![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
304 Cards in this Set
- Front
- Back
|
What are common causes of persistent cough? |
- Upper airway cough syndrome (UACS - previously called post-nasal drip) - Vocal cord dysfunction - Asthma - GERD - Cough d/t meds (eg, ACE-inhibitors) - Tobacco-related cough - Post-infectious cough - COPD (especially chronic bronchitis) - Non-asthmatic eosinophilic bronchitis |
|
|
What are the serious, but less common, causes of persistent cough? |
- Pulmonary conditions such as bronchogenic carcinoma of the lung, including sarcoidosis and tuberculosis - Cardiac conditions such as CHF |
|
|
What are some causes of wheezing? |
- Asthma - COPD - CHF - Foreign body aspiration - Persistent bronchitis - Upper airway cough syndrome (aka, post-nasal drip) - Vocal cord dysfunction - Pulmonary embolism |
|
|
What is the most common cause of persistent cough and wheezing? |
Asthma |
|
|
What pulmonary auscultatory finding would you expect with pneumonia? |
Rales |
|
|
What pulmonary auscultatory finding would you expect with epiglottitis? |
Stridor |
|
|
What pulmonary auscultatory finding would you expect with obstructive sleep apnea? |
None, may present with daytime sleepiness, nocturnal snoring, and irregular breathing when asleep |
|
|
What conditions may require treatment to improve the control of asthma? |
- GERD - Obesity / overweight - OSA - Rhinitis or sinusitis - Stress / depression |
|
|
What are the symptoms of acute sinusitis? |
- Fever - Opaque / mucopurulent nasal discharge - Headaches - Facial pain - Toothache - Failure to respond to decongestants - Initial improvement after a viral URI and then a reoccurrence of worsening symptoms (minimum of 7-10 days following a viral URI) |
|
|
A patient presents complaining of one week of URI sx including nasal congestion and drainage. On the day the sx began he had a low-grade fever that has now resolved. His nasal congestion persisted and he has had yellow nasal drainage for five days with associated mild headaches.
On exam he is afebrile and in no distress. Exam of his TM and throat are normal. Exam of his nose is unremarkable although a slight amount of yellowish-clear drainage is noted. There is tenderness when you lightly percuss his maxillary sinuses.
How should you treat this patient? |
Observation and reassurance
This is more likely to be a viral rhino sinusitis because this patient has had symptoms <10 days and sx are not worsening, so you can continue to observe the patient and reassure him that antibiotics are not necessary at this time
Have patient return if he develops a fever or worsening symptoms |
|
|
When are antibiotics recommended for acute bacterial sinusitis? |
- Moderate to severe pain - Temp ≥ 101 F - Worsening symptoms - Failure to improve 7 days after diagnosis |
|
|
What antibiotics are indicated first-line for acute bacterial sinusitis? |
Amoxicillin TMP-SMX |
|
|
What are the characteristics of chronic sinusitis? |
Similar symptoms to patients with acute sinusitis, but they last >12 weeks! |
|
|
How do you diagnose chronic sinusitis? |
Must have 2 of the following symptoms: - Nasal obstruction / congestion - Mucopurulent drainage - Facial pain - Pressure or fullness - Decreased sense of smell
Must last for at least 12 weeks |
|
|
Why should you ask a patient who may have asthma whether they are allergic to aspirin? |
21% of adults who have asthma have aspirin-induced asthma and should avoid NSAIDs |
|
|
What are some potential asthma co-morbid conditions? |
- Overweight / obesity - GERD - OSA - Stress / depression |
|
|
What parts of the physical exam should you do for a patient with persistent cough? |
- Eyes - Ears - Nose - Sinuses - Throat - Neck - Chest / lungs - Cardiovascular - Abdomen - Extremities - Skin - Mental status |
|
|
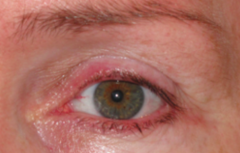
What are you looking for on the eye exam in a patient with a persistent cough? |
- May show signs of allergic conjunctivitis - Also can look for "allergic shiners" |
|
|
What are you looking for on the ear exam in a patient with a persistent cough? |
Should be performed in any patient with nasal symptoms for signs of infection, but may be normal |
|
|
What are you looking for on the nose exam in a patient with a persistent cough? |
Nasal turbinates and pallor of the nasal mucosa consistent with allergic rhinitis
Clear, watery nasal discharge may also be present in patients with allergic rhinitis |
|
|
What are you looking for on the sinus exam in a patient with a persistent cough? |
Percussing the frontal and maxillary sinuses may be useful in assessing sinus tenderness that may indicate the possibility of an acute or chronic sinus infection |
|
|
What are you looking for on the throat exam in a patient with a persistent cough? |
Throat exam may reveal postnasal drainage, which may be a clue that the patient has "upper airway cough syndrome" |
|
|
What are you looking for on the neck exam in a patient with a persistent cough? |
If an infection is suspected, examining the neck for lymphadenopathy may be useful |
|
|
What are you looking for on the chest/lung exam in a patient with a persistent cough? |
- Lung exam may be useful if wheezing is heard - However the absence of wheezing does not rule out asthma or other cardiac or pulmonary condition - The lung exam may also be useful if rales or other lung abnormalities are heard that are suggestive of CHF or pneumonia |
|
|
What are you looking for on the CV exam in a patient with a persistent cough? |
Cardiac exam is useful only if abnormalities such as extra heart sounds (S3 or S4) are heard suggesting CHF |
|
|
What are you looking for on the abdominal exam in a patient with a persistent cough? |
Exam of the abdomen is unlikely to be helpful in this patient |
|
|
What are you looking for on the extremities exam in a patient with a persistent cough? |
- Look for clubbing, cyanosis, or edema - Clubbing is not a finding in patients with asthma, but if present, may be a sign of other pulmonary conditions - Cyanosis is unlikely to be present in patients seen in the office setting, but if present, may indicate a hypoxic lung or cardiac condition - If edema is present, it may be a sign of CHF, one of the conditions in the differential diagnosis |
|
|
What are you looking for on the skin exam in a patient with a persistent cough? |
Skin exam may be useful in certain patients if eczema is present, since eczema and asthma may coincide |
|
|
What are you looking for on the mental status exam in a patient with a persistent cough? |
It is appropriate to note his affect and mood as you perform your exam |
|
|
Case: 40-year old non-smoker with a history of allergic rhinitis who presents with a productive cough worse at night for 2 months with associated wheezing but no chest pain, shortness of breath, or fever.
Exam is completely normal other than swelling of the inferior turbinates, pallor of the nasal mucosa with some clear drainage present.
What are the top five items on your differential? |
1. Asthma with uncontrolled allergic rhinitis and possible chronic sinusitis 2. COPD 3. Non-asthmatic eosinophilic bronchitis 4. Vocal cord dysfunction 5. GERD |
|
|
Case: 40-year old non-smoker with a history of allergic rhinitis who presents with a productive cough worse at night for 2 months with associated wheezing but no chest pain, shortness of breath, or fever.
Exam is completely normal other than swelling of the inferior turbinates, pallor of the nasal mucosa with some clear drainage present.
What tests can you order to narrow the differential? |
Spirometry, both with and without bronchodilation |
|
|
Case: 40-year old non-smoker with a history of allergic rhinitis who presents with a productive cough worse at night for 2 months with associated wheezing but no chest pain, shortness of breath, or fever.
Exam is completely normal other than swelling of the inferior turbinates, pallor of the nasal mucosa with some clear drainage present.
Why is a CXR not useful at this time? |
A CXR is useful in the evaluation of a patient with a persistent cough to rule in or rule out a suspected infection such as pneumonia. You may find hyper-inflated lungs on a patient with asthma, but this is non-specific (since COPD can also cause this). |
|
|
Case: 40-year old non-smoker with a history of allergic rhinitis who presents with a productive cough worse at night for 2 months with associated wheezing but no chest pain, shortness of breath, or fever.
