![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
137 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
17. (Variation of old Question). Paediatric ALS – 20 kg, VF has had 2 shocks only. Next step |
ANSWER A
Infant/Child ALS guidelines from UK Resus Council Etieology : respiratory or circulatory failire more common than arrythmias, leading to secondary cardiopulmonary arrest Changes in 2010 -adrenaline is given after 3rd shock for shockable rhythms and then every alternate cycle (3-5min of CPR) -if non shockable, adrenaline should be given ASAP -amiodarone is given after 3rd shock for shockable rhythms, repeat after 5th shock - Compression to Vent Ratio |
|
|
|
PP (Q90 Aug 2008) A 6 month old baby is booked for an elective right inguinal hernia repair. An apropriate fasting time is
A. 2 hours breast milk B. 4 hours formula milk C. 5 hours breast and formula milk D. 6 hours solids E. 8 hours solids, 4 hours all fluids |
ANSWER B
As per RCH guidelines 2 hours clear fluids 3 hours for breast milk 4 hours for formula/cows milk 6 hours for solids But infants less than 6 months 4 hours for solids and forumula milk |
|
|
|
PP (Q139 Aug 2008) Arrest in a 10 year old. Has ventricular tachycardia after a near drowning accident. Patient is intubated and is being ventilated with 100% O2 and has IV access. A single DC monophasic shock of 60J has been given. The next step is to give
A adrenaline 10mcg/kg and DC shock 60J B adrenaline 10mcg/kg and DC shock 120J C amiodarone 5mg/kg D DC shock 60J E DC shock 120J |
ANSWER E
Sequence of actions for APLS UNWITNESSES 1. Establish BLS (ABC) 2. Oxygenate, ventilate, chest compressions 100% BMV or intubation early, resp rate 10-12/min Compression rate 100-120/min uninterrupted Ratio 15:2 IV access or intraosseous 3. Attach defibrillator and Assess rhythm Shockable VT/VF a. initial defibrillate with mono or biphasic 4J/kg -> resume CPR 2min, do not assess rhythm or pulse b. assess rhythm if VF/VT second shock 4J/kg ->resume CPR 2min c. assess rhythm if VF/VT give adrenaline 10mcg/kg IV/IO or 100mcg/kg ETT and shock 4J/kg d. repeat C -adrenaline should be given every second CPR cycle -Consider 4Ts and 4Ps -Refractory VT/VF consider : Amiodarone 5mg/kg bolus Lignocaine 1mg/kg bolus (do not give if amiodarone given) -Last resort attempts Sodium Bicarbonate 1mmol/kg Magnesium Sulphate 0.05-0.1 mmol/kg Potassium Chloride 0.05 mmol/kg 4J/KG Non shockable : continue CPR for 2min WITNESSED ei. cardiac cath lab, ICU, resus etc 3 stacked shocks at 4J 4J 4J |
|
|
|
PP (Q150 Aug 2008) 6 month old baby for VSD repair. Induced with 50% N2O, O2, sevoflurane 8%. While obtaining IV access, the patient desaturates to 85%. The manouevre to increase the O2 saturations is to
A give a fluid bolus B change from sevoflurane to isoflurane C institute CPAP D decrease the FiO2 E reduce the sevoflurane concentration |
ANSWER E
Poorly worded question, depends if examiner is looking at causes of laryngospam or reversal of shunt in VSD. The clinical situation will reveal which is more likely. VSD in children typically non cyanitic, restrictive CHD. Normally left to right shunt. Resulting in high pulmonary flow and therefore pressure. VSD most common isolated CHD 20% of all defects Classifed by anatomical location 1. Supracristal :above crista supraventricularis just under annulus of aorta 2. Infracristal : lower in membranous septum 3. Canal type : auriculo-ventricular canal 4. Muscular : anywhere in muscular septum Children with small defects have few symptoms due to restricted flow across defect, muscular type may close spontaneously Larger defects, heart failure develops due L-R shunt, increasing pulmonary hypertension and volume overload. Hypoxemia results when shunt is reversed R-L shunt Avoiding increases in PVR -Hypoxia -hypercapnia -acidosis -hypothermia -hyperinflation, CPAP, PEEP -atelectasis -sympathetic stimulation Maintain SVR -anaesthetic doses of fentanyl - |
|
|
|
Characterize innocent murmurs in children.
