![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
221 Cards in this Set
- Front
- Back
|
Enzyme Kinetics - explain Km
|
![Km reflects the affinity of the enzyme for its substrate. It is the point on the substrate concentration vs. velocity graph where the substrate concentration leads to a reaction rate that is 1/2 of Vmax.
Km = [s] at 1/2 Vmax](https://images.cram.com/images/upload-flashcards/890414/565701_m.gif)
Km reflects the affinity of the enzyme for its substrate. It is the point on the substrate concentration vs. velocity graph where the substrate concentration leads to a reaction rate that is 1/2 of Vmax.
Km = [s] at 1/2 Vmax |
|
|
Enzyme Kinetics - explain Vmax
|
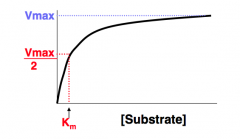
Vmax is directly proportional to the enzyme concentration. It is the maximum reaction rate that can be achieved, after which point increasing the substrate concentration will not increase the rate. Thus, the enzymes are completely saturated with substrate.
|
|
|
Enzyme Kinetics - explain the inverse graph and how to interpret Km and Vmax
|
![If you plot 1/[s] vs. 1/[v] the curve becomes linear. The y-intercept is 1/Vmax and the x-intercept is 1/-Km. If the x intercept moves to the right, Km is increased and thus affinity is lower. If the y intercept moves up, Vmax goes down.
The slope o](https://images.cram.com/images/upload-flashcards/890414/565703_m.jpeg)
If you plot 1/[s] vs. 1/[v] the curve becomes linear. The y-intercept is 1/Vmax and the x-intercept is 1/-Km. If the x intercept moves to the right, Km is increased and thus affinity is lower. If the y intercept moves up, Vmax goes down.
The slope of this line is Km/Vmax. |
|
|
Enzyme Kinetics - explain the effects of competitive and non-competitive inhibitors on the inverse line (1/[s] vs. 1/v)
|
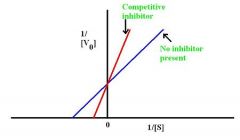
A non-competitive inhibitor will decrease Vmax but the binding affinity remains unchanged (Km does not change). Therefore you see the line rotate counter-clockwise, with a higher y-intercept but the same x-intercept.
A competitive inhibitor does not effect Vmax but it increases Km (lower binding affinity). Therefore, the x-intercept shifts to the right and the y-intercept remains unchanged. Thus the line has a steeper slope (see picture). |
|
|
Enzyme Kinetics - explain the differences between competitive and non-competitive inhibitors
|
Competitive inhibitors -
Resemble substrate. Overcome by increased [s] Bind the active site No effect on Vmax. Increases Km Decreases potency. Noncompetitive inhibitors - Does not resemble substrate Not overcome by increased [s] Does not bind the active site Decreases Vmax No effect on Km Decreases efficacy. |
|
|
Pharmacokinetics - Volume of Distribution (Vd)
|
Relates the amount of drug in the body to the plasma concentration. Vd of plasma protein-bound drugs can be altered by liver and kidney disease (decreased protein binding, increased Vd).
Vd = (amount of drug in the body) / (plasma drug concentration) Drugs with: Low Vd (4-8 L) distribute in blood; are large or charged molecules. Medium Vd distribute in extracellular space or body water; are small hydrophilic molecules that do not bind plasma proteins. High Vd (> body weight) distribute into all tissues; are small, lipophilic molecules that bind strongly to extravascular proteins. |
|
|
Pharmacokinetics - Clearance (CL)
|
Relates the rate of elimination to the plasma concentration.
CL = (rate of elimination of drug) / (plasma drug concentration) = Vd x Ke (elimination constant) |
|
|
Pharmacokinetics - Half-life (t1/2)
|
The time required to change the amount of drug in the body by 1/2 during elimination (or constant infusion). Property of first-order elimination. A drug infused at a constant rate takes 4-5 half-lives to reach steady state.
t1/2 = ( 0.7 x Vd) / CL # half lives / concentration 1 / 50% 2 / 75% 3 / 87.5% 4 / 93.75% |
|
|
Pharmacokinetics - Bioavailability (F)
|
Fraction of administered drug that reaches circulation.
IV: F = 100% Orally: F = % that survives first pass in liver or gut |
|
|
Dosage calculations - Loading dose? Maintenance dose?
|
Loading dose = Cp x Vd/F
- If you have a large volume of distribution, the loading dose needs to be higher - If you have a small bioavailability, the loading dose needs to be higher Maintenance dose = Cp x CL/F - If the clearance rate is high, you needa high maintenance dose. Cp = target plasma concentration In renal or liver disease, maintenance dose decreases and loading dose is unchanged. Frequency of dosing is not affected by time to steady state but is affected by t1/2. |
|
|
Elimination of drugs - Zero-order elimination
|
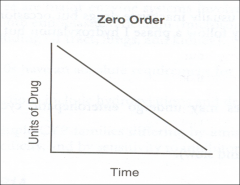
Rate of elimination is constant regardless of Cp (i.e., constant AMOUNT of drug is eliminated per unit time). Cp decreases linearly with time. Examples of drugs - Phenytoin, Ethanol, and Aspirin (at high or toxic concentrations).
|
|
|
How to remember some examples of drugs that are zero-order elimination?
|
PEA - a pea is round, shaped like the "O" in zero-order
Phenytoin Ethanol Aspirin (at high or toxic concentrations) |
|
|
Elimination of drugs - First-order elimination
|
Rate of elimination is proportional to the drug concentration (i.e., constant FRACTION of drug eliminated per unit time). Cp decreases exponentially with time.
|
|
|
Urine pH and drug elimination - basics
|
Ionized species are trapped in urine and cleared quickly. Neutral forms can be reabsorbed.
|
|
|
Urine pH and drug elimination - Weak acids
|
Examples: phenobarbital, methotrexate, aspirin. Trapped in basic environments. Treat overdose with bicarbonate.