Exam is completely normal other than swelling of the inferior turbinates, pallor of the nasal mucosa with some clear drainage present.
Why is a CT scan of chest not useful at this time? |
A CT scan of the chest would be helpful if there were an abnormality on the CXR, such as a lung mass or if there was a concern about a pulmonary embolus, but is unlikely to be helpful in a patient presenting with wheezing. |
|
|
Case: 40-year old non-smoker with a history of allergic rhinitis who presents with a productive cough worse at night for 2 months with associated wheezing but no chest pain, shortness of breath, or fever.
Exam is completely normal other than swelling of the inferior turbinates, pallor of the nasal mucosa with some clear drainage present.
Why is a methacholine challenge not useful at this time? |
A methacholine challenge test may be considered if the spirometry findings are normal. This test should be carried out by a "trained individual" and therefore the patient most likely will be referred out for this test. |
|
|
Case: 40-year old non-smoker with a history of allergic rhinitis who presents with a productive cough worse at night for 2 months with associated wheezing but no chest pain, shortness of breath, or fever.
Exam is completely normal other than swelling of the inferior turbinates, pallor of the nasal mucosa with some clear drainage present.
Why is a ventilation/perfusion scan not useful at this time? |
While there can be a ventilation/perfusion mismatch in patients with asthma, it is unlikely that a ventilation/perfusion scan is helpful in the initial management of asthma. A V/Q scan is more useful in diagnosing PE. |
|
|
What is the function of spirometry? |
Measures how much air the patient can inhale and exhale, as well as how fast the patient can exhale. It is repeated 3x to make sure it is reliable.
First a baseline sample is obtained. Then the pt is given a bronchodilator. |
|
|
Case: 40-year old non-smoker with a history of allergic rhinitis who presents with a productive cough worse at night for 2 months with associated wheezing but no chest pain, shortness of breath, or fever.
Exam is completely normal other than swelling of the inferior turbinates, pallor of the nasal mucosa with some clear drainage present.
What are the best medication to offer the patient at this point? |
For cough due to suspected asthma: - Inhaled albuterol (bronchodilator) - 1-2 puffs QID PRN + spacer
For long-standing allergic rhinitis: - Oral antihistamine (eg, cetirizine) - Inhaled nasal corticosteroid (eg, fluticasone) |
|
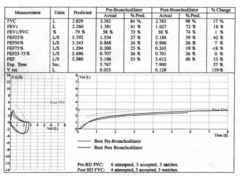
What are the findings on the spirometry test? |
Obstructive lung disease with reversible findings (improvement after a bronchodilator is given) |
|
|
How do you determine if there was "reversibility" of the obstruction? |
Asthma: - Improvement in the FEV1 by >12% OR - Increase in the percent predicted FEV1 by 10% after a bronchodilator is given |
|
|
What are the spirometry findings in restrictive lung disease? |
Decreased FEV1 and decreased FVC values, so that the FEV1/FVC ratio may be normal or increased |
|
|
What findings would make you choose the diagnosis of asthma? |
- Reversible obstructive findings on spirometry - Improvement following treatment with inhaled corticosteroids - Patients with chronic, severe asthma may have less or no reversibility of their obstructive findings, similar to COPD |
|
|
What findings would make you choose the diagnosis of non-asthmatic eosinophilic bronchitis? |
- Respond to inhaled corticosteroids like patients with asthma - Normal spirometry and normal CXR - Diagnostic finding is sputum eosinophilia on induced sputum or bronchial wash obtained with bronchoscopy |
|
|
What findings would make you choose the diagnosis of vocal cord dysfunction? |
- Flattening of the inspiratory loop on spirometry, but do not typically have reversible obstructive findings like patients with asthma - Diagnostic finding is visualizing abnormal vocal cord moment during an episode of wheezing |
|
|
What findings would make you choose the diagnosis of COPD? |
- Improves following treatment with bronchodilators and inhaled corticosteroids - Obstructive findings are seen on spirometry but are not reversible |
|
|
What findings would make you choose the diagnosis of GERD? |
- Usually present with heartburn symptoms or findings of esophagitis on upper endoscopy - Even if asymptomatic, reflux can trigger bronchoconstriction and serve as an exacerbating factor for patients with asthma - If a patient with asthma fails to improve with standard therapy, it is reasonable to consider GERD |
|
|
How do you establish a diagnosis of asthma? |
1. Episodic symptoms of airflow obstruction of hyper-responsiveness 2. Obstructive airflow is at least partially reversible 3. Alternative diagnoses are excluded |
|
|
How should you initially evaluate a patient with asthma? |
1. Classify asthma severity 2. Assess the patient's knowledge and skills for self-management 3. Identify and control environmental factors and comorbid conditions that may aggravate asthma 4. Offer appropriate meds |
|
|
What factors do you use to classify asthma severity? |
- Frequency of symptoms - Frequency of night-time awakenings - Frequency of short-acting beta-2 agonist use for symptom control - Interference with normal activity - FEV1 value - FEV1/FVC ratio |
|
|
What are the characteristics of "intermittent" asthma severity? |
- Symptoms: ≤2 days/week - Nighttime awakenings: ≤2x/month - Short-acting beta2-agonist use for symptom control: ≤2 days/week - Interference with normal activity: none - Lung function: normal FEV1 between exacerbations, FEV1>80% predicted, FEV1/FVC normal - Exacerbations requiring oral systemic corticosteroids: 0-1/year |
|
|
What are the characteristics of "persistent mild" asthma severity? |
- Symptoms: >2 days/week, but not daily - Nighttime awakenings: 3-4x/month - Short-acting beta2-agonist use for symptom control: >2 days/week, but not daily, and not more than 1x on any day - Interference with normal activity: minor limitation - Lung function: FEV1 >80% predicted, FEV1/FVC normal - Exacerbations requiring oral systemic corticosteroids: ≥2 / year |
|
|
What are the characteristics of "persistent moderate" asthma severity? |
- Symptoms: daily - Nighttime awakenings: >1x/week but not nightly - Short-acting beta2-agonist use for symptom control: daily - Interference with normal activity: some limitation - Lung function: FEV1 60-80% predicted, FEV1/FVC reduced 5% - Exacerbations requiring oral systemic corticosteroids: ≥2/year |
|
|
What are the characteristics of "persistent severe" asthma severity? |
- Symptoms: throughout the day - Nighttime awakenings: often 7x/week - Short-acting beta2-agonist use for symptom control: several times per day - Interference with normal activity: extremely limited - Lung function: FEV1 <60% predicted, FEV1/FVC reduced >5% - Exacerbations requiring oral systemic corticosteroids: ≥2/year |
|
|
How do you distinguish the classification of asthma severity based on symptoms? |
- Intermittent: ≤2 days/week - Mild persistent: >2 days/week but not daily - Moderate persistent: daily - Severe persistent: throughout the day |
|
|
How do you distinguish the classification of asthma severity based on night-time awakenings? |
- Intermittent: ≤2x/month - Mild persistent: 3-4x/month - Moderate persistent: >1x/week - Severe persistent: often 7x/week |
|
|
How do you distinguish the classification of asthma severity based on short-acting beta-2 agonist use for symptom control? |
- Intermittent: ≤2 days/week - Mild persistent: >2 days/week but not daily and not more than 1x on any day - Moderate persistent:daily - Severe persistent: several times per day |
|
|
How do you distinguish the classification of asthma severity based on interference with normal activity? |
- Intermittent: none - Mild persistent: minor limitation - Moderate persistent: some limitation - Severe persistent: extremely limited |
|
|