|
INNOCENT MURMURS
-Most commonly functional, innocent, physiological heart murmur -10% of normal children -Most common is Still's Murmur, followed by flow murmurs due to increased CO eg fever or anaemia -Heart is structurely normal -No signs or symptoms of cardiac disease, features 1. soft, no thrill 2. systolic murmur, short (never pansystolic) 3. asymptomatic 4.best heard over left sternal edge, no radiation 5. changes with posture, softer when standing Pathological prematurity other congenital problems feeding intolerance failure to thrive respiratory symptoms - particularly repeated infections cyanosis chest pain syncope family history of sudden death Examination palpation : precordial activity : ASD, moderate to large VSD, significant PDA Thrill at lower left sternal border : VSD Thrill at left upper : pulmonary valve stensosis Thrill at suprasternal notch : aortic stenosis Timing of brachial and femoral pulses should be equal in timing and intensity and pressure to exclude aortic coarctation http://findarticles.com/p/articles/mi_6811/is_3_26/ai_n32369899/?tag=content;col1 |
|
|
|
Characterize pathological murmurs in children.
|
PATHOLOGICAL MURMURS
HISTORY Birth History : prematurity, birth asphyxia, Cardiac Symptoms -Cyanosis (R->Lshunt) -Hypercyanotic spells (typical of TOF) -Respiratory symptoms : breathlessness, slow feeding,cold clammy sweatiness, poor weight gain, limited exercise tolerance, frequent resp tract infections -Syncope : sudden collapse due to arrhythmias, collapse with exercise (cHOCM/AS), -Chest pain : coronary arteries abnormalities are rare, but maybe due Kawasaki disease or Anomalous Origin of the Left Coronary Artery -Poor weight gain -General history including another congenital abnormalities or syndromes, family history of cardiac disease, history of rheumatic fever or endocarditis |
EXAMINATION
Inspection -Dysmorphic features eg Down's Syndrome, Cleft palate, spinal deformity -Sign of poor weight gain/failure to thrive -Signs of breathlessness : RR, intercoastal and sub-costal recession, nasal flaring, grunting -Peripheral vs central cyanosis; confirm with pulse oximetry -JVP is difficult to assess in children <5 Palpation -pulses : rate, rhythm, colume and character Radio-femoral delay : aortic coarctation -Suprasternal thrill :AS -Heave : ventricular hypertrophy -Normal position of apex : 4th IC space nipple <5yo, 5th IC space nipple line >5 -Peripheral edeman is late sign Percussion -liver size Auscultation SYSTOLIC Murmurs Ejection systolic murmur Upper right sternal edge +/- carotid thrill = AS Upper left sternal edge : PS or ASD Long harsh murmur with cyanosis = TOF Pansystolic murmur Lower left sternal edge +/-thrill = VSD Apex = MR DIASTOLIC murmurs Unusual in children Lower left sternal edge, sitting forward, collapsing pulses = AR CONTINIOUS murmur Left infraclavicular region = PDA Any site (back, shoulder, lungs) = AV malformation |
|
|
PP 12 year old child with hip dislocation at 4pm. Ate 1 hour after injury. Now 11 pm. Best anaesthetic:
A. RSI with ETT B. delay until next day then treat elective C. inhalational induction and continue with face mask D. Reduce immediately with iv sedation E. inhalational induction and continue with face mask |
ANSWER A
|
|
|
|
PP child for grommets with clear runny nose, coryza. dry cough, clear chest, otherwise well, no fever. management:
A. delay 2 weeks B. delay 1 week C. proceed with ETT D. proceed with face mask E. |
ANSWER D
Traditionally, children who present for elective surgery with RTI are postoned at least until asymptomatic Paedatric Anaesthesia 2001 11:29-40 Clinical predictors of anaesthetic complications in children with respiratory tract infections -Prospective case control study -Highlighted 8 Variables 1. Airway management 2. Parent states the child has a 'cold' 3. Child has nasal congestion 4. Child Snores 5. Child is a passive smoker 6. Induction agent used 7. Child produces sputum 8. Reversal agent used RTI in preceding 6 weeks did not increase probability of complications Risk factors for airway complications during general anaesthesia in paediatric patients Pediatric Anesthesia Volume 12, Issue 9, pages 762–769, November 2002 3 Independent Risk Factors 1. Age <6 2. RTI 3. Airway manipulation FM>LMA>ETT Anesthesia for the Child with an Upper Respiratory Tract Infection: Still a Dilemma? Anesthesia & Analgesia Issue: Volume 100(1), January 2005, pp 59-65 |
|
|
|
PP When using a T piece for a small child, which is not an advantage?
