![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
99 Cards in this Set
- Front
- Back
|
Michaelis-Menton kinetics |
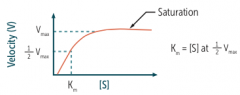
Km - inversely related to affinity of enzyme for substrate Vmax - directly proportional to enzyme concentration |
|
|
Lineweaver-Burk plot |
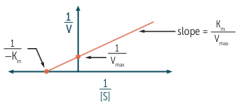
Inc. y-intercept, dec. Vmax Inc. x-intercept (toward O), inc. Km |
|
|
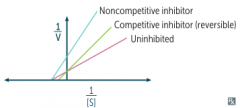
Competitive inhibitors, reversible
Resemble substrate: Overcome by inc. [S]: Bind active site: Effect on Vmax: Effect on Km: Pharmacodynamics: |
Competitive inhibitors, reversible
Resemble substrate: Yes Overcome by inc. [S]: Yes Bind active site: Yes Effect on Vmax: Unchanged Effect on Km: Increase Pharmacodynamics: decrease potency |
|
|
Competitive inhibitors, irreversible
Resemble substrate: Overcome by inc. [S]: Bind active site: Effect on Vmax: Effect on Km: Pharmacodynamics: |
Competitive inhibitors, irreversible
Resemble substrate: Yes Overcome by inc. [S]: No Bind active site: Yes Effect on Vmax: Decrease Effect on Km: Unchanged Pharmacodynamics: Decrease efficacy |
|
|
Noncompetitive inhibitors
Resemble substrate: Overcome by inc. [S]: Bind active site: Effect on Vmax: Effect on Km: Pharmacodynamics: |
Noncompetitive inhibitors
Resemble substrate: No Overcome by inc. [S]: No Bind active site: No Effect on Vmax: Decrease Effect on Km: Unchanged Pharmacodynamics: Decrease efficacy |
|
|
Enzyme inhibition graph |
|
|
|
Bioavaliability |
Fraction of drug reaching systemic circulation unchanged (F) |
|
|
Bioavalibility: IV and Oral |
IV: F = 100%
Oral: F <100% - incomplete absorption and first-pass metabolism |
|
|
Volume of distribution (Vd) |
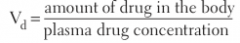
Volume occupied by total amount of drug in body relative to its plasma concentration
|
|
|
Low Vd
Compartment: Drug types: |
Compartment: Blood
Drug types: Large/charged molecules; plasma protein bound
Apparent Vd of plasma protein-bound drugs can be altered by liver/kidney disease (dec. protein binding, inc. Vd) |
|
|
Medium Vd
Compartment: Drug types: |
Medium Vd
Compartment: ECF
Drug types: small hydrophilic molecules |
|
|
High Vd
Compartment: Drug types: |
High Vd
Compartment: All tissues including fat
Drug types: Small lipophilic molecules, especially if bound to tissue protein |
|
|
Clearance (CL) |
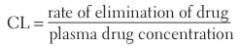
CL = Vd x Ke (elimination constant)
Decreased with cardiac, hepatic, renal problems |
|
|
Half-life |
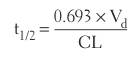
Property of first-order elimination
|
|
|
More half-life info:
How many half-lives until drug infused at constant rate reaches steady-state?
How many half-lives until it reaches 90% of steady-state level?
Half-life chart: # half-lives and % remaining |
Infused drug at constant rate takes 4-5 half-lives to reach steady state
Takes 3.3 half-lives to reach 90% of steady state level |
|
|
Loading dose |
![Cp = target plasma [ ] at steady state
Unchanged by liver/renal disease](https://images.cram.com/images/upload-flashcards/37/52/10/8375210_m.png)
Cp = target plasma [ ] at steady state Vd = distribution volume F = bioavailability
Unchanged by liver/renal disease |
|
|
Maintenance dose |
![Cp = target plasma [ ] at steady state
Tau = dosage interval (if not given continuously)
Decreased by liver/renal disease](https://images.cram.com/images/upload-flashcards/37/52/16/8375216_m.png)
Cp = target plasma [ ] at steady state Tau = dosage interval (if not given continuously) F = bioavailability
Decreased by liver/renal disease |
|
|
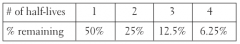
Zero-order elimination |
Constant rate of elimination, regardless of Cp - Constant amount eliminated with time - Cp decreases linearly with time - Capacity-limited elimination
Phenytoin, Ethanol, and Aspirin - PEA is shaped like 0
|
|
|
First-order elimination |
![Elimination rate directly proportional to [drug]
- Constant fraction eliminated with time
- Cp decreases exponentially with time
- Flow dependent elimination](https://images.cram.com/images/upload-flashcards/36/90/36/8369036_m.png)
Elimination rate directly proportional to [drug] - Constant fraction eliminated with time - Cp decreases exponentially with time - Flow dependent elimination |
|
|
Trapped in urine/cleared in urine or reabsorbed?