How do you distinguish the classification of asthma severity based on lung function? |
- Intermittent: normal FEV1 between exacerbations, FEV1>80% predicted, FEV1/FVC normal - Mild persistent: FEV1 >80% predicted, FEV1/FVC normal - Moderate persistent: FEV1 60-80% predicted, FEV1/FVC reduced 5% - Severe persistent: FEV1 <60% predicted, FEV1/FVC reduced >5% |
|
|
What is a normal FEV1/FVC based on age? |
- 8-19 years: 85% - 20-39 years: 80% - 40-59 years: 75% - 60-80 years: 70% |
|
|
What kinds of cells are affected by asthma? |
- Mast cells - Eosinophils - T lymphocytes - Macrophages - Neutrophils - Epithelial cells |
|
|
What is the appropriate treatment for moderate persistent asthma? |
Either: - Combination of low-dose inhaled corticosteroid and long-acting beta2-agonist inhaler (systematic review makes this a more effective treatment) OR - Mediam-dose inhaled corticosteroid alone |
|
|
How can you reduce exposure to dust mites? |
- Use allergen-proof covers and mattress covers - Remove carpet if possible - Reduce clutter and objects that collect dust - Wash bedding in hot water |
|
|
What other measures can be done to help patients with allergies? |
- Frequent vacuuming with HEPA filter or microfilmer bag - Use a humidifier or air-conditioning to keep the house at low humidity |
|
|
How can you reduce exposure to pollen allergens? |
- Keep windows in the car and house closed - Use A/C - Avoid outdoor activities when pollen counts are high |
|
|
What is the best pharmaceutical therapy for allergic rhinitis? |
- Nasal corticosteroids are the most effective --> improve symptoms of nasal blockage, nasal discharge, sneezing, nasal itch, and post-nasal drip compared to antihistamines
- Allergen immunotherapy (shots) assist in controlling symptoms and decreasing medication use in patients with seasonal allergic rhinitis |
|
|
What immunizations should be offered to a 40-year old patient with asthma? |
- Influenza vaccine - due to age - Tetanus, Diphtheria, accellular Pertussis vaccine - due to age - Pneumococcal Polysaccharide (PPSV) vaccine - due to asthma |
|
|
For whom is the Haemophilus influenza type B conjugate vaccine offered? |
For children only |
|
|
For whom is the Pneumococcal Polyconjugate Valent (PCV13) vaccine offered? |
Children and adults with other specific chronic medical conditions (but not chronic lung disease) |
|
|
What is on an "asthma plan"? |
- Top of the sheet: long-term controller and quick-relief meds and their dosages and instructions on use - Bottom of the sheet: defines three levels of asthma control, green zone (doing well), yellow zone (getting worse), and red zone (medical alert) - At the bottom of the red zone section is a short description of what symptoms should prompt the patient to call 911 and go to the ER
- 2nd page details environmental factors that may make asthma worse, these are best addressed while pt is in green zone to prevent further exacerbations |
|
|
What are the three levels of asthma control? |
- Green zone = doing well - Yellow zone = getting worse - Red zone = medical alert |
|
|
How can patients monitor their asthma at home? |
With a peak flow meter - measure twice per day |
|
|
How can you determine how well controlled a patient's asthma is based on their peak flow reading? |
- Green = doing well = peak flow >80% of best peak flow - Yellow = getting worse = peak flow 50-79% of best peak flow - Red = medical alert = peak flow <50% of best peak flow |
|
|
What are red zone signs and symptoms? |
- Very short of breath including when walking or talking - Gray or blue lips or fingernails - Symptoms not improving with quick-acting meds - A peak flow reading that is <50% of the personal best reading |
|
|
What are long-term effects from asthma? |
- Airway remodeling - Subepithelial fibrosis - Angiogenesis - Airway smooth muscle hypertrophy - Mucus gland hyperplasia and hyper-secretion - Incomplete reversibility of airway obstruction |
|
|
How can you evaluate a patient for a chronic sinus infection? |
CT scan of sinuses |
|
|
How important is patient education in the treatment of asthma? |
- Increased hospitalization rates for patients with non-adherence to treatment plans - 88% of patients with asthma did not properly follow their regimen of inhaled meds |
|

What do you seen on this CT scan? |

- Ethmoid sinus opacification - Maxillary sinus mucosal thickening |
|
|
How do you treat chronic sinusitis? |
- Maximize treatment for allergic rhinitis, including regular use of nasal corticosteroids and if indicated, allergen immunotherapy - Regular nasal saline irrigation is a useful adjunct, though not as effective as nasal corticosteroids - NO evidence to support the use of antibiotics |
|
|
What does red eye signify? |
Ocular inflammation |
|
|
What is the most common cause of red eye? |
Conjunctivitis |
|
|
What are other common causes of red eye besides conjunctivitis? |
- Blepharitis - Corneal abrasion - Foreign body - Subconjunctial hemorrhage - Keratitis - Iritis - Glaucoma - Chemical burn - Scleritis |
|
|
What are the signs and symptoms of red eye? |
- Discharge - Redness - Pain - Photophobia - Itching - Visual changes |
|
|
How do you differentiate and then treat the different causes of conjunctivitis? |
- Viral and bacterial - Difficult to differentiate - Therefore most cases are treated using broad-spectrum antibiotics
- Other causes are allergies or irritants |
|
|
When does red eye warrant an emergency referral to an ophthalmologist? |
- Severe pain not relieved with topical anesthetics - When topical steroids are needed - When patient has vision loss, copious purulent discharge, corneal involvement, traumatic eye injury, recent ocular surgery, distorted pupil, herpes infection, or recurrent infections |
|
|
What questions should you ask a patient presenting with red eye? |
- Unilateral or bilateral eye involvement - Duration of symptoms - Type and amount of discharge - Visual changes - Severity of pain - Photophobia - Previous treatments - Presence of allergies or systemic disease - Use of contact lenses |
|
|
What should the physical exam include in a patient with red eye? |
- Eyelids - Lacrimal sac - Pupil size and reaction to light - Corneal involvement - Pattern and location of hyperemia - Pre-auricular lymph node involvement - Visual acuity |
|
|
What is the most common cause of viral conjunctivitis? |
Adenovirus |
|
|
How does the cause of viral conjunctivitis differ in terms of how contagious it is? |
- Adenovirus is highly contagious - Other viruses (e.g., HSV) is less likely to survive |
|
|
How does viral conjunctivitis spread? |
Through direct contact with contaminated fingers, medical instruments, swimming pool water, or personal items
|
|
|
What is the typical clinical presentation of viral conjunctivitis? |
Mild with spontaneous remission after one to two weeks |
|
|
How do you treat viral conjunctivitis? |
Supportive, may include cold compresses, ocular decongestants, and artificial tears
Topical antibiotics are rarely necessary because secondary bacterial infections are uncommon |
|
|
How should you prevent the spread of viral conjunctivitis? |
- Strict hand washing - Avoid sharing personal items - Food handlers and health care workers should not work until eye discharge ceases - Physicians should clean instruments after every use |
|
|
When should referral to an ophthalmologist be made for viral conjunctivitis? |
If symptoms do not resolve after 7-10 days or if there is corneal involvement
Suspected ocular herpetic infection
Topical corticosteroid therapy for any cause of red eye is used only under direct supervision of an ophthalmologist |
|
|
How contagious is bacterial conjunctivitis? |
Highly contagious |
|
|
How is bacterial conjunctivitis spread? |
Through direct contact with contaminated fingers |
|
|
How can you categorize bacterial conjunctivitis? Wha tis the most common form? |
Based on duration and severity of signs/symptoms: - Hyperacute - Acute - most common form - Chronic |
|
|
