![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
103 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
T/F FRCA MCQ B [45].
The recurrent laryngeal nerve supplies: a) sensation below the cords b) the intrinsic muscles of the pharynx c) the cricothyroid muscle d) the inferior constrictor muscle e) the epiglottis |
A. T B. F C. F D. F E. F
The recurrent laryngeal nerve is a branch of the vagus nerve (Xth CN) that supplies motor function and sensation to the larynx (voice box) LEFT laryngeal nerve -is longer, -branches from the vagus nerve to loop under the arch of the aorta, posterior to the ligamentum arteriosum before ascending. RIGHT branch loops around the right subclavian artery -giving off several cardiac filaments to the deep part of the cardiac plexus BOTH -As it ascends in the neck it gives off branches, more numerous on the left than on the right side, to the mucous membrane and muscular coat of the oesophagus; branches to the mucous membrane and muscular fibers of the trachea; and some pharyngeal filaments to the superior pharyngeal constrictor muscle. The nerve splits into anterior and posterior rami before supplying muscles in the voice box — it supplies all laryngeal muscles except for the cricothyroid, which is innervated by the external branch of the superior laryngeal nerve. The recurrent laryngeal nerve enters the pharynx, along with the inferior laryngeal artery and inferior laryngeal vein, below the inferior constrictor muscle to innervate the Intrinsic Muscles of the larynx responsible for controlling the movements of the vocal folds. |
|
|
|
RB01
Thoracic epidural blockade to T5 using bupivacaine 0.5% with adrenaline 1:200,000 involves: A. Blockade of resistance vessels B. Blockade of capacitance vessels C. Blockade of cardiac sympathetic nerves, causing bradycardia D. Beta-adrenergic stimulation |
ALL TRUE
A True " Resistance: skin gets profound dilation. Autoregulated organs don't change blood flow much (eg kidney, heart, brain). Splanchic vasculature changes < muscle < skin. B True - venodilation > arteriodilation C True - Sympathetic blockade usually higher than sensory but it is highly variable - Cardiac accelerators are T1-4 D True - due to systemic absoption of adrenaline WITH SPINALS: Sympathetic block is approx 6 segments higher than sensory block. Temperature block is 2 segments higher than Touch block. |
|
|
|
RB02 ANZCA version [2004-Aug] Q97
Epidural sensory blockade to T2 in healthy adults is associated with each of the following EXCEPT A. bradycardia B. decreased circulating catecholamines C. dyspnoea D. vasodilatation E. raised PaCO2 |
ANSWER E
A. bradycardia - true: will affect sympathetic cardiac plexus B. decreased circulating catecholamines - true: Decreased sympathetic response to pain C. dyspnoea - true : commonly results from loss of intercoastal muscle function, resulting in diaphragmatic breathing D. vasodilatation - true : loss of sympathetic tone E. raised PaCO2 - false : loss of intercoasts results in a rise in PaCO2 which is sensed by chemoreceptors to adjust minute ventilation. Hypercapnia does not result as the diaphragm is spared and aveolar ventilation can be maintained. |
|
|
|
RB03
A caudal to L1 will anaesthetise: A. The perianal region B. Dome of the bladder C. Sole of the foot D. Medial side of the leg E. All of the above |
ANSWER A C D
A. TRUE : Perianal region S2-4 B. FALSE : Dome of bladder T10-L2 C. TRUE : Sole of foot L5/S1 D. TRUE : Medial side of leg L4 |
|
|
|
RB05 [Mar91]
The pressure in the epidural space: A. Lower in the lumbar region sitting then supine B. Is negative in the thoracic area due mainly to tenting of the dura by the needle C. Is higher in the thoracic region then lumbar when sitting D. ? |
ANSWER B
The epidural space is slightly positive, but large negative pressures are induced by tenting of the epidural space from the Tuohy needle and account for the rapid inward entry of saline using the hanging-drop method. |
|
|
|
RB06 [Apr96]
Epidurals in the elderly: A. Increased mass of drug required B. Decreased volume required C. Increased incidence of dural puncture D. Increased incidence of hypotension |
ANSWER B and D
A. FALSE : Factors affecting spread: *Major: dose (concentration x volume), age, thoracic > lumbar. *Minor: morbid obesity, pregnancy, position. *No effect: gender, height, weight (except as above), direction of needle, speed of injection, atherosclerosis, mode of injection (bolus vs fractionated) B. TRUE C. FALSE : Risk Factors for Post-Dural Puncture Headache * Beveled (Quincke) needle (pencil-point needles are preferable) * Larger needle * Female gender * Pregnancy * Younger age * History of headache prior to the dural puncture D. TRUE |
|
|
|
RB07
The spread of an epidural block depends on: A. Speed of injection of the local anaesthetic B. Mass of local anaesthetic C. The direction in which the solution is injected D. The age of the patient E. All of the above |
ANSWER D
PATIENT FACTORS 1. Age : conflicting data and highly debatable, data suggestive of increased spread by 3-8 segments, results include : reduced epidural fat, increased epidural compliance, increased permeability of dura, decrease in number of myelinated nerve fibres 2. Height : poor correlation 3. Weight and BMI : no correlation with thoracic epidurals but sight positive correlation with lumbar epidurals probably secondary to reduced epidural space 4. Pregnancy : no data on thoracic epidurals, but strong positive correlation with lumbar epidurals, due to engorgement of epidural veins resulting in reduced CSF volume -other similar factors include : ascities, large intra-abdominal tumors TECHNICAL FACTORS 1. Epidural site : suggestive that thoracic spread greater than lumbar (larger doses for lumbar), probably due to increased epidural fat in lumbar epidurals -no statistical difference between high, mid and low thoracic -high thoracic : caudal spread -mid thoracic : even distribution (mid shown to have higher negative pressure, maybe drawing solution into this space from high and low) -low thoracic : cephalad spread 2. Patient position and gravity -in lumbar : injection in the lateral position produces higher sensory block in dependent side -in lumbar : head down results in higher spread -no studies regarding position and gravity with thoracic -sitting : onset is quickers and blockade 102 segments greater than supine 3. Needle direction and catheter position -epidural injection through Touhy needle with different bevel orientation has little effect on spread -Threading an epidural catheter with the Tuohy needle rotated 45deg toward operative side has been shown to produce preferential sensory and motor block -orientating bevel caudad or cranially does not reliably predict final tip position -thoracic epidural have been shown to progressively withdraw an average of 1 cm during the first 3 days -optimal distance is 4-6cm, the longer the increased incidence of venous cannulation, paresthesia and inadequate analgesia |
4. Injection through needle vs catheter
-controversial -studies trending towards bolus injection through catheter results in greater spread and better analgesia 5. Epidural Catheter Design -single orifice vs multi orifice catheters -studies show multiorifice is superior : lower incidence of inadequate block and replacement; paresthesia -no differences in the frequency of replacement for subarachnoid placement or migration, immediate intravascular placement, vascular migration, or absence of any block -however, newer soft tip single orifice catheters have resulted in lower rates of venous cannulation and neuropraxia 6. Fractional vs bolus injection -large single bolus produced greater spread than smaller fractions -fractional injection resembles single shot injection when intervals are shorter -similarly when LOR technique is used, greater spread of blockade -however this correlation is poor and controversal 7. Speed of Injection -studies show speed of onset and greater perianal blockade with fast injection -however spread of blockade is still controversial LOCAL ANAESTHETIC 1. Total mass determines spread of sensory blockade (given in different volumes and concentrations) *** MOST IMPORTANT FACTOR 2. Additives -Bicarbonate : increased depth of sensory and motor block, reduced time to block but no difference in spread -Clonidine/adrenaline : faster onset, longer duration of sensory and motor blockade, no spread -Opiods : exert thier effects at dorsal horn, allows reduction in LA dose, enhancing analgesia, faster onset, but no effect on spread |
|
|
RB07b [Apr99]
Factors in spread of (thoracic) epidural EXCEPT (type A): A. Age B. Height C. Weight D. Volume of LA E. Pregnancy |
ANSWER A and E
|
|
|
|
RB07
The spread of an epidural block depends on: A. Speed of injection of the local anaesthetic B. Mass of local anaesthetic C. The direction in which the solution is injected D. The age of the patient E. All of the above |
ANSWER B and D
|
|
|
|
RB08
The pain of uterine contraction can be blocked by which of the following? A. Lumbar epidural B. Sacral epidural C. Uterosacral block D. Pudendal block |
ANSWER A
Uterine Contraction is carried with sympathetic fibres to T11/12 Blocked by : spinal, llumbar/low thoracic epidural, paravertebral, lumbar plexus block, paracerival block Second stage : pain carried by pudendal nerve Blocked by pudendal nerve block, spinal, sacral epidural |
|
|
|
RB09 [1988] [Aug91] [Mar92] [Aug92] [Mar93] [Aug93]
The nerve roots which usually conduct the pain of uterine contraction & cervical dilatation in the first stage of labour are: A. T8-T12 B. T10-L1 C. T11-L2 D. T12-L4 E. T10-L4 |
ANSWER B
|
|
|
|
RB10 [1987] [1988] [Mar93] [Apr96] [Jul97] [Apr98] (type K)
Paracervical block causes: 1. Foetal bradycardia 2. Prevents bearing down reflex 3. Foetal acidosis 4. Causes urinary retention |
ANSWER A and C
Paracervical block effectively relieved pain during first stage of labor but is rarely used due to high incidence of fetal asphyxia and poor neonatal outcome This may be related to uterine artery constriction or increased uterine tone |
|
|
|
RB11 [1985] [1987] [1988] [Mar91] [Aug91] [Aug93]
The third modality to be blocked with spinal anaesthesia is: A. Touch B. Pain C. Autonomic efferents D. Proprioception E. Motor |
