![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
247 Cards in this Set
- Front
- Back
|
Respiratory tree - conducting zone - details?
|
Consists of nose, pharynx, trachea, bronchi, bronchioles, and terminal bronchioles. Cartilage is present only in the trachea and bronchi. Brings air in and out. Warms, humidifies, filters air. Anatomic dead space. Walls of conducting airways contain smooth muscle.
|
|
|
Respiratory tree - respiratory zone - details?
|
Consists of respiratory bronchioles, alveolar ducts, and alveoli. Participates in gas exchange.
|
|
|
What type of epithelial cells exist in the respiratory conducting zone?
|
Pseudostratified ciliated columnar cells extend up to and including the terminal bronchioles, at which point the cells become cuboidal ciliated (macrophages clear debris in the alveoli)
|
|
|
Pneumocytes - Type I cells
|
97% of alveolar surfaces. Line the alveoli. Squamous; thin for optimal gas diffusion.
|
|
|
Pneumocytes - Type II cells
|
3% of alveolar surface. Secrete pulmonary surfactant (dipalmitoyl phosphatidylcholine, a.k.a. Lecithin), which decreases alveolar surface tension. Cuboidal and clustered epithelial cells.
Also serve as precursors to type I cells and other type II cells. Type II cells proliferate during lung damage. |
|
|
Pneumocytes - Clara cells
|
nonciliated; columnar with secretory granules. Secrete components of surfactant; degrade toxins; act as reserve cells.
|
|
|
What substance composes respiratory surfactant?
|
Dipalmitoyl phosphatidylcholine, a.k.a. Lecithin
|
|
|
Epithelial cell type of Type I vs. Type II pneumocytes? Clara cells?
|
Type I - Squamous
Type II - Cuboidal and clustered Clara cells - nonciliated, columnar with secretory granules |
|
|
What is the ratio that is the cutoff in amniotic fluid for indicating fetal lung maturity?
|
Lecithin-to-sphingomyelin ratio > 2.0
|
|
|
Gas Exchange barrier - histology
|
Continuous endothelium with tight junctions is juxtaposed to Type I epithelial cells to create the Air-Blood barrier. Type II epithelial cells are sporadically placed one cell layer deep to the Type I cells and have Lamellar bodies. Surfactant is secreted constitutively. Macrophages are also scattered throughout, one cell layer deep to type I cell layer.
|
|
|
Lung relations - Left vs. Right lung - details?
|
Right lung has 3 lobes; Left has 2 lobes and a Lingula (homologue of right middle lobe). Right lung is more common site for inhaled foreign body because the right main stem bronchus is wider and more vertical than the left.
Instead of a middle lobe, the left lung has a space occupied by the heart. The relation of the pulmonary artery to the bronchus at each lung hilus is described by RALS - Right Anterior; Left Superior |
|
|
Aspirating a peanut - where does it go while upright? While supine?
|
Upright - lower portion of right inferior lobe
Supine - superior portion of right inferior lobe |
|
|
Name 2 fissures of the R lung. Relation in space?
|
Horizontal fissure and oblique fissure.
Horizontal fissure is superior to oblique fissure. |
|
|
Diaphragm structures
|
Structures perforating the diaphragm:
At T8: IVC At T10: Esophagus At T12: Aorta, thoracic duct, azygous vein Diaphragm is innervated by C3, 4 and 5 (phrenic nerve). Pain from the diaphragm is referred to the shoulder. |
|
|
What three structures pierce the diaphragm at T12?
|
Aorta, azygous vein, thoracic duct
|
|
|
Muscles of respiration - quiet breathing
|
Inspiration - diaphragm
Expiration - passive |
|
|
Muscles of respiration - exercise
|
Inspiration - external intercostals, scalene muscles, sternomastoids
Expiration - rectus abdominis, internal and external obliques, transversus abdominis, internal intercostals |
|
|
5 important lung products
|
1. Surfactant - produced by type II pneumocytes, decreased alveolar surface tension, increased compliance, decreased work of inspiration
2. Prostaglandins 3. Histamine - increases bronchoconstriction 4. Angiotensin-converting enzyme (ACE) - angiotensin I -> angiotensin II; inactivates bradykinin (ACE inhibitors increase bradykinin and cause cough, angioedema) 5. Kallikrein - activates bradykinin |
|
|
Equation for Collapsing pressure in alveoli?
|
Collapsing Pressure = P = 2(surface tension) / radius
Tendency to collapse on expiration increases as radius decreases (law of Laplace) |
|
|
Lung volumes - Residual volume (RV)
|
air in lung after maximal expiration; cannot be measured on spirometry
|
|
|
Lung volumes - Expiratory reserve volume (ERV)
|
air that can still be breathed out after normal expiration
|
|
|
Lung volumes - Tidal volume (TV)
|
air that moves into lungs with each quiet inspiration, typically 500 mL
|
|
|
Lung volumes - Inspiratory reserve volume (IRV)
|
air in excess of tidal volume that moves into lung on maximum inspiration
|
|
|
Lung volumes - vital capacity (VC)
|
everything but the residual volume
VC = TV + IRV + ERV |
|
|
Lung volumes - Functional residual capacity (FRC)
|
RV + ERV (volume in lungs after normal expiration)
|
|
|
Lung volumes - Inspiratory capacity (IC)
|
IRV + TV
|
|
|
Lung volumes - Total lung capacity (TLC)
|
IRV + TV + ERV + RV
|
|
|
Physiologic dead space
|
Vd = Vt x (PaCO2 - PeCO2) / PaCO2
Vd = physiologic dead space = anatomical dead space of conducting airways plus functional dead space in alveoli; apex of healthy lung is largest contributor of functional dead space. Volume of inspired air that does not take part in gas exchange. |
|
|
Lung and Chest Wall - compliance curves
|
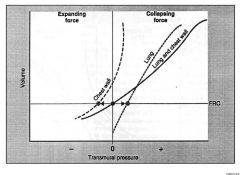
There is a tendency for the lungs to collapse inward and chest wall to spring outward.
At FRC, inward pull of lung is balanced by outward pull of chest wall, and system pressure is atmospheric. Elastic properties of both chest wall and lungs determine their combined volume. At FRC, airway and alveolar pressure are 0, and intrapleural pressure is negative (prevents pneumothorax). Compliance - change in lung volume for a given change in pressure; decreased in pulmonary fibrosis, insufficient surfactant, and pulmonary edema |
|
|
Hemoglobin molecule - details?
|
Composed of 4 polypeptide subunits (2 alpha and 2 beta) and exists in 2 forms:
1. T (taut) form has low affinity for O2 2. R (relaxed) form has high affinity for O2 (300x). Hemoglobin exhibits positive cooperativity and negative allostery (accounts for the sigmoid-shaped O2 dissociation curve for hemoglobin), unlike myoglobin. Increased Cl-, H+, CO2, 2,3-BPG, and temperature favor T form over R form (shifts dissociation curve to right, leading to increased O2 unloading). |
|
|
What is different about fetal hemoglobin characteristics that make its O2 binding affinity different from adult hemoglobin?
|
2 alpha and 2 gamma subunits, has lower affinity for 2,3-BPG than adult hemoglobin (HgA) and thus has higher affinity for O2.
|
|
|
Methemoglobin - details?
|
Methemoglobin is the oxidized form of hemoglobin (ferric, Fe3+) that does not bind O2 as readily, but has increased affinity for CN-.
Iron in hemoglobin is normally in a reduced state (ferrous, Fe2+). To treat cyanide poisoning, use nitrites to oxidize hemoglobin to methemoglobin, which binds cyanide, allowing cytochrome oxidase to function. Use thiosulfate to bind this cyanide forming thiocyanate, which is renally excreted. |
|
|
How to treat cyanide poisoning?
|
Methemoglobin binds to CN- readily, so convert hemoglobin to methemoglobin by administering Nitrites. This allows cytochrome oxidase to function in peripheral tissue cells. Then use thiosulfate to bind this cyanide to form thiocyanate which is renally excreted.
|
|
|
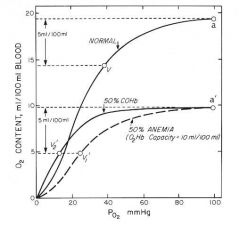
Carboxyhemoglobin - details?
|
Form of hemoglobin bound to CO in place of O2. Causes decreased oxygen-binding capacity with left shift in the oxygen-hemoglobin dissociation curve. Decreased oxygen unloading in tissues.