Ionized species: Neutral species: |
Trapped in urine/cleared in urine or reabsorbed?
Ionized species: Trapped/cleared Neutral species: Reabsorbed |
|
|
Urine pH and drug elimination
Weak acids |
Weak acids - Trapped in basic environments - Treat overdose with bicarbonate
RCOOH <=> RCOO- + H+ (Lipid soluble) (Trapped)
Ex: phenobarbital, methotrexate, aspirin, TCAs
|
|
|
Urine pH and drug elimination
Weak bases |
Weak bases - Trapped in acidic environments - Treat overdose with ammonium chloride
RNH3+ <=> RNH2 + H+ (Trapped) (Lipid soluble) |
|
|
Drug metabolism: Phase I |
Reduction, oxidation, and hydrolysis with cytochrome P-450
Yields slightly polar, water-soluble metabolites - May still be active
Lost by geriatrics first |
|
|
Drug metabolism: Phase II |
Conjugation (Glucuronidation, Acetylation, Sulfation)
Yields polar, inactive metabolites - renally secreted
Geriatric patients have GAS Slow acetylators: dec. metabolism, inc. side effects |
|
|
Efficacy |
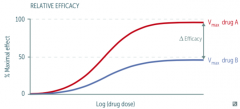
Max effect drug can produce - Y-value = Vmax - Inc y = inc Vmax = inc efficacy - Unrelated to potency |
|
|
Potency |
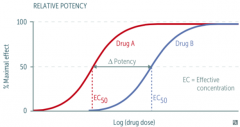
Amount of drug needed for a given effect - Inc potency (dec EC50) = less drug needed - X-value = EC50 - Left shift = dec EC50 = inc potency - Unrelated to efficacy |
|
|
Competitive agonist
Shift curve? Effect on potency or efficacy? Overcome by increasing [S]? Example |
![Competitive agonist
Shift curve right
Dec potency
Overcome by inc [S]
Flumazenil vs. diazapam (agonist) on GABA receptor](https://images.cram.com/images/upload-flashcards/36/92/10/8369210_m.png)
Competitive agonist
Shift curve right Dec potency Overcome by inc [S]
Flumazenil vs. diazapam (agonist) on GABA receptor |
|
|
Noncompetitive agonist
Shift curve? Effect on potency or efficacy? Overcome by increasing [S]? Example |
![Noncompetive agonist
Shift curve down
Dec efficacy
Not overcome by inc [S]
Phenoxybenzamine vs. norepinephine (agonist) on alpha-receptors](https://images.cram.com/images/upload-flashcards/36/92/16/8369216_m.png)
Noncompetive agonist
Shift curve down Dec efficacy Not overcome by inc [S]
Phenoxybenzamine vs. norepinephine (agonist) on alpha-receptors |
|
|
Partial agonist
Shift curve? Effect on potency or efficacy? Overcome by increasing [S]? Examples |
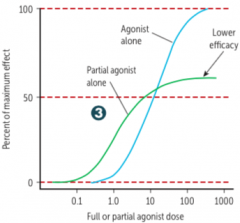
Acts on same site as full agonist but with lower max effect (dec efficacy) - Potency is an independent variable
Buprenorphine vs. morphine (full agonist) at opioid mu-receptors |
|
|
Therapeutic index |
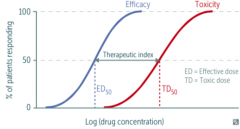
TD50/ED50 = median toxic dose/median effective dose
Safe drugs: high TI Low TI: Digoxin, lithium, theophylline, warfarin LD50 (lethal) often replaces TD50 in animal studies |
|
|
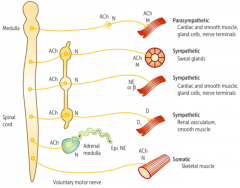
Adrenal medulla and sweat glands are part of sympathetic nervous system but are innervated by cholinergic fibers
Botulinum toxin prevents release of ACh at cholinergic terminals |
|
|
ACh receptors
Nicotinic Muscarinic |
NAChR: ligand-gated Na+/K+ channels - Nn (autonomic ganglia) and Nm (neuromuscular junction)
MAChR: G-protein-coupled recptors - Act through second messengers - 5 subtypes: M1through M5 |
|
|
G-protein-linked 2nd messenger mnemonic |
Qiss and qiq until you're siq of sqs
alpha (1, 2) beta (1, 2) m (1,2,3) d (1,2) h (1,2) v (1,2) |
|
|
Alpha receptors |
Sympathetic