RCOOH <===> RCOO- + H+ (lipid soluble) (trapped) |
|
|
Urine pH and drug elimination - Weak bases
|
Examples: amphetamines. Trapped in acidic environments. Treat overdose with ammonium chloride.
RNH3+ <======> RNH2 + H+ (trapped) (lipid soluble) |
|
|
Phase I vs. phase II metabolism
|
Phase I - (reduction, oxidation, hydrolysis) usually yields slightly polar, water-soluble metabolites (often still active) - cytochrome P-450
Phase II - (Glucuronidation, Acetylation, Sulfation) usually yields very polar, inactive metabolites - Conjugation Geriatric patients lose phase I first. Patients who are slow acetylators have greater side effects from certain drugs because of decreased rate of metabolism. |
|
|
How to remember which phase of metabolism geriatric patients still have?
|
Geriatric patients have GAS (phase II).
|
|
|
Efficacy vs. Potency
|
Efficacy - maximal effect a drug can produce. High-efficacy drug classes are analgesic (pain) medications, antibiotics, antihistamines, and decongestants.
Potency - amount of drug needed for a given effect. Increased potency, increased affinity for receptor. Highly potent drug classes include chemotherapeutic (cancer) drugs, antihypertensive (blood pressure) drugs, and antilipid (cholesterol) drugs. |
|
|
Pharmacodynamics - Competitive antagonists
|
Shift dose vs. % of maximum effect curve to right --> decreased potency, no change in efficacy.
Example - Diazepam + flumazenil on GABA receptor |
|
|
Pharmacodynamics - Noncompetitive antagonists
|
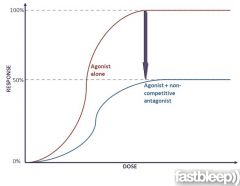
Shifts curve down --> decreased efficacy.
Example - NE + phenoxybenzamine on alpha-receptors |
|
|
Pharmacodynamics - Partial agonists
|
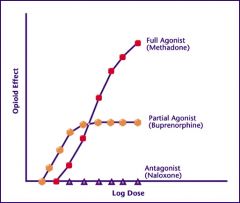
Acts at same site as full agonist, but with reduced maximal effect --> decreased efficacy.
Potency is a different variable and can be increased or decreased. Examples - Morphine + buprenorphine at opioid mu receptor. |
|
|
Therapeutic Index
|
Measurement of drug safety.
LD50 (median lethal dose) ------------------------------------ ED50 (median effective dose) Safer drugs have higher TI values. |
|
|
How to remember the numerator and denominator for therapeutic index?
|
TILE
TI = LD50 / ED50 |
|
|
Central and peripheral nervous system - pharmacology details?
|
Parasympathetic - Preganglionic ACh (N), postganglionic ACh (M) - Cardiac and smooth muscle, gland cells, nerve terminals
Sympathetic - preganglionic ACh (N), postganglionic varies Sweat glands - Postsynaptic ACh (M) Most sympathetic - Postsynaptic NE (alpha, beta) - cardiac and smooth muscle, gland cells, nerve terminals Renal vascular smooth muscle - D (D1) Adrenal medulla - Presynaptic is ACh (N), postsynaptic is endocrine (secretes NE, Epi) Somatic - ACh (N) - skeletal muscle Note that adrenal medulla and sweat glands are part of the sympathetic NS but are innervated by cholinergic fibers. Botulinum toxin prevents release of neurotransmitter at all cholinergic terminals. |
|
|
ACh receptors - details?
|
Nicotinic ACh receptors are ligand-gated Na+/K+ channels; N(n) (found in autonomic ganglia) and N(m) (found in neuromuscular junction) subtypes.
Muscarinic ACh receptors are G-protein-coupled receptors that act through 2nd messengers; 5 subtypes: M1, M2, M3, M4, M5 |
|
|
G-protein-linked second messengers - alpha 1 - G-protein class? Major functions?
|
Gq
Increases vascular smooth muscle contraction, increases pupillary dilator muscle contraction (mydriasis), increases intestinal and bladder sphincter muscle contraction. |
|
|
G-protein-linked second messengers - alpha 2 - G-protein class? Major functions?
|
Gi
Decreases sympathetic outflow, decreases insulin release. |
|
|
G-protein-linked second messengers - Beta 1 - G-protein class? Major functions?
|
Gs
Increased heart rate, increased contractility, increased renin release, increased lipolysis. |
|
|
G-protein-linked second messengers - Beta 2 - G-protein class? Major functions?
|
Gs
Vasodilation, bronchodilation, increased heart rate, increased contractility, increased lipolysis, increased insulin release, decreased uterine tone. |
|
|
G-protein-linked second messengers - M1 - G-protein class? Major functions?
|
Gq
CNS, enteric nervous system |
|
|
G-protein-linked second messengers - M2 - G-protein class? Major functions?
|
Gi
Decreases heart rate and contractility of atria |
|
|
G-protein-linked second messengers - M3 - G-protein class? Major functions?
