maternal smoking
2. prior preterm delivery 3. vaginal bleeding during pregnancy 4. poor maternal nutrition Complication: infection |
|
|
Define the following terms:
Chorioamnionitis Funisitis |
chorioamnionitis: inflammation of placental membranes
funisitis: inflammation of umbilical cord |
|
|
LIst 2 placental factors for fetal growth restriction (intrauterine growth retardation).
3 fetal factors? 2 maternal factors? |
placental factors - uteroplacental insufficiency, confined placental mosaicism.
Fetal factors - chromosomal disorders, congeital anomalies, congental infections (esp. TORCH group) Maternal factors - decreased placental blood flow (most commonly associated SGA) and maternal malnutrition |
|
|
What is the most common cause of respiratory distress in the neonates?
|
Hyaline membrane disease (neonatal respiratory distress syndrome)
|
|
|
What is the etiology and pathogenesis of neonatal RDS (hyaline membrane disease)?
|
etiology - pulmonary immaturity
pathogenesis - surfactant deficiency --> increased alveolar surface tension --> atelectasis(lack of gas exchange in the alveoli)--> uneven perfusion and hypoventilation --> --> pulmonary vasoconstriction and hypoperfusion --> endothelial and epithelial damage --> fibrin + necrotic cells (hyaline membrane formation) |
|
|
List 4 factors predipose an infant to HMD (hyaline membrane disease).
|
1. Prematurity - surfactant production about 35wks gestation
2. Male sex 3. Maternal DM - high insulin antagonizes corticosteroids, which induces surfactant formation 4. Cesarean birth |
|
|
Describe the anatomic lesions of HMD.
|
damage to alveolocapillary membrane --> fibrongen leakage and type II pneumocyte necrosis --> fibrin + cell debris visualized as hyaline membrane
|
|
|
What are clinical signs and symptoms of HMD?
|
dyspnea and cyanosis within 30 mins after birth
Progressive signs of respiratory difficulty: tachypnea, grunting, nasal flaring, intercostal and substernal retractions, and cyanosis |
|
|
How can HMD be prevented? (2)
How do you measure lung maturity? (2) |
1. delay delivery
2. maternal administration of corticosteroids --> production of surfactants Measure lung maturity via amniotic fluid analysis of: 1. Lecithin:sphingomyelin (L:S); L:S ratio ≥2 preferred 2. Phosphatidylglycerol (PG) level; PG presence indicates lung maturity. |
|
|
What is the classic treatment for HMD? modern treatment?
|
Classic treatment: supportive
1. O2 + high PRESSURE mechanical ventilation Modern treatment 1. O2 + high-FREQUENCY mechanical ventilation (HFV) 2. aerosolized exogenous surfactant. |
|
|
What are complications of HMD and its treatment?
Describe each. |
1. Bronchopulmonary dysplasia (BPD) - alveolar hypoplasia, alveolar wall fibrosis, and arrest of pulmonary septation
2. Retrolental fibroplasia (retinopathy of prematurity) - endothelial cell apoptosis and eventaully retinal detachment and blindness 3. pulmonary air-leak syndromes 4. patent ductus arteriosus (PDA) - hypoxia --> pulmonary arterial vasoconstriction --> R to L shunting through PDA. |
|
|
Discuss the pathogenesis of retrolental fibroplasia.
|
high O2 levels -->
decreased VEGF expression --> endothelial cell apoptosis return to room air --> increased VEGF expression --> neovascularization and fibrosis --> growth of new vessels and fibroblasts into vitreous --> fibrovascular tissue contraction --> retinal detachment --> blindness |
|
|
List 2 complications of prematurity other than HMD.
|
1. necrotizing enterocolitis (NEC)
2. Intracerebral hemorrhage |
|
|
What is the pathogenesis of necrotizing enterocolitis (NEC)?
Complications of NEC? |
hypoxia --> intestinal ischemia (prerequisite) + intro of bacteria from feeding + inflammatory mediators (esp. PAF) --> transmural intesttinal inflammation with gas formation by bacteria
complications 1. high perinatal mortality 2. survivors: fibrosis --> post-NEC strictures |
|
|
Where are 2 common places of hemorrhage in neonetal intracerebral hemorrage?
|
Germinal matrix hemorrange.
Periventricular hemorrhage extending to intraventricular spaces. |
|
|
What are 4 consequences of intracerebral hemorrhage?
|
1. increased intracranial pressure
2. damage to brain substance 3. herniation of brain into foramen magnum 4. fatal depression of vital medullary centers |
|
|
What is the most common cause of an intra-abdominal mass in an infant?
What other differential diagnoses can be made? |
unilateral utereopelvic junction obstruction resulting in an enlarged hydronephrotic kidney
Cysts in kidneys or pancreas Benign neoplasms - mature teratoma, lymphagioma Malignant neoplasms neuroblastoma Wilms tumor (nephroblastoma) hepatoblastoma immature teratoma lymphoma |
|
|
What are tumor markers are present in urine and blood in neuroblastoma patients?
|
blood - catecholamines
Urine - catecholamine metabolites (VMA and HVA) |
|
|
How is ganglion neuroblastoma different from neuroblastoma?
Which one is less aggressive? why? What is a "favorable" histological feature in ganglionneuroblastoma? |
Ganglion neuroblastoma is more differentiated.