Alpha 1 - q Inc: vascular smooth muscle contraction, pupillary dilator muscle contraction (mydriasis), intestinal and bladder sphincter contraction
Alpha 2 - i Dec: sympathetic outflow, insulin release, lipolysis, aqueous humor production Inc: platelet aggregation |
|
|
Beta receptors |
Sympathetic
Beta 1 - s Inc: HR, contractility, renin release, lipolysis
Beta 2 - s Inc: vasodilation, bronchodilation, lipolysis, insulin release, aqueous humor production Dec: uterine tone (tocolysis), ciliary muscle tone |
|
|
Muscarinic receptors |
Parasympathetic
M1 - q CNA, enteric nervous system
M2 - i Dec: HR and atrial contractility
M3 - q Inc: exocrine gland secretions (lacrimal, salivary, gastric acid), gut peristalsis, bladder contraction, bronchoconstriction, pupillary sphincter contraction (miosis, ciliary muscle contraction (accommodation)
|
|
|
Dopamine receptors |
D1 - s Relaxes renal vascular smooth muscle
D2 - i Modulates transmitter release, especially in brain |
|
|
Histamine receptors |
H1 - q Inc: nasal bronchial mucus production, vascular permeability, contraction of bronchioles, pruritus, pain
H2 - s Inc gastric acid secretion |
|
|
Vasopressin receptors |
V1 - q Inc vascular smooth muscle contraction
V2 - s Inc H2O permeability and reabsorption in collecting tubules of kidney V2 is found in 2 kidneys |
|
|
What receptors use phospholipase C, protein kinase C, and Ca2+ in their pathways? |
H1, A1, V1, M1, M3 (Gq)
All Gq receptors follow this pathway |
|
|
What receptors use adenylyl cyclase, ATP, cAMP, and protein kinase A in their pathways? |
B1, B2, D1, H2, V2 (Gs)
M2, A2, D2 (Gi) MAD 2's
All Gs and Gi receptors follow this pathway |
|

|
Sea otters sleep holding paws so they don't drift apart at night
Just wanted to include all the images. Sorry this is small on phones. |
|
|
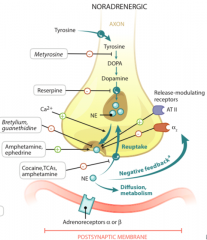
Release of norepi from a sympathetic nerve ending is modulated by norepi itself, acting on presynaptic alpha-2 autoreceptors
Just wanted to include all the images. Sorry this is small on phones. |
|
|
Bethanechol
Category: Clinical application: Action: |
Category: cholinomimetic - direct agonist
Clinical application: postop ilius, neurogenic ileus, urinary retention
Action: activates bowel and bladder smooth muscle; resistant to AChE |
|
|
Carbachol
Category: Clinical application: Action: |
Category: cholinomimetic - direct agonist
Clinical application: constricts pupil, relieves intraocular pressure in glaucoma
Action: carbon copy of acetylcholine |
|
|
Methacholine
Category: Clinical application: Action: |
Category: cholinomimetic - direct agonist
Clinical application: Challenge test for asthma diagnosis
Action: methacholine stimulates muscarinic receptors of airways |
|
|
Pilocarpine
Category: Clinical application: Action: |
Category: cholinomimetic - direct agonist
Clinical application: potent stimulator of sweat, tears, and saliva; open- and closed-angle glaucoma
Action: Contracts ciliary eye muscles (open-angle), pupillary sphincter (closed-angle); resistant to AChE "You cry, drool, and sweat on your pillow" |
|
|
Donepezil, galantamine, rivastigmine
Category: Clinical application: Action: |
Category: cholinomimetic - indirect agonist (anticholinesterase)
Clinical application: Alzheimer disease
Action: inc ACh |
|
|
Edrophonium
Category: Clinical application: Action: |
Category: cholinomimetic - indirect agonist (anticholinesterase)
Clinical application: historically used to dx myasthenia gravis (very short acting), but now MG diagnosed by anti-AChR Ab test