CO has 200x greater affinity than O2 for hemoglobin. |
|
|
Oxygen-hemoglobin dissociation curve - details?
|
Sigmoidal shape due to positive cooperativity, i.e., hemoglobin can bind 4 oxygen molecules and has higher affinity for each subsequent oxygen molecule bound. Myoglobin does not show positive cooperativity; curve lacks sigmoidal appearance.
When curve shifts to the right, decreased affinity of hemoglobin for O2 (facilitates unloading of O2 to tissue). An increase in all factors (except pH) causes a shift of the curve to the right, and vice-versa. Fetal Hb has a higher affinity for oxygen than adult Hb, so its dissociation curve is shifted left. Hb saturation increases at any given PO2 in the presence of CO due to positive cooperativity. |
|
|
Pulmonary Circulation - details?
|
Normally a low-resistance, high-compliance system. PO2 and PCO2 exert opposite effects on pulmonary and systemic circulation. A decrease in PAO2 causes a hypoxic vasoconstriction that shifts blood away from poorly ventilated regions of lung to well-ventilated regions of lung.
|
|
|
Pulmonary circulation - perfusion limited substances
|
Perfusion limited - O2 (normal health), CO2, N2O. Gas equilibrates early along the length of the capillary. Diffusion can be increased only if blood flow increases. (See First Aid for graphs, p. 564)
|
|
|
Pulmonary circulation - diffusion limited substances
|
O2 (emphysema, fibrosis), CO. Gas does not equilibrate by the time blood reaches the end of the capillary. (See First Aid for graphs, p. 564)
|
|
|
Pulmonary circulation - Diffusion equation
|
Vgas = A/T x Dk(P1 - P2)
where A = Area, T = thickness, and Dk(P1-P2) = difference in partial pressures. A decreases in emphysema. T increases in pulmonary fibrosis. |
|
|
Pulmonary hypertension - details?
|
Normal pulmonary artery pressure = 10-14 mmHg; pulmonary hypertension >/= 25 mmHg or >35 mmHg during exercise.
Results in atherosclerosis, medial hypertrophy, and intimal fibrosis of pulmonary arteries. Course: severe respiratory distress --> cyanosis and RVH --> death from decompensated cor pulmonale |
|
|
Pulmonary hypertension - Primary
|
Due to an inactivating mutation in the BMPR2 gene (normally functions to inhibit vascular smooth muscle proliferation); poor prognosis.
|
|
|
What gene is altered in primary pulmonary hypertension?
|
BMPR2 is inactivated (normally functions to inhibit vascular smooth muscle proliferation)
|
|
|
Pulmonary Hypertension - Secondary
|
Due to COPD (destruction of lung perenchyma); mitral stenosis (increased resistance --> increased pressure); recurrent thromboemboli (decreased cross-sectional area of pulmonary vascular vascular bed); autoimmune disease (e.g., systemic sclerosis; inflammation --> intimal fibrosis --> medial hypertrophy); left-to-right shunt (increased shear stress --> endothelial injury); sleep apnea or living at high altitude (hypoxic vasoconstriction)
|
|
|
Name 6 diseases associated with development of pulmonary hypertension.
|
1. COPD (destruction of lung perenchyma)
2. Mitral Stenosis (increased resistance --> increased pressure) 3. Recurrent thromboemboli (decreased cross-sectional area of pulmonary vascular bed) 4. Autoimmune disease (e.g., systemic sclerosis; inflammation --> intimal fibrosis --> medial hypertrophy) 5. left-to-right shunt (increased shear stress --> endothelial injury) 6. sleep apnea or living at high altitude (hypoxic vasoconstriction) |
|
|
Equation for Pulmonary Vascular Resistance
|
PVR = [P (pulm artery) - P (L atrium)] / Cardiac Output
P (pulm artery) = pressure in pulmonary artery P (L atrium) = Pulmonary capillary wedge pressure |
|
|
Oxygen content of blood
|
O2 content = (O2 binding capacity x % saturation) + dissolved O2
Normally 1 g Hb can bind 1.34 mL O2; normal Hb amount in blood is 15 g/dL. Cyanosis results when deoxygenated Hb > 5 g/dL. O2 binding capacity = 20.1 mL O2/dL O2 content in arterial blood decreases as Hb falls, but O2 saturation and arterial PO2 do not. Arterial PO2 decreases with chronic lung disease because physiologic shunt decreases O2 extraction ratio. Exercise decreases venous PO2. Oxygen delivery to tissues = cardiac output x oxygen content of blood |
|
|
Alveolar gas equation
|
PAO2 = PIO2 - PaCO2/R
Can normally be approximated as: PAO2 = 150 - PaCO2/0.8 PAO2 = alveolar PO2 (mmHg) PIO2 = PO2 in inspired air (mmHg) PaCO2 = arteriolar PCO2 (mmHg) R = respiratory quotient = CO2 produced/O2 consumed A-a gradient = PAO2 - PaO2 = 10-15 mmHg Increased A-a gradient may occur in hypoxemia; causes include shunting, V/Q mismatch, fibrosis (impairs diffusion) |
|
|
Oxygen deprivation - Hypoxemia with a normal A-a gradient
|
High altitude, Hypoventilation
|
|
|
Oxygen deprivation - Hypoxemia with increased A-a gradient
|
V/Q mismatch, Diffusion limitation, Right-to-left shunt
|
|
|
V/Q mismatch - details?
|
Ideally, ventilation is matched to perfusion (V/Q = 1) in order for adequate gas exchange to occur.
Lung zones: 1. Apex of the lung - V/Q = 3 (wasted ventilation) 2. Base of the lung - V/Q = 0.6 (wasted perfusion) Both ventilation and perfusion are greater at the base of the lung than at the apex of the lung. With exercise (increased Cardiac Output), there is vasodilation of apical capillaries, resulting in V/Q ratio that approaches 1. Certain organisms that thrive in high O2 (e.g. TB) flourish in the apex. V/Q --> 0 = airway obstruction (shunt). In shunt, 100% O2 does not improve PO2. V/Q --> infinity = blood flow obstruction (physiologic dead space). Assuming <100% dead space, 100% O2 improves PO2. |
|
|
Explain the V/Q mismatch in the apices and base of the lung.
|
Gravity makes blood pressure/flow low in the apices.
PA > Pa > Pv Gravity pools blood in the bases, pushes air out. Pa > Pv > PA In the middle lobes, there is balance and the artery pressure is high enough to push spurts of blood during the cardiac cycle, while the venous pressure is low enough to allow the alveoli to be ventilated adequately. Pa > PA > Pv |
|
|
CO2 transport - 3 forms in blood
|
1. Bicarbonate (90%)
2. Bound to globin as carbaminohemoglobin (5%) 3. Dissolved CO2 (5%) |
|
|
CO2 transport - details?
|
Carbon dioxide is transported from tissues to the lungs in 3 forms:
1. Bicarbonate (90%) 2. Bound to hemoglobin at N terminus of globin (not heme) as carbaminohemoglobin (5%). CO2 binding favors taut form (O2 unloaded). 3. Dissolved CO2 (5%) In lungs, oxygenation of Hb promotes dissociation of H+ from Hb. This shifts equilibrium toward CO2 formation; therefore CO2 is released from RBCs (Haldane effect). In peripheral tissues, increased H+ from tissue metabolism shifts curve to right, unloading O2 (Bohr effect). Majority of blood CO2 is carried as bicarbonate in the plasma. |
|
|
Respiratory response to high altitude - details?