A. Can use low gas flows B. Feel compliance C. Assess tidal volume D. Can rapidly change levels of CPAP E. low resistance |
ANSWER A
|
|
|
|
PP Haemoglobin in infants:
A. 30% fetal Hb at birth, adult levels by 3 months B. 70% fetal Hb at birth, negligible amounts by 6 months C. Hb 90 at 6 months normal doesn't need Ix D. Hb 200 at birth unless delayed cord clamping E. ? |
At birth HbF 75-80%
HbF deliver O2 effectively to tissues in hypoxic conditions but holds onto O2 after brith Compensated by polycythemia Hb 120-200 At 6/12 HbF replaced by HbA coupled with increases in 2,3 DPG there is right shift of curve which aids O2 offloading in tissues Although, neonates have high Hb, CO and low risk of arterial disease, their trigger for transfusion is higher due to the presence of HbF. TRIGGER FOR TRANSFUSION Neonate = Hb 120 Infant/Child = Hb 6.5 Adult = Hb 80 |
|
|
|
How much blood would you give to raise the Hb by 10?
|
Packed Red Cells 4 ml/kg
Whole Blood 8 ml/kg |
|
|
|
A naked neonate in an incubator (room temp 20C) loses heat mainly by:
A. Radiation B. Conduction C. Convection D. Evaporation from skin E. Evaporation from airway |
ANSWER A
|
|
|
|
What are the principles of fluid administration in neonates?
|
Neonates have reduced renal function and produce dilute urine.
They are unable to tolerate dehydration; a high fluid load or sodium load in the first few days of life. They undergo a diuresis after a few days of life. If a baby requires intravenous fluids from birth, they should be given as 10% dextrose in the following volumes : Fluid volume (ml/kg/day) Day 1 60 Day 2 90 Day 3 120 Day 4 150 Day 5 150 Sodium 3 mmol/kg/day and potassium 2 mmol/kg/day should be added after the postnatal diuresis or if the baby becomes hyponatraemic: A premature neonate may require an additional 30 ml/kg/day because of increased insensible fluid losses and may also require additional sodium supplements (4 mmol/kg/day). Replacement fluids (ie during surgery or to correct hypovolaemia) should be given as isotonic fluid (0.9% saline or Ringers-Lactate/Hartmann’s) or blood to maintain the haemoglobin at 10-12 g/dl. 50% dextrose 25ml may be added to 500ml of isotonic solution to give a 2.5% solution if the blood sugar is low. It is safer to administer fluids via a burette to avoid fluid overload. Postoperatively fluids should be restricted to 60% of maintenance (or remain at day1-2 levels of restriction if the child undergoes early surgery). |
|
|
|
What are the normal values for heart rate, respiratory rate and blood pressure in a term neonate?