Action: inc ACh |
|
|
Neostigmine
Category: Clinical application: Action: |
Category: cholinomimetic - indirect agonist (anticholinesterase)
Clinical application: Postop and neurogenic ileus and urinary retention, myasthenia gravis, reversal of neuromuscular junction blockade (postop)
Action: inc ACh Neo CNS = no CNS penetration |
|
|
Physostigmine
Category: Clinical application: Action: |
Category: cholinomimetic - indirect agonist (anticholinesterase)
Clinical application: ACh toxicity; crosses blood-brain-barrier (CNS)
Action: inc ACh Physostigmine phyxes atropine overdose |
|
|
Pyridostigmine
Category: Clinical application: Action: |
Category: cholinomimetic - indirect agonist (anticholinesterase)
Clinical application: Myasthenia gravis (long acting); doesn't penetrate CNS
Action: inc ACh; inc muscle strength Pyridostigmine gets rid of myasthenia gravis |
|
|
Potential side-effect of cholinomimetics to watch for |
Cholinomimetics can cause exacerbation of COPD, asthma, and peptic ulcers |
|
|
Cholinesterase inhibitor poisoning |
Due to organophosphates that irreversibly inhibit AChE Antidote: atropine (competitive inhibitor) + pralidoxime (regenerates AChE if given early)
DUMBBELSS diarrhea, urination, miosis, bronchospasm, bradycardia, excitation of skeletal muscle and CNS, lacrimation, sweating, salivation |
|
|
Atropine, homatropine, tropicamide
Category: Organ systems: Clinical application:
|
Category: muscarinic antagonist
Organ systems: Eye
Clinical applications: produce mydriasis and cycloplegia |
|
|
Benztropine
Category: Organ systems: Clinical application: |
Category: muscarinic antagonist
Organ systems: CNS
Clinical applications: Parkinson disease (park my Benz); acute dystonia |
|
|
Glycopyrrolate
Category: Organ systems: Clinical application: |
Category: muscarinic antagonist
Organ systems: GI, respiratory
Clinical applications: Parenteral: preoperatively to reduce airway secretions Oral: drooling, peptic ulcer
|
|
|
Hyoscyamine, dicyclomine
Category: Organ systems: Clinical application: |
Category: muscarinic antagonist
Organ systems: GI
Clinical applications: antispasmodic for irritable bowel syndrome |
|
|
Ipratropium, tiotropium
Category: Organ systems: Clinical application: |
Category: muscarinic antagonist
Organ systems: respiratory
Clinical applications: COPD, asthma I pray I can breathe soon! |
|
|
Oxybutynin, solifenacin, tolterodine
Category: Organ systems: Clinical application: |
Category: muscarinic antagonist
Organ systems: genitourinary
Clinical applications: reduce bladder spasms and urge urinary incontinence (overactive bladder) |
|
|
Scopolamine
Category: Organ systems: Clinical application: |
Category: muscarinic antagonist
Organ systems: CNS
Clinical applications: motion sickness |
|
|
Albuterol, salmeterol
Category: Receptors effected: Clinical application: |
Category: Sympatheticomimetic
Receptors effected: B2 > B1
Clinical application: Albuterol for acute asthma, salmeterol for long-term asthma or COPD |
|
|
Dobutamine
Category: Receptors effected: Clinical application: |
Category: Sympatheticomimetic
Receptors effected: B1 > B2, A
Clinical application: heart failure (inotropic > chronotropic), cardiac stress testing |
|
|
Dopamine
Category: Receptors effected: Clinical application: |
Category: Sympatheticomimetic
Receptors effected: D1 = D2 > B > A
Clinical application: unstable bradycardia, HF, shock - Inotropic and chronotropic alpha effects predominate at high doses |
|
|
Epinephrine