|
1. Acute increase in ventilation, decreased PO2 and PCO2
2. Chronic increase in ventilation 3. Increased erythropoietin --> increased hematocrit and hemoglobin (chronic hypoxia) 4. Increased 2,3-BPG (binds to hemoglobin so that hemoglobin releases more O2). 5. Cellular changes (Increased mitochondria) 6. Increased renal excretion of bicarbonate (e.g., can augment by use of acetazolamide) to compensate for the respiratory alkalosis 7. Chronic hypoxic pulmonary vasoconstriction results in RVH |
|
|
Respiratory response to exercise - details?
|
1. increased CO2 production
2. Increased O2 consumption 3. Increased ventilation rate to meet O2 demand 4. V/Q ratio from apex to base becomes more uniform 5. Increased pulmonary blood flow due to increased cardiac output 6. Decreased pH during strenuous exercise (secondary to alctic acidosis) 7. No change in PaO2 and PaCO2, but increase in venous CO2 content |
|
|
Oxygen deprivation - hypoxia examples
|
Decreased cardiac output, Hypoxemia, Anemia, Cyanide poisoning, CO poisoning
|
|
|
Oxygen deprivation - ischemia details
|
Impeded arterial flow, reduced venous drainage
|
|
|
Embolus types
|
Fat, Air, Thrombus, Bacteria, Amniotic Fluid, Tumor
Fat emboli are associated with long bone fractures and liposuction. Amniotic fluid emboli can lead to DIC, especially postpartum. Pulmonary embolus - Chest pain, tachypnea, dyspnea Approximately 95% of pulmonary emboli arise from deep leg veins. Helical CT is the imaging test of choice for PE. |
|
|
How to remember the types of embolism?
|
An embolus moves like a FAT BAT.
Fat Air Thrombus Bacterial Amniotic fluid Tumor |
|
|
Pulmonary thromboembolism - histology findings
|
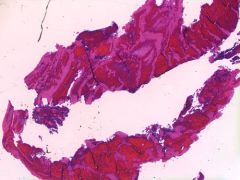
"Lines of Zahn" - interdigitating areas of pink and red in embolus, representing layers of RBCs, platelets, and fibrin laid down if thrombus formed before death
|
|
|
Deep venous thrombosis - details?
|
Can lead to pulmonary embolus.
Homan's sign - dorsiflexion of foot --> tender calf muscle Prevent and treat with heparin Predisposed by Virchow's triad: 1. Stasis 2. Hypercoagulability (e.g., defet in coagulative cascade proteins) 3. Endothelial damage (exposed collagen triggers clotting cascade) |
|
|
Obstructive Lung Disease (COPD)
|
Obstruction of air flow resulting in air trapping in the lungs. Airways close prematurely at high lung volumes, resulting in increased RV and decreased FVC.
PFTs: very decreased FEV1, decreased FVC --> decreased FEV1/FVC ratio (hallmark), V/Q mismatch |
|
|
Obstructive Lung Disease - Chronic Bronchitis
|
"Blue Bloater"
Hypertrophy of mucus-secreting glands int he bronchi --> in COPD, Reid index >50% (Reid index = gland depth/total thickness of bronchial wall) Productive cough for >3 months per year for > 2 years. Disease of small airway. Findings: wheezing, crackles, cyanosis (early-onset hypoxemia due to shunting), late-onset dyspnea |
|
|
Obstructive Lung Disease - Emphysema
|
"Pink puffer," barrel-shaped chest
Enlargement of air spaces and decreased recoil resulting from destruction of alveolar walls; increased compliance. Increased elastase activity, increased lung compliance due to loss of elastic fibers. Exhalation through pursed lips to increase airway pressure and prevent airway collapse during respiration. |
|
|
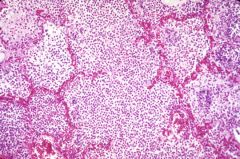
Emphysema - histology findings
|
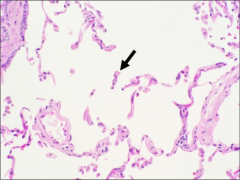
Enlarged alveoli are seen separated by thin septa, some of which appear to float in alveolar spaces.
|
|
|
Emphysema - gross pathology findings
|
Gross specimen shows multiple cavities linked by heavy black carbon deposits.
|
|
|
Obstructive lung disease - Asthma
|
Bronchial hyperresponsiveness causes reversible bronchoconstriction. Smooth muscle hypertrophy and Curschmann's spirals (shed epithelium forms mucous plugs).
Can be triggered by viral URIs, allergens and stress. Test with methacholine challenge. Findings: cough, wheezing, tachypnea, dyspnea, hypoxemia, decreased I/E ratio, pulsus paradoxus, mucus plugging |
|
|
What are Curschmann's spirals?
|
Seen with asthma. Represent shed epithelium from mucous plugs on histology of lung biopsy.
|
|
|
Obstructive Lung Disease - Bronchiectasis
|
Chronic necrotizing infection of bronchi --> permanently dilated airways, purulent sputum, recurrent infections, hemoptysis.
Associated with bronchial obstruction, poor ciliary motility (smoking), Kartagener's syndrome. Aspergillus is a possible risk factor. |
|
|
Describe pulsus paradoxus.
|
>10 mmHg drop in SBP measurement during maximal inspiration. Associated with asthma exacerbations.
|
|
|
Restrictive Lung Diseases - details and 2 major categories
|
Restricted lung expansion causes decreased lung volumes (decreased FVC and TLC). PFTs - FEV1/FVC ratio >80%
Types: 1. Poor breathing mechanics (extrapulmonary, peripheral hypoventilation) 2. Interstitial lung diseases (pulmonary, lowered diffusing capacity) |
|
|
Restrictive Lung Diseases - Poor breathing mechanics
|
Poor muscular effort - polio, myasthenia gravis
Poor structural apparatus - scoliosis, morbid obesity |
|
|
Restrictive Lung Diseases - Interstitial lung diseases
|
1. Acute respiratory distress syndrome (ARDS)
2. Neonatal respiratory distress syndrome (hyaline membrane disease) 3. Pneumoconioses (coal miner's, silicosis, asbestos) 4. Sarcoidosis: bilateral hilar lymphadenopathy, noncaseating granuloma, increased ACE and calcium 5. Idiopathic pulmonary fibrosis (repeated cycles of lung injury and wound healing with increased collagen deposition) 6. Goodpasture's syndrome 7. Wegener's granulomatosis 8. Eosinophilic granuloma (histiocytosis X) 9. Drug toxicity (bleomycin, busulfan, amiodarone) |
|
|
Pneumoconioses - Coal miner's
|
Associated with coal mines. Can result in cor pulmonale, Caplan's syndrome (rheumatoid arthritis involvement)
Affects upper lobes. |
|
|
What is Caplan's syndrome?
|
Rheumatoid arthritis associated with Coal Miner's Pneumoconiosis
|
|
|
Pneumoconioses - Silicosis
|

Associated with foundries, sandblasting, and mines.
Macrophages respond to silica and release fibrogenic factors, leading to fibrosis. It is thought that silica may disrupt phagolysosomes and impair macrophages, increasing susceptibility to TB. Affects upper lobes. "Eggshell" calcifications of hilar lymph nodes (see picture). |
|
|
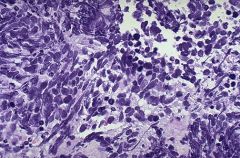
Pneumoconioses - Asbestosis
|

Associated with shipbuilding, roofing, and plumbing. Results in "ivory white," calcified pleural plaques. Associated with an increased incidence of bronchogenic carcinoma and mesothelioma.
Affects lower lobes. Asbestos bodies are golden-brown fusiform rods resmbling dumbbells, located inside macrophages (see picture). |
|
|
Which pneumoconioses affect upper lobes? Lower lobes?
|
Upper - Coal miner's, silicosis
Lower - Asbestosis |
|
|
Neonatal respiratory distress syndrome (Hyaline membrane disease)
|
Surfactant deficiency leading to increased surface tension, resulting in alveolar collapse. Surfactant is made by type II pneumocytes most abundantly after 35th week of gestation. The lecithin-to-sphingomyelin (L:S) ratio in the amniotic fluid, a measure of lung maturity, is usually < 1.5 in neonatal respiratory distress syndrome. Persistently low O2 tension --> risk of PDA. Therapeutic supplemental O2 can result in retinopathy of prematurity.