What is the most common cause of hyper acute bacterial conjunctivitis? |
Neisseria gonorrhoeae in sexually active adults |
|
|
What are the characteristics of hyper acute bacterial conjunctivitis? |
- Sudden onset - Progresses rapidly - Leads to corneal perforation - Copious, purulent discharge - Pain - Diminished vision loss |
|
|
How should you manage a patient with hyper acute bacterial conjunctivitis? |
Prompt ophthalmology referral for aggressive management |
|
|
What are the signs/symptoms of acute bacterial conjunctivitis? |
Signs and symptoms last for less than 3-4 weeks |
|
|
What are the common causes of acute acute bacterial conjunctivitis? |
- Staphylococcus aureus (adults) - Streptococcus pneumoniae and Haemophilus influenzae (children) |
|
|
What are the characteristics of chronic bacterial conjunctivitis? |
>4 weeks with frequent relapses |
|
|
How should you treat a patient with chronic bacterial conjunctivitis? |
Refer to an ophthalmologist |
|
|
When should you identify bacteria and sensitivities to antibiotics for patients with bacterial conjunctivitis? |
Only in patients with: - Severe cases - Immunocompromise - Contact lenses - In neonates - When initial treatment fails |
|
|
What are the pros/cons of antibiotic treatment for conjunctivitis? |
- Quicker recovery - Early return to work or school - Prevention of further complications - Decreased future physician visits
- Increased antibiotic resistance - Additional expense for patient - Medicalization of minor illness |
|
|
Is bacterial conjunctivitis self-limiting? How often? What percent of patients? |
65% of patients improved after 2-5 days without antibiotic treatment |
|
|
How often are bacterial pathogens isolated from clinically diagnosed bacterial conjunctivitis cases? |
50% |
|
|
Should you immediately treat acute bacterial conjunctivitis? |
Delaying antibiotic therapy is an option
A shared decision making approach is appropriate, and many patients are willing to delay antibiotic therapy when counseled about the self-limiting nature of the disease
Some schools require proof of antibiotic treatment for at least 2 days before readmitting patients |
|
|
For whom should you consider immediate antibiotic therapy for acute bacterial conjunctivitis? |
- Health care workers - Patients who are in a hospital or other health care facility - Patients with risk factors, such as immune compromise, uncontrolled DM, contact lens use, dry eye, or recent ocular surgery - Children going to schools or day care centers that require antibiotic therapy before returning |
|
|
For whom should you consider delaying antibiotic therapy for acute bacterial conjunctivitis? |
- Patients without risk factors who are well informed and have access to follow-up care - Patients without risk factors who do not want immediate antibiotic therapy |
|
|
What should you do for a patient treated with antibiotics for acute bacterial conjunctivitis if it does not improve within one week of treatment? |
Refer to an ophthalmologist |
|
|
What diagnosis should you consider in sexually active patients who have typical signs/symptoms of bacterial conjunctivitis and do not respond to standard antibacterial treatment? |
Chlamydial conjunctivitis |
|
|
How do you diagnose chlamydial conjunctivitis? |
PCR testing of conjunctival scrapings (but not usually needed) |
|
|
How do you treat chlamydial conjunctivitis? |
- Topical therapy with erythromycin ophthalmic ointment - Oral therapy with azithromycin (Zithromax; single 1-g dose) or doxycycline (100 mg BID for 14 days)
- Must also treat patient's sexual partners |
|
|
What diagnosis should you consider in a patient with conjunctivitis who also has associated atopic diseases (e.g., allergic rhinitis, eczema, asthma)? |
Allergic conjunctivitis |
|
|
How common are ocular allergies in the U.S.? |
25% of the population |
|
|
What are the signs/symptoms of allergic conjunctivitis? |
* Itching of the eyes - Seasonal is the most common form and symptoms are related to season-specific aeroallergens - Perennial allergic conjunctivitis persists throughout the year |
|
|
How do you treat patients with allergic conjunctivitis? |
- Avoiding exposure to allergens - Use artificial tears - OTC anti-histamine / vasoconstrictor agents are effective in treating mild allergic conjunctivitis - More effective option is second-generation topical histamine H1 receptor antagonist |
|
|
What is the technical name for dry eyes? |
Keratoconjunctivitis sicca |
|
|
What causes dry eyes? |
Decreased tear production or poor tear quality |
|
|
What are dry eyes associated with? |
- Increased age - Female sex - Medications (eg, anticholinergics) - Some medical conditions |
|
|
What is the single best diagnostic test for dry eye? |
Tear osmolarity
Combine tear osmolarity with assessment of tear turnover rate and evaporation |
|
|
What should you do if you suspect Sjögren syndrome? |
Test for auto-antibodies |
|
|
How should you treat dry eyes? |
- Frequent application of artificial tears throughout the day - Nightly application of lubricant ointments, which reduces the rate of tear evaporation - Use of humidifiers and well-fitting eyeglasses with side shields can decrease tear loss |
|
|
What should you do if artificial tears cause itching or irritation? |
Switch to preservative free form or an alternative preparation |
|
|
What should you do for treatment if inflammation is the main factor in dry eye? |
- Cyclosporine ophthalmic drops (restasis) - may increase tear production - this may take several months to provide subjective improvement - Systemic omega-3 fatty acids - Topical corticosteroids |
|
|
What is the goal of treatment for dry eye? |
To prevent corneal scarring and perforation |
|
|
When should you refer a patient for an ophthalmology appointment to treat dry eyes? |
If the patient needs topical steroid therapy or surgical procedures |
|
What is the term for chronic inflammation of the eyelid margins? |
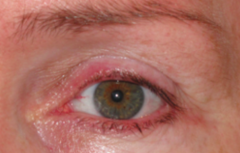
Blepharitis |
|
|
What should you examine for in a patient presenting with chronic inflammation of the eyelid margins? |
- Scalp or facial skin flaking (seborrheic dermatitis) - Facial flushing and redness and swelling on the nose or cheeks (rosacea) |
|
|
How do you treat patients with chronic inflammation of the eyelid margins (Blepharitis)? |
Continue indefinitely: - Eyelid hygiene (cleansing with mild soap, such as diluted baby shampoo or eye scrub solution) - Gentle lid massage - Warm compresses
If patients don't respond to eyelid hygiene: - Topical erythromycin or bacitracin ophthalmic ointment to eyelids - Or azithromycin eye drops |
|
|
How do you treat patients with SEVERE chronic inflammation of the eyelid margins (Blepharitis)? |
Prolonged use of oral antibiotics (doxycycline or tetracycline)
Topical steroids may also be useful for severe cases |
|
|
How do you diagnose a corneal abrasion? |
- Clinical presentation and eye exam - Short-term topical anesthetics may be used to facilitate eye exam - Fluorescein staining under a cobalt blue filter or Wood lamp is confirmatory - a branching pattern of staining suggests HSV infection of a healing abrasion |
|
|
What should you do if there is HSV infection with corneal involvement? |
Ophthalmology referral within 1-2 days |
|
|
What should you look for in a patient with a corneal abrasion? |
Retained foreign body under the upper eyelid |
|
|
How should you treat a patient with a corneal abrasion? |
- Supportive care - Cycloplegics (atropine, cyclopentolate / Cyclogyl, homatropine, scopolamine, tropicamide) - Pain control (topical NSAIDs or oral analgesics)
|
|
|
What therapies are not indicated for patients with a corneal abrasion? |
- The need for topical antibiotics for uncomplicated abrasions has not been proven - Topical aminoglycosides should be avoided because they are toxic to corneal epithelium - Eye patches do not improve comfort or healing - All steroid preps are contraindicated |
|
|
When should you refer a patient with a corneal abrasion to an ophthalmologist? |