Category: Receptors effected: Clinical application: |
Category: Sympatheticomimetic
Receptors effected: B > A
Clinical application: anaphylaxis, asthma, open-angle glaucoma - Alpha effects predominate at high doses - Significantly stronger effect at beta 2 receptor than norepi |
|
|
Isoprotenrenol
Category: Receptors effected: Clinical application: |
Category: Sympatheticomimetic
Receptors effected: B1 = B2
Clinical application: electrophysiologic evaluation of tachyarrhythmias - Can worse ischemia |
|
|
Norepinephrine
Category: Receptors effected: Clinical application: |
Category: Sympatheticomimetic
Receptors effected: A1 > A2 > B1
Clinical application: hypotension (but dec renal perfusion) - Weaker effect on beta 2 receptor than epi |
|
|
Phenylephrine
Category: Receptors effected: Clinical application: |
Category: Sympatheticomimetic
Receptors effected: A1 > A2
Clinical application: hypotension (vasoconstriction), ocular procedures (mydriatic), rhinitis (decongestant) |
|
|
Amphetamine
Category: Mechanism: Clinical application: |
Category: Indirect sympatheticomimetic
Mechanism: indirect general agonist, reuptake inhibitor, also releases stored catecholamines
Clinical application: narcolepsy, obesity, ADHD |
|
|
Cocaine
Category: Mechanism: Symptoms: |
Category: Indirect sympatheticomimetic
Mechanism: indirect general agonist, reuptake inhibitor
Symptoms: causes vasoconstriction and local anesthesia
Never give beta-blockers if cocaine intox suspected (can lead to unopposed alpha 1 activation and extreme HTN) |
|
|
Ephedrine
Category: Mechanism: Clinical application: |
Category: Indirect sympatheticomimetic
Mechanism: indirect general agonist, reuptake inhibitor, releases stored catecholamines
Clinical application: nasal decongestion, urinary incontinence, hypotension |
|
|
Norepinephrine vs. isoproterenol |
Norepinephrine inc BP (alpha 1) but dec HR b/c inc mean arterial pressure causes reflex bradycardia
Isoproterenol has little alpha effect but causes vasodilation (beta 2), resulting in dec MAP and inc HR through beta 1 and reflex activity |
|
|
Clonidine
Category: Applications: Toxicity: |
Category: Sympatholytic (alpha 2 agonist)
Applications: hypertensive urgency (limited situations); doesn't decrease renal blood flow ADHD, Tourette syndrome
Toxicity: CNS depression, bradycardia, hypotension, respiratory depression, miosis |
|
|
Alpha-methyldopa
Category: Applications: Toxicity: |
Category: Sympatholytic (alpha 2 agonist)
Applications: HTN in pregnancy
Toxicity: direct Coombs positive hemolysis, SLE-like syndrome |
|
|
Non-selective alpha blockers
Applications: Side effects: |
Phenoxybenzamine (irreversible) Applications: pheochromocytoma (preoperative) to prevent catecholamine (hypertensive) crisis
Phentolamine (reversible) Applications: give to patients on MAO inhibitors who eat tyramine-containing foods
Side effects: orthostatic hypotension, reflex tachycardia
|
|
|
Alpha 1 selective blockers
Examples: Applications: Side effects: |
Examples: prazosin, terazosin, dexazosin, tamsulosin (all end in -osin)
Applications: urinary symptoms of BPH, PTSD (prazosin), HTN (except tamsulosin)
Side effects: 1st-dose orthostatic hypotension, dizziness, headache |
|
|
Alpha 2 selective blockers
Applications: Side effects: |
Mirtazapine
Applications: depression
Side-effects: inc serum cholesterol and appetite |
|
|
Effect on blood pressure of alpha-blockade of epinephrine vs. phenylephrine |