|
Gq
Increased exocrine gland secretions (e.g., sweat, gastric acid), increased gut peristalsis, increased bladder contraction, bronchoconstriction, increased pupillary sphincter muscle contraction (miosis), ciliary muscle contraction (accomodation) |
|
|
G-protein-linked second messengers - D1 - G-protein class? Major functions?
|
Gs
Relaxes renal vascular smooth muscle. |
|
|
G-protein-linked second messengers - D2 - G-protein class? Major functions?
|
Gi
Modulates transmitter release, especially in brain. |
|
|
G-protein-linked second messengers - H1 - G-protein class? Major functions?
|
Gq
Increases nasal and bronchial mucus production, contraction of bronchioles, pruritis, and pain |
|
|
G-protein-linked second messengers - H2 - G-protein class? Major functions?
|
Gs
Increases gastric acid secretion. |
|
|
G-protein-linked second messengers - V1 - G-protein class? Major functions?
|
Gq
Increased vascular smooth muscle contraction |
|
|
G-protein-linked second messengers - V2 - G-protein class? Major functions?
|
Increased H2O permeability and reabsorption in the collecting tubules of the kidney (V2 is found in the 2 kidneys).
|
|
|
How can you remember the G-protein class of the various ANS and other receptors?
|
Kiss (qiss) and kick (qiq) til you're sick (siq) of sex (sqs).
Alpha 1 - q Alpha 2 - i Beta 1 - s Beta 2 -s M1 - q M2 - i M3 - q D1 - s D2 - i H1 - q H2 - s V1 - q V2 - s |
|
|
Explain the pathway for Gq, Gi, and Gs.
|
Gq - receptor is activated by ligand, then Gq activates phospholipase C. This cleaves lipids to create PIP2. PIP2 splits into DAG and IP3. DAG --> protein kinase C, IP3 -> increases [Ca2+]in.
Gs: Receptor is activated by ligand, Gs activates adenylyl cyclase --> ATP is converted to cAMP --> activates protein kinase A --> increases [Ca2+]in (heart) and activates Myosin light-chain kinase (smooth muscle0 Gi - inhibits adenylyl cyclase --> decreases [Ca2+] in (heart) and deactivates MLCK (smooth muscle) |
|
|
Explain the cholinergic nerve terminal.
|
Choline is transported into the cell (blocked by hemicholinium). Choline + acetyl-CoA (catalyzed by Choline Acetyltransferase) is converted to Acetylcholine. ACh is then transported into vesicles (blocked by vesamicol). Vesicles are then released by exocytosis (activated by Ca2+, inhibited by botulinum).
ACh binds to cholinoceptors on the postsynaptic membrane. ACh is degraded by Acetylcholinesterase to Choline + Acetate. |
|
|
Explain the noradrenergic nerve terminal.
|
Tyrosine is transported into cells. It is converted first to DOPA (inhibited by metyrosine). DOPA is then converted to Dopamine. Dopamine is transported into vesicles (blocked by reserpine) where it is converted to norepinephrine. Norepinephrine is released by exocytosis (activated by Ca2+, inhibited by Guanethidine), activated by amphetamine).
NE acts on adrenoceptors (alpha or beta) and then diffuses out of the cleft, or is brought back by reuptake transport molecules (blocked by cocaine, TCAs, and amphetamine). |
|
|
Explain negative feedback at the NE nerve terminal.
|
NE diffuses back and hits alpha2 receptors which inhibit further exocytotic release of NE molecules. Angiotensin II receptors, when activated, promote exocytosis of NE. M2 receptors, when activated, also act to prevent NE release.
|
|
|
Cholinomimetic agents - Bethanechol - Clinical uses? Action?
|
Uses: Postoperative and neurogenic ileus and retention
Action: Activates Bowel and Bladder smooth muscle; resistant to AChE. |
|
|
How to remember action of bethanechol?
|
"Bethany, call (bethanechol) me if you want to activate your Bowels and Bladder."
|
|
|
Cholinomimetic agents - Carbachol - Clinical uses? Action?
|
Uses: Glaucoma, pupillary contraction, and relief of intraocular pressure
Action: CARBon copy of acetylcholine |
|
|
Cholinomimetic agents - Pilocarpine - Clinical uses? Action?
|
Clinical uses: Potent stimulator of sweat, tears, saliva
Action: Contracts ciliary muscle of eye (open angel), pupillary sphincter (narrow angle); resistant to AChE. |
|
|
How to remember actions of pilocarpine?
|
You cry, drool, and swaet on your PILOw.
|
|
|
Cholinomimetic agents - Methacholine - Clinical uses? Action?
|
Uses: Challenge test for diagnosis of asthma.
Action: Stimulates muscarinic receptors in airway when inhaled. |
|
|
Cholinomimetic agents - Neostigmine - Clinical uses? Action?
|
Uses: Postoperative and neurogenic ileus and urinary retention, myasthenia gravis, reversal of neuromuscular junction blockade (postoperative)
Action: Increases endogenous ACh; no CNS penetration. |
|
|
How to remember the details of neostigmine?
|
NEO CNS = NO CNS penetration.
|
|
|
Cholinomimetic agents - Pyridostigmine - Clinical uses? Action?
|
Uses: Myasthenia gravis (long acting); does not penetrate CNS.
