![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
59 Cards in this Set
- Front
- Back
|
|
|
Complete! |
|
|
|
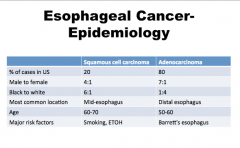
What are some risk factors for squamous cell carcinoma? |
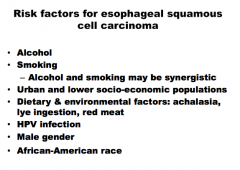
Most common = alcohol and smoking |
|
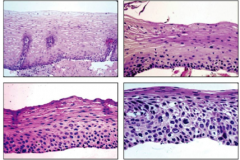
Identify moderate dysplaisa, mild, normal, and severe |
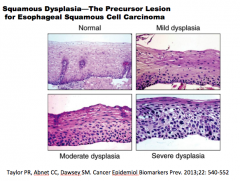
Similar to cervix but uses OLD terminology |
|
|
Amplification of the transcription factor gene SOX2 (believed to be involved in cancer stem cell self-renewal and survival) Esophageal squamous cell carcinoma:
Overexpression of the cell cycle regulator _______ |
Esophageal squamous cell caricnoma Amplification of the transcription factor gene SOX2 (believed to be involved in cancer stem cell self-renewal and survival) |
|
|
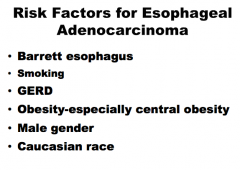
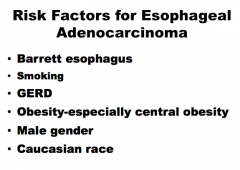
What are the risk factors for esophageal adenocarcinoma? |
|
|
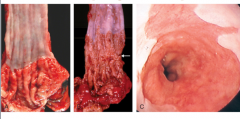
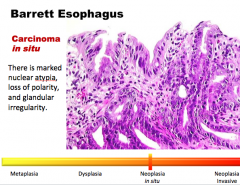
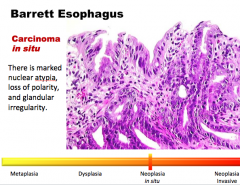
What is the condition? Is this metaplasia? Dysplasia? Neoplasia? Etc? |
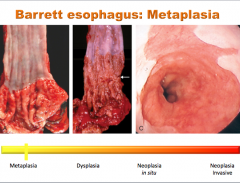
Can see pink glandular mucosa extending up into mucosa |
|
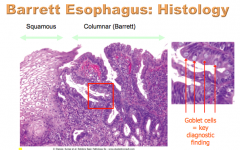
What is the key diagnostic finding of Barrett esophagus?
What is the TYPE of metaplasia? |
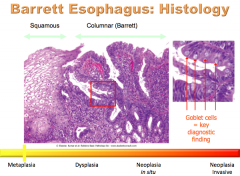
Goblet cells => intestinal metaplasia! |
|
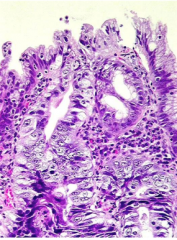
What is the condition? Describe the polarization of glandular cells, nuclei, and maturation. What is this (metaplasia, etc)? |
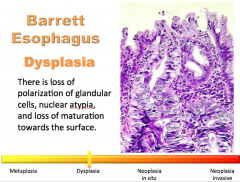
|
|
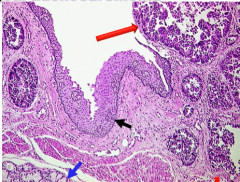
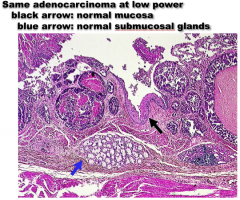
What is the condition? Identify the arrows. |
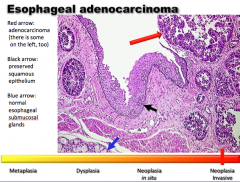
|
|