ANSWER A
Temperature Pain Touch Proprioception Skeletal muscle tone |
|
|
|
RB13 [1988] [Aug91] [Mar92]
Spinal headache which is INCORRECT A. Occurs within 24 hours B. Neck pain C. Can be associated with intracranial haemorrhage D. Can be treated with IV caffeine E. Frontal headache |
ANSWER A
Post Dural Puncture Headache Symptoms -30-70% with known ADP will develop PDPH -rare for spinal to cause headache -severe, dull and non-trobbing headache -fronto-occiptial -aggrevated when sits up or strains -may be accompanied by nausea, vomiting, anorexia, visual distrubances (photophobia, blurred vision), audio disturbances (tinnitus) or neck stiffness Assessment / Investigations -the nature of the headache and should include the following: * time of onset * location * severity (? interference with daily activities) * postural element (i.e. Is the headache worse when sitting up / standing?) * visual / audio disturbances * analgesia given and if there has been some relief A full neurological assessment should also be performed. Management -Recognised dural puncture at time of epidural insertion. * If needle puncture, thread catheter into subarachnoid space. * If catheter puncture, leave catheter in CSF. * Ensure that the catheter / filter is clearly labelled as 'subarachnoid'. OR * Alternatively, attempt to re-site the catheter at another space. If this is difficult, there is uncertainty with correct placement or another puncture occurs, contact the anaesthetic consultant in charge. * subarachnoid boluses must be given by the anaesthetic registrar. * The PCEA or continuous infusion techniques should not be utilised as there is an increased risk for total spinal block. * The woman must be informed of the ADP and a management plan discussed with her. This management plan must be documented in the progress notes. |
For women where a PDPH has been identified, the following steps should be taken:
0-24 hours following dural puncture Conservative management is best as PDHP is self-limiting process 75% will resolve in first week 90% in 6 weeks 1. Encourage fluid intake Ensures that the rate of CSF production is adequate. It is thought that improvements in the ratio of CSF production to CSF leak will improve the outcome. Dehydration can result in a decrease in CSF production. Conversely, in the presence of adequate hydration, there is no evidence to suggest that overhydration will increase the production of CSF any further. 2. Bedrest Lying in the flat supine position is advised to lessen the severity of symptoms. If the headache is mild and does not interfere with daily activities, then bed rest is not necessary. 3. Analgesia Mild PDPH * paracetamol 4-6 hourly and a NSAID such as voltaren (unless contraindicated) Moderate - Severe PDPH * treat as with mild PDPH (above) plus an opioid (e.g. oxycodone and/or tramadol) * SC, IV or PR routes should be considered in the presence of nausea and vomiting. *use of caffeine is reported 500mg of caffeine sodium benzoate in one litre of fluid, infused over an hour -oral caffeine is only slightly better than placebo -vasoconstriction of cerebral vessls attentuates the vascular distention -avoid in pre-eclamptic patients who are have increased sensitivity to vasoconstrictiors 24-48 hours following dural puncture Women with a mild PDPH, which does not interfere with daily activities, then the above management should be continued. Where the PDPH is moderate-severe and is interfering with daily activities, an epidural blood patch should be considered and discussed with the women. An epidural blood patch should not be performed within the first 24 hours following dural puncture. The anaesthetic consultant in charge should be notified when an epidural blood patch is considered. |
|
|
RB14 [1986]
Dural puncture headache: A. Is common in females B. May refer to the neck C. Has a reduced incidence if the bevel of the needle is parallel to the fibers of the dura D. Requires a prophylactic blood patch E. May be associated with intracranial haemorrhage |
A. TRUE
B. TRUE C. FALSE : reduced incidence with smallest gauge and pencil point needles D. FALSE : Prophylactic epidural blood patch improved PDPH compared to no treatment (OR 0.11, 95% CI 0.02 to 0.64, one study), conservative treatment (OR 0.06, 95% CI 0.03 to 0.14, two studies) and epidural saline patch (OR 0.16, 95% CI 0.04 to 0.55, one study). However, prophylactic epidural blood patch did not result in less PDPH than a sham procedure (one study). |
|
|
|
RB15b ANZCA version [2001-Aug] Q148
Following accidental dural puncture associated with an epidural for a Caesarean Section a patient developed a post-dural puncture headache. Epidural blood patch 1. would be more effective if performed within 24 hours of dural puncture 2. should be delayed till residual neuraxial block has resolved completely 3. will preclude the patient from epidural anaesthesia for future Caesarean sections 4. will be more successful if followed by a period of bed rest, of at LEAST 2 hours duration |
1. FALSE : most will resolve spontaneously, EBP is indicated if headache continues beyond 48 hours and is severe enough to limit activities of daily living despite analgesia
2. TRUE 3. FALSE 4. TRUE |
FACTORS IMPROVING EPB FOR PDPH
Greater blood volume used 15-20mls Recombinant bed rest for 4 hours Do not squat or squeeze |
|
|
Differentials for PDPH
|
Meningitis
Central venous sinus thrombosis (CVST) Spinal hematoma Cortical/cerebral vein thrombosis Intracranial subdural hematoma Benign intracranial hypertension Migraine Caffeine-withdrawal headache |
|
|
|
Risk Factors for PDPH
|
Risk Factors for Post-Dural Puncture Headache
* Beveled (Quincke) needle (pencil-point needles are preferable Sprotte, GM ,Whitacre) * Larger needle * Female gender * Pregnancy * Younger age * History of headache prior to the dural puncture Possibly *Operator experience *Amount of CSF removed No effect *recumbent positioning for 30 minutes after LP |
|
|
|
How would you perform an EBP?
|
Prepare the patient by:
1. Explaining the technique, hazards and anticipated success rate. 2. Obtaining consent for the procedure. 3. Pre-medicating if necessary. 4. Starting an intravenous infusion of crystalloid. 5. Positioning in the left lateral, fully-flexed position. The EBP is, preferably, a two-operator technique. Both operators should scrub, gown and glove as is standard in the particular institution. Operator 1. 1. Cleans and drapes the patient's back using a standard epidural kit and technique, 2. Identifies the site of original puncture and locates the epidural space using a standard technique. Operator 2. 1. At the same time as operator 1 is prepping the back, the second operator cleans and drapes the antecubital area of (usually) the left (downside) arm. A second epidural/spinal kit and drapes containing a 20cc glass syringe with 22G sterile straight or butterfly needle is ideal for the task. 2. Once the epidural space is located by operator 1, the second operator, using a rigidly aseptic technique, performs a venepuncture, withdraws 22ml of blood, removes the needle from the syringe, hands the syringe to the first operator (without breaching the integrity of the sterile fields) and applies pressure and a sterile dressing to the venepuncture site. How should the blood should be injected? 1. Inject the blood slowly until either, the patient complains of tightness in the buttocks, lower back or thighs (usually when 12 to 15ml are injected) (11) or, until 20 ml is injected. 2. Withdraw the needle, apply a sterile dressing and turn the patient to the supine position. 3. Inject the residual blood through a fresh, sterile needle into a blood culture bottle and send to bacteriology for culture and antibiotic sensitivity. Recovery orders : 1. Place a pillow under the mother's knees. 2. Nurse her supine for four hours. Discharge orders: 1. not to carry anything heavier than the baby for 2-3 weeks, 2. to squat rather than bend when picking items in a low position, 3. to avoid excessive straining, - all of which can cause 'patch blow-out' with return of the PDPH. 4. To report pyrexia, back or radicular pain, return of PDPH or other untoward symptoms immediately. |
|
|
|
RB15a [1986] [Aug93] [Mar94] [Aug94] [Aug99] [Jul00]
An epidural blood patch: A. Better results if rest in bed for several hours after patch B. May cause neck and back pain C. Is reported to be very effective D. Always reduces the effect of the next block because obliterates space E. ?must wait 24 hours before patching F. Wait until resolution of sensory blockade |
A. TRUE
B .TRUE C. TRUE D. FALSE E. FALSE F. TRUE |
|
|
|
RB15c ANZCA version [2006- Mar] Q108
Epidural blood patch for severe post-dural puncture headache A. is contraindicated in patients with Acquired Immunodeficiency Syndrome (AIDS) B. has NOT been shown to be associated with a higher success rate if performed more than 24 hours after dural puncture C. is associated with a higher success rate if more than 20 ml of blood is used D. is rarely associated with back pain during injection E. is most effective when given immediately following accidental dural puncture |
A. FALSE - HIV NOT a contraindication, unless active bacterial or viral infection
B. FALSE - see above C. TRUE - best results with 20-30ml blood D. FALSE - it's always associated since that's your indication to stop injecting more blood! E. FALSE - More effective if delayed by >24 hours |
|
|
|
RB16 [Mar91] [Aug92]
Postdural puncture headache: which of the following have (NOT) been reported to help? A. Dopamine B. Saline C. Blood D. Binders E. IV caffeine F. Bed Rest |
ANSWER A
|
|
|
|
RB18 [Mar93] [Aug93] [Apr97]
The incidence of spinal headache may be reduced by: A. The use of Quincke point spinal needles B. Use of the paramedian approach rather than midline C. Strict bed rest for 24 hours D. Alignment of the bevel of the spinal needle transverse to the long axis of the spine E. .....?? facial n block ?? |
ANSWER B
Entering the dura at an angle (either paramedian, cephalad angulation, use of fine guage needles which bend more in the interspinous ligaments) all decrease risk. Theorie is that it creates a flap valve defect which self-seals. |
|
|
|
SF What increases the risk of threading an epidural catheter into a blood vessel?