Ganglion neuroblastoma is less aggressive and has the potential to differentiate and become benign. Presence of schwannian stroma indicates more favorable histology |
|
|
List favorable (5) and unfavorable (5) prognostic features of neuroblastoma.
|
favorable
1. low stage 2. age ≤ 18 months 3. favorable histology (more schwannian stroma) 4. N-MYC not amplified 5. hyperdiploid* Unfavorable 1. high stage 2. age > 18 months 3. unfavorable histology 4. N-MYC amplified 5. near-diploid |
|
|
What are 3 distinct histological features of Wilms tumor (nephroblastoma) that differentiate it from neuroblastoma?
|
1. blastema - embryonal cells
2. epithelium: abortive glomeruli and tubule 3. stroma - spindle cells |
|
|
What constitutes unfavorable histology in Wilms tumor?
|
Anaplasia
1. large, hyperchromatic, pleomorphic nuclei 2. mitoses |
|
|
Where do malignant neoplasms rank with regard to causes of death in children?
|
early childhood (1-4 yrs): 3rd
Later childhood (5-14 yrs): 2nd |
|
|
Where are 2 most frequent sites of primary malignancy in children?
|
Hematopoietic system and Nervous system
|
|
|
What is most common neoplasm of infancy?
Most common childhood malignancy? Most common cause of cancer death in childhood? 3 most common solid malignancies in childhood? |
Most common neoplasm of infancy: HEMANGIOMA (benign tumor of endothelial cells)
Most common childhood malignancy: LEUKEMIA Most common cause of cancer death in childhood: LEUKEMIA Three most common solid malignancies in childhood BRAIN TUMORS (collectively) NEUROBLASTOMA WILMS TUMOR (NEPHROBLASTOMA) |
|

This is CXR of an infant.
What do you see? Most common cause of this? |
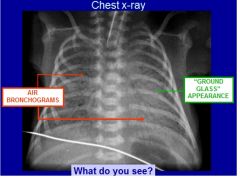
Common cause - Hyaline Membrane disease
|
|
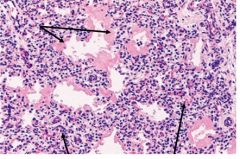
This is a slide of an infant lung.
ID the upper arrows and lower arrows. diagnosis? |
Upper arrows - hyaline membranee
Lower arrows: atelectatic alveoli Hyaline Membrane Disease |
|
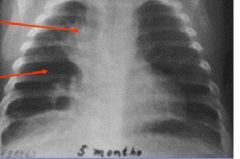
This is a CXR of an infant with HMD that developed complications from mechanical ventilation treatment.
ID the upper and lower arrows. |
Upper arrow - residual fibrosis
Lower arrow - hyperlucency (darker) indicates alveolar hypoplasia |
|

This CXR indicates pneumopericardium of an infant.
What syndrome is this? What is a possible cause of this? |
Pulmonary air-leak syndromes.
Caused by high pressure mechanical ventilation (treatment of HMD). |
|
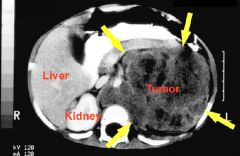
This is a CT scan in the region of the left kidney.
What do the darker areas indicate in the tumor? Its significance? |
indicates necrosis and hemorrhage.
Suggests rapidly growing and malignant. |
|
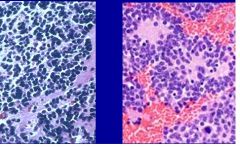
This is a microscopic section of an intra-abdominal mass(near the kidney region) in an infant.
What is the Dx? How do you know? |
Neuroblastoma
Must be malignancy of kidney or adrenal gland. aplastic and No triphasic histology --> neuroblastoma |
|
This is a section of neuroblastoma
Is there necrosis? If so, what kind? |
Yes
Coagulative necrosis. |
|
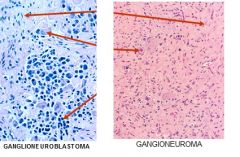
The left picture is a slide of ganglioneuroblastoma and the right picture is a slide of ganglioneuroma.
ID the arrows. |
Ganglioneuroblastoma
Top - Schwannian storma middle - ganglion cells bottom - residual neuroblasts Ganglioneuroma top - schwannian stroma bottom - ganglion cells |
|
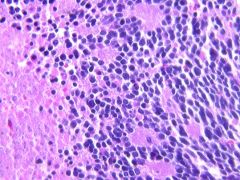
ID each picture as either neuroblastoma or Wilms tumor
|
Left - Neuroblastoma
Middle and Right - Wilms tumor (nephroblastoma) |
|
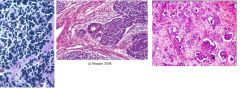
These are pictures of Wilms tumor.
Which one has favorable histology. How do you know? |
Left one.
The right one has cells with properties of anaplasia: Large, hyperchromatic, and plemorphic nuclei and mitoses. |
|
These are slides of Neuroblastoma, ganglioneuroblastoma, and ganglioneuroma.
ID each picture. Which one is most favorable? Least favorable? How do you know? |
Left - ganglioneuroblastoma
Middle - ganglioneuroma Right - neuroblastoma Ganglioneuroma (middle) is most favorable b/c there is no aplasia (benign) and lots of Schwannian stroma (more = favorable) Ganglioneuroblastoma is more favorable than neuroblastoma b/c there is some Schwannian stroma. |