Action: Increases endogenous ACh; increases strength |
|
|
How to remember details of pyridostigmine?
|
pyRIDostigmine gets RID of myasthenia gravis
|
|
|
Cholinomimetic agents - Edrophonium - clinical uses? Action?
|
Uses: Diagnosis of myasthenia gravis (extremely short acting)
Action: Increases endogenous ACh. |
|
|
Cholinomimetic agents - Physostigmine - clinical uses? action?
|
Uses: Glaucoma (crosses blood-brain barrier --> CNS) and atropine overdose
Action: Increases endogenous ACh. |
|
|
How to remember details of physostigmine?
|
PHYsostigmine PHYxes atropine overdose.
|
|
|
Cholinomimetic agents - Echothiophate - Clinical uses? Action?
|
Uses: Glaucoma
Action: Increases endogenous ACh. |
|
|
Cholinomimetic agents - Donepezil - Clinical uses? Action?
|
Uses: Alzheimer's disease
Action: Increases endogenous ACh. |
|
|
What do you need to watch out for with all cholinomimetic agents?
|
Exacerbation of COPD, asthma, and peptic ulcers when giving to susceptible patients.
|
|
|
Cholinesterase inhibitor poisoning - details?
|
Often due to organophosphates, such as parathion, that irreversibly inhibit AChE.
Causes Diarrhea, Urination, Miosis, Bronchospasm, Bradycardia, Excitation of skeletal muscle and CNS< Lacrimation, Sweating, and Salivation. Antidote - atropine + pralidoxime (regenerates active AChE) Organophosphates are components of insecticides; poisoning usually seen in farmers. |
|
|
How to remember effects of cholinesterase inhibitor poisoning?
|
DUMBBELSS
Diarrhea Urination Miosis Bronchospasm Bradycardia Excitation of smooth muscle and CNS Lacrimation Sweating Salivation |
|
|
Muscarinic antagonists - Atropine, homatropine, tropicamide - Organ System? Application?
|
Eye - produces mydriasis and cycloplegia
|
|
|
Muscarinic antagonists - Benztropine - Organ system? Application?
|
CNS - Parkinson's disease
|
|
|
How to remember details of benztropine?
|
PARK my BENZ - treats parkinson's disease
|
|
|
Muscarinic antagonists - Scopalamine - organ system? Application?
|
CNS - motion sickness
|
|
|
Muscarinic antagonists - Ipratropium - Organ system? Application?
|
Respiratory - Asthma, COPD
|
|
|
Muscarinic antagonists - Oxybutynin, glycopyrrolate - Organ system? Application?
|
Genitourinary - Reduce urgency in mild cystitis and reduce bladder spasms
|
|
|
Muscarinic antagonists - Methscopolamine, pirenzepine, propantheline - Organ system? Application?
|
Gastrointestinal - Peptic ulcer treatment
|
|
|
Atropine - effects on Eye? Airway? Stomach? Gut? Bladder? Toxicity?
|
Muscarinic antagonist. Used to treat bradycardia and for opthalmic applications.
Eye - Increased pupil dilation, cycloplegia Airway - Decreased secretions Stomach - Decreased acid secretions. Gut - Decreased motility Bladder - decreased urgency in cystitis Blocks DUMBBELSS Toxicity - Increased body temperature (due to decreased sweating); rapid pulse; dry mouth; dry, flushed skin; cycloplegia; constipation; disorientation. Can cause acute angle-closure glaucoma in elderly, urinary retention in men with prostatic hyperplasia, and hyperthermia in infants. |
|
|
how to remember side effects of atropine?
|
Hot as a hare
Dry as a bone Red as a beet Blind as a bat Mad as a hatter |
|
|
Sympathomimetics - Epinephrine - Which receptors? Applications?
|
alpha 1 - strong
alpha 2 - strong beta 1 - strong beta 2 - medium Dopamine 1 - no effect Used for anaphylaxis, glaucoma (open angle), asthma, hypotension |
|
|
Sympathomimetics - Norepinephrine - Which receptors? Applications?
|
alpha 1 - strong
alpha 2 - strong beta 1 - medium beta 2 - no effect Dopamine - no effect Used for hypotension (but decreases renal perfusion) |
|
|
Sympathomimetics - Isoproterenol - Which receptors? Applications?
|
Alpha 1 - no effect
alpha 2 - no effect Beta 1 - strong Beta 2 - strong Dopamine - no effect Used for AV block (rarely used) |
|
|
Sympathomimetics - Dopamine - Which receptors? Applications?
|
Alpha 1 - strong (high dose)
alpha 2 - strong (high dose) beta 1 - strong (medium dose) beta 2 - medium (medium dose) dopamine 1 receptor - weak agonist (low dose) Used for shock (renal perfusion), heart failure; inotropic and chronotropic; D1 > Beta > alpha |
|
|
Sympathomimetics - Dobutamine - Which receptors? Applications?
|
alpha 1 - weak
alpha 2 - weak beta 1 - strong beta 2 - weak dopamine - no effect Used for heart failure, cardiac stress testing; inotropic, but not chronotropic. |
|
|
Sympathomimetics - Phenylephrine - which receptors? applications?
|
alpha 1 - strong
alpha 2 - medium beta 1 - no effect beta 2 - no effect dopamine - no effect Used for pupillary dilation, vasoconstriction, nasal decongestion. |
|
|
Sympathomimetics - Metaprotereonol, albuterol, salmeterol, terbutaline - Which receptors? Applications?
|
alpha 1 - no effect
alpha 2 - no effect beta 1 - medium beta 2 - strong dopamine - no effect MAST: Metaproterenol and Albuterol for acute asthma; salmeterol for long-term treatment; Terbutaline to reduce premature uterine contractions |
|
|
Sympathomimetics - Ritodrine - Which receptors? Applications?
|
alpha 1 - no effect
alpha 2 - no effect beta 1 - no effect Beta 2 - strong dopamine - no effect Used to reduce premature uterine contractions. |
|
|
Indirect Sympathomimetics - Amphetamine - Action? Application?
|
Indirect general agonist, releases stored catecholamines.