Surfactant - dipalmitoyl phosphatidylcholine Risk factors: prematurity, maternal diabetes (due to elevated insulin), cesarean delivery (decreased release of fetal glucocorticoids) Treatment: maternal steroids before birth; artificial surfactant for infant; thyroxine |
|
|
Supplemental O2 for treatment of neonatal RDS can result in what complication?
|
Retinopathy of Prematurity
|
|
|
Name 3 risk factors for neonatal RDS.
|
Prematurity
Maternal diabetes (due to elevated insulin) Cesarean delivery (dec. release of fetal glucocorticoids) |
|
|
Why is maternal diabetes associated with an increased risk of neonatal respiratory distress syndrome?
|
Elevated insulin
|
|
|
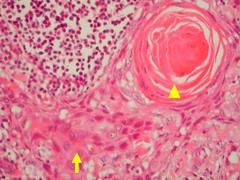
Acute Respiratory Distress Syndrome - Details?
|
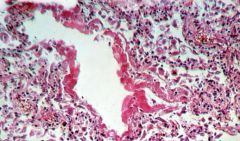
May be caused by trauma, sepsis, shock, gastric aspiration, uremia, acute pancreatitis, or amniotic fluid embolism.
Diffuse alveolar damage --> increased alveolar capillary permeability --> protein-rich leakage into alveoli. Results in formation of intra-alveolar hyaline membrane (see picture). Initial damage due to release of neutrophilic substances toxic to alveolar wall, activation of coagulation cascade, and oxygen-derived free radicals. |
|
|
Name 7 causes of ARDS
|
Trauma
Sepsis Shock Gastric aspiration Uremia Acute Pancreatitis Amniotic fluid embolism |
|
|
Obstructive vs. Restrictive Lung disease
|
Normal - FEV1/FVC = 80%
Obstructive - FEV1/FVC < 80% Restrictive - decreased TLC Obstructive lung volumes > normal (Increased TLC, FRC, RV); restrictive lung volumes < normal. In both obstructive and restrictive FEV1 and FVC are reduced, but in obstructive, FEV1 is more dramatically reduced, resulting in a decreased FEV1/FVC ratio. (see First Aid p 570 for graphs) |
|
|
Sleep Apnea
|
Person stops breathing for at least 10 seconds repeatedly during sleep.
Central sleep apnea - no respiratory effort Obstructive sleep apnea - respiratory effort against airway obstruction Associated with obesity, loud snoring, systemic/pulmonary hypertension, arrhythmias, and possibly sudden death. Individuals may become chronically tired. Treatment: weight loss, CPAP, surgery Hypoxia --> increased EPO release --> increased erythrocytosis |
|
|
Lung-physical findings - Bronchial obstruction
|
Absent or decreased breath sounds over affected area.
Decreased resonance. Decreased fremitus. Tracheal deviation toward the side of lesion. |
|
|
Lung-physical findings - Pleural effusion
|
Decreased breath sounds over effusion.
Hyporesonance. Decreased fremitus. No tracheal deviation. |
|
|
Lung-physical findings - Pneumonia (lobar)
|
May have bronchial breath sounds over lesion.
Hyporesonance. Increased fremitus. No tracheal deviation. |
|
|
Lung-physical findings - Tension pneumothorax
|
Decreased breath sounds.
Hyperresonant. Absent fremitus. Tracheal deviation away from side of lesion. |
|
|
Lung-physical findings - Spontaneous pneumothorax
|
Decreased breath sounds.
Hyperresonant. Decreased fremitus. Tracheal deviation toward the side of the lesion. |
|
|
Lung cancer - basics?
|
Lung cancer is the leading cause of cancer death.
Presentation: cough, hemoptysis, bronchial obstruction, wheezing, pneumonic "coin" lesion on x-ray film or noncalcified nodule on CT Metastases to lung are most common, often from breast, colon, prostate, and bladder cancer. Sites of metastases - adrenals, brain (epilepsy), bone (pathalogic fracture), liver (jaundice, hepatomegaly) |
|
|
How to remember complications of lung cancer?
|
SPHERE of complications
Superior vena cava syndrome Pancoast tumor Horner's syndrome Endocrine (paraneoplastic) Recurrent laryngeal symptoms (hoarseness) Effusions (pleural or pericardial) |
|
|
Lung cancer - Small cell (oat cell) carcinoma
|
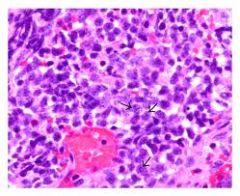
Location: central
Characteristics: Undifferentiated --> very aggressive; often associated with ectopic production of ACTH or ADH; may lead to Lambert-Eaton syndrome (autoantibodies against calcium channels). Responsive to chemotherapy. Inoperable. Histology: Neoplasm of neuroendocrine Kulchitsky cells --> small dark blue cells. "Salt and pepper" neuroendocrine-type chromatin (see picture). |
|
|
What are Kulchitsky cells?
|
Small dark blue cells of neuroendocrine origin associated with Small cell carcinoma of the lung
|
|
|
Lung cancer - Adenocarcinoma (Bronchial type)
|
Location: Peripheral
CHaracteristics: Develops in site of prior pulmonary inflammation or injury (most common lung cancer in nonsmokers and females). Both bronchial and bronchioalveolar have Clara cells --> type II pneumocytes; multiple densities on x-ray of chest |
|
|
Lung cancer - Adenocarcinoma (Bronchioalveolar type)
|
Location: peripheral
Characteristics: Not linked to smoking; grows along airways; can present like pneumonia. Can result in hypertrophic osteoarthropathy. Both bronchial and bronchioalveolar types: Clara cells --> type II pneumocytes; multiple densities on x-ray of chest |
|
|
Lung cancer - Squamous cell carcinoma
|
Location: Central
Characteristics: Hilar mass arising from bronchus; Cavitation; Clearly linked with smoking; parathyroid-like activity (PTHrP) Histology: keratin pearls and intercellular bridges |
|
|
Lung cancer - Large cell carcinoma
|
Location: peripheral
Characteristics: Highly anaplastic undifferentiated tumor; poor prognosis; less responsive to chemotherapy. Removed surgically. Histology: pleomorphic giant cells with leukocyte fragments in cytoplasm (Giant Cells - think Large Cell Carcinoma) |
|
|
Lung cancer - Carcinoid tumor
|
Characteristics:
Secretes serotonin, can cause carcinoid syndrome (flushing, diarrhea, wheezing, salivation). Fibrous deposits in right heart valves may lead to tricuspid insufficiency, pulmonary stenosis, and right heart failure. |
|
|
Lung cancer - Mesothelioma
|
Location: pleural
Characteristics: Malignancy of the pleura associated with asbestosis. Results in hemorrhagic pleural effusions and pleural thickening. Histology: Psammoma bodies |
|
|
Small cell carcinoma of the lung - histology findings
|
Sheets of tumor cells with nuclear modling, highmitotic rate, necrosis, and "salt-and-pepper" neuroendocrine-type chromatin.
|
|
|
Squamous cell carcinoma of the lung - histology findings
|
Sheets of large squamous cells with dysplasia and keratin "pearls"
|
|
|
Pancoast tumor
|
Carcinoma that occurs in apex of lung and may affect cervical sympathetic plexus, causing Horner's syndrome.
|
|
|
Horner's syndrome - classic triad
|
Ptosis, miosis, anhidrosis
|
|
|
Superior vena cava syndrome
|
An obstruction of the SVC that impairs blood drainage from the head ("facial plethora"), neck (jugular venous distension), and upper extremities (edema). Most commonly caused by neoplasms and thromboses. Can raise intracranial pressure (if obstruction is severe), which presents as headaches and dizziness and can increase the risk of aneurysm/rupture of cranial arteries.
|
|
|
Pneumonia - Lobar - Organisms? Characteristics?
|

Pneumococcus most frequently, Klebsiella
Intra-alveolar exudate --> consolidation; may involve entire lung. |
|
|
Pneumonia - Bronchopneumonia - organisms? characteristics?