|
Heart rate 120-180 beats per min
Respiratory rate 30-40 breaths per min Mean arterial blood pressure 30-50 mmHg Mean systolic BP 50-90 mmHg Mean diastolic BP 25-60 mmHg |
|
|
|
The optimal skin temperature of a premature neonate being nursed in an incubator is:
A. 28C B. 30C C. 32C D. 34C E. 36C |
Neutral Thermal Environment - environmental air temperature at which baby with a normal body temp has minimal metabolic rate and therefore minimal oxygen consumption
Neonatal Core Normothermia 36.6-37.5 Guidelines from the Womens for Skin Temperature Neonates < 1750g : 36.8 degC Neonates > 1750g : 36.5 degC Optimal abdominal skin temperature control at 36.5°C (slightly warmer than previously reported but less than 37.5°C) is recommended for premature neonates nursed on radiant warmer beds. Frequent monitoring of core temperature for these infants is strongly recommended to avoid central hyperthermia. PEDIATRICS Vol. 79 No. 1 January 1987, pp. 47-54 |
|
|
|
PP04 [1985] [1986] [Mar91] [Apr96] [Aug96] [Apr97] [Jul97]
A 5kg baby is 5% dehydrated. The body water deficit: A. 150mls B. 200mls C. 250mls D. 300mls E. 350mls |
ANSWER C
The % dehydrated is a % of total body weight. Five percent of 5,000g is 250g. |
|
|
|
PP05a
What is the fluid replacement for maintenance of a 3kg neonate in the first 24 hours of life? A. 50mls B. 100mls C. 150mls D. 200mls E. 250mls |
ANSWER ?D
Maintenance Water Requirements Age ml/kg/day 1st day of life 60 2nd day 90 3rd day 120 up to 9 months 120–140 12 months 90–100 2 years 80–90 4 years 70–80 8 years 60–70 12 years 50-60 Frank Shann's book has * 2ml/kg/h first day * 3ml/kg/h second day * 4ml/kg/h subseqently Factors modifying water requirements Extra Required * Fever (add 12% for each °c above 37°C) * Hyperventilation * High ambient temperature * Extreme activity * Any other abnormal losses e.g. diarrhoea, polyuria Less required * Hypothermia (subtract 12% for each°c below 37°C) * Very high humidity * Oliguria or anuria * Extreme inactivity * Fluid retention e.g. cardiac failure |
|
|
|
PP05b [1985] [Aug93]
The fluid requirements of a one day old full term neonate would be: A. 5 ml/hr B. 10 ml/hr C. 20 ml/hr D. 30 ml/hr E. 40 ml/hr |
ANSWER B
Frank Shann's book has * 2ml/kg/h first day * 3ml/kg/h second day * 4ml/kg/h subseqently 3 ml/kg/hr x 3.3 kg = 10 ml/hr |
|
|
|
The APGAR score of a neonate who is blue in colour with weak respirations, weak cry, pulse of 84, flo[[PPy with slight flexion to stimulation is:
A. 1 B. 2 C. 3 D. 4 E. 5 |
ANSWER D
APPEARANCE 0 - blue or pale 1 - pink body, blue extremities 2 - completely pink PULSE 0 - abscent 1 - slow <100 2 - normal >100 GRIMACE 0 - no response 1 - Grimace 2 - Cough or sneeze ACTIVITY 0 - Limp 1 - some flexion 2 - active movement RESPIRATIONS 0 - absent 1 - slow irregular 2 - crying A=0, P=1, G=1, A=1, R=1 |
|
|
|
What is the APGAR score?
What the implications and management of APGAR scores? |
Score 8 to 10
* This is 90% of all neonates. Normally, no treatment is required except nasal and oral suctioning, drying of the skin and maintenance of normal body temperature. * Carefully reevaluate the neonate at 5 minutes because some neonates hypoventilate when stimulation ceases. * As soon as stable, wrap the neonate in a warm blanket and return to the parents . [edit] Score 5 to 7 * This score suggests the neonate suffered mild asphyxia just before birth. They usually respond to vigorous stimulation with oxygen blown over the face. * If they are slow to respond and to become pink, ventilate with 80% to 100% oxygen by bag and mask. * By 5 minutes of age, patients who have Apgar scores of 5 to 7 at 1 minute are usually well. * At 2 minutes of age, PaO2 is usually 50 to 70 mm Hg (FIO2 = 0.21),PaCO2 is 40 to 50 mm Hg, pHa is about 7.15 and base deficit is approximately 12 mEq/L. * By 10 minutes of age, pHa increases to 7.30, PaCO2 decreases to below 40 mm Hg, and base deficit usually returns to normal (-3.0 to +3.0 mEq/L). Score 3 to 4 * These neonates are moderately depressed and are typically cyanotic with poor respiratory effort. They usually respond to bag-and-mask ventilation, breathe, and become pink. * If they have not breathed spontaneously, ventilating the lungs with a bag and mask may be difficult because