Used to treat narcolepsy, obesity, attention deficit disorder. |
|
|
Indirect Sympathomimetics - Ephedrine - Action? Application?
|
Indirect general agonist, releases stored catecholamines.
Nasal decongestion, urinary incontinence, hypotension. |
|
|
Indirect Sympathomimetics - Cocaine - Action? Application?
|
Indirect general agonist, uptake inhibitor.
Causes vasoconstriction and local anesthesia. |
|
|
Describe how norepinephrine effects SBP, DBP, and HR.
|
NE has alpha > beta effects.
Increased SBP due to increased contractility (Beta 1). Increased DBP due to increased TPR (alpha 1). Decreased HR due to reflex bradycardia. |
|
|
Describe how isoproterenol effects SBP, DBP, and HR.
|
Isoproteronol is beta effects only.
Increased SBP due to increased contractility (but then reduces due to Beta 2 response and reflex sympathetic outflow from hypotension). Decreased DBP due to vasodilation. Increased HR due to Beta 1 agonism. |
|
|
Sympathoplegics - Clonidine, alph-methyldopa - action? application?
|
Centrally acting alpha-2-agnonist --> decreased central adrenergic outflow.
Treats hypertension, especially with renal disease (no decrease in blood flow to kidney). |
|
|
Alpha-blockers - Phenoxybenzamine - Application? Toxicity?
|
Nonselective, irreversible alpha blocker
Pheochromocytoma (use phenoxybenzamine before removing tumor, since high levels of released catecholamines will not be able to overcome blockage). Toxicity: Orthostatic hypotension, reflex tachycardia. |
|
|
Alpha-blockers - Phentolamine - Application? Toxicity?
|
Nonselective, reversible alpha blocker
Give to patients on MAO inhibitors who eat tyramine-containing foods (It is thought that tyramine displaces norepinephrine from vesicles, causing huge release of NE --> hypertensive crisis). |
|
|
Alpha-blockers - Prazosin, terazosin, doxazosin - Application? Toxicity?
|
Selective alpha1 blockers
Used for hypertension, urinary retention in BPH. Toxicity: 1st-dose orthostatic hypotension, dizziness, headache |
|
|
Alpha-blockers - Mirtazapine - Application? Toxicity?
|
Treats depression with insomnia.
Toxicity: Sedation (has H1 agonist properties), increased serum cholesterol,, increased appetite. |
|
|
Describe the effects of epinephrine injection in terms of the effects of epinephrine without alpha blockade and after alpha blockade.
|
Before alpha blockade, epinephrine causes increase in SBP due to Beta-1 agonism and increase in DBP due to alpha-1 agonism.
After alpha blockade, you only have Beta activity and so their is a net depressor effect. |
|
|
Describe the effects of phenylephrine injection in terms of the effects of phenylephrine without alpha blockade and after alpha blockade.
|
Before alpha blockade, you have a net pressor effect (stronger than epinephrine because ONLY alpha agonist).
After alpha blockade, you have no response to the phenylephrine injection. |
|
|
Beta-blockers - give examples
|
anything ending in -lol
Acebutolol, betaxolol, esmolol, atenolol, metoprolol, propranolol, timolol, pindolol, labetalol |
|
|
Beta-blockers - Effect on hypertension
|
Decreased cardiac output, decreased renin secretion (due to beta-receptor blockade on JGA cells)
|
|
|
Beta-blockers - Effect on Angina Pectoris
|
Decreased heart rate and contractility --> decreased O2 consumption
|
|
|
Beta-blockers - Effect on MI
|
Beta-blockers decrease mortality
|
|
|
Beta-blockers - effect on SVT
|
Propranolol, esmolol
Decrease AV conduction velocity (class II antiarrhythmic) |
|
|
Beta-blocker effects on CHF
|
Slows progression of chronic failure
|
|
|
Beta-blocker effects on Glaucoma
|
Timolol
Decreases secretion of aqueous humor. |
|
|
Beta-blocker - toxicities
|
Impotence, exacerbation of asthma, cardiovascular adverse effects (bradycardia, AV block, CHF), CNS adverse effects (sedation, sleep alterations); use with caution in diabetics
|
|
|
Beta-blocker - Beta1 selective antagonists (Beta1 > Beta2)
|
Acebutolol (partial agonist), Betaxolol, Esmolol (short acting), Atenolol, Metoprolol
A BEAM of beta1-blockers. Advantageous in patients with comorbid pulmonary disease. |
|
|
Beta-blocker - Nonselective antagonists (Beta1 = Beta2)
|
Propranolol, Timolol, Nadolol, and Pindolol
Please Try Not Being (beta) Picky |
|
|
Beta blockers - Nonselective (vasodilatory) alpha- and beta-antagonists
