![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
55 Cards in this Set
- Front
- Back
- 3rd side (hint)
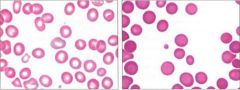
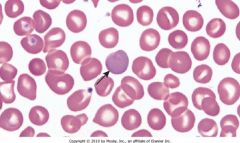
Name each RBC morphology |
Left: Reticulocylte (blue hue from mitochondria)
Right: Spherocyte |
|
|
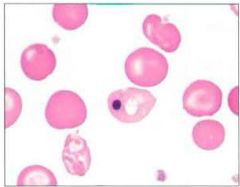
What is this and what can cause it? |
Howell-Jolly body
Basophilic nuclear reminants/framents in RBCs, which are normally removed by spleen.
Asplenic or hyposplenic patients can have these (e.g. splenectomy for sperocytosis) |
|
|
|
Coombs test and pneumonic |
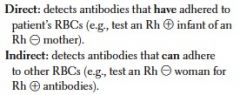
DBICM = Don't buy inexpensive combs for Mom |
|
|
|
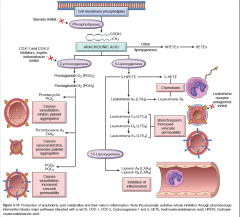
Inflammation and repair chart from Robbins |
|
|
|
|
Function of TXA2 |
Causes vasoconstriction, promotes platelet aggregation |
|
|
|
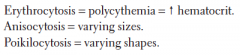
Define anisocytosis, erythrocytosis, poikilocytosis, polycythemia |
|
|
|
|
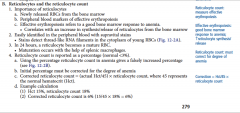
How do you calculate the reticulocyte index? |
|

|
|
|
Platelets, including receptors |

|
|
|
|
Leukocytes, including normal leukocyte percentages |

|
|
|
|
What compound activates macrophages and what is its CD marker? |

|
|
|
|
Eosinophil and causes of eosinophilia |

|
|
|
|
Basophil and causes of basophilia |

|
|
|
|
Mast cell |

|
|
|
|
Dendritic cell is called what in skin? |
Langerhans cell |
|
|
|
Explain how to prevent hemolytic disease of the newborn (erythrolastosis fetalis) |

|
|
|
|
Coagulation cascade components (procoagulation and antiticoagulation) |

|
|
|
|
Platelet plug formation and thrombogenesis |

|

|
|

|

|
G6PD = Hb precipitate |
|

|
|
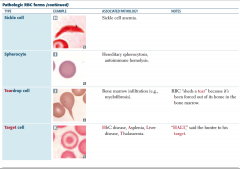
Teardrop cell = dacrocyte
Target cell = Intravascular hemolysis; dehydrated RBC causes it to bleb |
|

|

|
To see Heinz bodies, need Heinz prep
Asplenia: e.g. treatment for spherocytosis |
|
|
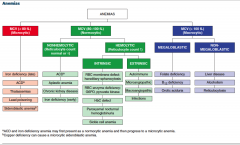
Anemia chart and signs and symptoms of anemia |
|
S/s: weakness, fatigue, dyspnea, pale conjunctiva and skin, headache, faintness, angina
<13.5 for men <12.5 for women
MCV = size of RBC |
|
|
Iron deficiency anemia |
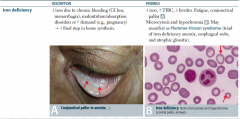
|
1/3 of World Population!
Iron absorbed in duodenum
Fe2+ absorbed more easily than Fe3+ (aside converts to Fe2+)
Increased FEP (free erythrocyte protoporphorin) associated with IDA (i.e. not found to anything)
Other causes: breast feeding; PUD; colon polyps; hookworm; colon carcinoma; celiac disease; gastrectomy
Findings include hypochromia and increased RDW |
|
|
Alpha-thalassemia |