the airway resistance exceeds that of the esophagus. If so, gas may preferentially enter and distend the oesophagus, stomach, and gut, which may interfere with ventilation and cause vomiting and regurgitation. Decompressing the stomach makes it easier to ventilate the lungs * If the neonate has not breathed or is breathing ineffectively, insert an endotracheal tube before ventilating the lungs. * Obtain umbilical artery and vein blood from a double-clamped segment of umbilical cord to measure blood gases and pH. The blood gases are frequently abnormal: PaO2 below 20 mm Hg, PaCO2 above 60 mm Hg, and pH below 7.15. * If the pH and base deficit are unchanged or worse on a sample of blood obtained from a radial artery, an umbilical artery catheter should be inserted, and if necessary, sodium bicarbonate should be administered. Score 0 to 2 * These neontates are severely asphyxiated and require immediate resuscitation. * It is not appropriate to wait to see how the patient will do as their condition usually worsens. Resuscitate immediately. |
|
|
|
PP98 ANZCA version Jul07
With respect to gastric volumes and fasting in children A. casein-predominant milks empty faster than whey-predominant milks B. children have a higher incidence of aspiration than adults C. solids rely on first order kinetics for gastric emptying but liquids follow zero order kinetics D. the rate of gastric emptying is NOT related to the energy content of the meal E. unlimited clear fluid ingestion 2 hours before surgery does NOT affect volume, but does affect the pH of stomach contents |
ANSWER B
A. FALSE : Human milk and whey predominant formula empty faster than casein predominant formula and cow's milk. Probably due to lower protein content in human and whey based milk. B. TRUE : Paediatric aspiration is slightly more common than in adults (1 per 1200–2600 compared to 1 per 2000–3000 in adults) C. FALSE : Solids follow zero order (linear decay) kinetics and liquids first order (exponential decay), in regards to stomach emptying. D. FALSE : fats slower than CHO E. FALSE : Clear fluids up to 2 hrs preop do not increase gastric volume or signicantly change gastric pH (there may be an increase in pH with clear fluids up to 2 hrs) |
|
|
|
ANZCA Version [Jul07]
You are commencing general anaesthesia for a 2-year-old child to allow biopsy of an anterior mediastinal mass, A pre-operative CT scan demonstrated compression of the lower trachea and the carina by Ihe mass. During inhalational induction, the child desaturates to 70% due to airway compression by the mass. You should A. apply continuous positive airway pressure (CPAP) via facemask B. arrange urgent median sternotomy C. intubate the patient and allow spontaneous ventilation D. intubate the patient and provide positive pressure ventilation E. place the patient in the prone position |
ANSWER A
See review medind.nic.in/iad/t05/i4/iadt05i4p344.pdf Simple maneuvers first, Sats are 86% 1. Chin lift/thrust 2. CPAP 3. Lateral position, semi sitting, prone 4. Intubate/ventilate 5. Median Sternotomy Recommended technique for Anterior Mediastonal Mass for biopsy ??? TBA |
|
|
|
PP96 [Jul07]
Newborn with diaphragmatic hernia. Initially sats 95% on RA. Now beginning to develop respiratory distress. Next appropriate step: A. Awake intubation B. Trial NO prior to intubation and ventilation C. Rapid sequence induction D. Mask ventilation throughout case with CPAP E. Gas down with CPAP |
A. Difficult in newborn
B. Contraindication to nitrous oxide as it will cause distention and worsen hypoemia C. RSI sounds good D. No CPAP E. NO CPAP |
|
|
|
PP95 [Jul07]
A one year old child arrests with VT. Has had 2x DC shocks, and 100 mcg adrenaline. Further 1x DC shock given. What is next step? A. 20 J DC shock B. 40 J DC shock C. 50 mg amiodarone D. 100 mcg adrenaline E. 1000 mcg adrenaline |
Answer is C