|
Carvedilol, labetalol
|
|
|
Beta-blockers - Partial Beta-agonists
|
Pindolol, Acebutolol
(PAPA) |
|
|
Specific Antidotes - Acetaminophen
|
N-acetylcysteine (replenishes glutathione)
|
|
|
Specific Antidotes - Salicylates
|
NaHCO3 (alkalinize urine), dialysis
|
|
|
Specific Antidotes - Amphetamines (basic)
|
NH4Cl (acidify urine)
|
|
|
Specific Antidotes - Acetylcholinesterase inhibitors, organophosphates
|
Atropine, pralidoxime
|
|
|
Specific Antidotes - Antimuscarinic, anticholinergic agents
|
Physostigmine salicylate
|
|
|
Specific Antidotes - Beta-blockers
|
Glucagon
|
|
|
Specific Antidotes - Digitalis
|
Stop dig; normalize K+, Lidocaine, Anti-dig Fab fragments, Mg2+ (KLAM)
|
|
|
Specific Antidotes - Iron
|
Deferoxamine
|
|
|
Specific Antidotes - Lead
|
CaEDTA, dimercaprol, succimer penicillamine
|
|
|
Specific Antidotes - Mercury, arsenic, gold
|
Dimercaprol (BAL), succimer
|
|
|
Specific Antidotes - Copper, Arsenic, Gold
|
Penicillamine
|
|
|
Specific Antidotes - Cyanide
|
Nitrite, Hydroxocobalamin, Thiosulfate
|
|
|
Specific Antidotes - Methemoglobin
|
Methylene blue, vitamin C
|
|
|
Specific Antidotes - Carbon monoxide
|
100% O2, hyperbaric O2
|
|
|
Specific Antidotes - Methanol, ethylene glycol (antifreeze)
|
Fomepizole > ethanol, dialysis
|
|
|
Specific Antidotes - Opioids
|
Naloxone/naltrexone
|
|
|
Specific Antidotes - Benzodiazepines
|
Flumazenil
|
|
|
Specific Antidotes - TCAs
|
NaHCO3 (plasma alkalinization)
|
|
|
Specific Antidotes - Heparin
|
Protamine
|
|
|
Specific Antidotes - Warfarin
|
Vitamin K, fresh frozen plasma
|
|
|
Specific Antidotes - tPA, streptokinase, urokinase
|
Aminocaproic acid
|
|
|
Specific Antidotes - Theophylline
|
Beta-blocker
|
|
|
Drug reactions - Coronary vasospasm
|
Cocaine, sumatriptan
|
|
|
Drug reactions - Cutaneous flushing
|
VANC: Vancomycin, Adenosine, Niacin, Ca2+ channel blockers
|
|
|
Drug reactions - Dilated cardiomyopathy
|
Doxorubicin (adriamycin), daunorubicin
|
|
|
Drug reactions - Torsades de pointes
|
Class III (sotalol), class IA (quinidine) antiarrhythmics
|
|
|
Drug reactions - Agranulocytosis
|
Clozapine, Carbamezapine, Colchicine, Propylthiouracil, Methimazole, Dapsone
|
|
|
How to remember drugs that cause agranulocytosis?
|
Agranulocytosis Could Certainly Cause Pretty Major Damage
Clozapine, Carbamezapine, Colchicine, Propylthiouracil, Methimazole, Dapsone |
|
|
Drug reactions - Aplastic anemia
|
Chloramphenicol, benzene, NSAIDs, propylthiouracil, methimazole
|
|
|
Drug reactions -
Direct Coombs-positive hemolytic anemia |
Methyldopa
|
|
|
Drug reactions -
Gray baby syndrome |
Chloramphenicol
|
|
|
Drug reactions -
Hemolysis in G6PD-deficient patients |
Isoniazid (INH), Sulfonamides, Primaquine, Aspirin, Ibuprofen, Nitrofurantoin
|
|
|
How to remember drugs that cause hemolysis in G6PD-deficient patients?
|
hemolysis IS PAIN
Isoniazid (INH), Sulfonamides, Primaquine, Aspirin, Ibuprofen, Nitrofurantoin |
|
|
Drug reactions - Megaloblastic anemia
|
Phenytoin, Methotrexate, Sulfa drugs
|
|
|
How to remember drugs that cause megaloblastic anemia?
|
having a blast with PMS
Phenytoin, Methotrexate, Sulfa drugs |
|
|
Drug reactions - Thrombotic complications
|
OCPs (e.g., estrogens and progestins)
|
|
|
Drug reactions - Cough
|
ACE inhibitors (note: ARBs like losartan -- no cough)
|
|
|
Drug reactions - Pulmonary fibrosis
|
Bleomycin
Amiodarone Busulfan |
|
|
How to remember drugs that cause pulmonary fibrosis?
|
it's hard to BLAB when you have pulmonary fibrosis
Bleomycin Amiodarone Busulfan |
|
|
Drug reactions - Acute cholestatic hepatitis
|
Macrolides
|
|
|
Drug reactions - Focal to massive hepatic necrosis
|
Halothane, Acetaminophen, Valproic acid, Amanita phalloides (liver HAVAc)
|
|
|
How to remember drugs that cause focal to massive hepatic necrosis?
|
Liver HAVAc
Halothane Acetaminophen Valproic acid Amanita phalloides |
|
|
Drug reactions - Hepatitis
|
INH
|
|
|
Drug reactions - Pseudomembranous colitis
|
Clindamycin, Ampicillin
|
|
|
Drug reactions - adrenocortical insufficiency
|
Glucocorticoid withdrawal (HPA suppression)
|
|
|
Drug reactions - Gynecomastia
|
Spironolactone, Digitalis, Cimetidine, chronic Alcohol use, estrogens, Ketoconazole
|
|
|
How to remember drugs that cause gynecomastia?