|
S. aureus, H. flu, Klebsiella, S. pneumoniae
Acute inflammatory infiltrates from bronchioles into adjacent alveoli; patchy distribution involving >/= 1 lobes. |
|
|
Pneumonia - Interstitial (atypical) pneumonia - organisms? characteristics?
|
Viruses (RSV, adenoviruses), Mycoplasma, Legionella, Chlamydia
Diffuse patchy inflammation localized to interstitial areas at alveolar walls; distribution involving >/= 1 lobes. Generally follows a more indolent course than bronchopneumonia. |
|
|
Bronchopneumonia - histology findings
|
Neutrophils in alveolar spaces.
|
|
|
Bronchopneumonia - gross pathology findings
|
Large area of consolidation
|
|
|
Lung abscess
|
Localized collection of pus within perenchyma. Caused by: bronchial obstruction (e.g., cancer); aspiration of oropharyngeal contents (especially in patients predisposed to loss of consciousness, e.g., alcoholics or epileptics)
Air-fluid levels often seen on CXR. Often due to S. aureus or anaerobes (Bacteroides, Fusobacterium, Peptostreptococcus) |
|
|
Hypersensitivity Pneumonitis
|
Mixed type III/IV hypersensitivity reaction to environmental antigen --> dyspnea, cough, chest tightness, headache. Often seen in farmers and those exposed to birds.
|
|
|
What are two risk factors for developing Hypersensitivity Pneumonitis?
|
Farmers and being exposed to birds
|
|
|
Pleural Effusions - 3 types and details of each
|
Transudate - decreased protein content. Due to CHF, nephrotic syndrome, or hepatic cirrhosis.
Exudate - Increased protein content, cloudy. Due to malignancy, pneumonia, collagen vascular disease, trauma (occurs in states of increased vascular permeability). Must be drained in light of risk of infection. Lymphatic - also known as chylothorax. Milky-appearing fluid; increased triglycerides |
|
|
Pneumothorax - Signs and Symptoms?
|
Unilateral chest pain and dyspnea, uilateral chest expansion, decreased tactile fremitus, hyperresonance, diminished breath sounds
|
|
|
Spontaneous pneumothorax
|
Accumulation of air in the pleural space. Occurs most frequently in tall, thin, young males because of rupture of apical blebs. Trachea deviates toward affected lung.
|
|
|
Tension pneumothorax
|
Usually occurs in setting of trauma or lung infection. Air is capable of entering pleural space but not exiting. Trachea deviates away from affected lung.
|
|
|
H1 blockers - details
|
Reversible inhibitors of H1 histamine receptors.
|
|
|
H1 blockers - 1st generation - Examples? clinical uses? toxicity?
|
Diphenhydramine, dimenhydrinate, chlorpheniramine
Clinical uses: allergy, motion sickness, sleep aid Toxicity: Sedation, antimuscarinic, anti-alpha-adrenergic Names usually contain "-en/-ine" or "-en/-ate" |
|
|
H1 blockers - 2nd generation - Examples? Clinical uses? Toxicity?
|
Loratidine, fexofenadine, desloratadine, cetirizine
Clinical uses: Allergy Toxicity: Far less sedating than 1st generation because of decreased entry into CNS. Names usually end in "-adine" |
|
|
Asthma drugs - details
|
Bronchoconstriction is mediated by (1) inflammatory processes and (2) parasympathetic tone; therapy is directed at these two pathways.
|
|
|
Asthma drugs - nonspecific Beta-agonist
|
Isoproterenol - relaxes bronchial smooth muscle (Beta-2). Adverse effect is tachycardia (Beta-1).
|
|
|
Asthma drugs - Beta-2 agonists
|
Albuterol - relaxes bronchial smooth muscle (Beta-2). Use during acute exacerbation.
Salmeterol - long-acting agent for prophylaxis. Adverse effects are tremor and arrhythmia. |
|
|
Asthma drugs - methylxanthines
|
Theophylline - likely causes bronchodilation by inhibiting phosphodiesterase, thereby decreasing cAMP hydrolysis. Usage is limited because of narrow therapeutic index (cardiotoxicity, neurotoxicity); metabolized by P-450. Blocks actions of adenosine.
|
|
|
Asthma drugs - Muscarinic antagonists
|
Ipratropium - competitive blocker of muscarinic receptors, preventing bronchoconstriction. Also used for COPD.
|
|
|
Asthma drugs - Cromolyn
|
Prevents release of mediators from mast cells. Effective only for the prophylaxis against asthma. Not effective during an acute asthmatic attack. Toxicity is rare.
|
|
|
Asthma drugs - Corticosteroids
|
Beclomethasone, prednisone - inhibit snthesis of virtually all cytokines. Inactivate NF-kappaB, the transcription factor that induces the production of TNF-alpha, among other inflammatory agents. 1st line therapy for chronic asthma.
|
|
|
Asthma drugs - antileukotrienes - Zileuton
|
A 5-lipoxygenase pathway inhibitor. Blocks conversion of arachidonic acid to leukotrienes.
|
|
|
Asthma drugs - antileukotrienes - Zafirlukast, montelukast
|
Block leukotriene receptors. Especially good for aspirin-induced asthma.
|
|
|
What drug is particularly good at treating aspirin-induced asthma?
|
Leukotriene receptor blockers (Montelukast, Zafirlukast)
|
|
|
Guaifenesin
|
Expectorant - removes excess sputum, does not suppress cough reflex
|
|
|
N-acetylcysteine
|
Mucolytic - can loosen mucous plugs in CF patients. Also used as an antidote for acetaminophen overdose.
|
|
|
Bosentan
|
Used to treat pulmonary hypertension. Competitively antagonizes endothelin-1 receptors, decreasing pulmonary vascular resistance.
|
|
|
Dextromethorphan
|
Antitussive (antagonizes NMDA glutamate receptors). Synthetic codeine analog. Has mild opioid effect when used in excess. Naloxone can be given for OD. Mild abuse potential.
|
|
|
How does dextromethorphan elicit its antitussive effects?
|
antagonizes NMDA glutamate receptors
|
|
|
Pseudoephedrine, phenylephrine - Mechanism? Clinical use? Toxicity?
|
Mechanism: sympathomimetic alpha-agonist nonprescription nasal decongestants
Clinical use: reduces hyperemia, edema, and nasal congestion; opens obstructed Eustachian tubes. Pseudoephedrine also used as a stimulant. Toxicity: Hypertension. Can also cause CNS stimulation/anxiety (pseudoephedrine). |
|
|
Methacholine - mechanism? clinical use?
|
Mechanism: Muscarinic receptor agonist
Clinical use: Used in asthma challenge testing. |
|
|
Explain bronchial tone mediators
|
cAMP causes bronchodilation while ACh and Adenosine cause bronchoconstriction.
Beta-agonists increase Adenylate Cyclase activity, thus increasing cAMP and bronchodilation. Theophylline blocks phosphodiesterase which prevents hydrolysis of cAMP and promotes bronchodilation. Muscarinic antagonists block acetylcholine's bronchoconstrictive effect. Theophylline also blocks adenosine's bronchoconstrictive effect directly. |
|
|
How long does it take for hemoglobin levels to elevate to the point where blood oxygen content is near normal after moving to a high altitude environment (>4000 meters above sea level).
|
EPO begins being secreted after several hours but it takes 10-14 days for hemoglobin concentrations and blood oxygen content to have adjusted adequately.
