![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
100 Cards in this Set
- Front
- Back
|
What are common types of headaches in the out-patient setting? |
1. Tension headache 2. Migraine 3. Medication overuse |
|
|
What are serious causes of headaches? |
1. Meningitis 2. Brain tumor 3. Intracranial hemorrhage |
|
|
How can you classify headaches? |
Primary vs. secondary |
|
|
What are causes of primary headaches? |
- Migraine - Tension headaches - Cluster headaches |
|
|
What are the characteristics of migraine headaches? |
- Moderate to severe pain - Often occurs with nausea/vomiting, photophobia, or phonophobia; may occur with aura - Quality: pulsating, can be unilateral - Worsened with physical activity - Lasts 4-72 hours - 5 episodes needed for diagnosis |
|
|
What are the characteristics of tension headaches? |
- Mild to moderate pain - May occur with photophobia or phonophobia - Quality: pressing, tightening, and bilateral - Typically not worsened with physical activity - Lasts 30 minutes to 7 days - 10 episodes needed for diagnosis |
|
|
What are the characteristics of cluster headaches? |
- Severe pain - Associated with rhinorrhea, lacrimation, facial sweating, miosis (constriction of pupil), eyelid edema, conjunctival edema, and ptosis (eyelid drooping) - Quality: severe unilateral orbital, periorbital, supraorbital, or temporal pain - Lasts 15-180 minutes - 5 episodes needed for diagnosis |
|
|
How do migraines, tension headaches, and cluster headaches compare based on severity of pain? |
- Migraine: moderate to severe - Tension: mild to moderate - Cluster: severe |
|
|
How do migraines, tension headaches, and cluster headaches compare based on associated symptoms? |
- Migraine: often occurs with n/v, photophobia, phonophobia; may occur with aura - Tension: may occur with photophobia or phonophobia - Cluster: rhinorrhea, lacrimation, facial sweating, miosis, eyelid edema, conjunctival injection, ptosis |
|
|
How do migraines, tension headaches, and cluster headaches compare based on quality of pain? |
- Migraine: pulsating, can be unilateral - Tension: pressing, tightening, and bilateral - Cluster: severe unilateral orbital, periorbital, supraorbital, or temporal pain |
|
|
How do migraines, tension headaches, and cluster headaches compare based on aggravating factors? |
- Migraine: worsened with physical activity - Tension: typically not worsened with physical activity - Cluster: - |
|
|
How do migraines, tension headaches, and cluster headaches compare based on duration of symptoms? |
- Migraine: 4-72 hours - Tension: 30 minutes - 7 days - Cluster: 15-180 minutes |
|
|
How do migraines, tension headaches, and cluster headaches compare based on number of episodes required for diagnosis? |
- Migraine: 5 episodes - Tension: 10 episodes - Cluster: 5 episodes |
|
|
What are the causes of secondary headaches? |
Caused by another medical condition: - Meningitis - Intracranial hemorrhage - Brain tumor - Anxiety / depression - Medication overuse |
|
|
What findings in the H&P would make you suspicious for meningitis? |
- Headache with fever - Mental status change - Stiff neck |
|
|
What findings in the H&P would make you suspicious for intracranial hemorrhage? |
- Sudden onset of headache - Severe headache - Recent trauma - Elevated BP |
|
|
What findings in the H&P would make you suspicious for a brain tumor? |
- Cognitive impairment - Weight loss or other systemic symptoms - Abnormal neurologic exam |
|
|
What are the features of headaches due to depression or anxiety? |
Similar to tension type headache: - Bilateral, pressing, and/or tight - Lasts from 30 minutes to 7 days
Some experts feel depression or anxiety can trigger tension type headaches. In those cases, tension-type headaches are considered secondary, not primary headaches. |
|
|
What causes medication overuse headaches? |
AKA analgesic rebound headache; chronic use of any analgesic can cause this type of headache |
|
|
What are the features of medication overuse headaches? |
- Mild to moderate in severity - Diffuse, bilateral headaches that occur almost daily and are often present on first waking up in the morning - Often aggravated by mild physical or mental exertion - Can be associated with restlessness, nausea, forgetfulness, and depression - Headaches may improve slightly with analgesics but worsen when medication wears off; tolerance develops to abortive medications and there is decreased responsiveness to preventive medications |
|
|
How severe are medication overuse headaches? |
Mild to moderate |
|
|
Where are medication overuse headaches localized to? |
Diffuse, bilateral |
|
|
When / how often do medication overuse headaches occur? |