A. not doing a CSE B. injecting saline prior to threading catheter C. LOR to saline instead of air D. paramedine instead of midline approach E. sitting position instead of lateral |
ANSWER E
A - it is thought that CSE decreases risk by ensuring catheter is midline, but no documented research. B : LOR NS decreases risk by distenting epidural space. OR 0.45 LOR NS vs LOR air. C : See B D : no difference (only 1 RCT showing this, ?insufficient data) E : epidural vein engorgement/ distention is greater when sitting instead of lateral position. Risk of epidural vein cannulation is higher in sitting position. Anesth Analg 2009;108:1232–42 : Metanalysis of 7 techniques in obstretric women 1. position : supine vs sittting OR 0.53 6 RCT 2. approach : paramedian vs midline no difference 1 RCT 3. touhy size : 16 vs 18 no difference 1 RCT 4. LOR technique : NS vs air, OR 0.45 8 RCT 5. oriface catheter : single vs multi OR 0.64 5 RCT 6. wire embbeded catheter 1 RCT 7. limiting catheter insertion to 6cm, >7cm OR 0.27 3 RCT |
|
|
|
TMP-144 [Apr08] Q127
You are performing epidural anaesthesia on an adult patient. To minimize the chance of inserting the epidural catheter into a blood catheter into a blood vessel you could: A. avoid using a combined spinal-epidural technique B. establish loss-of-resistance with saline rather than air C. inject saline prior to threading the catheter D. perform the procedure in the sitting rather than the lateral position E. use a midline rather than a paraspinous (paramedian) approach |
ANSWER B and C
|
|
|
|
RB64b ANZCA version Apr08 Q121
Regarding thoracic epidural analgesia for acute post-operative pain: A. it has NO role in improving preservation of total body protein after upper abdominal surgery B. opioids alone via the thoracic epidural provide significantly better analgesia than systemic opioids alone C. there is NO effect on the incidence of postoperative myocardial infarction D. the addition of adrenalin (epinephrine) to a local anaesthetic mixture has NO measurable benefit E. using local anaesthetics improves bowel recovery after abdominal surgery |
ANSWER E
A - FALSE : The combination of thoracic epidural analgesia with local anaesthetics and nutritional support leads to preservation of total body protein after upper abdominal surgery (U) (Level II). B - FALSE : epidural better than PCA except when epidural using hydrophilic opioids only C - FALSE : Thoracic epidural analgesia extended for more than 24 hours reduces the incidence of postoperative myocardial infarction D - FALSE: Addition of adrenaline improves block E - TRUE: reduced duration of ileus after colorectal surgery. |
|
|
|
RB64 ANZCA version Jul07 Q142
Regarding the use of epidurals for post-operative analgesia, A. epidural analgesia following bowel surgery may increase the risk of anastomotic leakage B. epidurals have similar analgesic efficacy to intravenous PCA (patient controlled analgesia) with morphine C. studies show the overall failure rate of epidurals to be less than 2% D. the incidence of pulmonary infections with epidural local anaesthetics is LESS than that with parenteral opioids E. the incidence of significant epidural haematoma is NOT affected by concomitant anti-thrombotic therapy |
ANSWER D
A. FALSE : there have been numerous case reports, however, there is no statistically significant evidence from the small RCT's available in bowel surgery. Thoracic epidural analgesia is protective for anastomotic leakage after oesophagectomy. B. FALSE : epidurals provide superior analgesia as compared to PCA C. FALSE : large prospective study showed 22% premature termination of epidural treatment D. TRUE : Epidural local anaesthetics improve oxygenation and reduce pulmonary infections and other pulmonary complications compared with parenteral opioids E. FALSE : Anticoagulation is the most important risk factor for the development of epidural haematoma after neuraxial blockade |
|
|
|
RB A thoracic epidural inserted for pain relief:
A. Allows earlier return of bowel function B. Prevents wasting of total body protein C. Does NOT reduce the incidence of MI D. Epidural opioids alone provide better analgesia than systemic opioids alone E. Addition of adrenaline significantly reduces local anesthetic dose requirement |
ANSWER A
A. TRUE : Level 1 evidence for thoracic but not for lumbar B. FALSE : Level 1 evidence that thoracic epidurals AND nutritional support C. FALSE : High thoracic epidural analgesia used for coronary artery bypass graft surgery reduces postoperative pain, risk of dysrhythmias, pulmonary complications and time to extubation when compared with IV opioid analgesia D. FALSE : For all types of surgery, epidural analgesia provides better postoperative pain relief compared with parenteral (including PCA) opioid administration (S) (Level I [Cochrane review]); EXCEPT epidural analgesia using a hydrophilic opioid only (N) (Level I). E. FALSE : the addition of adrenaline improves analgesia, prolongs motor and sensory block, but has no documented effect in reducing local anaesthetic dose requirement |
|
|
|
RB Man with peripheral vascular disease, post unilateral lumbar sympathectomy injection - most likely Cx:
A. orthostatic hypotension B. genitofemoral nerve neuralgia C. ?L2-L4 paraesthesia D. psoas haematoma E. |
ANSWER B
Lumbar Sympathectomy Anatomy -sympathetic outflow to lower extremities originates from spinal cord segments T10-L3 and conveys to L1-4 ganglia Physiology -abolishing basal and reflex constriction of arterioles and precapillary sphinters -flow increase 20-200% has been observed -maximal vasodilation noted immediately after, tapers within 5-7days, resting vasomotor tone returns after 6 months (due to incomplete denervation, cross over, hyper reactivity to circulating catecholamines -altered pain transmission, decreases noxious stimulus Indications -inoperable arterial occlusive disease -urogential pain -renal colic -complex regional pain syndromes -frostbite -stump pain, phantom limb pain Contraindications Patients on anticoagulant therapy Hemorrhagic disorder Allergies to medications injected Local infection Local neoplasm Local vascular anomalies Method Equipment : Sterile sutff, long needle, XR image intensifier, La or phenol Positioning : Prone or Lateral Technique : 1. needle inserted 10-12cm from middle aiming needle at L2 vertebral body 2. when needle strikes bone, walk need off vertebral body anteriorly to slide of antero-lateral surface of the vertebral body 3. contrast injection should be easy after aspiration to exclude intravascular placement, spread up and down vertebral column should be demonstrated (between vertebral body and psoas muscle) 4. 15-20 injected Complications •Genitofemoral Neuralgia occurs in 5% of all blocks. This causes pain in the L1 groin area and is thought to be due to bruising of the L1 nerve root by the needle passing by it. More than 90% of cases recover spontaneously after 6 weeks. Treatment with amitriptyline and gabapentin / pregabalin can help greatly. *Bleeding due to aorta and inferior vena cava injury by the needle. •Intravascular injection (should be prevented by checking the needle position with radio-opaque dye). •Upper abdominal organ puncture with abscess / cyst formation. *Paraplegia from injecting phenol into the arteries that supply the spinal cord (should be prevented by checking the needle position with radio-opaque dye). |
|
|
|
RH Patient has IDDM and stable angina. Present for cataract extration. Surgeon was not willing to do it with topical LA, but you accidently block the WRONG eye. After explanation and apologising to pt, what do you do next?
A. cancel surgery and re schedule on a day that is convenient to patient B. cancel surgery, do not rebook case until an incident form has been processed and you are aware of the outcome of the enquiry C. give a GA D. block the other eye (topical) and continue (edit: i think this stem was proceed with eye block to correct side - definitely a block I agree) E. proceed under topical LA (edit: convince the surgeon to do the correct eye with topical anaethesia) |
ANSWER A
No references, but seems the most logical approach |
|
|
|
37. Globe perforation with eye blocks is most likely with:
A. Axial length <25mm B. Medial canthus peribulbar injection C. Inferotemperal peripulbar injection D. Age < 40 years E. Sub-Tenons |
ANSWER C
Unintentional globe perforation and rupture is the most devastating complication of eye blocks -poor prognosis, especially when the diagnosis is delayed -incidence 1 in 350 and 7 in 50,000 cases Main risk factors include -inadequate experience of the physician -highly myopic eye (axia length < 26mm) -injection temporal or inferior margin (peri and retrobulbar) |
|
|
|
RH Retrobulbar block is least likely to block which muscle?
A. Lateral rectus B. Superior oblique C. Levator palpebrae superioris D. Inferior rectus E. Medial rectus |
ANSWER B
All nerves except the trochlea nerve (CN IV) pass through the muscle cone. Therefore with retrobulbar blocks, the superior oblique is spared (incomplete akineses). |
|
|
|
RB (2008 August Q106) You are seeing a 60yo man in the pre-anaesthetic clinic before his right total knee replacement. He weighs 70kg and apart from his osteoarthritis is fit and well. You discuss with him the options of a general anaesthetic with multi-modality analgesia and enoxaparin postoperatively as well as the option of an epidural for both the anaesthetic and post operative pain management. What is incorrect regarding the epidural?
A. It will shorten his hospital stay and accelerate his rehabilitation B. It will give him better pain relief particularly for the CPM machine (the continuous pain machine) C. It will reduce his risk of myocardial ischaemia D. There will be little difference in his risk of thromboembolism. E. If he has no sedation, his risk of post-operative delirium and cognitive impairment will be reduced |
ANSWER C
A. FALSE : B. FALSE : After hip or knee replacement, epidural analgesia provides better pain relief than parenteral opioids, in particular with movement (Choi et al, 2003 Level I). C. TRUE : Only thoracic epidruals have been should to reduce the risk of AMI D. FALSE : There is little difference in risk for thromboembolism E. FALSE : |
|
|
|
RB63 (Q133 Aug 2008) Aug10
When hearing loss occurs following spinal anaesthesia, it is usually in which of the following frequency ranges: A. 125 - 1000 Hz B. 1500 - 3000 Hz C. 3500 - 5500 Hz D. 6000 - 10000Hz E. > 11000Hz |
ANSWER A
Hearing loss after spinal anesthesia at 125-1000Hz A decrease in CSF pressure may lead to an endolymphatic hydrops. No relation to age, weight, height, blood pressure. No association with post-dural puncture headache. |
|
|
|
RB Effect of Injecting 5 mL of saline into the epidural space:
a. increase incidence of patchy block b. decreased risk of epidural vein catheterisation c. no effect d. increased ease of threading catheter e. ? decreased effectiveness of block |
ANSWER B
A&A August 2007 (105, 2, 460-464) -Reduced risk of cannulation -Reduced risk of patchy block -Reduced time of onset -Easier to thread |
|
|
|
RB PDPH.