Epinephrine Initial response: increase BP (alpha response) After alpha-block: decrease BP below normal (beta response)
Phenylephrine Initial response: increase BP (alpha response) After alpha-block: BP back to normal (not decreased like epi b/c it has no beta action) |
|
|
Beta-blocker application and effects |
Angina pectoris: dec HR and contractility, dec O2 consumption MI: decrease mortality SVT (metoprolol, esmolol): dec AV conduction velocity (class II antiarrhythmic) HTN: dec cardiac output, dec renin secretion (beta 1 receptor blockade on JGA cells) Heart failure: dec mortality in chronic HF Glaucoma (timolol): dec secretion of aqueous humor |
|
|
Beta-blocker toxicity |
Impotence Heart issues (bradycardia, AV block, HF) CNS issues (seizures, sedation, sleep alterations) Dyslipidemia (metoprolol) Asthma/COPD exacerbations
Don't give with cocaine (unopposed alpha - HTN)
Still give to diabetics - don't worry about hypoglycemia b/c benefits outweigh risks |
|
|
Beta 1 selective antagonists |
Acebutolol, (partial agonist), atenolol, betaxolol, esmolol, metoprolol
Selective antagonists mostly go from A to M Beta 1 with 1st 1/2 of alphabet |
|
|
Non-selective beta antagonists |
Nadolol, pindolol (partial agonist), propranolol, timolol
Non-selective antagonists mostly go from N to Z Beta 2 with the 2nd 1/2 of the alphabet |
|
|
Non-selective alpha and beta antagnoists |
Carvedilol and labetalol
Non-selective alpha and beta antagonists have modified endings (-ilol and -atol instead of -olol) |
|
|
Nebivolol - what's special about it? |
Combines cardiac-selective beta 1 blockade with stimulation of beta 3 receptors, activating nitric oxide synthase in vasculature |
|
|
Study the list of specific antidotes and drug reactions from page 257 to 260 in First Aid 2015. |
It is too long of a list for flashcards. Sorry :( |
|
|
Drugs that cause.....
Vasospasm |
Cocaine, sumatriptan, ergot alkaloids |
|
|
Drugs that cause.....
Cutaneous flushing |
Vancomycin, adenosine, niacin, Ca2+ channel blockers
Vanc |
|
|
Drugs that cause.....
Dilated cardiomyopathy |
Anthacyclines (doxorubicin, daunorubicin)
Prevent with dexrazoxane |
|
|
Drugs that cause.....
Torsades de pointes |
Class II (solatol) and class IA (quinidine) antiarrhymics, macrolide antibiotics, antipsychotics, TCAs |
|
|
Drugs that cause.....
Adrenocortical insufficiency |
HPA surpression secondary to glucocorticoid withdrawal |
|
|
Drugs that cause.....
Hot flashes |
Tamoxifen, clomiphene |
|
|
Drugs that cause.....
Hyperglycemia |
Tacrolimus, protease inhibitors, niacin, HCTZ, corticosteroids
Taking pills necessitates having blood checked |
|
|
Drugs that cause.....
Hypothyroidism |
Lithium, amiodarone, sulfonamides |
|
|
Drugs that cause.....
Acute cholestatic hepatitis, jaundice |
Erythromycin |
|
|
Drugs that cause.....
Diarrhea |
Metformin, erythromycin, colchicine, orlistat, acarbose
Might excite colon on accident |
|
|
Drugs that cause.....
Focal to massive hepatic necrosis |
Halothane, amanita phalloides (death cap mushroom), valproic acid, acetaminophen
Liver HAVAc |
|
|
Drugs that cause.....
Hepatitis |
Rifampin, isoniazid, pyrazinamide, statins, fibrates |
|
|
Drugs that cause.....
Pancreatitis |
Didanosine, corticosteroids, alcohol, valproic acid, azathioprine, diuretics (furosemide, HCTZ)
Drugs causing a violent abdominal distress |
|
|
Drugs that cause.....
Pseudomembranous colitis |
Clindamycin, ampicillin, cephalosporins
Antibiotics predispose to superinfection by resistant C. difficile |