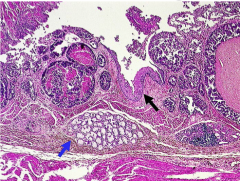
Identify the arrows: Normal mucosa, normal submucosal glands. What is the condition? |
|
|
|
Why is adenocarcinoma only seen at distal esophagus? |
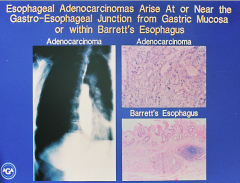
Barrett's or from gastric cancers growing up. |
|
|
What are the symptoms of esophageal carcinoma? |
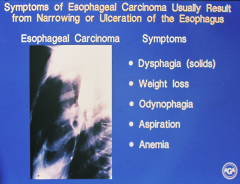
Odynophagia is pain with swallowing = probably not surgically resectable because has extended outside esophagus |
|
|
How do you diagnose esophageal cancer? What do you start with? |
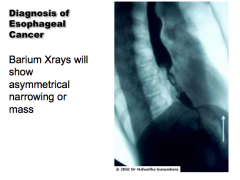
|
|
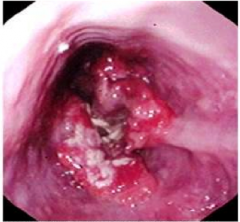
What is this? |
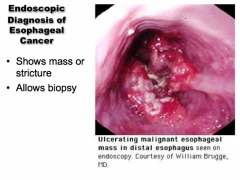
|
|
|
How do you stage esophageal cancer? What do you start with? What helps determine penetration into wall? |
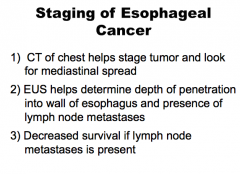
|
|
|
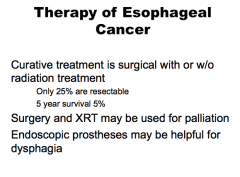
What is curative treatment of esophageal cancer? What is helpful for dysphagia? |
|
|
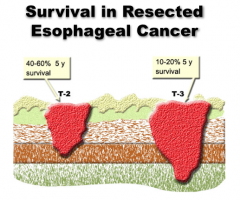
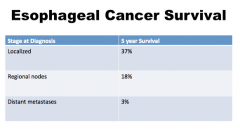
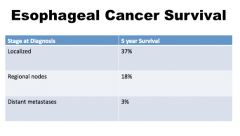
What is survival affected by? |
Wall depth |
|
|
|
|
|
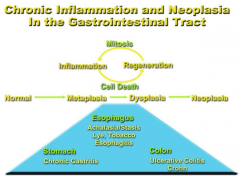
What predisposes to reflux which then predisposes to which three things?
What does alcohol and tobacco predispose to? |
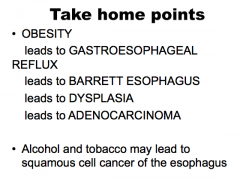
A and S are synergistic |
|
|
What are the two major types of gastric polyps? What are the subdivisions of each major type?
What are nodules protruding above the levels of the surrounding mucosa? Are they common in the stomach?
Most polyps in the stomach are what type? (75%) What cells are absent in this type? |
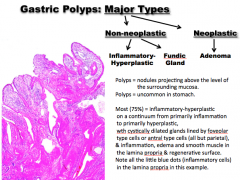
NOT PARIETAL CELLS! |
|
|
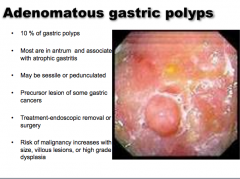
What accounts for 10% of gastric polyps?
Where are most located?
What types (shapes)?
Precursor lesion of what?
What is the treatment?