In VF/VT: 1. Defibrillate the heart: Give 1 shock of 4 J kg-1 if using a manual defibrillator. 2. Resume CPR: Without reassessing the rhythm or feeling for a pulse, resume CPR immediately, starting with chest compression. 3. Continue CPR for 2 min. 4. Pause briefly to check the monitor: If still VF/VT, give a second shock at 4 J kg-1 if using a manual defibrillator 5. Resume CPR immediately after the second shock. 6. Consider and correct reversible causes (see above: 4Hs and 4Ts). 7. Continue CPR for 2 min. 8. Pause briefly to check the monitor: If still VF/VT: Give adrenaline 10 microgram kg-1 followed immediately by a (3rd) shock. 9. Resume CPR immediately and continue for 2 min. 10. Pause briefly to check the monitor: If still VF/VT: Give an intravenous bolus of amiodarone 5 mg kg-1 and an immediate further (4th) shock. 11. Continue giving shocks every 2 min, minimising the breaks in chest compression as much as possible. 12. Give adrenaline immediately before every other shock (i.e. every 3-5 min) until return of spontaneous circulation (ROSC). The scenario described in the question outlines steps 1-9. Next step if still in VT is amiodarone 5 mg/kg ~ 50mg. So answer = C. |
|
|
|
PP93 [Apr07] Q124
The Neonatal Facial Coding Scale (NFCS) used to assess pain in neonates includes all of the following except A. Brow bulge B. Chin quiver C. Closed mouth D. Deep nasolabial fold E. Eyes squeezed shut |
ANSWER C
Neonatal Facial Coding System (NFCS) actions monitored: 1. Brow lowering (lowering and drawing together of the brow can result in brow bulge) 2. eyes squeezed shut 3. deepening of the naso-labial furrow (fold) 4. open lips (any separation of the lips is an occurrence) 5. vertical mouth stretch 6. horizontal mouth stretch 7. taut tongue (cupping of the tongue) 8. chin quiver (high frequency vibration of the chin and lower jaw) 9. lip pursing (tightening the muscles around the lips to form an "oo") In addition a tenth activity was monitored in preterm infants: 10. Tongue protrusion (this is a "no pain" response in full term infants) |
|
|
|
PP87 [Jul06] Which is an estimate of the weight (in kgs) of a child? (where age is in years)
A. (age+4)x2 B. (agex2)+4 C. (age+2)x3 D. (age+3)x2 E. ? |
ANSWER B
The "standard" anaesthetic formula are: From age 1-8: wt= (age x 2) + 8 From age 8-12 wt = (age) x 3 For practical use though, a simple easy-to-remember guide that I made up is the "1-6-10 rule": * At age 1 yrs -> 10kgs * At age 6 yrs -> 20kgs * At age 10yrs -> 30kgs And for the in-between years: * From 1->6, add 2kgs/yr * From 6->10, add 2.5kgs/yr Another rule of thumb for >1yr old is (2x Age)+9 until 9yrs old, and 3x Age thereafter. |
|
|
|
PP90 [Jul06] [Apr07] Q8
Child having multiple lower limb osteotomies. He has frequent painful muscle spasm and cerebral palsy. Best analgesia: A. continuous epidural infusion with bupivacaine and clonidine B. regular NSAID plus tramadol C. morphine PCA D. paracetamol and oxycodone E. spinal morphine |
ANSWER A
Current practice at RCH |
|
|
|
PP10 [Mar94] [Apr96] [Aug96] [Jul00] [2001-Apr] Q51, [2005-Apr] Q57, [Jul05] [Mar06]
The passage of an appropriately sized endotracheal tube in a neonate suffering from the idiopathic respiratory distress syndrome (hyaline membrane disease) will A. impair oxygenation by making grunting impossible B. impair oxygenation by increasing airway resistance C. improve oxygenation by reducing dead space D. improve oxygenation by eliminating laryngeal obstruction E. have no effect on oxygenation |
ANSWER A
Respiratory Distress Syndrome also called Idiopathic Respiratory Distress Syndrome, or Hyaline Membrane Disease. Result of lack of surfactant at birth Risk factors * Prematurity * Diabetic mothers Lack of surfactant implies that alveoli are more prone to collapse as surfactant decreases work of breathing and helps promote alveolar stability. Hence neonates with HMD have requirements for high PEEP when ventilated, as well as higher pressures due to decreases ventilatory compliance. Neonates will classically grunt at the end of expiration in order to apply some self-PEEP and hence keep alveoli open. Hence the correct answer is A. However it seems illogical to me that one would place an ETT without ventilation |
|
|
|
Clinical signs for dehydration in a child.
|
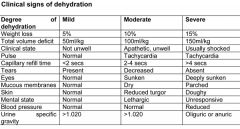
|
|
|
|
Tube Size in Neonates/Infants
|
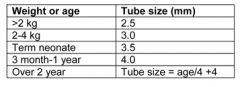
|
|
|
|
Describe the Holliday and Segar Formula
|
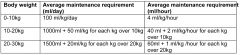
'4-2-1' formula to describe maintenance fluids in infants/children
|
|
|
|
How would you estimate a child's weight based on age?