|
decreased globin |
|
|
Beta-thalassemia |
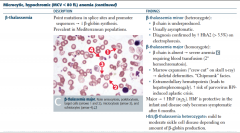
|
decreased globin |
|
|
Lead poisoning |

|
microcytic, hypochromic anemia |
|
|
Sideroblasic anemia |

|
Decreased protoporphorin
Alcohol damages mitochondria
isoniazid causes B6 deficiency
Image: Iron trapped in mitochondria of erythroid precursors in bone marrow. Prussian-blue stain (stains Fe).
Labs: increased ferritin decreased TIBC increased serum iron increased percent saturation |
|
|
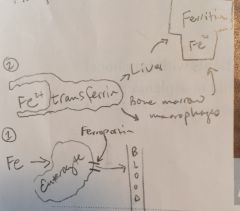
Pathophysiology of microcytic anemia (Goljan) |
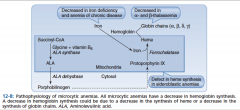
|
|
|
|
General cause of microcytic anemia |
Extra division due to decreased hemoglobin |
|
|
|
General cause of macrocytic anemia |
Cells fail to divide due to decreased DNA |
|
|
|
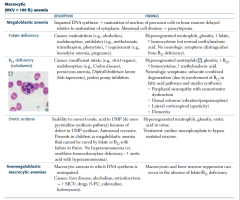
Macrocytic anemias |
|

1) All cells big, including RBCs and neutrophils (hyperhsegmented); enlargement of gut epithelial cells |
|
|
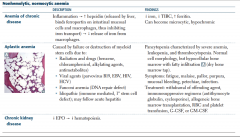
General:
normocytic, normochromic anemia
intravascular hemolysis
extravascular hemolysis |

|

|
|
|
Nonhemolytic, normocytic anemia:
anemia of chronic disease
aplastic anemia
chronic kidney disease |
|

|
|
|
Hereditary spherocytosis |

|
|
|
|
G6PD deficiency |

|

|
|
|
Pyruvate kinase deficiency |

|

|
|
|
HbC defect Paroxysmal nocturnal hemoglobinuria |

|

|
|
|
Sickle cell anemia |

|

|
|

Extrinsic hemolytic normocytic anemias |
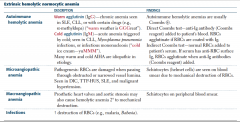
|
1) Warm, Tx: steroids, IVIG, splenectomy
Warm causes spheroctosis b/c membrane consumed by macrophages
Direct Baby Indirect Coombs Mom
Don't Buy Inexpensive Combs for Mom |
|
|
Lab values in anemia
and
Causes of leukopenia |
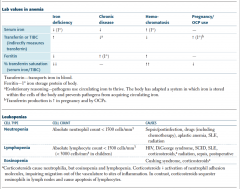
|
Haptoglobin: transports "freed" hemoglobin
Hemosiderin: Iron storage complex
Transferrin made in liver |
|
|
Heme synthesis, porphyrias, and lead poisoning |

|
|
|
|
Coagulation disorders: hemophilia A/B and Vitamin K deficiency |
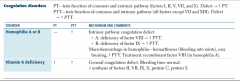
|

Also: liver failure: decreased production of cog factors, dec. Vit K activation, follow with PT
Also: large-volume transfusions (dilution) |
|
|
Platelet disorders
Bernard-Soulier
Glanzmann thrombasthenia
Immune thrombocytopenia
Thrombotic thrombocytopenia purpura
HUS |
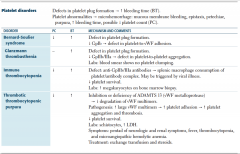
|

|
|
|
Mixed platelet and coagulation disorders:
von Willebrand disease
DIC |
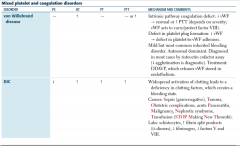
|