a. IV caffeine treatment used to relieve symptoms. b. Is usually frontal headache c. Bed rest for 24 hrs is beneficial d. no use if blood patch done after 48 hrs. e. usually manifests within first 4 hrs. |
ANSWER A
A. TRUE B. FALSE : occipital to frontal C. FALSE : no benefit in preventing or treating PDPH, but symptomatic relief D. FALSE E. FALSE : usually 24-36 hours |
|
|
|
NN (Q85 Aug 2008) The left recurrent laryngeal nerve
A hooks around the arch of the aorta anterior to the attachment of the ligamentum arteriosum B passes under cover of the lower border of the inerior constrictor muscle before entering the larynx C supplies the cricothyroid muscle D supplies sensation to the whole of the laryngeal mucosa on the left side E contains motor fibres derived from the spinal root of the accessory nerve |
ANSWER E
A. FALSE : posterior to the attachment of ligamentum arteriosim B. TRUE C. FALSE : supplies all the muscles of the larnyx except the cricothyroid D. FALSE : supplies the laryngeal mucosa below the vocal cords (above is the superior laryngeal nerve) E. FALSE : motor fibres are derived from the vagus nerve |
|
|
|
NL04 [1986] [Mar94] [2004-Aug] Q41, [2005-Apr] Q62 [Mar06] [Jul06]
The sciatic nerve supplies the following muscles EXCEPT A. biceps femoris B. semitendinosus C. semimembranosus D. gluteus maximus E. adductor magnus |
ANSWER D
Articular Branches -arise from the upper part of nerve to supply the hip-joint Muscular Innervation 1. Biceps Femoris 2. Semitendinosis 3. Semimembranosus 4. Adductor Magnus Divides into 1. Tibial Nerve (all muscles of foot except extensor digitorum brevis) 2. Common Fibular Nerve Sensory Supply 1. Posterior aspect of the thigh and gluteal regions 2. Entire lower leg except the medial aspect |
|
|
|
NN32 [Apr07] [Jul07]
Stellate ganglion is located: A. At the level of the body of C6 (spine of C6) B. Posterior to the brachial plexus sheath C. Anterior to the dome of the pleura D. Anterior to the thoracic duct E. Anterior to scalenius anterior |
ANSWER E
Anatomy -ganglion formed by the fusion of the inferior cervical and the first thoracic ganglion -it is present 80% of subjects -located anterior to vertebral body of T7, above the neck of the 1st rib Relations of stellate ganglion *Anterior skin and subcutaneous tissue, the sternocleidomastoid and the carotid sheath. The dome of the lung lies anterior and inferior to the ganglion. *Medial The prevertebral fascia, vertebral body of C7, oesophagus and thoracic duct lie medially. *Posterior the longus colli muscle, anterior scalene muscle, vertebral artery, brachial plexus sheath and neck of the first rib. Indications *Pain syndromes -Complex regional pain syndrome type I and II -Refractory angina -Phantom limb pain -Herpes zoster -Shoulder/hand syndrome -Angina *Vascular insufficiency -Raynaud's syndrome -Scleroderma -Frostbite -Obliterative vascular disease -Vasospasm -Trauma -Emboli Contraindications -Coagulopathy -Recent myocardial infarction -Pathological bradycardia -Glaucoma |
Technique
Equipment : image intensifier, resus equipment, assistant Position : supine with neck slightly extended and mouth open to relax neck muscles Landmarks : trachea, carotid sheath, sternocleidomastoid, cricoid cartilage and Chassaignac's tubericle Method 1. Retract SCM and carotid artery lateral 2. Palpate Chassaignac'ss tubercle (anterior tubercle of the transverse process of the 6th cervical vertebrae) 3. skin is pressed firmly onto the tubercle to reduce distance and push apex of lung out of the path of needle 4. needle is inserted onto the tubercle then redirectly medially and inferiorly towards the body of C6 until the body is contacted 5. withdraw 1-2mm to move needle out of belly of longus coli muscle 6. confirm position using fuoroscopy, contrast should spread cephalad and caudad along vertebral body 7. Aspirate and inject LA 3ml at a time looking for inadvertent arterial injection, total of 10-15ml 8. Onset of Horner's indicates successful block Complications *Misplaced needle -Haematoma from vascular trauma -Carotid trauma -Internal jugular vein trauma -Neural injury -Vagus injury -Brachial plexus roots injury -Pulmonary injury -Pneumothorax -Haemothorax -Chylothorax (thoracic duct injury) -Oesophageal perforation *Spread of local anaesthetic -Intravascular injection: -Carotid artery -Vertebral artery -Internal jugular vein *Neuraxial/brachial plexus spread: -Epidural block -Intrathecal -Brachial plexus anaesthesia or -injury (intraneural injection) *Local spread: -Horseness (recurrent laryngeal nerve) -Elevated hemidiaphragm (phrenic nerve) *Infection -Soft tissue (abscess) -Neuraxial (meningitis) -Osteitis |
|
|
Interscalene Nerve Block
|
Interscalene block is
-brachial plexus block at the level of the trunks at C6 -surgical anaesthesia for shoulder, upper arm and forearm * Indications: Shoulder, arm, elbow surgery *Environment -airway and resus equipment in case of LA toxicity -trained anaesthetic assistent *Positioning -supine to 20deg head up -head turned slightly to contralateral side -arm flexed and rest over abdomen (remove casts prior) * Landmarks: -Sternal notch -Clavicle -Clavicular head of the sternocleidomastoid muscle -Mastoid process -External jugular vein *Needle placement * Nerve stimulation: Twitch of the pectoralis, deltoid, arm, forearm, or hand muscles at 0.2-0.4 mA current * Pectoralis muscle * Deltoid muscle * Triceps muscles * Biceps muscle * Any twitch of the hand or forearm * Local anesthetic: 35-40 mL |
Trouble shooting
1. Local twitch of the neck muscles -direct stim of ant scalene or SCM -needle to anterior and medial to plexus -withdraw needle and redirect 15deg posteriorly 2. Contact of bone 1-2 depth, no twitches -needle hit transverse process, too posterior -redirect 15deg anteriorly 3. Twitches of diaphragm -phenic nerve, too anterior -redirect 15deg posterioly 4. Arterial blood, puncture of carotid artery -insertion too anterior -withdraw, apply pressure for 2-3 minutes -reinsert 1-2cm posterioly 5. Twitch of scapula -Twitch of the serratus anterior muscle; stimulation of the thoracodorsal nerve -Needle position is posterior/deep to the brachial plexus -withdraw and reinsert anteriorly 6. Trapezius muscle twitches -Accessory nerve stimulation -withdraw and reinsert Complications and How to Avoid Them Infection * A strict aseptic technique is used Hematoma * Avoid multiple needle insertions, particarly in anticoagulated patients * Keep a 5-minute steady pressure when carotid artery is inadvertenly punctured * Use a single-shot needle to localize the brachial plexus in patients with difficult anatomy * In the absence of spontaneous bleeding, the use of anticoagulant therapy should not be regarded as a contraindication for this block Vascular puncture * Vascular puncture is not common with this technique * Steady pressure of 5 minutes duration should be maintained when the carotid artery is punctured (rare) Local anesthetic toxicity * Systemic toxicity due to absorbtion of local anesthetic after intrascalene blockade is rare * Systemic toxicity most commonly occurs during or shortly after injection of local anesthetic; this is most commonly caused by an inadvertent intravascular injection or channeling or forcefully injected local anesthetic into small veins or lymphatic channels cut during needle manipulation * Large volumes of long-acting anesthetic should be reconsidered in older and frail patients * Careful and frequent aspiration should be performed during the injection * Avoid forceful, fast injection of local anesthetic Nerve injury * Never inject local anesthetic when pressure on injection is encountered * Local anesthetic should never be injected when patient complains of severe pain or exhibits a withdrawal reaction on injection Total spinal anesthesia * When stimulation is obtained with current intensity of <0.2mA, the needle should be pulled back to obtain the same response with the current >0.2mA before injecting local anesthetic to avoid injection into the dural sleeves and the consequent epidural or spinal spread * Never inject local anesthetic when pressure on injection is encountered Horner's syndrome * Occurence of ipsilateral ptosis, hyperemia of the conjuctiva, and nasal congestion is common and it is dependent on the site of injection (less common with the low intrascalene approach) and total volume of local anesthetic injected; the patients should be instructed on the occurence of this syndrome and reassured about its benign nature Diaphragmic paralysis * Invariably present; avoid interscalene blockade or the use of a large volume of local anesthetic in patients who have severe, chronic respiratory disease and use accessory respiratory muscles during breathing at rest |
|
|
Draw a transverse view of the neck - interscalene block
|
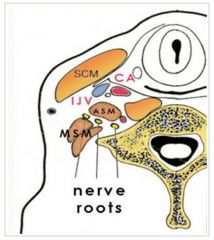
|
|
|
|
Draw an illustration of the sono-anatomy of the brachial plexus for an interscalene block.