- If symptoms worsen or do not resolve within 48 hours - If there is HSV infection with corneal involvement |
|

What should you do for patients with subconjunctival hemorrhage? |
Blood reabsorption over a few weeks, no treatment needed
Warm compresses and ophthalmic lubricants (eg, hydroxpropyl cellulose, methylcellulose, or artificial tears) may relieve symptoms |
|
|
If a patient with subconjunctival hemorrhage has pain, how should you evaluate this patient differently? |
You need to identify a cause - Check for corneal involvement or penetrating injury - Consider urgent referral to ophthalmology - Recurrent hemorrhages may require a workup for bleeding disorders - If patient is taking warfarin (Coumadin), the INR should be checked |
|

What is the term for localized area of inflammation involving the superficial layers of the episclera? |
Episcleritis |
|
|
How long does episcleritis last? |
Lasts up to three weeks |
|
|
When should you investigate underlying causes of episcleritis? |
Only for recurrent episodes and for symptoms suggestive of associated systemic diseases, such as rheumatoid arthritis |
|
|
How do you treat episcleritis? |
- Supportive care - Use of artificial tears - Topical steroids may be useful for severe cases
- Topical NSAIDs have not been shown to have significant benefit over placebo |
|
|
When should you refer to ophthalmologist for patients with episcleritis? |
- Recurrent episodes - Unclear diagnosis (early scleritis) - Worsening symptoms |
|
|
What is the first thing you should use to distinguish the underlying cause of red eye? |
Pain: - Mild or no pain, with mild blurring or normal vision Vs. - Moderate to severe pain |
|
|
If a patient has mild or no pain with mild blurring or normal vision, how should you proceed to distinguishing the cause of red eye? |
Hyperemia: - If focal hyperemia --> Episcleritis - If diffuse hyperemia --> continue |
|
|
If a patient has mild or no pain with mild blurring or normal vision and diffuse hyperemia, how should you proceed to distinguishing the cause of red eye? |
Presence of Discharge: - No: subconjunctival hemorrhage - Yes: continue |
|
|
If a patient has mild or no pain with mild blurring or normal vision, diffuse hyperemia, and discharge, how should you proceed to distinguishing the cause of red eye? |
- Intermittent discharge: dry eye - Continuous discharge: continue |
|
|
If a patient has mild or no pain with mild blurring or normal vision, diffuse hyperemia, and continuous discharge, how should you proceed to distinguishing the cause of red eye? |
- Mucopurulent to purulent: chlamydial conjunctivitis or acute bacterial conjunctivitis - Watery or serous: continue |
|
|
If a patient has mild or no pain with mild blurring or normal vision, diffuse hyperemia, and continuous watery / serous discharge, how should you proceed to distinguishing the cause of red eye? |
- Mild to no itching --> viral conjunctivitis - Moderate to severe itching --> allergic conjunctivitis |
|
|
What are the types of ophthalmic therapies for acute bacterial conjunctivitis? Which is best? |
Any ophthalmic antibiotic may be used for the treatment of acute bacterial conjunctivitis because they have similar cure rates: - Azithromycin 1% - Besifloxacin 0.6% - Ciprofloxacin 0.3% - Erythromycin 0.5% - Gatifloxacin 0.3% - Gentamicin 0.3% - Levofloxacin 1.5% or 0.5% - Moxifloxacin 0.5% - Ofloxacin 0.3% - Sulfacetamide 10% - Tobramycin 0.3% - Trimethoprim / Polymyxin B |
|
|
What are the signs/symptoms of keratitis (corneal inflammation)? |
- Diminished vision - Corneal opacities / white spot - Fluorescein staining under Wood lamp shows corneal ulcers - Eyelid edema - Hypopyon - Painful red eye - Photophobia - Mucopurulent discharge - Foreign body sensation |
|
|
What are the causes of keratitis (corneal inflammation)? |
- Bacterial: Staphylococcus species, Streptococcus - Viral: HSV, VZV, Ebstin-Barr virus, Cytomegalovirus - Abrasion from foreign body - Contact lenses |
|
|
What are the signs/symptoms of iritis? |
- Diminished vision - Poorly reacting, constricted pupils - Ciliary, perilimbal injection - Constant eye pain (radiating into brow/temple) developing over hours - Watering red eye - Blurred vision - Photophobia |
|
|
What are the causes of iritis? |
- Exogenous infection from perforating wound or corneal ulcer - Autoimmune conditions |
|
|
What are the signs/symptoms of glaucoma? |
- Marked reduction in visual acuity - Dilated pupils react poorly to light - Diffuse redness - Eyeball is tender and firm to palpation - Acute onset of severe, throbbing pain - Watering red eye - Halos appear when patient is around lights |
|
|
What are the causes of glaucoma? |
Obstruction to outflow of aqueous humor leading to increased intraocular pressure |
|
|
What are the signs/symptoms of chemical burn? |
- Diminished vision - Corneal involvement (common) - Severe, painful red eye - Photophobia |
|
|
What are the common causes of chemical burn to the eye? |
- Cement - Plaster powder - Oven cleaner - Drain cleaner |
|
|
What are the signs/symptoms of scleritis? |
- Diffuse redness - Diminished vision - Tenderness - Scleral edema - Corneal ulceration - Severe, boring pain radiating to periorbital area - Pain increases with eye movements - Ocular redness - Watery discharge - Photophobia - Intense nighttime pain - Pain upon awakening |
|
|
What are the causes of scleritis? |
Systemic diseases such as: - Rheumatoid arthritis - Wegener granulomatosis - Reactive arthritis - Sarcoidosis - Inflammatory bowel disease - Syphilis - Tuberculosis |
|
|
For what types of upper respiratory tract infections are antibiotics indicated early? |
- Acute otitis media - Group A beta-hemolytic streptococcal pharyngitis - Epiglottitis - Bronchitis caused by pertussis |
|
|
For what types of upper respiratory tract infections are antibiotics indicated later? |
Persistent cases of rhino-sinusitis if symptoms persist beyond a period of observation |
|
|
How common are uncomplicated URIs? |
25 million visits to FPs |
|
|
How often do patients miss work or school for URIs? |
20-22 million days of absence |
|
|
How often are URIs treated with antibiotics? |
65% |
|
|
What are the negative consequences of overuse of antibiotics for URIs? |
- Leads to resistance - Increased cost - Increased incidence of adverse effects, including anaphylaxis |
|
|
What are the common signs/symptoms of the common cold? |
- Mild, self-limited - Runny nose - Sore throat - Cough - Sneezing - Nasal congestion |
|
|
Who is most commonly affected by influenza? |
Children |
|
|
How do you treat patients with influenza? |
** Supportive care
- Antiviral therapy (neuraminidase inhibitor = oseltamivir and zanamivir) may decrease the duration of the illness by one day if started within 48 hours of onset |
|
|
When should patients with influenza be treated with antivirals? |
- Pts older than 65 years - Pts younger than 2 years - Pregnant women - Those with chronic illnesses |
|
|
When would antibiotics be indicated in a patient with influenza? |
If there is concern for secondary bacterial process - a gram stain and cultures of body fluids |
|
|
What is the incidence of acute rhino-sinusitis in adults? |
13% |
|
|
What is rhino-sinusitis? |
Inflammation of the nasal mucosa and sinuses |
|
|
What are the symptoms of rhino-sinusitis? |
- Nasal obstruction - Anterior or posterior purulent nasal discharge - Facial pain - Decrease in sense of smell - Cough |
|
|
When is rhino-sinusitis considered acute vs subacute vs chronic? |
- Acute: <4 weeks - Subacute: 4-12 weeks - Chronic: >12 weeks |
|
|
How can you determine the difference between viral and bacterial rhino-sinusitis? |
Acute bacterial rhino-sinusitis should not be made until symptoms have persisted for at least 10 days or after initial improvement followed by worsening of symptoms |
|
|
What symptoms are more predictive of bacterial rather than viral rhino-sinusitis? |
- Purulent nasal discharge - Maxillary tooth or facial pain - Unilateral maxillary sinus tenderness - Worsening symptoms after initial improvement |