Risk of malignancy increases with what? |
|
|
|
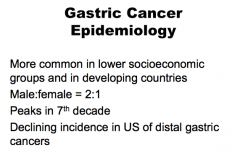
What groups is gastric cancer more common in? More common in which sex? Peaks in which decade? Is its incidence declining? |
|
|
|
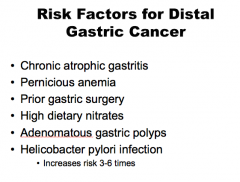
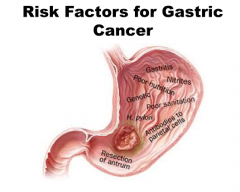
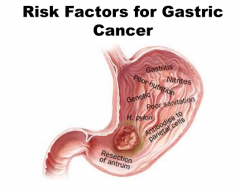
What are some risk factors for distal gastric cancer?
|
|
|
|
|
|
|
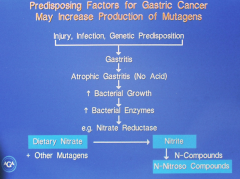
What is the mechanism of the predisposing factors that lead to gastric cancer? |
|
|
|
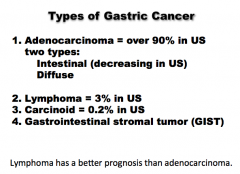
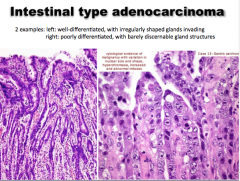
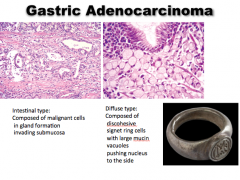
What are the four types of gastric cancer? Which is most common? What are the two types of the most common? |
|
|
|
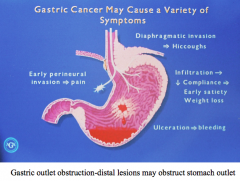
What are the symptoms of gastric cancer? |
|
|
|
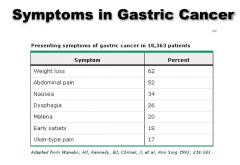
What are the three most common symptoms in gastric cancer? |
|
|
|
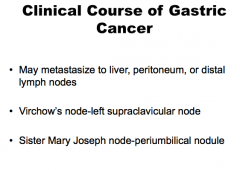
Where does gastric cancer metastasize?
Which node if often affected?
What is Sister Mary Joseph node? |
|
|

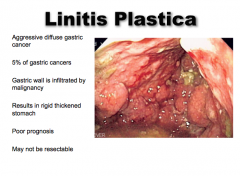
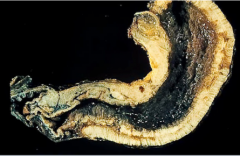
What is this aggressive diffuse cancer? What percent of gastric cancers? What does it result in (wall)? Is the prognosis good or bad?
Is it resectable? |
|
|
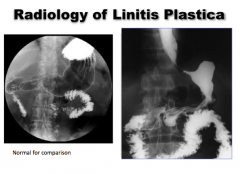
Notice wall thickness change |
|
|
|
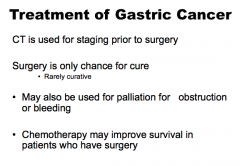
What is used for staging of gastric cancer prior to surgery? What is the only chance of cure and is rarely curative? |
|
|
|
Which infectious agent can cause chronic gastritis which can also cause gastric adenocarcinoma?
What is a diffuse type gastric cancer with no discrete mass and is difficult to diagnose? |
|
|
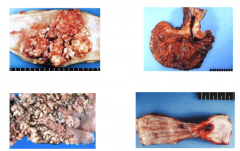
What is this? |
Esophageal squamous cell carcinoma |
|
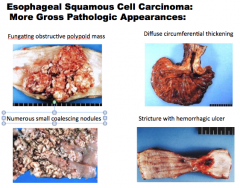
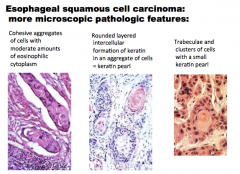
Identify the four different presentations of esophageal squamous cell carcinoma:
Numerous small coalescing nodules, diffuse circumferential thickening, stricture with hemorrhagic ulcer, fungating obstructive polypoid mass |
|
|
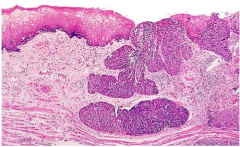
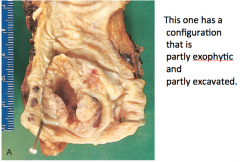
What is this squamous cell carcinoma doing? |
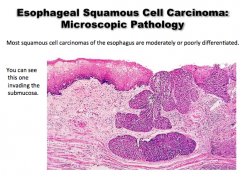
Invading the submucosa |
|
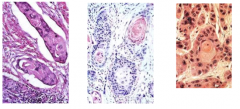
What is the type of cancer? |
|
|
|
What are some risk factors for esophageal adenocarcinoma?