|
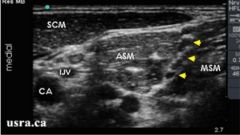
Arrowheads = nerve roots
ASM = anterior scalene muscle CA = carotid artery IJV = internal jugular vein MSM = middle scalene muscle SCM = sternocleidomastoid muscle Vertebral artery is deep |
|
|
|
NA11b ANZCA version [2004-Apr] Q41, [Mar06] Q33, [Jul06] Q60
The segmental nerve supply to the renal pelvis and the ureter gives an anatomical basis for the surface representation of the pain of renal colic. The segments concerned are A. T11 and T12 B. L1 C. L1 and L2 D. T11, T12, L1 and L2 E. T12 and L1 |
ANSWER D
KIDNEY Sympathetic preganglionic from T8-L1 converge onto celiac plexus and aorticorenal ganglia; post ganglionic to the kidney Parasympathetic from the Vagus nerve Pain T10-L1 URETER Sympathetic from the T10 to L2, post ganglionic fibres to aorticorenal and superior and inferior hypogastric plexuses Parasympathetic from the S2-S4 Pain T10-L2 BLADDER/URETHRA Sympathetic from T11 to L2 converge on the superior hypogastric plexus and supply the bladder through the right and left hypogastric nerves Parasympathetic from S2-S4 and form the pelvic parasympathetic plexus Pain dome : T11-L2 Neck S2-S4 Prostate Sympathetic T11-L2 Parasympathetic S2-S4 Pain T11-12, S2-4 Penis Sympathetic L1 and L2 Parasympathetic S2-4 Pain S2-4 from the pudendal nerve Scrotum is innervated anteriorly by the ilioinguinal and genitofemoral nerve (L 1 and L2), posteriorly by perineal branches of the pudenal nerve (S2 and S4) Testes (similar to kidneys where the begin during fetal development) Sympathetic T10-L2 Pain T10-L1 |
|
|
|
NH30 ANZCA version [2005-Apr] Q140, [2005-Sep] Q77, [Mar06] Q31
The muscles of the upper eyelid receive a somatic nerve supply from the A. oculomotor nerve and a parasympathetic supply from the superior vagus nerve B. oculomotor nerve and a sympathetic supply from the superior cervical ganglion C. ophthalmic division of the trigeminal nerve and a parasympathetic supply from the superior vagus nerve D. ophthalmic division of the trigeminal nerve and a sympathetic supply from the superior cervical ganglion E. ophthalmic division of the facial nerve only |
ANSWER B
The superior branch (of CNIII, the oculomotor) passes lateral to the optic nerve to supply the superior rectus muscle and levator palpebrae superioris; the inferior branch supplies three muscles: the medial rectus, the inferior rectus and the inferior oblique" (Ellis) and "The clinical manifestation of this is a Horner’s syndrome: the pupil is small (paralysis of the dilator pupillae), there is ptosis (paralysis of the sympathetic supply to levator palpebrae) |
|
|
|
NL04 ANZCA version [2004-Aug] Q41, [2005-Apr] Q62, [Mar06] Q42, [Jul06] Q24 (Similar version reported in [1986] [Mar94]) [Apr08] [Aug08] [Aug10]
The sciatic nerve supplies the following muscles EXCEPT A. biceps femoris B. semitendinosus C. semimembranosus D. gluteus maximus E. adductor magnus |
ANSWER D
The branches of the sciatic nerve can be grouped into the following (from Ellis p200): 1 Muscular to: BASS * (a) bicep femoris * (b) adductor magnus * (c) semitendinosis * (d) semimembranosis. 2 Articular to: * (a) the hip joint. 3 Terminal to: * (a) common peroneal (lateral popliteal) nerve; * (b) tibial (medial popliteal) nerve. |
|
|
|
NL08 [Aug91], [Mar06] Q80
The sural nerve A. Is a branch of the posterior tibial nerve B. Supplies the skin of the anterior two thirds of the sole of the foot C. Lies anterior to the lateral malleolus at the ankle D. Reaches the foot in contact with the short saphenous vein E. Supplies the small muscles of the foot |
SURAL NERVE
Description : Purely sensory nerve supplying the sensation to the lateral foot Branch of the Tibial nerve Follows the long saphenous vien |
|
|
|
NS15b ANZCA version [2003-Apr] Q28, [2003-Aug] Q68, [2005-Sep] Q52, [Mar06] Q6
Anatomical features of the spinal cord do NOT include A. an anterior median fissure and a posterior median septum B. thirty-two pairs of spinal nerves C. a filum terminale ending at the coccyx D. four to six spinal arteries arising from the posterior inferior cerebellar arteries E. the anterior spinal artery arising from the vertebral arteries |
ANSWER B
* A. an anterior median fissure and a posterior median septum - true: "The spinal cord presents an anterior median fissure and a shallow posterior median sulcus from which a glial posterior median septum extends about halfway into the substance of the cord." * B. thirty-two pairs of spinal nerves - false: "There are 31 pairs of spinal nervesaeight cervical, 12 thoracic, five lumbar, five sacral and one coccygeal. Each is formed by the fusion of an anterior and posterior spinal root." * C. a filum terminale ending at the coccyx - true: "Below, the spinal cord tapers into the conus medullaris, from which a glistening thread, the filum terminale, continues down to become attached to the coccyx." * D. four to six spinal arteries arising from the posterior inferior cerebellar arteries - unsure so make your own decision: "The posterior spinal arteries comprise one or two vessels on either side derived from the posterior inferior cerebellar arteries. They supply the posterior grey and white columns on either side. These arteries are reinforced serially by spinal branches of the vertebral, deep cervical, intercostal, lumbar, ilio-lumbar and lateral sacral arteries; the lower branches being responsible for the blood supply of the cauda equina." * E. the anterior spinal artery arising from the vertebral arteries - true: "The anterior spinal artery is a midline vessel lying on the anterior median fissure and is formed at the foramen magnum by the union of a branch from each vertebral artery." |
|
|
|
NT34b ANZCA version [Apr99] [2002-Aug] Q75, [2004-Apr] Q89, [Mar06] Q93, [Jul06] Q94
The intercostal nerves A. arise as the sensory fibres of the anterior primary rami from their spinal segments B. give off a lateral cutaneous branch at the angle of the rib C. lie in the subcostal groove in only 50% of people D. lie between the intercostalis intimi and the pleura E. are enclosed in a dural sheath from their origin to the angle of the rib |
ANSWER E
A. FALSE : mixed sensory and motor nerve B. FALSE : the collateral motor branch is given off at the angle of the rib, while the lateral cutaneous branch arises in the mid axillary line C. FALSE : found in the classical subcostal position in 16.6%, in the midzone in 73% and in the inferior supracostal position in 10%. D. FALSE : Nerves lie between intermediate and inner most layers, ie between internal and transversus or intimi E. TRUE : the dura occasionally extends out along the intercostal nerve a variable distance before it adheres to the nerve as the neurolemma or nerve sheath' thus accounting for the rare occurrence of spinal anaesthesia following intercostal blocks. |
|
|
|
NV38b ANZCA version [2005-Apr] Q65, [Mar06] Q41, [Jul06] Q28, [Apr07]
The median nerve A. can be blocked at the elbow immediately lateral to the brachial artery B. can be blocked at the wrist between palmaris longus and flexor carpi ulnaris C. can be blocked at the wrist medial to flexor carpi ulnaris D. is formed from the lateral, medial, and posterior cords of the brachial plexus E. provides sensation to the radial half of the palm |
ANSWER E
MEDIAN NERVE Definition : mixed sensory and motor nerve of the brachial plexus Spinal nerve : C5-8, T1 * C5 to C7 roots from lateral cord of brachial plexus * C8 and T1 roots from medial cord of brachial plexus Anatomy 1. Inputs from the lateral cord and medial head of the medial cord 2. unite to form the median nerve in front of the 3rd part of the axillary artery 3. descends through the arm lateral to the brachial artery, cross at the midde point of the upper arm, then medial to the brachial artery 4. crosses in front of the elbow, lying on brachialis, passing medial to the brachial artery 6. dives between two head of pronator teres separating from ulnar artery 7. descends through the forearm between flexor digitorum superficialis (FDS) and flexor digitorum produndus (FDP) 8. emerging between flexor carpi radialis (lateral) and flexor digitorum and palmaris longus (medial) 9. passes through carpal tunnel under the flexor retinaculum SUPPLIES 1. Muscular branches Superficial group: * Pronator teres * Flexor carpi radialis * Palmaris longus Intermediate group: * Flexor digitorum superficialis muscle Deep group: * Flexor digitorum profundus (only the lateral half) * Flexor pollicis longus * Pronator quadratus Hand : LOAF * Lumbrical 1 and 2 * Opponens Pollicis * Abductor pollicus brevis * Flexor pollicus brevis (also innervated by ulnar nerve) 2. Cutaneous branches : anterior aspects of radial 3 digits and skin over the dorsal aspect of the distal phalanges 3. Articular branches : to elbow and wrist TESTS Motor : Opposition and flexion of the thumb are lost (LOAF) Sensory : Palm - 3 1/2 Fingers |
|
|
|
NV45 [July06] Q15 ANZCA Version
At the wrist joint A. The median nerve lies between the tendons of palmaris longus and flexor carpi radialis B. The median nerve lies medial to the tendon of flexor carpi ulnaris C. The radial artery is usually palpable just medial to the tendon of flexor carpi radialis D. The ulnar artery and nerve enter the hand by passing deep to the flexor retinaculum |
ANSWER A
A. TRUE : at the wrist, the median nerve lies between the tendons of flexor carpi radialis (lateral) and palmaris longus (median) + flexor digitialis superficialis B. FALSE : very well lateral C. FALSE : The radial artery lies medial to BRACHIORADIALIS but lateral to FCR. D. FALSE Contents of the flexor retinaculum 1. 9 flexor tendons * flexor digitorum profundus (four tendons) * flexor digitorum superficialis (four tendons) * flexor pollicis longus (one tendon) 2. 1 nerve : median nerve Structures which pass superficially to flexor retinaculum 1. Palmaris longus 2. Ulnar artery 3. Ulnar nerve 4. Palmar cutaneous branch of the ulnar nerve 5. Palmar cutaneous branch of the median nerve |
|
|
|
NZ03 ANZCA version [2003-Aug] Q123, [2004-Apr] Q79, [Jul06] Q79, [Apr07] Q123, [Mar10]
Pre-ganglionic sympathetic fibres pass to the A. otic ganglion B. carotid body C. ciliary ganglion D. coeliac ganglion E. all of the above |
ANSWER D
The otic ganglion is supplied by pre-ganglionic parasympathetic fibres The carotid body is supplied by the glossopharyngeal nerve (NMS, The ciliary ganglion is supplied by pre-ganglionic parasymathetic and post-ganglionic sympathetic fibres Somatic nerves all get postganglionic. Head and neck receives postganglionic fibres from the sympathetic chain. The visceral plexuses: coeliac, hypogastric and pelvic are receive preganglionic via splanchnic nerves to supply postgangionic to viscera (except adrenal medulla). |
|
|
|
NH20a [1987]
The artery NOT supplied by the internal carotid is: A. Middle cerebral artery B. Anterior cerebral C. Posterior cerebral D. Choroidal E. Retinal |
ANSWER C
The following are the branches of the internal carotid artery, listed by segment: * C1: Branches from the cervical portion - none. * C2: Branches from the petrous portion o Caroticotympanic arteries o vidian artery * C3: Branches from the lacerum portion - none * C4: Branches from the cavernous portion o Branches of the meningohypophyseal trunk: + Tentorial basal branch + Tentorial marginal branch + Meningeal branch - helps supply blood to the meninges of the anterior cranial fossa + Clivus branches - tiny branches that supply the clivus + Inferior hypophyseal artery o Capsular branches - supplies wall of cavernous sinus o Branches of the inferolateral trunk: + Branches to trigeminal ganglion - provide blood to trigeminal ganglion + Artery of the foramen rotundum + Branches to nerves * C5: Branches from the clinoid portion - none * C6: Branches from the ophthalmic portion o Ophthalmic artery o Superior hypophyseal artery * C7: Branches from the communicating portion o Posterior communicating artery o Anterior choroidal artery o Anterior cerebral artery (a terminal branch) o Middle cerebral artery (a terminal branch) |