|
|
How should you treat mild cases of acute bacterial rhino-sinusitis? |
- Managed with watchful waiting if appropriate follow-up can be ensured - Worsening symptoms within 7 days warrant the initiation of antibiotics in these patients |
|
|
Antibiotics for bacterial rhino-sinusitis should cover what bugs? What antibiotics are first line? |
- Strep pneumoniae - Haemophilus influenzae - Moraxella catarrhalis
First-line: amoxicillin or TMP-SMX (for PCN allergies) |
|
|
Whens should you consider switching to a different antibiotic for treatment of bacterial rhino-sinusitis? |
If symptoms worsen within 7 days |
|
|
How long should antibiotics be used for treating bacterial rhino-sinusitis? |
Short course (5 days) is as effective as long-course (10 days) |
|
|
How do you diagnose acute otitis media? |
- Acute onset of symptoms - Presence of middle ear effusion - Signs/symptoms of middle ear inflammation |
|
|
What are the most common causes of otitis media? |
- H. influenzae - S. pneumoniae - M. catarrhalis |
|
|
What are other common causes of otitis media in infants up to 8 weeks of age? |
- Group B streptococcus - Gram negative enteric bacteria - Chlamydia trachomatis |
|
|
When is observation in cases of otitis media an acceptable plan? When should you initiate antibiotics? |
- For children >6 months - Defer antibiotics for 48-72 hours, initiate therapy only if symptoms persist or worsen |
|
|
How should you evaluate a febrile infant (up to 8 weeks of age) with acute otitis media? |
Full sepsis workup - Otolaryngology consultation if available for tympanocentesis |
|
|
When is immediate initiation of antibiotics recommended for acute otitis media? |
Children <2 years with bilateral AOM and in those with AOM and otorrhea |
|
|
What is the first-line treatment for acute otitis media? |
Amoxicillin (80-90 mg/kg/day in two divided doses) |
|
|
When should you follow-up with a patient being treated with amoxicillin for acute otitis media? How should you evaluate? |
- If no response within 48-72 hours, need to follow-up, re-examine, and confirm diagnosis - If no response, Augmentin (Amoxcillin/Clavulanate) should be started
- If vomiting, use Ceftriaxone (Rocephin) |
|
|
How does the time course of antibiotics for acute otitis media affect efficacy of treatment? |
Longer courses of antibiotics (>7 days) have lower failure rates than shorter courses |
|
|
When should you follow-up with a child with acute otitis media? |
Check in 3 months to document clearance of middle ear effusion |
|
|
Are antibiotics recommended for the treatment of otitis media with effusion? |
No, they only have modest short-term benefit |
|
|
How commonly is a pharyngitis caused by a viral infection? |
- 90% of adults - 70% of children |
|
|
What is the leading cause of bacterial pharyngitis? |
Group A beta-hemolytic streptococcus |
|
|
What are the benefits of treating Group A beta-hemolytic streptococcus pharyngitis with antibiotics? |
- Decrease the risk of rheumatic fever - Alleviate symptoms - Decreases communicability |
|
|
What is antibiotic therapy for Group A beta-hemolytic streptococcus pharyngitis not effective at preventing? |
- Glomerulonephritis - Inconsistent results in the prevention of peritonsillar abscess |
|
|
What criteria can be used to help diagnose strep throat? |
"Modified Centor criteria": - Age: (1) 3-14 years, (0) 15-45 years, (-1) >45 years - (1) Absence of cough - (1) Anterior cervical lymphadenopathy - (1) Fever - (1) Tonsillar erythema or exudates
If ≤1, does not require further testing or treatment (unless they have 1 point and hx of contact w/ a patient with documented strep, then they should be tested)
If 2-3, have rapid antigen detection testing, if positive give antibiotics
If 4-5, give antibiotics without testing |
|
|
How do you get points for the modified Centor criteria for strep throat? |
- Age: (1) 3-14 years, (0) 15-45 years, (-1) >45 years - (1) Absence of cough - (1) Anterior cervical lymphadenopathy - (1) Fever - (1) Tonsillar erythema or exudates |
|
|
What does a score of ≤1 mean for working up a patient you think may have strep throat? |
If ≤1, does not require further testing or treatment (unless they have 1 point and hx of contact w/ a patient with documented strep, then they should be tested) |
|
|
What does a score of 2-3 mean for working up a patient you think may have strep throat? |
If 2-3, have rapid antigen detection testing, if positive give antibiotics |
|
|
What does a score of 4-5 mean for working up a patient you think may have strep throat? |
If 4-5, give antibiotics without testing |
|
|
What is the recommended therapy for patients with strep throat? |
10-day course of Penicillin
Erythromycin can be used in patients allergic to PCN
Other alternatives: Amoxicillin, Azithromycin (Zithromax), and first-generation cephalosporins (Cefazolin, Cephalexin) are appropriate alternatives |
|
|
What is the term for inflammation of the vocal cords and larynx? |
Laryngitis |
|
|
What is the time course of "acute" laryngitis? |
Less than 3 weeks |
|
|
What are the symptoms of laryngitis? |
- Loss or muffling of the voice - Sore throat - Other classic URI symptoms: cough, fever, runny nose, headache |
|
|
How should you treat laryngitis? |
Antibiotic therapy does not reduce the duration or lead to voice improvement!! |
|
|
What is the most likely cause of laryngitis? |
Virus |
|
|
What is epiglottitis? |
Inflammatory condition of the epiglottis and adjacent supraglottic structures that can rapidly progress to airway compromise and potentially death |
|
|
What has decreased the incidence of epiglottitis? |
H. influenzae type b (Hib) conjugate vaccines in early infancy |
|
|
How can you treat epiglottitis? |
Combination of IV anti-staphylococcal agent that is active against MRSA + 3rd-generation cephalosporin (Ceftriaxone, Cefotaxime, Cefdinir)
IV mono therapy with Ceftriaxone, Cefotaxime, or Ampicillin/Sulbactam (Unasyn) is also recommended |
|
|
What diagnosis presents with cough and possibly phlegm production? Cause? |
Bronchitis - inflammation of large airways due to viral infection |
|
|
How should patients with acute bronchitis be treated? |
Antibiotics are not effective since most cases are due to viruses
Focus on symptom relief, as well as explaining to patients why antibiotics are not indicated |
|
|
What are some non-viral causes of bronchitis? |
- Bordetella pertussis - Atypical bacteria - Chlamydia pnumoniae - Mycoplasma pneumoniae |
|
|
Should bacterial causes of bronchitis be treated with antibiotics? |
There are a few bacterial causes but they don't need to be treated with antibiotics because these are self-limited conditions except in rare cases in which pneumonia develops or the patient is immunocompromised |
|
|
If a child has a cough and you suspect pertussis, what should you do to treat? |
Macrolides should be given early in the course (this is to curb the spread of the disease, rather than to change patient outcomes)
Macrolides = Azithromycin, Erythromycin, etc |
|
|
What are the clinical features of pneumonia? |
- Cough - Fever - Pleuritic chest pain |
|
|
When initially evaluating community acquired pneumonia, what do you need to decide? |
Whether the patient can be managed as an out-patient or requires hospitalization --> using validated mortality or severity prediction scores |
|
|
What diagnostic test is indicated for patients requiring hospitalization for pneumonia but is not useful for patients who can be treated as an out-patient? |
Sputum and blood cultures |
|
|
What should initial out-patient therapy for pneumonia consist of? |
Macrolide (Azithromycin, Erythromycin) or Doxycycline |
|
|
What therapy should be given for out-patients with pneumonia and co-morbidities? |
- Respiratory fluoroquinolone (Levofloxacin, Gemifloxacin, or Moxifloxacin) OR - Beta-lactam antibiotic + macrolide |
|
|
What therapy should be given for out-patients with pneumonia who have used antibiotics within the previous three months? |