Previous conditions, bad habits, sex, lifestyle, race |
|
|
|
Esophageal adenocarcinoma:
Molecular Pathogenesis: Early: mutation of ____ and downregulation of cyclin-dependent kinase inhibitor ____ (also known as ____, by both allelic loss and hypermethylation-induced epigenetic silencing). Later: amplification of EGFR, ____, MET, cyclin __ , and cyclin __ genes. |
Molecular Pathogenesis: Early: mutation of TP53 and downregulation of cyclin-dependent kinase inhibitor CDKN2A (also known as p16/INK4a, by both allelic loss and hypermethylation-induced epigenetic silencing). Later: amplification of EGFR, ERBB2, MET, cyclin D1 , and cyclin E genes. |
|
|
|
|
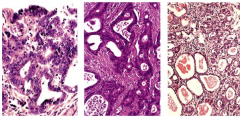
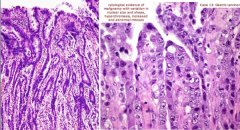
Esophageal adeocarcinoma
Which one shows nuclear atypia the best? |
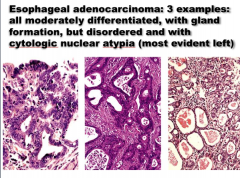
Left |
|

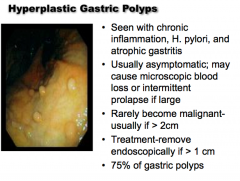
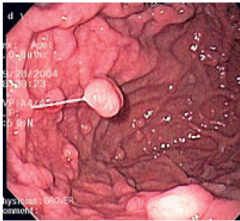
What is the condition? Seen with what conditions? Is it usually asymptomatic? Does it often become malignant? What is the treatment? What percent of gastric polyps? |
|
|
|
What is this an image of? What is inflamed? Describe the mucosal epithelium. |
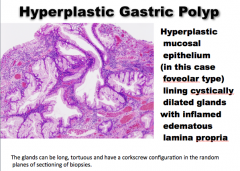
|
|
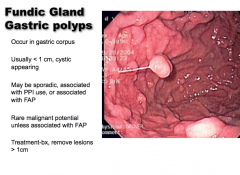
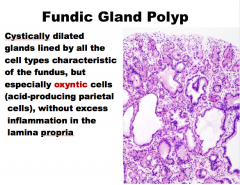
Fundic gastric polyp:
Where do they occur? Size usually? Are they sporadic? What are they often associate with?
Do they have malignant potential?
What is the treatment? |
|
|
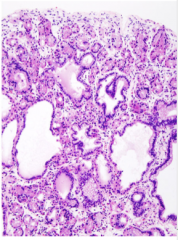
What is this?
Cystically dilated
|
|
|
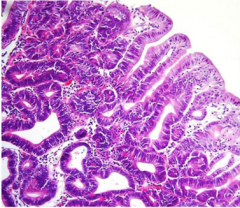
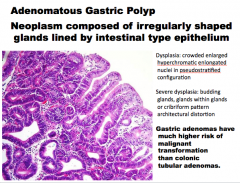
What type of polyp? Neoplasm composed of what shape of glands?
What will you see in dysplasia? Severe dysplasia?