|
|
|
NH20b [Aug91]
The most direct branch of the internal carotid artery: A. Ophthalmic artery B. Choroidal artery C. Anterior cerebral artery D. Middle cerebral artery E. Posterior cerebral artery |
ANSWER D
|
|
|
|
NH20c ANZCA Version [Jul06] Q16 [Apr07] Q7
The largest and most direct branch of the internal carotid artery is the A. ophthalmic B. anterior cerebral C. middle cerebral D. posterior cerebral E. choroidal |
ANSWER C
|
|
|
|
NH14b ANZCA version [Jul06] Q10 Apr07 Q16
The nerve which supplies the lobule of the ear is the A. greater auricular B. lesser occipital C. auricular branch of the vagus D. auriculo-temporal E. greater occipital |
ANSWER A
Multiple nerves supply the ear. Greater Auricular Nerve -cervical plexus -posterior surface of ear and lower third anterior surface Auriculotemporal nerve -branch of the mandibular division of the trigeminal nerve -superior 2/3 of the anterior surface Auricular branch of vagus -sensory supply to the external auditory meatus and lower part of the tympanum Greater occipital nerve -spinal nerve of dorsal primary ramus of C1 and C2 (along with lesser occipital nerve) -emerges from the subocciptial triangle obliquely between inferior oblique and semispinalis capitis muscle -passes through trapezius -innervates the skin along the posterior part of the scalp to vertex Lesser occipital -cutaneous nerve arising form C2 and C3 -follows greater occipital -innervates the scalp in the lateral area posterior to ear |
|
|
|
NH14 ANZCA version [1985] [Mar93] [Mar94] [Aug96] [Apr99] [2004-Aug] Q24, [2005-Apr] Q48, [Jul07]
Sensation from the lobule of the external ear is mediated mostly by: A. The auriculotemporal nerve B. The great auricular nerve C. The lesser occipital nerve D. The greater occipital nerve E. None of the above |
ANSWER B
|
|
|
|
NN13b ANZCA version [2004-Aug] Q29, [2005-Apr] Q75, [Apr07] [Jul07] [Aug10]
The innervation of the human larynx is such that A. the internal laryngeal branch of the superior laryngeal branch of the vagus supplies the lingual surface of the epiglottis B. in the cadaveric position the cords are fully abducted C. the recurrent laryngeal nerve supplies all the intrinsic muscles of the larynx D. the glossopharyngeal nerves are sensory to the laryngeal mucous membrane above the level of the vocal cords E. cord paralysis can be produced by a distended endotracheal cuff in the larynx compressing a branch of the recurrent laryngeal nerve against the thyroid cartilage |
ANSWER E
A. FALSE : -Glossopharyngeal supplies the lingual surface of the epiglottis. -Superior laryngeal supplies the interior of the larynx to the vocal cords B. FALSE : half abducted C. FALSE. RLN supplies all the intrinsic muscles of the larynx except cricothyroid (supplied by SLN) Both are from the vagus nerve D. FALSE : . The internal laryngeal branch of the superior laryngeal nerve supplies base of tongue, posterior epiglottis, aryepiglottic folds and arytenoids E. TRUE |
|
|
|
NN13c ANZCA version [Apr97] [2002-Mar] Q105, [2002-Aug] Q140
Regarding the anatomy of the larynx 1. the cricothyroid muscles are cord tensors 2. the superior laryngeal artery accompanies the recurrent laryngeal nerve 3. the vagus nerve supplies motor fibres to all the intrinsic muscles of the larynx 4. the posterior cricoarytenoid muscles are adductors of the cords |
ANSWER 1 and 3
|
|
|
|
NN05 ANZCA version [2004-Aug] Q17, [2005-Apr] Q63, [Apr07] (Similar question reported in [1985] [Aug96] [Jul97] [Jul98])
The carotid sinus derives its nerve supply from the A. vagus nerve B. glossopharyngeal nerve C. ansa cervicalis (hypoglossi) D. middle cervical ganglion E. stellate ganglion |
ANSWER B
Carotid sinus innervation: A. T vagus (CN X) (efferent) B. T glossopharyngeal (CN IX) (afferent) Glossopharyngeal -> Nucleus of the tractus solitarius of the medulla (also true for baroreceptors in aortic arch) carotid sinus : baroreceptor at the origin of the ICA; rich nerve supply from IX (Glossopharyngeal), stimulation à fall in BP carotid body : chemoreceptor : small, oval, reddish brown structure deep to bifurcation of CCA, also innervated by IX |
|
|
|
NN13b ANZCA version [2004-Aug] Q29, [2005-Apr] Q75, [Apr07] [Jul07] [Aug10]
The innervation of the human larynx is such that A. the internal laryngeal branch of the superior laryngeal branch of the vagus supplies the lingual surface of the epiglottis B. in the cadaveric position the cords are fully abducted C. the recurrent laryngeal nerve supplies all the intrinsic muscles of the larynx D. the glossopharyngeal nerves are sensory to the laryngeal mucous membrane above the level of the vocal cords E. cord paralysis can be produced by a distended endotracheal cuff in the larynx compressing a branch of the recurrent laryngeal nerve against the thyroid cartilage |
ANSWER E
A. FALSE : -Glossopharyngeal supplies the lingual surface of the epiglottis. -Superior laryngeal supplies the interior of the larynx to the vocal cords B. FALSE : half abducted C. FALSE. RLN supplies all the intrinsic muscles of the larynx except cricothyroid (supplied by SLN) Both are from the vagus nerve D. FALSE : . The internal laryngeal branch of the superior laryngeal nerve supplies base of tongue, posterior epiglottis, aryepiglottic folds and arytenoids E. TRUE |
|
|
|
NN13c ANZCA version [Apr97] [2002-Mar] Q105, [2002-Aug] Q140
Regarding the anatomy of the larynx 1. the cricothyroid muscles are cord tensors 2. the superior laryngeal artery accompanies the recurrent laryngeal nerve 3. the vagus nerve supplies motor fibres to all the intrinsic muscles of the larynx 4. the posterior cricoarytenoid muscles are adductors of the cords |
ANSWER 1 and 3
|
|
|
|
NN05 ANZCA version [2004-Aug] Q17, [2005-Apr] Q63, [Apr07] (Similar question reported in [1985] [Aug96] [Jul97] [Jul98])
The carotid sinus derives its nerve supply from the A. vagus nerve B. glossopharyngeal nerve C. ansa cervicalis (hypoglossi) D. middle cervical ganglion E. stellate ganglion |
ANSWER B
Carotid sinus innervation: A. T vagus (CN X) (efferent) B. T glossopharyngeal (CN IX) (afferent) Glossopharyngeal -> Nucleus of the tractus solitarius of the medulla (also true for baroreceptors in aortic arch) carotid sinus : baroreceptor at the origin of the ICA; rich nerve supply from IX (Glossopharyngeal), stimulation à fall in BP carotid body : chemoreceptor : small, oval, reddish brown structure deep to bifurcation of CCA, also innervated by IX |
|
|
|
NN13b ANZCA version [2004-Aug] Q29, [2005-Apr] Q75, [Apr07] [Jul07] [Aug10]
The innervation of the human larynx is such that A. the internal laryngeal branch of the superior laryngeal branch of the vagus supplies the lingual surface of the epiglottis B. in the cadaveric position the cords are fully abducted C. the recurrent laryngeal nerve supplies all the intrinsic muscles of the larynx D. the glossopharyngeal nerves are sensory to the laryngeal mucous membrane above the level of the vocal cords E. cord paralysis can be produced by a distended endotracheal cuff in the larynx compressing a branch of the recurrent laryngeal nerve against the thyroid cartilage |
ANSWER E
A. FALSE : -Glossopharyngeal supplies the lingual surface of the epiglottis. -Superior laryngeal supplies the interior of the larynx to the vocal cords B. FALSE : half abducted C. FALSE. RLN supplies all the intrinsic muscles of the larynx except cricothyroid (supplied by SLN) Both are from the vagus nerve D. FALSE : . The internal laryngeal branch of the superior laryngeal nerve supplies base of tongue, posterior epiglottis, aryepiglottic folds and arytenoids E. TRUE |
|
|
|
NN13c ANZCA version [Apr97] [2002-Mar] Q105, [2002-Aug] Q140
Regarding the anatomy of the larynx 1. the cricothyroid muscles are cord tensors 2. the superior laryngeal artery accompanies the recurrent laryngeal nerve 3. the vagus nerve supplies motor fibres to all the intrinsic muscles of the larynx 4. the posterior cricoarytenoid muscles are adductors of the cords |
ANSWER 1 and 3
|
|
|
|
NN05 ANZCA version [2004-Aug] Q17, [2005-Apr] Q63, [Apr07] (Similar question reported in [1985] [Aug96] [Jul97] [Jul98])
The carotid sinus derives its nerve supply from the A. vagus nerve B. glossopharyngeal nerve C. ansa cervicalis (hypoglossi) D. middle cervical ganglion E. stellate ganglion |
ANSWER B
Carotid sinus innervation: A. T vagus (CN X) (efferent) B. T glossopharyngeal (CN IX) (afferent) Glossopharyngeal -> Nucleus of the tractus solitarius of the medulla (also true for baroreceptors in aortic arch) carotid sinus : baroreceptor at the origin of the ICA; rich nerve supply from IX (Glossopharyngeal), stimulation à fall in BP carotid body : chemoreceptor : small, oval, reddish brown structure deep to bifurcation of CCA, also innervated by IX |
|
|
|
Can02-56 All are true about stellate ganglion block except:
A. it is lateral to the carotid. B. it is lateral to longus coli muscle. C. it is medial to ant vertebral artery |
ANSWER A
Stellate Ganglion -formed from the fusion of the inferior cervical ganglion with the first thoracic ganglion -located at the level of C7 Relations Anterior The structures anterior to the ganglion include the skin and subcutaneous tissue, the sternocleidomastoid and the carotid sheath. The dome of the lung lies anterior and inferior to the ganglion. Medial The prevertebral fascia, vertebral body of C7, oesophagus and thoracic duct lie medially. Posterior Structures posterior to the ganglion include the longus colli muscle, anterior scalene muscle, vertebral artery, brachial plexus sheath and neck of the first rib. |
|
|
|
Canadian MCQ 2010
127. All of EXCEPT ONE of the following is seen following stellate ganglion block. Indicate the exception A. mydriasis B. facial anhydrosis C. enopthalmos D. nasal congestion |
ANSWER A
Horner’s syndrome Horner's syndrome is characterised by an interruption of the oculosympathetic nerve pathway somewhere between its origin in the hypothalamus and the eye. The classic clinical findings associated with Horner's syndrome are * ptosis * pupillary miosis * facial anhidrosis. * enophthalmos * increased amplitude of accommodation * heterochromia of the irides (if it occurs before the age of 2 years), paradoxical contralateral eyelid retraction, transient decrease in intraocular pressure and changes in tear viscosity. |
|
|
|
Canadian MCQ 2010
114. What is the anatomic location of the celiac plexus? A. anterior to the body of L1 B. lateral to adrenals and kidneys C. surrounding the IVC D. posterior to the crus of the diaphragm |
ANSWER A
Celiac Plexus -largest sympathetic plexus -main junction for autonomic nerves supplying the upper abdominal organs : * liver * gall bladder * spleen * stomach * pancreas * kidneys * small bowel * 2/3 of the large bowel Relations -surrounds the root of the coeliac artery at the level of L1 -medial to the adrenals and kidney -posterior to the IVC on the right and aorta on the left -anterior to the crura of the diaphragm Sympathetic supply: * Greater splanchnic nerve (T5/6 to T9/10) * Lesser splanchnic nerve (T10/11) * Least splanchnic nerve (T11/12) |
|
|
|
Canadian MCQ 2010
115. A patient presents with a herniated disc complaining of pain in the left buttock and posterior thigh, numbness on the left lateral malleolus and on exam has decreased left Achilles reflex. What level is the herniation? A. L2-L3 B. L3-L4 C. L4-L5 D. L5-S1 |
ANSWER D
|
|
|
|
Canadian MCQ 2010
116. Name the most common complication of thoracic paravertebral block A. Pneumothroax B. IV injection C. Subarachnoid injection D. Epidural injection |
ANSWER ??