- Respiratory fluoroquinolone (Levofloxacin, Gemifloxacin, or Moxifloxacin) OR - Beta-lactam antibiotic + macrolide |
|
|
What therapy should be given for in-patients with pneumonia who are not in the ICU? |
- Respiratory fluoroquinolone (Levofloxacin, Gemifloxacin, or Moxifloxacin) OR - Beta-lactam antibiotic + macrolide |
|
|
What therapy should be given for patients with pneumonia and risk factors for Pseudomonas? |
Beta-lactam antibiotic (Piperacillin/Tazobactam, Imipenem/Cilastatin, Meropenem, Doripenem, or Cefepime) + Aminoglycoside + Azithromycin OR anti-pseudomonal fluoroquinolone (levofloxacin or ciprofloxacin) |
|
|
What are the pseudomonal fluoroquinolone? |
Levofloxacin and Ciprofloxacin |
|
|
What therapy should be given to patients with pneumonia and risk factors for MRSA? |
Vancomycin or Linezolid |
|
|
When can hospitalized patients with pneumonia be switched from IV to oral antibiotics? |
After they have clinical improvement and are able to tolerate PO meds, typically in first 3 days |
|
|
What should physicians promote as a means to prevent community-acquired pneumonia and pneumococcal bacteremia? |
Pneumococcal and influenza vaccinations |
|
|
What are the criteria for classifying pneumonia as "community-acquired"? |
- Not acquired in the hospital - Not acquired in a long-term care facility - No recent contact with the health care system |
|
|
What are the common etiologies of community-acquired pneumonia that is appropriate for out-patient treatment? |
Median percentage in parentheses - Mycoplasma pneumoniae (16) - Respiratory viruses (15) - Streptococcal pneumoniae (14) - Chlamydophila pneumoniae (12) - Legionella species (2) - Haemophilus influenzae (1) - Unknown (44) |
|
|
What are the common etiologies of community-acquired pneumonia that requires in-patient treatment but not in the ICU? |
Median percentage in parentheses - Streptococcal pneumoniae (25) - Respiratory viruses (10) - Mycoplasma pneumoniae (6) - Haemophilus influenzae (5) - Chlamydophila pneumoniae (3) - Legionella species (3) - Unknown (37) |
|
|
What are the common etiologies of community-acquired pneumonia that requires in-patient treatment in the ICU? |
Median percentage in parentheses: - S. pneumoniae (17) - Legionella species (10) - Gram negative bacilli (5) - Staphylococcus aureus (5) - Respiratory viruses (4) - Haemophilus influenzae (3) - Unknown (41) |
|
|
What is the 8th leading cause of death in the U.S.? |
Pneumonia and influenza combined |
|
|
What is the most common cause of infection related mortality in the U.S.? |
Pneumonia and influenza |
|
|
How common is death from influenza or pneumonia in a year? |
~50,000 |
|
|
How common is the annual incidence of CAP? |
5-11 / 1000 persons (more common in winter months) |
|
|
How common are ambulatory visits for CAP in the U.S. annually? |
>4 million |
|
|
What is the most commonly identified pathogen that causes CAP? |
S. pneumoniae |
|
|
How much does CAP cost the U.S. yearly? |
>$17 billion |
|
|
What is the typical cause of pneumonia? |
S. pneumoniae |
|
|
What are the atypical causes of pneumonia? |
- Mycoplasma pneumoniae - Chlamydophila pneumonia - Legionella species - Respiratory viruses |
|
|
What are the common symptoms of pneumonia? |
- Fever - Chills - Pleuritic chest pain - Cough producing mucopurulent sputum |
|
|
What factors are associated with CAP caused by Legionella infection? |
- High fever (>104 F) - Male sex - Multilobar involvement - GI and neurologic abnormalities |
|
|
How does the presentation of pneumonia differ in the elderly? |
- More subtle, may not have classic symptoms - Present with weakness and decline in functional and mental status |
|
|
What should the patient history focus on when you suspect pneumonia? |
- Detect symptoms consistent with CAP - Underlying defects in host defenses - Possible exposure to specific pathogens - Ask about occupations, animal exposures, sexual history, recent travel history |
|
|
What kinds of patients have increased incidence of CAP? |
- Pts with COPD - Pts with HIV |
|
|
What increases your risk for Legionella pneumonia? |
Stays at hotels and on cruise ships (in last 2 weeks) |
|
|
What are the physical exam findings in pneumonia? |
- Fever - Dullness to percussion - Egophony - Tachycardia - Tachypnea - Rales or bronchial breath sounds
- Relatively uncommon, but highly specific: asymmetric breath sounds, pleural rubs, egophony, increased fremitus |
|
|
What physical exam finding of pneumonia is more common in older patients? |
Tachypnea (up to 70% of those >65 years) |
|
|
When should you get a CXR in a patient you consider may have pneumonia? |
Any patient with at least one of the following abnormal vital signs: - T >100 - HR >100 bpm - RR >20 breaths/min
Any patient with at least 2 of the following clinical findings: - Decreased breath sounds - Crackles (rales) - Absence of asthma |
|
|
What is required for diagnosis of CAP? |
Infiltrate on lung imaging |
|
|
What CXR findings suggest a bacterial etiology? |
- Lobar consolidation - Cavitation - Pleural effusions |
|
|
What CXR findings suggest Legionella or viral pneumonia? |
Diffuse parenchymal involvement |
|
|
What sorts of criteria should make you do diagnostic testing in patients you think have CAP to further determine the pathogen to direct therapy? |
- Admission to ICU - Alcohol abuse - Asplenia - Cavitary infiltrates - Chronic severe liver disease - Leukopenia - Out-patient therapy ineffective - Pleural effusion - Positive Legionella urine antigen test result - Positive pneumococcal urine antigen test result - Recent travel (within past 2 weeks) - Severe obstructive lung disease |
|
|
What diagnostic testing should you do in a patient you suspect of having CAP who also is admitted to the ICU? |
- Blood cultures - Sputum cultures - Legionella urine antigen test - Pneumococcal urine antigen test - Endotracheal aspirate if intubated |
|
|
What diagnostic testing should you do in a patient you suspect of having CAP who also is known to abuse alcohol? |
- Blood cultures - Sputum cultures - Legionella urine antigen test - Pneumococcal urine antigen test |
|
|
What diagnostic testing should you do in a patient you suspect of having CAP who also has asplenia? |
- Blood culture - Pneumococcal urine antigen test |
|
|
What diagnostic testing should you do in a patient you suspect of having CAP who also has a cavitary lesion? |
- Blood culture - Sputum culture - Fungal and TB cultures |
|
|
What diagnostic testing should you do in a patient you suspect of having CAP who also has severe chronic liver disease? |
- Blood culture - Pneumococcal urine antigen test |
|
|
What diagnostic testing should you do in a patient you suspect of having CAP who also has leukopenia? |
- Blood culture - Pneumococcal urine antigen test |
|
|
What diagnostic testing should you do in a patient you suspect of having CAP for whom out-patient therapy was ineffective? |
- Sputum culture - Legionella urine antigen test - Pneumococcal urine antigen test |
|
|
What diagnostic testing should you do in a patient you suspect of having CAP who also has pleural effusions? |
- Blood culture - Sputum culture - Legionella urine antigen test - Pneumococcal urine antigen test - Thoracentesis and pleural fluid cultures |
|
|
What diagnostic testing should you do in a patient you suspect of having CAP who also has positive Legionella urine antigen test results? |
Sputum culture |
|
|
What diagnostic testing should you do in a patient you suspect of having CAP who also has positive pneumococcal urine antigen test results? |
- Blood culture - Sputum culture |
|
|
What diagnostic testing should you do in a patient you suspect of having CAP who also has recent travel (within past 2 weeks)? |
Legionella urine antigen test |
|
|
What diagnostic testing should you do in a patient you suspect of having CAP who also has severe obstructive lung disease? |
Sputum culture |
|
|
How does pathogen-drive therapy compare to empiric therapy in patients with CAP? |