Therefore, blood PaO2 will be low (~60 mmHg) for many days following the move. |
|
|
Chronic rejection after lung transplant affects what anatomical region of the lung?
|
Small airways (small bronchioles) - termed "bronchiolitis obliterans"
|
|
|
In a patient with suspicion of CF but a normal sweat test, what other test should be performed?
|
Nasal transepithelial potential difference - measures the charge on the respiratory epithelial surface as compared to the interstitial fluid
CF patients have a significantly more negative nasoepithelial surface than normal due to increased luminal sodium absorption |
|
|
Why do CF patients have increased sodium absorption in ductal epithelial cells?
|
CFTR has a tonic inhibitory effect on the opining of apical sodium channels (which absorb sodium into the cell) - if CFTR is nonfunctioning, sodium absorption goes on unchecked
|
|
|
Explain the "Chloride shift"
|
RBCs have a higher chloride content in the venous circulation than the arterial circulation (systemically) because chloride shifts into the RBCs to maintain electrical neutrality, given the excretion of HCO3- ions out of the cells
|
|
|
What finding points you away from left heart failure and towards ARDS, most notably?
|
Normal PCWP in ARDS.
|
|
|
Which leukotriene stimulates neutrophil chemotaxis?
|
Leukotriene B4
|
|
|
Panacinar emphysema occurs in patients with what risk factor, most commonly?
|
alpha1-antitrypsin deficiency
|
|
|
The process by which centriacinar emphysema develops is mediated by many proteases and oxidant molecules. Which molecule plays a particularly central role, and what cell secretes it?
|
Elastase, neutrophils
|
|
|
How are particles of different sizes cleared from the respiratory tract?
|
10-15 um - trapped in upper respiratory tract
2.5 - 10 um - enter the trachea and bronchi and are cleared by mucociliary transport < 2um - reach terminal bronchioli and alveoli and are phagocytized by macrophages |
|
|
what epithelial cell type covers the true vocal cords?
|
stratified squamous epithelium
|
|
|
What epithelial cell type covers the paranasal sinuses, laryngeal vestibule, false vocal cords, and tracheal bifurcation?
|
ciliated, pseudostratified, columnar, mucus-secreting epithelium
|
|
|
what is Potter syndrome?
|
congenital condition marked by pulmonary hypoplasia, limb deformities and characteristic facies (suborbital creases, a depressed nasal tip, low-set ears, and retrognathia) as a result of oligohydramnios from bilateral renal agenesis
|
|
|
why do patients with restrictive lung disease typically have relatively high expiratory flow rates?
|
increased elastic recoil pressure and increased radial traction on the conducting airways by the fibrotic pulmonary interstitium leads to less conducting airway resistance
|
|
|
what is the most common mutation in CF patients?
|
Delta508 - deletes the three nucleotides that code for phenylalanine at amino acid position 508 (70% of cases)
this causes abnormal protein folding and failure of glycosylation - the CFTR protein is degraded before it reaches the cell surface, causing its complete absence fromt he apical membrane of exocrine ductal epithelial cells |
|
|
what marker of mast cell activation is elevated in an anaphylactic reaction (besides Histamine)
|
tryptase
|
|
|
what mechanism triggers vasoactive substance release by mast cells?
|
IgE-Fc receptor aggregation on mast cell surface -> produces various intracellular cascades that ultimately cause mast cell degranulation
|
|
|
how does suppurative destruction of lung parenchyma within an abscess cavity induced?
|
lysosomal content release by macrophages
|
|
|
how does surfactant reduce the variation in distending pressure amongst spheres of varying sizes?
|
Surfactant decreases the surface tension as a sphere decreases in size. As the inside area of the sphere decreases, the surfactant becomes more concentrated and thus is able to decrease surface tension to a greater extent. Conversely, as a sphere grows larger, the surfactant molecules become more spread out and do not reduce the surface tension as much.
|
|
|
what molecule do both amphotericin B and nystatin bind to in fungal cell wall that allows them to create pores?
|
ergosterol - they will not work if ergosterol is not synthesized adequately by the fungal cells
|
|
|
what are the Echinocandins?
|
Caspofungin and Micafungin (antifungals) - inhibit glucan synthesis (a component of the fungal cell wall)
|
|
|
Name three mechanisms for the development of lung abscesses.
|
1. aspiration of oropharyngeal contents (most commoN) - Fusobacterium, Peptostreptococcus, and bacteroides species are usually found
2. Complication of bacterial pneumonia - immunosuppressed, old age and underlying chronic diseases - usually nosocomial and caused by S. aureus, E. coli, K. pneumoniae, or S. pneumoniae type 3 3. Hematogenous spread - in sepsis or infective endocarditis, usually multiple abscesses are found - staphylococcus and streptococcus are most common (may also be e. coli and fungi) |
|
|
what are the four stages of a lobar pneumonia?
|
Congestion (first 24 hours) - grossly red, heavy and boggy; microscopically vascular dilation, alveolar exudate containing mostly bacteria
Red hepatization (days 2-3) - grossly red, firm lobe (liver-like consistency) - alveolar exudate contains erythrocytes, neutrophils and fibrin Gray hepatization (days 4-6) - gray-brown firm lobe - RBCs disintegrate, alveolar exudate contains neutrophils and fibrin Resolution - restoration of normal architecture - enzymatic digestion of the exudate |
|
|
how does amphoterocin B cause most of its side effects
|
has some activity against human cell cholesterol molecules
|
|
|
main toxicities of Amphotericin B
|
1. acute infusion related reactions
2. dose-dependent nephrotoxicity 3. Electrolyte abnormalities (hypomagnesemia and hypokalemia) 4. Anemia 5. Thrombophlebitis at site of injection may occur |
|
|
How does N-acetylcysteine induce its mucolytic effects?
|
Reducing intermolecular disulfide bridges within mucus glycoproteins
|
|
|
explain the mechanism of panacinar emphysema development in alpha1-antitrypsin deficiency
|
Unopposed action of neutrophil elastase on alveolar walls
|
|
|
explain two ways that smoking is thought to contribute to panacinar emphysema development in patients with alpha1-antitrypsin deficiency
|
Oxidant products of smoke (include free radicals) can inactivate endogenous alpha1-antitrypsin, producing a "functional" alpha1-antitrypsin deficiency.
Smoking also enhances elastase activity in macrophages and macrophage elastase (unlike neutrophil derived elastase) is not inhibited by alpha1-antitrypsin. |
|
|
vitamin D (calcitriol) is thought to be secreted in what respiratory conditions?
|
granulomatous disorders (sarcoidosis, tuberculosis, Hodgkin's disease, non hodgkin's lymphoma)
|
|
|
if you are given a PaO2 and a PaCO2, how can you calculate the A-a gradient?
|
alveolar gas equation
PAO2 = 150 - PaCO2 / 0.8 A-a gradient = PAO2 - PaO2 |
|
|
streptomycin inhibits what step of protein translation?
|
Aminoglycosides inhibit the INITIATION step
|
|
|
recurrent respiratory infections with pseudomonas, chronic diarrhea and weight loss with the death of a 9-year-old sibling due to respiratory infection suggest what disease?
|
Cystic Fibrosis
|
|
|
what enzyme can be replaced in CF patients to help with chronic diarrhea and weight loss?
|
pancreatic lipase
|
|
|
reduced pulmonary parenchymal compliance is the hallmark of what disease?
|
pulmonary fibrosis
|
|
|
In the Reid index, what layer of the bronchial wall is not included in the measurement?
|
the outer cartilage layer is excluded
|
|
|
if a question mentions long, branched lipids within some bacterial cells, it is most likely referring to what?
|
mycolic acid in M. tuberculosis
|
|
|
why do patients with CF develop squamous metaplasia of exocrine ducts in the pancreas?
|
Vitamin A deficiency from long-standing pancreatic insufficiency
Vitamin A and its metabolite, Retinoic acid, are required to maintain orderly differentiation of specialized epithelia, including mucus-secreting columnar epithelium. When a deficiency state exists, the epithelium undergoes squamous metaplasia to a keratinizing epithelium. |
|
|
What is Bosentan used for?
|
Given to patient's with pulmonary hypertension while awaiting lung transplantation.
It is an oral endothelin-receptor antagonist recently approved for treatment of pulmonary hypertension. Endothelin is a potent vasoconstrictor and stimulant of endothelial proliferation. |
|
|
What drug inhibits synthesis of the fungal cell wall?
|
Caspofungin (and other echinocandin antifungals such as micafungin)
Blocks glucan synthesis (glucan is a major polysaccharide component of the fungal cell wall.) |
|
|
How many days does it take for the kidneys to compensate for severe respiratory acid-base disturbances?
|
3-5 days
|
|
|
A white newborn develops bilious vomiting and laparotomy reveals an inspissated green fecal mass obstructing the small bowel lumen.