Almost daily; often present on first waking up in the morning |
|
|
What are medication overuse headaches associated with? |
- Restlessness - Nausea - Forgetfulness - Depression - Aggravated by mild physical or mental exertion |
|
|
What are the diagnostic criteria for medication overuse headaches? |
- >15 headaches / month - Regular overuse of an analgesic for more than 3 months - Development or worsening of a headache during medication overuse |
|
|
How do you treat medication overuse headaches? |
Stop the overused medication |
|
|
What are the guidelines for obtaining neuroimaging in the setting of a headache? |
- Patient has migrate with atypical headache patterns or neurologic signs - Patient is at higher risk of a significant abnormality - Results of the study would alter the management of the headache |
|
|
What are the symptoms that increase the odds of positive neuroimaging results? |
- Rapidly increasing frequency of headaches - Abrupt onset of severe headache - Marked change in headache pattern - History of poor coordination, focal neurologic signs/symptoms, and a headache that awakens the patient from sleep - Worsened with use of Valsalva's maneuver - New onset of headache in a person >35 years - History of cancer or HIV |
|
|
What is the quick method for screening for anxiety? |
GAD-2 - Over the last 2 weeks how often have you been bothered by the following problem: 1) Feeling, nervous, anxious, or on edge? 2) Not being able to stop or control worrying?
0 - not at all; 1 - several days; 2 - nearly half the days; 3 - nearly every day
Positive screening test is >3 points |
|
|
What is the quick method for screening for depression? |
PHQ-2 - Over the past 2 weeks how often have you been bothered by the following problem: 1) Little interest or pleasure in doing things 2) Feeling down, depressed, or hopeless
0 - not at all; 1 - several days; 2 - more than half the days; 3 - nearly every day
Negative response to both questions is a negative result for depression |
|
|
If a patient has a positive response to either question in the PHQ-2 (depression) or the GAD-2 (anxiety), what should be done? |
Screen with a more comprehensive tool, such as the PHQ-9 or the GAD-7
These are more specific in identifying depression or anxiety |
|
|
What physical exam findings should you look for in a patient with a headache? |
Signs of increased intracranial pressure: - Papilledema - Altered mental status
Other important findings: - Signs of meningeal irritation - Kerning's sign or Brudzinski's sign - Focal neurologic deficits - unilateral loss of sensation, unilateral weakness, unilateral hyperreflexia |
|
|
What is Kernig's sign? |
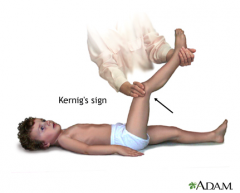
One of the physically demonstrable symptoms of meningitis; severe stiffness of the hamstrings causes an inability to straighten the leg when the hip is flexed to 90 degrees |
|
|
What is Brudzinski's sign? |
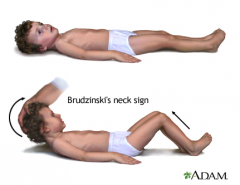
One of the physically demonstrable symptoms of meningitis; severe neck stiffness causes a patient's hips and knees to flex when the neck is flexed |
|
|
How do you evaluate CN II and III? |
Test whether pupils are equal, round, and reactive to light |
|
|
How do you evaluate CN II? |
Test visual fields with confrontation |
|
|
How do you evaluate CN III, IV, and VI? |
Test extra-ocular eye movements Test convergence |
|
|
How do you evaluate CN V? |
Ask pt to close their eyes and ask if the two stimuli feel the same when you lightly touch her right, then left forehead; right, then left cheek; right, then left chin |
|
|
How do you evaluate CN VII? |
Observe for facial symmetry 1. Raise eyebrows 2. Frown 3. Close both eyes tightly while you try to open them 4. Show both upper and lower teeth 5. Smile 6. Puff out both cheeks |
|
|
How do you evaluate CN VIII? |
Rub your fingers near each ear |
|
|
How do you evaluate CN XI? |
Have pt elevate her shoulders against resistance |
|
|
How do you evaluate CN IX, X, and XII? |
Assess whether speech is clear Assess whether tongue and palate are midline |
|
|
Besides CN, what other exam maneuvers should be done to complete the neurologic exam? |
- Light touch - Motor - Reflexes - Cerebellar exam - Gait exam - walk on heels, walk on toes, walk heel to toe |
|
|
What are the components of the cerebellar exam? |
- Finger-to-nose test - Heel-to-shin test |
|
|
Case: 24-year old woman with family history of migraines presents complaining of two chronic progressively worsening headaches. The first type is severe, throbbing, and unilateral; associated with nausea, photophobia, and phonophobia; lasts all day, occurs 1-2x/week, and does not improve with ibuprofen.