No statistically significant difference in mortality rate of length of hospitalization |
|
|
What factor at presentation in pneumonia is associated with increased 30-day mortality? |
Hypoglycemia |
|
|
What lab test is elevated in many patients with bacterial infections? |
Procalcitonin level (however the time to get results can be prolonged, limiting its usefulness) |
|
|
What WBC count amount is suggestive of infection but when normal does not rule out pneumonia? |
>10,400 / mm3 |
|
|
What C-reactive protein level is suggestive of infection but when normal does not rule out pneumonia? |
>5.0 mg/dL |
|
|
Does the presence of bacteremia in CAP affect outcomes? |
No increase in poor outcomes among those with bacteremia
Also, false-positive blood culture results have been associated with prolonged hospitalization and more vancomycin use |
|
|
Why should blood cultures be ordered for patients with severe CAP? |
They are more likely to be infected with bacteria other than S. pneumoniae
They are more likely to grow pathogens not covered by empiric therapy, and have the potential to influence antibiotic choice |
|
|
What do the Infectious Diseases Society of America / American Thoracic Society (IDSA/ATS) guidelines recommend about sputum specimens? |
They should be obtained before the initiation of antibiotic therapy in in-patients |
|
|
What makes a sputum culture a good-quality sample? |
Positive for neutrophils but <25 epithelial cells / low-power field |
|
|
Necrotizing or cavitary pneumonia may be caused by what? |
MRSA |
|
|
When should pleural effusions be drained by thoracentesis? |
If >5 cm on lateral CXR |
|
|
What testing should be done on thoracentesis samples in patients with pneumonia? |
- Gram stain - Aerobic and anaerobic cultures |
|
|
What tests are helpful when an adequate sputum culture is unobtainable or when antibiotic therapy has already started? |
Urine antigen tests |
|
|
How useful is the pneumococcal urine antigen test? |
- Sensitivity: 50-80% - Specificity: >90% |
|
|
How useful is the Legionella urine antigen test? |
It only detects serogroup 1, but this causes 80-95% of CAP
Sensitivity: 70-90% Specificity: 99% |
|
|
How do the results from urine antigen tests help you? |
They are better at ruling in disease when positive, a negative test does not rule out infection with a specific pathogen given its somewhat limited sensitivity |
|
|
What are the criteria for severe CAP? |
Any major criterion --> admit to ICU One or more minor criteria --> increased risk for death, admission to ICU may be appropriate
Major: - Invasive mechanical ventilation - Septic shock with need for vasopressors
Minor: - BUN ≥20 mg/dL - Confusion / disorientation - Hypotension requiring aggressive fluid resuscitation - Hypothermia (<96.8) - Leukopenia (WBC <4000) - Multilobar infiltrates - PaO2 /FiO2 ratio ≤250 - RR ≥30 breaths/min - Thrombocytopenia <100,000 |
|
|
What is the average cost of a single CAP hospitalization? |
$3000 - $13,000 |
|
|
What are the risks for patients with in-patient care for pneumonia? |
- Thromboembolic events - Superinfections (eg, C. difficile) - Catheter-associated UTIs |
|
|
What is the mortality prediction tool for patients with CAP which can help you determine in what setting your patient should be treated? |
CURB-65 - Confusion - Uremia - BUN >20 - RR ≥30 - BP (systolic <90 or diastolic ≤60) - Age ≥65 years
Score: - 0-1: treat as out-patient, 30-day mortality is 0.7-2.1% - 2: treat as in-patient, 30-day mortality is 9.2% - ≥3: treat in ICU, 30-day mortality is 15-40% |
|
|
What is the prediction tool to determine the need for intensive respiratory or vasopressor support (IRVS) for patients with CAP? |
SMART-COP - Systolic BP <90 = 2 - Multilobar CXR = 1 - Albumin level <3.5 g/dL = 1 - RR ≥25 (if <50y) or ≥30 (if >50y) = 1 - Tachycardia ≥125 bpm = 1 - Confusion = 1 - Oxygen level SaO2 ≤93% (if <50y) or ≤90% (if >50y) = 2 - pH (arterial) <7.35 = 2
Score: - 0-2: low risk of needing IRVS - 3-4: moderate risk of needing IRVS (1 in 8) - 5-6: high risk of needing IRVS (1 in 3) - ≥7: very high risk of needing IRVS (2 in 3) |
|
|
How does the score on the SMART-COP assessment help you understand who will need intensive respiratory or vasopressor support? |
Score >3 identifies 92% of those who will need IRVS |
|
|
Patients who are admitted to the ICU with CAP are more likely to be what? |
Men with CHF or COPD |
|
|
What should be the initial therapy for CAP for a patient who is previously health, can be treated as an out-patient, and has no antibiotic use in the past 3 months? |
Macrolide (Azithromycin, Erythromycin) or Doxycycline |
|
|
What should be the initial therapy for CAP for an out-patient with comorbidities or antibiotic use in the past 3 months? |
Respiratory fluoroquinolone (levofloxacin, gemifloxacin, or moxifloxacin)
OR
Beta-lactam (high-dose amoxicillin, amoxicillin / clavulanate, or cefpodoxime) + Macrolide (Azithromycin or Erythromycin) |
|
|
What should be the initial therapy for CAP for an in-patient, non-ICU? |
Respiratory fluoroquinolone (levofloxacin, gemifloxacin, or moxifloxacin)
OR
Beta-lactam (high-dose amoxicillin, amoxicillin / clavulanate, or cefpodoxime) + Macrolide (Azithromycin or Erythromycin) |
|
|
What should be the initial therapy for CAP for an in-patient ICU? |
Beta-lactam antibiotic (Ceftriaxone, Cefotaxime, or Ampicillin / Sulbactam)
+ Azithromycin OR a respiratory fluoroquinolone (levofloxacin, gemifloxacin, or moxifloxacin) |
|
|
What should be the initial therapy for CAP for a patient with risk factors for pseudomonas? |
Beta-lactam antibiotic (Pip/Tazo, Cefepime, Imipenem/Cilastatin, Meropenem, or Doripenem) + Ciprofloxacin or Levofloxacin OR The above beta-lactam + Aminoglycoside + Azithromycin OR The above beta-lactam + Aminoglycoside + anti-Pneumococcal respiratory fluoroquinolone |
|
|
What should be the initial therapy for CAP for a patient with risk factors for MRSA? |
Vancomycin or Linezolid
Consider in patients with severe CAP after an episode of influenza or viral illness; characterized by severe, bilateral, necrotizing pneumonia induced by Panton-Valentine leukocidin and other toxins. |
|
|
What should be the initial therapy for CAP from influenza virus? |
Oseltamivir (Tamiflu) or Zanamivir (Relenza) |
|
|
What is the traditional duration of therapy for patients with CAP? |
10-14 days, more recent evidence suggests a shorter course of up to 7 days is equally effective |
|
|
What oral regimen can be effective after completing IV azithromycin and ceftriaxone? |
Oral azithromycin |
|
|
How should you treat a patient with delayed response to therapy for CAP with no improvement after 72 hours? |
Considerations: - Resistant microorganism or uncovered pathogen - Parapneumonic effusion or empyema - Nosocomial super-infection - Non-infectious condition such as PE, drug fever, bronchiolitis obliterans, organizing pneumonia, CHF, vasculitis |
|
|
How should you treat a patient with CAP who has clinical deterioration or continued progression of illness? |
Considerations: - Severity of illness at presentation - Metastatic infection, such as empyema, endocarditis, meningitis, arthritis - Inaccurate diagnosis, such as acute respiratory distress syndrome, aspiration - Exacerbation of comorbid illness or co-existing non-infectious disease, such as renal failure, acute MI, PE |
|
|
How does adjunctive prednisolone therapy affect outcomes in hospitalized patients with CAP? |
One week therapy did not improve outcomes in hospitalized patients with CAP |
|
|
What drug should be considered within the first 24 hours of hospital admission for patients with severe CAP and persistent septic shock? |
Drotrecogin alfa (Xigris) |
|
|
For whom is the pneumococcal vaccination recommended? |
- Adults >65 years - Adults <65 years with chronic illnesses or asplenia - All adults who smoke or have asthma |
|
|
What is the influenza vaccine good for in older persons? |
Shown to effectively prevent pneumonia, hospitalization, and death |