What disease does the baby have? |
Cystic Fibrosis leading to a meconium ileus
|
|
|
what is the major enzyme that is released by eosinophils in atopic asthma?
|
Major Basic Protein
|
|
|
in a chronic smoker, metaplasia from what cell type to what cell type occurs in the bronchi?
|
From ciliated pseudostratified epithelium to stratified squamous epithelium
|
|
|
what is the most likely mechanism of tissue damage in patients with caseating granuloma from reactivation TB?
|
Delayed-type hypersensitivity (the mechanism by which granuloma is formed) - this leads to collateral damage from inflammation
|
|
|
What is the most potent mediator of cerebral blood flow?
|
PaCO2 - direct, linear relationship
|
|
|
what gives sputum its green color in patients with lobar pneumonia?
|
Myeloperoxidase - a blue green, heme-based pigment molecule contained in azurophilic granules of neutrophils that catalyzes the production of hypochlorous acid (HOCl) from chloride and hydrogen perxoide during the phagocytic respiratory burst
|
|
|
why is blood in the left atrium slightly less oxygenated than blood in the pulmonary capillaries?
|
Bronchial blood is mixed in which is deoxygenated - bronchioles are supplied from branches off the descending aorta and much of this blood flow then returns to the heart via the pulmonary arteries
|
|
|
what two gene mutations lead to TB resistance to Isoniazid in the setting of monotherapy administered to a patient with active TB?
|
Decreased expression of catalase-peroxidase enzyme that is required for isoniazid activation once the drug enters the bacterial cell.
Modification of the protein target binding site for Isoniazid |
|
|
What is the most common cause of death in patients with Asbestos exposure?
|
Lung Cancer - specifically bronchogenic carcinoma
NOT MESOTHELIOMA - that is the second most common cause of death |
|
|
what type of NMJ blocker is succinylcholine?
|
depolarizing - action is more rapid than with most non-depolarizing NMJ blockers (such as rocuronium)
|
|
|
What is train-of-four stimulation? Explain what it looks like in a patient on succinylcholine.
|
used to assess the degree of muscle relaxation induced by NMJ-blocking agents
Depolarizing blockers show sustained and equal reduction of all 4 twitches during phase 1 blockade. Continued administration of succinylcholine results in eventual transition to phase II blockage. Twitch response during this phase mimics those seen in nondepolarizing NMJ bloackade and show a fading pattern with progressive reduction in each of the 4 responses. |
|
|
Ethambutol works by what mechanism?
|
Inhibits arabinosyl transferase, an enzyme that polymerizes arabinose into arabinan and then arabinogalactan (a constituent of the mycobacterial cell wall). This carbohydrate polymerization is necessary for mycobacterial cell wall synthesis.
|
|
|
Superior vena cava syndrome is most commonly caused by what?
|
Bronchogenic carcinoma is most common, but any mediastinal mass can cause it
|
|
|
what finding on a biopsy of a lung coin lesion would suggest hamartoma?
|
Cartilage tissue - hamartoma (a.k.a. pulmonary chondroma) is the most common benign lung tumor.
Hamartoma is an excessive growth of a tissue type native to the organ of involvement. Lung hamartomas often contain islands of mature hyaline cartialge, fat, smooth muscle and clefts lined by respiratory epithelium. |
|
|
What separates silica from the other pneumoconioses in terms of x-ray findings and histology?
|
Eggshell calcification of hilar nodes on CXR and birefringent silica particles surrounded by fibrous tissue in the nodes themselves.
|
|
|
which lung cancer is inoperable in all cases?
|
small cell carcinoma
|
|
|
What lung disease can develop in patients with OSA?
|
Pulmonary Hypertension --> Cor Pulmonale
|
|
|
Fat embolism syndrome - describe
|
Triad of acute-onset neurologic abnormalities, hypoxemia, and a petechial rash in a patient with severe long bone and/or pelvic fractures.
Traumatic event dislodges fat globules from the bone marrow, allowing them to travel through the marrow vascular sinusoids and into the pulmonary microvessels. The release of free fatty acids from the fat globules causes local toxic injury to the endothelium (with the potential to cause ARDS.) Thrombocytopenia and petechiae that are associated with the fat embolism syndrome arise secondary to platelet adherence to and coating of the fat microglobules. |
|
|
What is the mechanism of action of Terbinafine?
|
Inhibition of squalene epoxidase inhibits synthesis of ergosterol of the fungal membrane.
|
|
|
Which TB drug works best in acidic environments and therefore works well against intracellular TB organisms?
|
Pyrazinamide
|
|
|
Why is minute ventilation different from alveolar ventilation?
|
Minute ventilation incorporates dead space while alveolar ventilation only accounts for air that is involved in gas exchange.
|
|
|
What two ways does COPD lead to obstructive flow-volume loop profile?
|
increased bronchial resistance (due to anatomic narrowing as in chronic bronchitis) and/or from decreased lung elasticity (e.g. due to destruction of interalveolar walls as in emphysema)
|
|
|
How can you distinguish Absolute versus relative erythrocytosis?
|
Need to check for increased total RBC mass - increased suggests absolute erythrocytosis, nromal suggests relative erythrocytosis - can check this with 51Cr-tagged RBC infusion test
|
|
|
What SaO2 is the cutoff for developing secondary polycythemia?
|
<92% (PaO2 < 65 mm Hg)
NOTE THAT THE SaO2 is a percentage - use the PaO2 |
|
|
How can you tell primary from secondary erythrocytosis?
|
EPO is low in primary (myeloproliferative disorders)
EPO is high in secondary (chronic hypoxia) |
|
|
How does Cromolyn work?
|
Prevents release of mediators from mast cells.
|
|
|
At what point on the spirometry graph showing all the various possible lung volumes, is the pulmonary vascular resistance the lowest?
|
Functional residual capacity (end of normal exhalation) - if you exhale more forcibly, although the alveoli are less expanded and exert less force on the vaculature, the chest wall and muscles is pushing down on the vessels from increased intrathoracic pressure - therefore the end expiratory volume of a normal breath is where pressure is the lowest
|
|
|
What are possible symptoms of locally invasive superior sulcus tumor in the lung?
|
1. Severe pain in the shoulder that radiates toward the axilla and scapula (most common). Can also have arm parasthesia, weakness, and muscle atrophy.
2. Horner's syndrome 3. Compression of the subclavian vessels may cause edema of the upper extremity 4. Extension of the tumor into the intervertebral foramina may lead to spinal cord compression and paraplegia. |
|
|
Why is it theorized that apical subpleural blebs form and lead to spontaneous pneumothorax in tall, thin young men?
|
It is thought that intrapleural pressure is more negative in the apical lung in this patient population.
|
|
|
Why is haptoglobin lower in patients with sickle cell anemia?
|
Haptoglobin is a free plasma protein that binds hemoglobin in order to prevent its renal excretion. haptoglobin levels are decreased in patients with hemolytic anemias because the half-life of the haptoglobin-hemoglobin complex is about 90 minutes (the complex is hepatically cleared); in contrast, free haptoglobin has a half-life of 5 days.
|
|
|
Increased HR and CO with preservation of PaO2 and PaCO2 is consistent with what integrated response?
|
Cardiorespiratory response to exercise
|
|
|
stab wound just superior to the clavicle and lateral to the manubrium could damage what structure?
|
lung pleura --> tension pneumothorax
|
|
|
Patient with normal PaO2, normal SaO2 and low oxygen content likely has what?
|
Anemia - low concentration of hemoglobin but saturation of hemoglobin molecules would remain unchanged, and PaO2 is independent of Hg concentration
|
|
|
What drug can improve postmenopausal osteoporosis and simultaneously reduce the chance of developing breast cancer?
|
Raloxifene, a selective-estrogen receptor modulator (SERM) - binds to estrogen receptors and exhibits tissue-specific behavior that can imitate or antagonize the effects of natural estrogen.