The overall incidence of complications is 2.6-5%. Failure rate is 6.5-10% Hypotension 4.6% Vacular puncture 3.8% Pleural puncture 1.1% Pneumonthorax 0.5% |
|
|
|
Canadian MCQ 2010
117. A patient is undergoing forearm surgery under axillary nerve block. What would indicate a failure of proximal spread within the axillary sheath?? A. Preserved sensation in the 5th and medial 4th digits B. Preserved sensation of the lateral forearm C. Preserved sensation of the medial forearm D. Preserved sensation of the palmar surface of the hand excluding the medial 4th and 5th digits |
ANSWER C
A. FALSE : this supplied by ulnar nerve B. FALSE : this is supplied by the radial nerve C. TRUE : the medial cutaneous nerve branches early from the medial cord D. FALSE : median nerve |
|
|
|
Canadian MCQ 2010
118. Advantages of RA vs. GA for TURP include: A. Less post-operative confusion B. Lower DVT risk C. Less blood loss D. Earlier recognition of electrolyte changes |
ANSWER D
|
|
|
|
Canadian MCQ 2010
119. A patient develops a nerve injury post-operatively after a long surgery in the lithotomy position. What would you most likely see a loss of? A. dorsi flexion B. plantar flexion C. inversion D. sensation to the lateral aspect of the foot |
ANSWER A
Most commonly injured lower extremity nerve in patients undergoing surgery in lithotomy position was the common peroneal nerve (L4-S2, represented 78% of nerve injuries in a study which looked retrospectively at 198,461 patients undergoing surgery in the lithotomy position). Etiology: Is thought to be secondary to compression of the nerve between the lateral head of the fibula and the bar holding the legs. When the candy cane stirrups are used, special attention must be paid to avoid compression. Associated factors: patients with a low body mass index, recent cigarette smoking, prolonged duration of surgery A prospective review of 991 patients undergoing surgery in the lithotomy position from 1997 to 1998, showed that there were no motor neuropathies in the lower extremity, although paresthesias in the distribution of the obturator, lateral femoral cutaneous, sciatic, and peroneal nerves were found [Warner MA et al. Anesthesiology 93: 938, 2000] Nerve Injuries in Lithotomy Position * Most Commmon: common peroneal (78%) * Etiology: compression * Risk Factors: low BMI, smoking, prolonged surgery * Manifestation: common peroneal is L4-S2, responsible for foot dorsiflextion and toe extension (thus leads to foot drop) |
|
|
|
Canadian MCQ 2010
120. While performing a popliteal block, how do you know that you are stimulating the common peroneal nerve? A. dorsiflexion B. plantarflexion C. inversion D. ? |
ANSWER A
|
|
|
|
Canadian MCQ 2010
122. A patient is having surgery on the distal phalanx of his fifth digit. Which of the following regional techniques is the LEAST appropriate? A. Infraclavicular B. Digital C. Interscalene D. Axillary |
ANSWER C
|
|
|
|
NN32 [Apr07] [Jul07]
Stellate ganglion is where: A. at the level of the body of C6 (spine of C6) B. posterior to the brachial plexus sheath C. anterior to the dome of the pleura D. anterior to the thoracic duct E. anterior to scalenius anterior |
ANSWER E
Relations of stellate ganglion Anaesthesia UK website (http://www.anaesthesiauk.com/article.aspx?articleid=100538) * Anterior o The structures anterior to the ganglion include the skin and subcutaneous tissue, the sternocleidomastoid and the carotid sheath. The dome of the lung lies anterior and inferior to the ganglion. * Medial o The prevertebral fascia, vertebral body of C7, oesophagus and thoracic duct lie medially. * Posterior o Structures posterior to the ganglion include the longus colli muscle, anterior scalene muscle, vertebral artery, brachial plexus sheath and neck of the first rib |
|
|
|
NV42 [Apr07] [Jul07]
What do C6/7 motor function do A. flex/extension of fingers B. flex /extend wrist C. shoulder ext rotation / abduction D. elbow pronation/supination E. flexion at elbow |
ANSWER E
UPPER ARM Nerve Muscle Roots Axillary Deltoid C5 Musculocutaneous Biceps C5,6 Radial Triceps C6,7,8 Radial Brachioradialis C5,6 Radial Wrist extensors C6,7 Radial Finger extensors C7,8 Median Wrist Flexor C6,7 Median Abduct Poll Brev C8,1 Ulnar Finger ABD/ADD C8,1 * all small muscles of the hand are innervated by C8 and Tl roots. * all small muscles of the hand are innervated by the ulnar nerve except for the muscles of the thenar eminence. * both wrist flexion and extension are innervated by C6,7. Nerve Muscle Roots Hip Extension L2,3,4 Femoral Knee Extension L2,3,4 Obturator Thigh Adduction L2,3,4 Sciatic Knee Flexion L5 S1 Sciatic Branches: Peroneal Ankle dorsiflex L4,5 Tibial Plantarflex S1,2 peroneal nerve everts the foot; tibial inverts it. |
|
|
|
NN14a ANZCA version [Mar93] [Aug93] [Aug96] [Jul98] [Apr99] [2004-Aug] Q28, [2005-Apr] Q34
The muscles of the larynx which separate the vocal cords are the A. thyro-arytenoids B. lateral crico-arytenoids C. oblique arytenoids D. posterior crico-arytenoids |
ANSWER D
|
|
|
|
NN14b ANZCA version [2005-Sep] Q138, [Mar06] Q8
Muscles which abduct the vocal cords include the A. aryepiglottic B. cricothyroid C. lateral cricoarytenoid D. posterior cricoarytenoid E. thyroarytenoid |
ANSWRER D
|
|
|
|
NN14c ANZCA version [Jul07]
The muscles of the larynx which separate the vocal cords are the A. inter-arytenoids B. lateral crico-arytenoids C. oblique arytenoids D. posterior crico-arytenoids E. thyro-arytenoids |
ANSWER D
|
|
|
|
Black Bank April 2008
NH You are performing an awake nasal fibreoptic intubation and wish to topicalise the airway. Which nerves do you need to anaesthetise from proximal to distal.. A. Trigeminal, then glosspharyngeal, then vagal (different combinations of the nerves given in different orders) B. Facial, trigeminal, vagal C. Facial, trigeminal, glossopharyngeal D. Trigeminal, vagal, glossopharyngeal E. ? |
ANSWER A
3 Sensory nerves 1. Terminal branches of the Opthalmic and Maxillary divisions of Trigeminal : Nasal cavity and turbinates 2. Glossopharyngeal (IX) : oropharynx and posterior 3rd of the tongue 3. Vagus SLN AND RLN : epiglottis and distal airway |
|
|
|
BLACK BANK August 2008
NN (Q85 Aug 2008) The left recurrent laryngeal nerve A hooks around the arch of the aorta anterior to the attachment of the ligamentum arteriosum B passes under cover of the lower border of the inerior constrictor muscle before entering the larynx C supplies the cricothyroid muscle D supplies sensation to the whole of the laryngeal mucosa on the left side E contains motor fibres derived from the spinal root of the accessory nerve |
ANSWER B
A false posterior to ligamentum arteriosum B TRUE C False innervates all intrinsic muscles of the larynx except the cricothyroid D False supplies sensation to mucosa BELOW the cords (Superior laryngeal nerve above cords) E False Vagus nerve. |
|
|
|
NT (Q62 Aug 2008) The ascending aorta
A has no branches B begins at the semilunar valve C arises from right ventricle D occupies the superior mediastinum E lies inferior to the SVC |
ANSWER B
A. FALSE : coronary arteries B. TRUE C. FALSE : left ventricle D. FALSE : middle mediastinum E. FALSE : left and anterior |
|
|
|
BLACK BANK AUGUST 2008
NN (Q102 Aug 2008) The nerve providing sensory supply to the airway muscle below (inferor) to the vocal cords is the A phrenic nerve B posterior thyroid nerve C recurrent laryngeal nerve D superior laryngeal nerve E tracheal nerve |
ANSWER C
Above the cord : SLN Below the cords : RLN |
|
|
|
Black Bank August 2008
NH (Q138 Aug 2008) Ciliary ganglion A sympathetic from inferior cervical ganglion B located inferiorly within orbit C may be damaged during a peribulbar block D preganglionic parasympathetic supply from the supra trochlear nerve E preganglionic parasympathetic originates from the Edinger Westpal nucleus |
ANSWER E
CILIARY GANGLION Mixed parasymp and sympathetic Located Posterior orbit, apex of orbit, between optic nerve and lateral rectus Parasympathetic Preganglionic efferent via Edinger Westphal Nucleus along CN III Postganglionic to short ciliary fibres : miosis and accomodation Sympathetic Carotid plexus causing vasoconstriction and midriaiss Sensory Nasociliary branch of ophthalmic nerve of trigeminal nerve Sensation of the globe |
|
|
|
Black Bank April 2009
NU Which distinguishes C8-T1 from an ulnar nerve lesion at elbow? A. Paraethesia of the 5th digit B. Paraesthesia over index finger C. Flexor carpi ulnaris function D. Paraesthesia/sensory loss over medial forearm E. Adductor pollicis function |
ANSWER D
The medial cutaneous nerve of the forearm arises from the medial cord of the brachial plexus which is prior to the formation of the ulnar nerve. |
|
|
|
NH07
Which nerve does not run in contact with the mandible? A. Nerve to mylohyoid B. Auriculotemporal nerve C. Lingual nerve D. Inferior alveolar nerve E. Buccal nerve |
ANSWER E
* All are branches of the mandibular division of V. * Lingual related to medial pterygoid and mandible. * Inf alveolar goes through. * Mylohyoid n comes off inf alveolar and runs along mandible. * Auriculotemporal runs between mandible and sphenomandibular ligament. * Buccal does not run right next to mandible |
|
|
|
RH06
A successful inferior dental nerve block is: A. Associated with loss of taste on the ipsilateral anterior 2/3rds of the tongue B. Associated with sensory loss on the ipsilateral anterior 2/3rds of the tongue C. Associated with cutaneous sensory loss over the chin and lip of the ipsilateral side D. Unsuited for extraction of the incisor teeth of the ipsilateral side |
ANSWER A, B, C