Second type are mild-to-moderate and bilateral, lasts all days most days, and have associated neck discomfort.
On exam, afebrile with normal vital signs, mildly tender occiput, no focal neurologic defects, signs of increased ICP, or meningeal irritation.
What are the most likely causes of her headaches? |
- Migraines - Tension type headache |
|
|
Case: 24-year old woman with family history of migraines presents complaining of two chronic progressively worsening headaches. The first type is severe, throbbing, and unilateral; associated with nausea, photophobia, and phonophobia; lasts all day, occurs 1-2x/week, and does not improve with ibuprofen.
Second type are mild-to-moderate and bilateral, lasts all days most days, and have associated neck discomfort.
On exam, afebrile with normal vital signs, mildly tender occiput, no focal neurologic defects, signs of increased ICP, or meningeal irritation.
What features are suggestive of migraine headaches? |
- Severe headaches 1-2x/week - Unilateral and throbbing - Associated nausea, photophobia, phonophobia - Family history of migraines - Increased caffeine consumption and poor sleep are possible triggers - Normal neuro exam |
|
|
Case: 24-year old woman with family history of migraines presents complaining of two chronic progressively worsening headaches. The first type is severe, throbbing, and unilateral; associated with nausea, photophobia, and phonophobia; lasts all day, occurs 1-2x/week, and does not improve with ibuprofen.
Second type are mild-to-moderate and bilateral, lasts all days most days, and have associated neck discomfort.
On exam, afebrile with normal vital signs, mildly tender occiput, no focal neurologic defects, signs of increased ICP, or meningeal irritation.
What features are suggestive of tension type headaches? |
- Mild to moderate bilateral headaches that last all day on most days - Pain radiates down neck with tender occiput - Increased stressors and poor sleep in recent weeks are possible trigger - Normal neuro exam |
|
|
Case: 24-year old woman with family history of migraines presents complaining of two chronic progressively worsening headaches. The first type is severe, throbbing, and unilateral; associated with nausea, photophobia, and phonophobia; lasts all day, occurs 1-2x/week, and does not improve with ibuprofen.
Second type are mild-to-moderate and bilateral, lasts all days most days, and have associated neck discomfort.
On exam, afebrile with normal vital signs, mildly tender occiput, no focal neurologic defects, signs of increased ICP, or meningeal irritation.
Why is it unlikely she is having cluster headaches? |
Her pain is not associated with autonomic features |
|
|
Case: 24-year old woman with family history of migraines presents complaining of two chronic progressively worsening headaches. The first type is severe, throbbing, and unilateral; associated with nausea, photophobia, and phonophobia; lasts all day, occurs 1-2x/week, and does not improve with ibuprofen.
Second type are mild-to-moderate and bilateral, lasts all days most days, and have associated neck discomfort.
On exam, afebrile with normal vital signs, mildly tender occiput, no focal neurologic defects, signs of increased ICP, or meningeal irritation.
Why is it unlikely she has bacterial meningitis? |
Unlikely due to chronic nature of her headache and absence of fever, lack of changes in mental status, or history of recent illness. She had no findings concerning for meningitis on physical exam. |
|
|
Case: 24-year old woman with family history of migraines presents complaining of two chronic progressively worsening headaches. The first type is severe, throbbing, and unilateral; associated with nausea, photophobia, and phonophobia; lasts all day, occurs 1-2x/week, and does not improve with ibuprofen.
Second type are mild-to-moderate and bilateral, lasts all days most days, and have associated neck discomfort.
On exam, afebrile with normal vital signs, mildly tender occiput, no focal neurologic defects, signs of increased ICP, or meningeal irritation.