|
|
|
Hereditary thrombosis syndromes leading to hypercoagulability:
Factor V Leiden
Prothrombin gene mutation
Antithrombin deficiency
Protein C or S deficiency |

|

|
|
|
Blood transfusion therapy
Packed RBCs
Platelets
Fresh frozen plasma
Cryo |
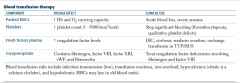
|
|
|
|
Polychromasia |
|
|

|
basophilic stippling |
|
|
|
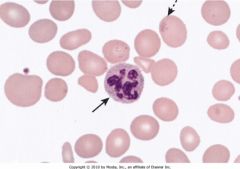
Peripheral blood in megaloblastic anemia showing a hypersegmented neutrophil (solid arrow) with nine lobes. Neutrophils normally have less than five nuclear segments. Hypersegmented neutrophils are excellent markers of folate and vitamin B12 deficiency. The enlarged, egg-shaped red blood cells (macro-ovalocytes; interrupted arrow) characteristic of macrocytic anemias are associated with problems in DNA maturation. |
|
|
|
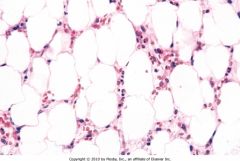
Bone marrow biopsy in aplastic anemia. The biopsy shows a marrow largely replaced by adipose cells. Scattered lymphocytes are present in between adipose cells. |
|
|

|
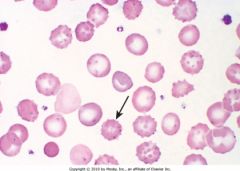
Peripheral blood with sickle cells and Howell-Jolly bodies. The three dense boat-shaped sickle cells and the two cells containing a single dark, round inclusion (arrows) represent nuclear remnants. Howell-Jolly bodies in sickle cell disease indicate splenic dysfunction. |
|
|
|
Peripheral blood smear in pyruvate kinase deficiency. The arrow shows one of many red blood cells with thorny projections (echinocytes) extending from the red blood cell membrane. |
|
|
|
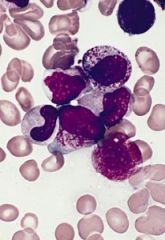
The hypergranular form of APL features faggot cells. This term is applied to these blast cells because of the presence of numerous Auer rods in the cytoplasm. The accumulation of these Auer rods gives the appearance of a bundle of sticks, from which the cells derive their name. |
|
|
|
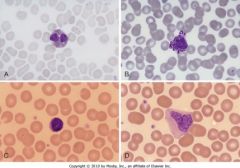
Normal morphology of eosinophil (A), basophil (B), lymphocyte (C), and monocyte (D). The cytoplasm of an eosinophil (A) is packed with reddish-orange granules that do not cover the nucleus. The cytoplasm of a basophil (B) is packed with large purplish black granules that cover the usually bilobed nucleus. The cytoplasm of a small lymphocyte (C) is scant and surrounds a nucleus that is usually round (sometimes indented) and contains condensed nuclear chromatin. The cytoplasm of a monocyte (D) is grayish blue and contains many fine azurophilic granules and one or more clear vacuoles. The nucleus is large, eccentrically located, and either round, kidney- or horseshoe-shaped (monocyte in the picture), or lobulated. |
|
|
|
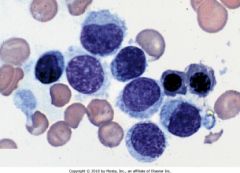
Peripheral blood in hairy cell leukemia. Clusters of neoplastic cells show dense chromatin and cytoplasmic projections. |
|
|
|
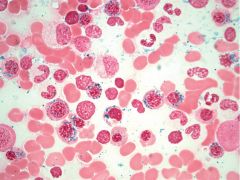
12-13: Ringed sideroblasts in a bone marrow aspirate. Dark blue iron granules around the nucleus of developing normoblasts (arrows) represent iron trapped within mitochondria and indicate a defect in mitochondrial heme synthesis (sideroblastic anemia). |
|