Raloxifene has estrogen agonist activity on bone leading to a decrease in net bone resorption. In the breast and uterus, however, raloxifene behaves as an estrogen antagonist. |
|
|
Describe breathing patterns in Cheyne-Stokes breathing.
|
Cyclic breathing in which apnea is followed by gradually increasing tidal volumes, and then gradually decreasing tidal volumes until the next apneic period. It is commonly seen in cardiac disease (e.g., advanced congestive heart failure) and neurologic disease (e.g., stroke, brain tumors, traumatic brain injury). It is frequently a poor prognostic sign in individuals with either neurological or cardiac disease.
|
|
|
What antibiotic is commonly used to treat lung abscess?
|
Clindamycin
|
|
|
What vessel has the highest oxygen content in a fetus besides the umbilical vein?
|
IVC (what it dumps into)
|
|
|
A patient with lung cancer, diplopia and erectile dysfunction likely has what?
|
Lambert-eaton syndrome - can have autonomic symptoms such as dry mouth or impotence
|
|
|
what areas of the lungs are most affected in panacinar emphysema 2/2 alpha1-antitrypsin deficiency? why?
|
lower lobes - they receive relatively greater perfusion, allowing greater rate of neutrophil infiltration
|
|
|
what is normal PO2 of inspired air, tracheal air, and alveolar air?
|
Inspired - 160 mm Hg
Tracheal - 150 mm Hg (due to humidification) Alveolar - 104 mm Hg (which is between tracheal air (150) and venous blood (40)) |
|
|
What is normal PCO2 of tracheal air, alveolar air, and venous blood?
|
Tracheal air - 0 mm Hg
Alveolar air - 40 mm Hg Venous blood - 46 mm Hg |
|
|
How are presbyopia and age-related skin wrinkles related?
|
They are both normal and age-related
|
|
|
What CF mutation is more common in Ashkenazi Jews?
|
mutation causing premature termination of the transmembrane protein, which leads to complete absence of membrane-bound CFTR protein
|
|
|
what are the only indications for Rifampin monotherapy?
|
prophylactic monotherapy for H. influenzae or N. meningitidis
|
|
|
What is the intrapleural pressure at the FRC?
|
-5 cm H2O -> during normal inspiration the inrapleural pressure drops to -7.5 which induces a slightly negative pressure in the alveoli that draws air into the lungs
|
|
|
What is coagulative necrosis?
|
Coagulative Necrosis: most common, characterized by relative preservation of cell outlines in the necrotic tissue. Most exogenous injuries, including a brown recluse spider bite, are associated with coagulative necrosis. Organ ischemia is the classic example. Cell cytoplasm becomes eosinophilic due to protein denaturation. The nucleus shrinks and there is chromatin clumping (pyknosis), fragmentation (karyorrhexis), and eventually lysis.
|
|
|
What is liquefactive necrosis?
|
usually occurs in the CNS, in sites of ischemic strokes. Necrotic cells undergo fragmentation and are phagocytized by macrophages with the formation of a cystic cavity.
|
|
|
What is fat necrosis?
|
Seen in acute pancreatitis. Pancreatic enzymes, including lipases, digest the perenchyma with formation of fatty acids. Saponification (soap formation) occurs when fatty acids combine with calcium.
|
|
|
What is caseous necrosis?
|
Occurs in tuberculosis. Necrotic tissue has a "cheesy" appearance and consists of fragmented cells and acellular material.
|
|
|
The methacholine challenge is used to rule out asthma by assessing for bronchial hyperreactivity (BHR). What is the definition for confirming BHR?
|
20% decline in FEV1 after inhalation of a bronchocontstrictive substance (e.g., methacholine).
|
|
|
What do the lamellar bodies of type II pneumocytes hold?
|
surfactant molecules
|
|
|
Explain how the optimum breathing rate goes up in conditions with increased elastic resistance in the lungs while the optimum breathing rate goes down in conditions with increased upper airway resistance.
|
In patients with increased elastic resistance, tidal volume needs to go down to minimize workload, as this is the main issue for these patients. Therefore, fast, shallow breaths are ideal.
In patients with upper airway obstruction (COPD, goiter, asthma), slow, deep breaths minimize work. |
|
|
Which portion of the bronchial tree has the highest airway resistance?
|
Medium and small-sized bronchi greater than 2 mm in diameter (the first 10 generations of bronchi) provide the greatest summated frictional resistance. In contrast, airways smaller than 2 mm in diameter normally produce less than 20% of the total airway frictional resistance because they have a much larger total cross-sectional area.
|
|
|
As epithelial cells transition as you go down the bronchial tree...which aspect of these cells is the last to stop being produced?
|
Cilia are the last thing and stop being produced just before the alveoli begin.
|
|
|
what TB-produced enzyme is necessary to activate Isoniazid molecules?
|
catalase-peroxidase (KatG)
|
|
|
If EM of a pleural biopsy shows numerous, long, slender microvilli and abundant tonofilaments, what are you seeing?
|
Mesothelioma (distinguish this from adenocarcinoma which has short, plump microvilli)
|
|
|
what cells are capable of dividing in response to alveolar injury?
|
Type II pneumocytes (NOT clara cells)
|
|
|
Why can oxygen supplementation be dangerous in patients with COPD?
|
If they are chronically hypoxemic (PaO2 < 60 mm Hg), oxygen becomes an important mediator of respiratory drive via its effects on the carotid body and aortic arch chemoreceptors.
If you give a patient supplemental oxygen who has been chronically hypoxemic, their medullary respiratory center may be inhibited and respiratory drive may decrease dramatically. |
|
|
In what clinical situation would it be most appropriate to perform a methacholine challenge test?
|
If a patient has normal spirometry values but a family history of allergic triad diseases. Can use methacholine challenge test as a good rule out (has good NPV).
|
|
|
why can an axillary lymph node dissection lead to an inability to abduct the arm above the horizontal?
|
long thoracic nerve injury leads to a denervation of the serratus anterior muscle...one of this muscles primary actions is to rotate the glenoid cavity superiorly in order to allow the humerus to be completely abducted
|
|
|
how does theophylline intoxication present?
|
abdominal pain, nausea, vomiting, cardiac arrhythmias and seizures
treat with gastric lavage, activated charcoal, and cathartics Treat cardiac tachyarrhytmias with beta blockers. Treat seizures with benzos and barbiturates. |
|
|
Explain the theorized mechanism for the development of hereditary pulmonary hypertension.
|
First insult is an autosomally dominant gene inheritence with variable penetrance. The gene is a Bone Morphogenic Protein receptor type 2 (BMPR2) gene mutation which predisposes the patient to pulmonary vascular disease.
The patient then receives a second insult such as a viral infection, ion channel defect, or drug side effect that activates the disease process, which is characterised by increased endothelin (vasoconstrictor), decreased prostacyclin (vasodilator and platelet inhibitor), and decreased nitric oxide (vasodilator). The result is vasoconstriction, vascular smooth muscle proliferation, fibrosis, thrombosis of pulmonary arteries and arterioles, endothelial growth factor, and elevated pulmonary pressures. |
|
|
What are the four categories of lung cancer? Describe the commonly tested clinical presentations (not respiratory pathology) that are associated with them.
|
1. small cell carcinoma - ACTH, lambert-eaton, and SIADH
2. squamous cell carcinoma - PTHrP 3. adenocarcinoma - clubbing, hypertrophic osteoarthropathy 4. large cell carcinoma - gynecomastia, galactorrhea |
|
|
what category of transmembrane ion channel is CFTR?
|
ATP-gated
|
|
|
What stain is used to look for fat in the lung perenchyma in fat embolism syndrome? What does it cause to change (color)?
|
osmium tetroxide is used, imparts a black color to fat
|
|
|
What is the first step in primary TB infection of a host?
|
Gravity-assisted migration to the smallest airways and phagocytization by macrophages. Mycobacterium organisms then replicate intracellularly due to the presence of the sulfatide virulence factor.
|
|
|
How long does it take for the Th1 cell activation to occur in primary TB infection?
|
2-4 weeks!
|
|
|
Treat acute RSV bronchiolitis in a child with what drug?
|
Ribavirin - best results in immunocompromised patients
|