Why is it unlikely she has an intracranial hemorrhage? |
No history of recent trauma or a change in the pattern of her headaches. Her near exam was normal as well. Patients with ICH often describe the "worst headache of my life". |
|
|
Case: 24-year old woman with family history of migraines presents complaining of two chronic progressively worsening headaches. The first type is severe, throbbing, and unilateral; associated with nausea, photophobia, and phonophobia; lasts all day, occurs 1-2x/week, and does not improve with ibuprofen.
Second type are mild-to-moderate and bilateral, lasts all days most days, and have associated neck discomfort.
On exam, afebrile with normal vital signs, mildly tender occiput, no focal neurologic defects, signs of increased ICP, or meningeal irritation.
Why is it unlikely she has a brain tumor? |
- Age <50 - Lack of systemic symptoms - Absence of focal neurologic deficit - No change in headache pattern - Consider this in a first headache in a patient >50 years |
|
|
Case: 24-year old woman with family history of migraines presents complaining of two chronic progressively worsening headaches. The first type is severe, throbbing, and unilateral; associated with nausea, photophobia, and phonophobia; lasts all day, occurs 1-2x/week, and does not improve with ibuprofen.
Second type are mild-to-moderate and bilateral, lasts all days most days, and have associated neck discomfort.
On exam, afebrile with normal vital signs, mildly tender occiput, no focal neurologic defects, signs of increased ICP, or meningeal irritation.
Why is it unlikely she is having medication overuse headaches? |
- Not using analgesics frequently enough - For simple analgesics such as ibuprofen, patient must report using the med at least 15x/month for 3 months |
|
|
Case: 24-year old woman with family history of migraines presents complaining of two chronic progressively worsening headaches. The first type is severe, throbbing, and unilateral; associated with nausea, photophobia, and phonophobia; lasts all day, occurs 1-2x/week, and does not improve with ibuprofen.
Second type are mild-to-moderate and bilateral, lasts all days most days, and have associated neck discomfort.
On exam, afebrile with normal vital signs, mildly tender occiput, no focal neurologic defects, signs of increased ICP, or meningeal irritation.
Why is it unlikely she is having headaches due to anxiety or depression? |
She screened negative for anxiety and depression |
|
|
What directions should you give patients to help manage triggers of migraine and tension type headaches? |
1. Headache diary 2. Decrease caffeine intake slowly 3. Get more sleep |
|
|
What should patients note in a headache diary? |
- Make note each day of whether or not you have a headache - Keep track of the severity of the headaches and which treatments are effective - Identify and avoid headache triggers; use a list of things that trigger headaches, and monitor which of these triggers worsen your headaches |
|
|
What should a patient with migraines or tension type headaches do regarding their caffeine use? |
Slowly decrease use of sodas; caffeine worsens both migraines and tension type headaches, but coming off caffeine too quickly may make things worse in the short term |
|
|
What should a patient with migraines or tension type headaches do regarding their sleep? |
Try to get more sleep. Aim for 8 hours each night and establish a regular sleep routine, meaning try to go to sleep at the same time each night |
|
|
What are the types of triggers that may increase the frequency of migraines or tension headaches? |
- Physical or environmental triggers - Medications or substances - Possible dietary triggers |
|
|
What are some physical or environmental triggers that may increase the frequency of migraines or tension headaches? |
- Intense or strenuous exercise - Sleep disturbance - Menses - Ovulation - Pregnancy (though for many they improve) - Acute illness - Fasting - Bright or flickering lights - Emotional stress |
|
|
What are some medications or substances that could act as triggers that may increase the frequency of migraines or tension headaches? |
- Estrogen (birth control / hormone replacement) - Tobacco, caffeine, alcohol - Aspartame and phenylalanine (from diet colas) |
|
|
What are some possible dietary triggers that may increase the frequency of migraines or tension headaches? |