|
Some Drugs Create Awesome Knockers
Spironolactone Digitalis Cimetidine chronic Alcohol use Ketoconazole |
|
|
Drug reactions - Hot flashes
|
Tamoxifen, clomiphene (both are SERMs)
|
|
|
Drug reactions - Hypothyroidism
|
Lithium, amiodarone, sulfonamides
|
|
|
Drug reactions - Hyperglycemia
|
Niacin, tacrolimus, protease inhibitors
|
|
|
Drug reactions - fat redistribution
|
Glucocorticoids, protease inhibitors
|
|
|
Drug reactions - Gingival hyperplasia
|
Phenytoin, verapamil
|
|
|
Drug reactions - Gout
|
Furosemide, Thiazides, Niacin, Cyclosporin, Pyrazinamide
|
|
|
Drug reactions - Myopathies
|
Fibrates
Niacin Colchicine Hydroxychloroquine Interferon alpha Penicillamine Statins Glucocorticoids |
|
|
How to remember drugs that cause myopathies?
|
Fish N CHIPS Give you myopathies
Fibrates Niacin Colchicine Hydroxychloroquine Interferon alpha Penicillamine Statins Glucocorticoids |
|
|
Drug reactions - osteoporosis
|
Corticosteroids, heparin
|
|
|
Drug reactions - Photosensitivity
|
Sulfonamides
Amiodarone Tetracyclines |
|
|
How to remember drugs that cause photosensitivity?
|
i SAT for a photo
Sulfonamides Amiodarone Tetracyclines |
|
|
Drug reactions - Rash (Stevens-Johnson syndrome)
|
Penicillin, Ethosuximide, Carbamazepine, Sulfa drugs, Lamotrigine, Allopurinol, Phenytoin, Phenobarbital
|
|
|
How to remember drugs that cause rash (stevens-johnson syndrome)?
|
I got a rash after a PEC SLAPP
Penicillin Ethosuximide Carbamazepine Sulfa drugs Lamotrigine Allopurinol Phenytoin Phenobarbital |
|
|
Drug reactions - SLE-like syndrome
|
Hydralazine
Isoniazid Procainamide Phenytoin |
|
|
How to remember drugs that cause lupus-like syndrome?
|
its not HIPP to have lupus
Hydralazine INH Phenytoin Procainamide |
|
|
Drug reaction - Tendonitis, tendon rupture, and cartilage damage (kids)
|
Fluoroquinolones
|
|
|
Drug reaction - diabetes insipidus
|
Lithium, demeclocycline
|
|
|
Drug reaction - Fanconi's syndrome
|
Expired tetracycline
|
|
|
Drug reaction - Interstitial nephritis
|
Methicillin, NSAIDs, furosemide
|
|
|
Drug reaction - Hemorrhagic cystitis
|
Cyclophosphamide, ifosfamide (prevent by coadministering with mesna)
|
|
|
Drug reaction - SIADH
|
Carbamazepine, cyclophosphamide
|
|
|
Drug reaction - cinchonism
|
Quinidine, quinine
Cinchonism means overdose on quinine derivatives |
|
|
Drug reaction - Parkinson-like syndrome
|
Antipsychotics, reserpine, metoclopramide
|
|
|
Drug reaction - seizures
|
Bupropion, imipenem/cilastatin, isoniazid
|
|
|
Drug reaction - Tardive dyskinesia
|
Antipsychotics
|
|
|
Drug reaction - Antimuscarinic
|
Atropine, TCAs, H1 blockers, neuroleptics, digoxin
|
|
|
Drug reaction - Disulfiram-like reaction
|
Metronidazole, certain cephalosporins, procarbazine, 1st-generation sulfonylureas
|
|
|
Drug reaction - Nephrotoxicity/ototoxicity
|
Aminoglycosides, vancomycin, loop diuretics, cisplatin
|
|
|
P-450 Interactions - inducers (+)
|
Quinidine
Barbiturates St. John's Wort Phenytoin Rifampin Griseofulvan Carbamazepine Chronic alcohol use |
|
|
How to remember CYP450 inducers?
|
Queen Barb Steals Phen-phen and Refuses Greasy Carbs Chronically
Quinidine Barbiturates St. John's Wort Phenytoin Rifampin Griseofulvan Carbamazepine Chronic alcohol use |
|
|
P-450 interactions - Inhibitors (-)
|
Macrolides
Amiodarone Grapefruit juice Isoniazid Cimetidine Ritonavir Acute alcohol abuse Ciprofloxacin Ketoconazole Sulfonamides |
|
|
How to remember CYP450 inhibitors?
|
MAGIC RACKS
Macrolides Amiodraone Grapefruit Juice Isoniazid Cimetidine Ritonavir Acute alcohol abuse Ciprofloxacin Ketoconazole Sulfonamides |
|
|
Sulfa drugs - details?
|
Probenecid, Furosemide, Acetazolamide, Celecoxib, Thiazides, Sulfonamide antibiotics, Sulfasalazine, Sulfonylureas (Popular FACTSSS)
Patients with sulfa allergies may develop fever, UTI, pruritic rash, Stevens-Johnson syndrome, Hemolytic anemia, thrombocytopenia, agranulocytosis, and urticaria (hives). Symptoms range from mild to life-threatening. |
|
|
How to remember the sulfa drugs?
|
Popular FACTSSS
Probenacid Acetazolamide Celecoxib Thiazides Sulfonamide antibiotics Sulfasalazine Sulfonylureas |
|
|
Drug name - Category? Example?