What is the risk of malignant transformation? |
|
|

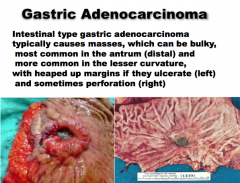
Intestinal type ______ adenocarcinoma |
|
|
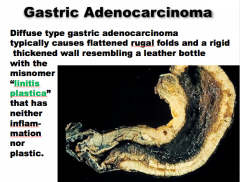
What type of adenocarcinoma?
What is the misnomer?
Does it have inflammation? |
|
|
|
Intestinal type gastric adenocarcinoma: Pathogenesis
“Sporadic intestinal-type gastric cancers are strongly associated with mutations that result in increased signaling via the _____. These include loss-of-function mutations in the adenomatous polyposis coli (_____) ______ gene and gain-of-function mutations in the gene encoding _____. Familial adenomatosis polyposis (FAP) patients, who carry germline APC mutations, have an increased risk of intestinal-type gastric cancer.”
|
“Sporadic intestinal-type gastric cancers are strongly associated with mutations that result in increased signaling via the Wnt pathway. These include loss-of-function mutations in the adenomatous polyposis coli (APC) tumor suppressor gene and gain-of-function mutations in the gene encoding β-catenin. Familial adenomatosis polyposis (FAP) patients, who carry germline APC mutations, have an increased risk of intestinal-type gastric cancer.” |
|
|
“Familial gastric cancer is strongly associated with germline loss-of-function mutations in the _____ , which encodes the _____. Thus, the loss of E-cadherin is a key step in the development of diffuse gastric cancer. CDH1 mutations are also common in sporadic and familial lobular carcinoma of the breast, which, like diffuse gastric cancer, tends to infiltrate as single cells, and individuals with _____ mutations are at increased risk of developing diffuse gastric cancer. Mutation of _____ is also found in the majority of sporadic gastric cancers of both diffuse and intestinal types. |
“Familial gastric cancer is strongly associated with germline loss-of-function mutations in the tumor suppressor gene CDH1 , which encodes the cell adhesion protein E-cadherin. Thus, the loss of E-cadherin is a key step in the development of diffuse gastric cancer. CDH1 mutations are also common in sporadic and familial lobular carcinoma of the breast, which, like diffuse gastric cancer, tends to infiltrate as single cells, and individuals with BRCA2 mutations are at increased risk of developing diffuse gastric cancer. Mutation of TP53 is also found in the majority of sporadic gastric cancers of both diffuse and intestinal types. |
|
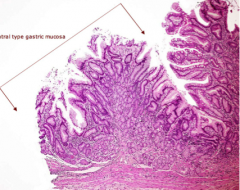
What is the precursor to intestinal type adenocarcinoma of the stomach and its most easily recognized by the goblet cells in it? |
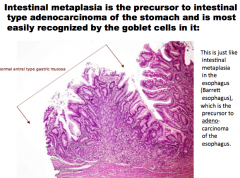
|
|
What is this? |
|
|
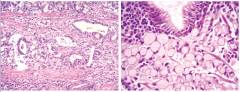
Gastric adenocarcinoma:
Where are the malignant cells invading? What is the signature histologic pattern? |
|
|
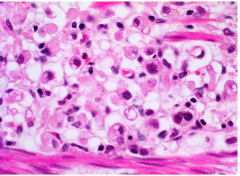
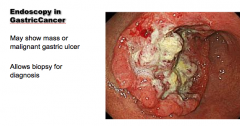
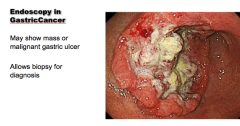
What is the condition? |
Diffuse type gastric adenocarcinoma |
|
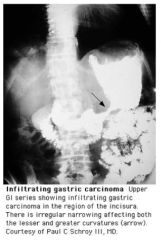
Radiology of gastric cancer. |
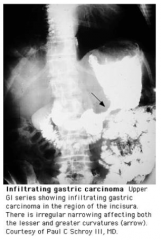
|
|
|
|
|

Metastatic gastric cancer. What's on the left and right? |
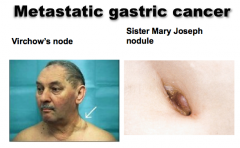
|
|
|
|