- Ripened cheeses - Alcohol, especially beer and red wine - Pickled or fermented foods - Monosodium glutamate (MSG) - Yeast-based products - Chocolate - Legumes and beans - Onions - Citrus fruits - Bananas |
|
|
What are some examples of effective stress relievers that may help relieve frequency/severity of headaches? |
- Meditation - Prayer, or even a scheduled amount of stillness - Listening to relaxation audio programs - Setting limits on other people's expectations - Getting moderate regular exercise - Getting at least 8 hours of sleep each night |
|
|
What are the types of medications that are useful for treating migraines? |
Migraine-specific meds: - Triptans - Ergot alkaloids
Non-specific treatments (effective for any pain disorder): - Aspirin/Butalbital/Caffeine - Acetaminophen/Butalbital/Caffeine - Acetaminophen/Dichloralphenazone - Acetaminophen/Aspirin/Caffeine |
|
|
What are some examples of triptans? |
- Sumatriptan (Imitrex, Imigran) - Naratriptan (Amerge, Naramig) - Rizatriptan (Maxalt) - Zolmitriptan (Zomig) - Frovatriptan (Frova, Migard) - Almotriptan (Axert) - Eletriptan (Relpax) |
|
|
What are the contraindications to triptan therapy? |
- Ergotamine - MAOIs - History of hemiplegic or basilar migraine - Significant cardiovascular, cerebrovascular, or peripheral vascular disease - Severe HTN - Pregnancy - In combination with SSRIs (may cause serotonin syndrome) |
|
|
What are the potential side effects of triptans? |
- Dizziness - Sleepiness - Nausea - Fatigue - Paresthesia - Throat tightness / closure - Chest pressure |
|
|
What are some examples of ergot alkaloids? |
- Ergotamine (Ergostat) - Ergotamine/Caffeine (Cafergot) - Dihydroergotamine (DHE) |
|
|
What are the contraindications to ergot alkaloids? |
- Triptans - Many possibly serious drug interactions - Heart disease or angina - HTN - Peripheral vascular disease - Pregnancy - Renal insufficiency - Breastfeeding |
|
|
What are the possible side effects of ergot alkaloids? |
- Severe reactions possible - MI - Ventricular tachyarrhythmia - Stroke - HTN - Nausea/vomiting - Diarrhea - Dry mouth - Rash |
|
|
What are the contraindications of aspirin / butalbital / caffeine (Fiorinal)? |
- History of porphyria or peptic ulcers - Bleeding risk - Caution in drug abuse - Pregnancy |
|
|
What are the possible side effects of aspirin / butalbital / caffeine (Fiorinal)? |
- Anaphylaxis - Toxic epidermal necrolysis - Stevens-Johnson syndrome - Myelosuppression / thrombocytopenia - GI bleed |
|
|
What are the contraindications of acetaminophen / butalbital / caffeine (Esgic, Fioricet, Phrenilin - lacks caffeine)? |
- History of porphyria - Pregnancy - Caution in drug abuse |
|
|
What are the possible side effects of acetaminophen / butalbital / caffeine (Esgic, Fioricet, Phrenilin - lacks caffeine)? |
- Dizziness - Drowsiness - Dyspnea - Nausea / vomiting - Abdominal pain - Agranulocytosis - Thrombocytopenia - Respiratory depression - Stevens-Johnson Syndrome |
|
|
What are the contraindications of acetaminophen / dichloralphenazone (Midrin)? |
- Hepatorenal insufficiency - Diabetes - HTN - Glaucoma - Heart disease - MAOI use |
|
|
What are the possible side effects of acetaminophen / dichloralphenazone (Midrin)? |
- HTN - Dizziness - Rash |
|
|
What are the contraindications of acetaminophen / aspirin / caffeine (Excedrin)? |
- Pregnancy - Sensitivity to aspirin |
|
|
What are the possible side effects of acetaminophen / aspirin / caffeine (Excedrin)? |
- Nausea - GI bleed - HTN |
|
|
What medications should be used as last resorts for migraines? Why? |
Opioids of Butalbital containing meds - there are other more effective, migraine-specific treatments available
Frequent use of these meds can worsen headaches. Opioids should be reserved for those with medical conditions precluding the use of migraine-specific treatments or those who fail those treatments. |
|
|
What is the utility of EEG for evaluating headaches? |
No advantage over clinical evaluation; does not improve outcomes and increases cost. |
|
|
How should a patient with migraines utilize a triptan? |
Take at the first sign of headache and repeat in 2 hours if the first dose was not effective |
|
|
What are methods for migraine prophylaxis? |
- Beta blockers - Neurostabilizers - Tricyclic antidepressants - Calcium channel blockers |
|
|
What are the types of beta-blockers that can be used for migraine prophylaxis? |