-azole |
Antifungal
Ketoconazole |
|
|
Drug name - Category? Example?
-cillin |
Penicillin
Methicillin |
|
|
Drug name - Category? Example?
-cycline |
Antibiotic, protein synthesis inhibitor
Tetracycline |
|
|
Drug name - Category? Example?
-navir |
Protease inhibitor
Darunivir |
|
|
Drug name - Category? Example?
-triptan |
5-HT(1b/1d) agonists (migraine)
Sumatriptan |
|
|
Drug name - Category? Example?
-ane |
Inhalation general anesthetic
Halothane |
|
|
Drug name - Category? Example?
-caine |
Local anesthetic.
Lidocaine |
|
|
Drug name - Category? Example?
-operidol |
Butyrophenone (neuroleptic)
Haloperidol |
|
|
Drug name - Category? Example?
-azine |
Phenothiazine (neuroleptic, antiemetic)
Chlorpromazine |
|
|
Drug name - Category? Example?
-barbital |
Barbiturate.
Phenobarbital |
|
|
Drug name - Category? Example?
-zolam |
Benzodiazepine
Alprazolam |
|
|
Drug name - Category? Example?
-azepam |
Benzodiazepine.
Diazepam |
|
|
Drug name - Category? Example?
-etine |
SSRI
Fluoxetine |
|
|
Drug name - Category? Example?
-ipramine |
TCA
Imipramine |
|
|
Drug name - Category? Example?
-triptyline |
TCA
Amitriptyline |
|
|
Drug name - Category? Example?
-olol |
Beta antagonist
Propranolol |
|
|
Drug name - Category? Example?
-terol |
Beta-2 agonist
Albuterol |
|
|
Drug name - Category? Example?
-zosin |
alpha1-antagonist
Prazosin |
|
|
Drug name - Category? Example?
-oxin |
Cardiac glycoside (inotropic agent)
Digoxin |
|
|
Drug name - Category? Example?
-pril |
ACE inhibitor
Captopril |
|
|
Drug name - Category? Example?
-afil |
Erectile dysfunction
Sildenafil |
|
|
Drug name - Category? Example?
-tropin |
Pituitary hormone
Somatotropin |
|
|
Drug name - Category? Example?
-tidine |
H2 antagonist
Cimetidine |
|
|
Which lipid lowering medication class causes hypertriglyceridemia as a side-effect?
|
Bile acid-binding resins (cholestyramine, etc). Because the enterohepatic circulation is inhibited, de novo bile acid synthesis is upregulated roughly 10-fold. This causes increased hepatic production of VLDL and triglycerides as a side effect.
|
|
|
How is lactase deficiency similar to the mechanism of polyethylene glycol laxative?
|
Both cause osmotic diarrhea
|
|
|
What is the mechanism by which ACE-inhibitors can cause angioedema?
|
ACE breaks down bradykinin, when ACE inhibitors are used, they can cause dangerous accumulation of bradykinin which is a potent vasodilator and can cause significant angioedema when at high levels
|
|
|
What is the main way that nitroglycerine works to treat angina pectoris?
|
Venodilation --> venous pooling and decreased Left heart preload --> decreased oxygen demand
NOT aterial dilation (does have this effect at high levels but this woudl cause reduced coronary perfusion) |
|
|
How does Ziduvodine work?
|
It ends cDNA chain elongation by preventing the 3' --> 5' phosphodiester bond formation.
It has an azido group in the place of the 3' OH group found on normal thymidine molecules |
|
|
A patient experiences sexual side effects associated with SSRI therapy. WHat alternate antidepressant is a good fit?
|
Bupropion - does not have sexual side effects (thought to be because it works on NE and not really on Serotonin)
|
|
|
What portion of the EKG is changed with beta blockers?
|
PR interval elongation (slows AV conduction)
|
|
|
Of spironolactone and furosemide, which has been shown to improve survival in patients with CHF?
|
Spironolactone - NOT by its diuretic effect, but by its blockage of aldosterone
Aldosterone has neurohormonal effects on the heart that induce further remodeling and fibrosis. Furosemide has been shown to significantly improve symptoms, but has NOT been shown to improve overall survival. |
|
|
What pharmacokinetic property of methadone makes it a good substitute for patients with heroine addiction?
|
long half-life --> chronic suppression of withdrawal symptoms
|
|
|
Thiopental is used for anesthesia induction because of what property?
|
It rapidly accumulates in the brain within 1 minute, but then its plasma and brain concentrations drop rapidly as it redistributes into skeletal muscle and adipose tissue where it accumulates.
This makes it a perfect induction agent because the patient is rendered unconscious from the drug very rapidly, but then the drug quickly leaves the CNS> |
|
|
What is the first line drug for trigeminal neuralgia, and how does it work?
|
Carbamazepine - inhibits neuronal high-frequency firing by reducing the ability of sodium channels to recover from inactivation
|
|
|
What property of lidocaine and other class IB antiarrhythmics makes them good for arrhythmias following an ischemic event?
|
They are use-dependent - they do not bind avidly to resting sodium channels. Therefore, they are particualrly useful in binding and inhibiting ectopic pacemakers, which are constitutively activated.
|
|
|
What woudl propranolol's effect on renin secretion be?
|
By blocking Beta1 receptors on JGA cells, renin secretion is inhibited.
|
|
|
What would propranolol's effect on bradykinin be?
|
Beta blockers have no effect on ACE levels, so bradykinin would be unaffected.
|