Inferior Alveolar Nerve Block - Successful execution of this technique results in anesthesia of the mandibular teeth on the ipsilateral side to the midline, associated buccal and lingual soft tissue, lateral aspect of the tongue on the ipsilateral side, and lower lip on the ipsilateral side. |
|
|
|
NH01c ANZCA version [2001-Aug] Q103, [2002-Mar] Q113
The trigeminal nerve 1. is attached to the pons 2. is sensory to the face 3. is motor to the muscles of mastication 4. is joined to the trigeminal (semilunar) ganglion by a motor root and by a sensory root |
ANSWER 1, 2, 3
1. is attached to the pons true 2. is sensory to the face true 3. is motor to the muscles of mastication true 4. is joined to the trigeminal (semilunar) ganglion by a motor root and by a sensory root false. |
|
|
|
RU19 [Mar10] [Aug10] The intercostobrachial nerve:
A. Arises from T2 trunk B. Is usually blocked in brachial plexus block C. Supplies antecubital fossa D. Can be damaged by torniquet E. Arises from inferior trunk |
ANSWER D
The intercostobrachial nerve is the (modified) lateral cutaneous branch of T2. It supplies inner side of upper arm, so in under the torniquet in arm surgery. * A - False. Arises from lat. cut. branch of 2nd intercostal nerve (from T2 originally, but not directly from the trunk) * B - False. It joins the medial cutaneous nerve of the arm which comes from the medial cord, but does not form part of the brachial plexus, and is not blocked in brachial plexus blocks. * C - False. Supplies medial side of upper arm, and joins medial cutaneous nerve of arm which supplies medial side of upper arm down to the elbow. * D - TRUE. Any nerve compressed by a tourniquet can be damaged. Would have to be high up the arm/close to axilla to compress it. * E - False. Not part of brachial plexus, or a branch from it. Arises from lat. cut. branch of 2nd intercostal nerve. |
|
|
|
RH12a
To operate on the ear you would have to block: A. Auriculotemporal nerve B. Greater auricular nerve C. Auricular branch of vagus D. Greater occipital nerve E. Lesser occipital nerve |
ANSWER A, B, C
Main Cutaneous nerves are * (Cervical plexus) greater auricular -> entire cranial surface + lower part of lateral surface * (Mandibular division) auriculotemporal -> upper part of lateral surface + most of meatal skin Other much smaller contributors are: * lesser occipital nerve (C2 root) -> small contribution of upper part of cranial surface * auricular br of vagus -> tympanic membrane + posterior meatal skin * facial nerve (via tympanic plexus) -> tympanie membrane + posterior meatal skin |
|
|
|
RH12b [Mar92]
To operate on the anterior 2/3rds of the ear you would need to block: A. Mandibular n B. Maxillary n C. Vagus n D. Greater auricular n |
ANSWER 1
Auriculotemporal is the first branch of the posterior trunk of V3 after it passes through the foramen ovale. |
|
|
|
NA15 The nerve supplying area of skin between greater trochanter and iliac crest:
A. subcostal nerve B. ilioinguinal nerve C. genitofemoral nerve D. femoral nerve E. lat cutaneous femoral nerve. |
ANSWER A
Subcostal nerve The 12th thoracic (subcostal) nerve runs along the lower border of the 12th rib below the subcostal vessels, passes behind the lateral arcuate ligament to run in front of quadratus lumborum behind the kidney and colon. The nerve then passes between transversus abdominis and internal oblique and then has a course and distribution which are similar to the lower intercostal nerves. However, there is one point of difference: the lateral cutaneous branch of the 12th nerve descends without branching to supply the skin over the lateral aspect of the buttock * Lateral cutaneous br of subcostal (T12) and iliohypogastric (L1) supply skin over upper lateral buttocks ie between iliac crest and great troc. * Superior gluteal n (L4,5 S1) is a muscular branch supplying gluteus medius & minimus (of interest is that superior glurteal n and assoc superior gluteal vessels are the only structures to pass through upper compartment of GSF) * Lateral cutaneous nerve of thigh - ant br supplys ant lat skin of thigh down to knee, post br supplys skin of lat thigh from greater troc. to mid-thigh |
|
|
|
Black Bank March 2011
25. NEW. The anterior branch of the femoral nerve supplies everything but: A: pectinius B: rectus femoris C: Medial thigh D: anterior thigh E: sartorius |
ANSWER B
Muscular Branches Anterior : Pectineus and Sartorius Posterior : Quadriceps femoris (4 Parts : Rectus Femoris, Vastus Lateralis, Vastus Medialis, Vastus Intermedius) Cutaneous Branches Anterior : * Intermediate cutaneous nerve of thigh * Medial cutaneous nerve of the thigh * Lateral cutaneous nerve Posterior : * terminal branch of saphenous nerve Articular Branches to knee joint |
|
|
|
BLACK BANK March 2011
28. NEW. During scoliosis surgery with monitoring of somatosensory evoked potentials, which tract are they mainly monitoring? A: Dorsal column B: Spinothalamic tract C: Lateral Corticospinal tract D: Cerebrospinal tract E: Anterior horn cells |
ANSWER A
Somatosensory evoked potentials provide monitoring for the dorsal columns of the spinal cord. (wiki) |
|
|
|
RB38b ANZCA version [2002-Aug] Q124
A woman has an epidural placed for forceps delivery after a prolonged second stage of labour. The next day she has a right foot drop, and numbness over the anterior part of her lower leg and the dorsal surface of her right foot. The most likely cause is A. right common peroneal nerve lesion from the use of stirrups in the lithotomy position B. right L5 nerve root lesion from the epidural placement C. right lumbar plexus lesion from compression by the fetal head D. L5 nerve root lesion from a disc protrusion E. transient neurological symptoms (TNS) syndrome |
ANSWER C
Common peroneal nerve * dorisiflexion * sensation to anterior calf and dorsum of foot * prolonged lithotomy Lumbar sacral plexus * quadraceps * dorsiflexion * hip abduction Risk factors - primip, vertex presentation, forceps, prolonged labour and CPD Femoral nerve (lithotomy damage) * quadraceps * loss of patella reflex * hyperalgesia ant thigh and med calf Anterior spinal syndrome * loss of motor function, pain and temperature, but touch retained TNS - pain and dysaesthesia in the bum, thigh or calf, usually within 24hrs and resolves in 72hrs Risk factors - lignocaine, small needles, hyperbaric solution, high conc, lithotomy |
|
|
|
RB38c ANZCA version [2003-Aug] Q131
A woman has an epidural placed for forceps delivery after a prolonged second stage of labour. The next day she has a right foot drop, and numbness over the anterior part of her lower leg and the dorsal surface of her right foot. The most likely cause is A. L4 nerve root lesion from trauma during epidural placement B. L5 nerve root lesion from trauma during epidural placement C. L5 nerve root lesion from an acute disc protrusion D. right common peroneal nerve lesion from compression by lithotomy stirrups E. right lumbar plexus lesion from compression by the fetal head |
ANSWER E
|
|
|
|
RB38d ANZCA version [2006-Mar] Q111
Post partum foot drop is most frequently caused by A. compression of the lumbosacral trunk by the foetal head or forceps B. damage to the common peroneal nerve from lithotomy position C. damage to the conus medullaris by misplaced spinal anaesthesia D. L4 Nerve root damage from epidural analgesia E. the excessive lumbar lordosis of pregnancy stretching nerve roots |
ANSWER A
|
|
|
|
RB51 ANZCA version [2002-Aug] Q86, [2003-Apr] Q5, [Mar06]
A recently published large Australian multicentre trial of patients undergoing major abdominal surgery (The MASTER Trial) concluded that the use of epidural anaesthesia (with general anaesthesia) and postoperative epidural analgesia, compared with general anesthesia alone, was associated with a decrease in: A. mortality at 30 days B. both mortality at 30 days and adverse cardiovascular events C. both mortality at 30 days and respiratory failure D. adverse cardiovascular events E. respiratory failure |
ANSWER E
|
|
|
|
RB52a ANZCA version [2002-Aug] Q80, [Mar06]
Twenty-four hours following a vaginal hysterectomy, a 48-year-old obese female complains of severe pain that radiates down both buttocks and thighs. She had received a spinal anaesthetic with hyperbaric lignocaine. The most likely explanation for these complaints is A. transient neurological symptoms syndrome B. lumbar disc herniation C. a spinal abscess D. trauma due to improper positioning E. a spinal haematoma |
ANSWER A
|
|
|
|
RB52b ANZCA version [2003-Apr] Q97
Twenty-four hours following a vaginal hysterectomy, a 48-year-old obese female complains of severe pain that radiates down both buttocks and thighs. She had received a spinal anaesthetic with hyperbaric lignocaine. A likely explanation for these complaints includes all of the following EXCEPT A. a spinal abscess B. a spinal haematoma C. lumbar disc herniation D. transient neurological symptoms syndrome E. trauma due to improper positioning |
ANSWER A
|
|
|
|
RH21 ANZCA version [Apr98] [2001-Aug] Q39, [2002-Mar] Q38, [2003-Apr] Q29, [2003-Aug] Q53, [2005-Sep] Q35, [Mar06] Q12
Regional anaesthesia for modified radical mastoidectomy requires blockade of the following nerves EXCEPT A. greater auricular B. auriculotemporal C. auricular branch of the vagus D. facial E. tympanic branch of the glossopharyngeal |
ANSWER D
Facial nerve block is not required. This nerve can become damaged during the operation. Greater auricular nerve block |
|
|
|
RN15 ANZCA version [Jul00] [2003-Apr] Q81, [2003-Aug] Q90 [Mar06]
Following superficial and deep cervical plexus blockade for carotid endarterectomy, the incidence of ipsilateral phrenic nerve block is A. less than 10% B. 20-30% C. 50-60% D. 80-90% E. nearly 100% |
ANSWER C
|
|