- Propranolol - Timolol |
|
|
Are beta-blockers (propranolol, timolol) FDA approved for migraine prophylaxis? Efficacy / Cost? Contraindications? Side effects? |
- FDA approved - Good-excellent efficacy - Cost is cheap - Contraindications: asthma, depression, severe COPD, DM requiring insulin, Raynaud's disease - Side effects: fatigue, bronchospasm, lightheadedness, insomnia, bradycardia, depression, sexual dysfunction |
|
|
What are the types of neurostabilizers that can be used for migraine prophylaxis? |
- Divalproex sodium - Topiramate - Gabapentin |
|
|
Are neurostabilizers (divalproex, topiramate, gabapentin) FDA approved for migraine prophylaxis? Efficacy / Cost? Contraindications? Side effects? |
- FDA approved - Good efficacy - Expensive - Contraindications: pregnancy / risk of pregnancy, gabapentin is category C, divalproex - hepatic disease - Side effects: divalproex - birth defects, weight gain, alopecia, pancreatitis, ovarian cysts; topiramate - renal stones, weight loss; gabapentin - dizziness, somnolence |
|
|
What are the side effects / contraindications of divalproex? |
- Birth defects - Weight gain - Alopecia - Pancreatitis - Ovarian cysts - Contraindicated in pregnancy / risk of pregnancy, hepatic disease |
|
|
What are the side effects / contraindications of topiramate? |
- Renal stones - Weight loss - Contraindicated in pregnancy / risk of pregnancy |
|
|
What are the side effects / contraindications of gabapentin? |
- Dizziness - Somnolence - Contraindicated in pregnancy / risk of pregnancy - Category C |
|
|
What tricyclic antidepressant may be used for migraine prophylaxis? |
Amitriptyline |
|
|
Are tricyclic antidepressants (amitriptyline) FDA approved for migraine prophylaxis? Efficacy / Cost? Contraindications? Side effects? |
- Not FDA approved (off-label) - Excellent efficacy - Cheap - Also works for fibromyalgia and tension-type headaches - Contraindications: cardiac conduction defects, MAOI - Side effects: drowsiness, weight gain, dry mouth |
|
|
What calcium channel blocker may be used for migraine prophylaxis? |
Verapamil |
|
|
Are calcium channel blockers (verapamil) FDA approved for migraine prophylaxis? Efficacy / Cost? Contraindications? Side effects? |
- Not FDA approved (off-label use) - Fair efficacy - Moderately expensive - Contraindications: AV block, sick sinus syndrome - Side effects: edema, nausea, headache, fatigue |
|
|
What are some other treatments for migraine prophylaxis? |
- Feverfew - Magnesium - Coenzyme Q - Vitamin B2 - Butterbur extract |
|
|
What would be the best initial preventative therapy for Sarah's migraine headaches if prophylaxis were indicated? Why? |
Amitriptyline - also effective in reducing tension-type headaches, inexpensive |
|
|
What are the characteristics of drug dependence? |
Maladaptive pattern of drug use causing clinically significant impairment or distress
Manifested by at least 3 of the following: - Tolerance - Withdrawal - Increasing doses - Desire or inability to cut down - Significant amount of time spent in search of drug - Interference with social, occupational, or recreational activities - Continued use despite persistent / recurrent physical or psychological problems due to the drug |
|
|
What are the characteristics of drug addiction? |
Persistent drug craving, loss of control over drug use, compulsive use, and a strong tendency to relapse after withdrawal |
|
|
What are the characteristics of drug tolerance? |
Need for increasing doses of medication to achieve the initial effect of the drug |
|
|
How should opiates be used for the treatment of pain? |
Short-acting opiates (eg, hydrocodone and oxycodone) are indicated ONLY for use in ACUTE pain or for BREAKTHROUGH pain, when long acting agents are insufficient to control symptoms |
|
|
What should the approach to chronic pain treatment be? |
1. Set clear goals 2. Use non-pharmacologic treatments 3. First select specifically targeted non-opiate therapies 4. When using opiates use long-acting agents along with other agents and use the lowest possible dose; use a pain med agreement |
|
|
What are the criteria for controlled headache symptoms? |
- Fewer than 2 headaches per week or 8 per month - Relieved with lifestyle modification and acute treatment medicine - Controlled headaches do not require additional follow-up unless the headaches change or get worse |

