![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
16 Cards in this Set
- Front
- Back
|
Discuss the purpose of physical assessment
|
- Includes health history and physical exam -Tocollect data/information about the client’s health, including physiological,psychological, sociocultural and spiritual aspects - Toidentify actual and potential problems - Toestablish the nurse-client relationship |
|
|
List the components of a health history |
1. Biographical/IdentifyingData 2. Source of the History; Reliability 3. Chiefcomplaint/reason for seeking health care in patient’s own words 4. History of Present Illness (HPI) chronology & symptom analysis) 5. Pasthistory (immunizations, allergies, medications, chronic illnesses, hospitalizations, childhood illnesses) 6. Familyhistory/genogram 7. Personaland social history (occupation, travel, habits, relationships, violence, pregnancy) 8. Reviewof symptoms |
|
|
Developing the HPI: OLDCART |
- Onset (when did it start?) - Location (point to the pain) - Duration (Pain all the time? Does the pain come and go?) - Characteristics (Quality and Severity) (Is it burning, cramping, stabbing pain?) - Aggravating/Alleviating (What makes it better? What makes it worse? -Radiating (does the pain radiate?) - Treatment/Timing (Have you tried anything?) |
|
|
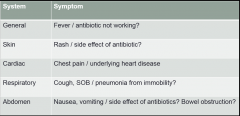
Review of Symptoms |
- Purpose is to evaluate past and present health state ofeach body system. - Includes only subjective data. - Does not include physical exam findings. |
|
|
|
|
|
Differentiate among the four types of health history |
|
|
|
What does SOAP stand for? |
Nursing Process Acronym S- Subjective Info O- Objective info A- Assessment P- Plan including outcomes |
|
|
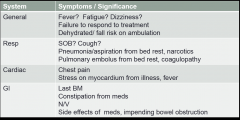
Subjective Info
|
- patient interview, symptom analysis, chronology
- comes from multiple sources such as patient, family, other providers, medical record |
|
|
Objective info
|
- Physical exam - Yourmeasurements, observations: Vitalsigns, Generalsurvey, HEENT , Skin, Respiratory, Cardiac, Abdomen, Neurologic, Musculoskeletal |
|
|
Assessment |
- Your analysis if the data you collected and the priorities you identified - Name the problem - Give nursing diagnosis which is your synthesis of S and O |
|
|
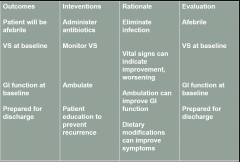
Plan |
- Measurable outcomes - Interventions and Rationales - Evaluation |
|
|
Plan |
|
|
|
What is the general survey? |
- An overall review or first impression that the health careprovider has of a person’s well being. - Beginswith first contact with the patient and continues throughout interview andphysical examination. |
|
|
Components of General Survey |
- Apparentstate of health - LOC or level of consciousness (awake, alert, responsive?) - Facialexpression - Distress - Ht,Wt, Build - Skincolor, obvious lesions - Dress,grooming, personal hygiene - Odors (body, breath) - Posture,gait, motor activity - Affect |
|
|
(4) Complete physical assessment |
–Currentand past health –Healthpromotion, screenings –Functionalability, ADLs, –Complete(head to toe) physical exam -primary care setting for check up or initial assessment at hospital |
|
|
(3) Focused/ Problem Centered |
–Smaller scope, one problem –Symptom analysis –Focused physical exam which means 1-2 systems examined |