|
Age < 9yrs
Wt(kg)approx=(2xAge)+9 OR Wt (kg)= (Age+4)x2 Age > 9yrs *Wt(kg)approx=3xAge |
|
|
|
What is the normal blood volume for a child?
|
80-85 ml/kg
|
|
|
|
PP10 ANZCA version [2001-Apr] Q51, [2005-Apr] Q57, [2005-Sep] Q66, [Mar06] Q47
The passage of an appropriately sized endotracheal tube in a neonate suffering from the idiopathic respiratory distress syndrome (hyaline membrane disease) will A. impair oxygenation by making grunting impossible B. impair oxygenation by increasing airway resistance C. improve oxygenation by reducing dead space D. improve oxygenation by eliminating laryngeal obstruction E. have no effect on oxygenation |
ANSWER A
Respiratory Distress Syndrome also called Idiopathic Respiratory Distress Syndrome, or Hyaline Membrane Disease. Result of lack of surfactant at birth Risk factors * Prematurity * Diabetic mothers Lack of surfactant implies that alveoli are more prone to collapse as surfactant decreases work of breathing and helps promote alveolar stability. Hence neonates with HMD have requirements for high PEEP when ventilated, as well as higher pressures due to decreases ventilatory compliance. Neonates will classically grunt at the end of expiration in order to apply some self-PEEP and hence keep alveoli open. |
|
|
|
PP36 ANZCA Version [2001-Aug] Q32, [2002-Mar] Q50, [2003-Aug] Q84, [2004-Apr] Q74 (Similar question reported in [Aug94] [Apr96] [Apr98] [Jul98])
A two year old child sustains a simple fracture of the lower end of the forearm one hour after having a full meal. The most appropriate approach is to A. postpone surgical reduction for 12 hours and treat as an elective case B. allow immediate reduction using a rapid sequence induction, cricoid pressure and intubation C. allow immediate reduction using a regional technique D. allow immediate reduction, after gastric emptying with a tube followed by rapid sequence induction, cricoid pressure and intubation E. wait 4 hours and treat as elective |
A is best answer? (C,D,E are more incorrect)
?B - never heard of a four/five hours fast, but it's close to six. This is an area fought with most contention. My own approach is at least six hour fast and low threshold of RSI with any of the following: - same day injury - meal close to time of injury - unwell looking and distressed child - pain and opioid - afterhour with little help around Face mask/LMA if next day, pt fasted, hungry, etc. Main thing is ensure adequate depth of anaesthesia prior to any manipulation (airway or bones). |
|
|
|
PP36 ANZCA March 2006 Version [Mar06] Q122 (Option B different)
A two-year-old child sustains a simple fracture of the lower end of the forearm one hour after having a full meal. The most appropriate approach is to A. postpone surgical reduction for 12 hours and treat as an elective case B. allow reduction after 4 hours using a rapid sequence induction, cricoid pressure and intubation C. allow immediate reduction using a regional technique D. allow immediate reduction, after gastric emptying with a tube followed by rapid sequence induction, cricoid pressure and intubation E. wait 4 hours and treat as elective |
A is best answer? (C,D,E are more incorrect)
?B - never heard of a four/five hours fast, but it's close to six. This is an area fought with most contention. My own approach is at least six hour fast and low threshold of RSI with any of the following: - same day injury - meal close to time of injury - unwell looking and distressed child - pain and opioid - afterhour with little help around Face mask/LMA if next day, pt fasted, hungry, etc. Main thing is ensure adequate depth of anaesthesia prior to any manipulation (airway or bones). |
|
|
|
PP83b ANZCA Version [2006-Mar] Q117, [Jul06] Q80
Regarding endotracheal tubes for paediatric patients A. a 2.5 mm endotracheal tube is the appropriate size for a term neonate B. armoured (wire spiral) endotracheal tubes have the same outside diameter as non-armoured endotracheal tubes (of the same internal diameter) C. the outside diameter (in mm) of an appropriately sized tube is given by the formula (Age/4) +4 D. the same diameter tube is used for nasal and oral intubation in a child E. uncuffed, paediatric endotracheal tubes do NOT have a Murphy’s eye |
ANSWER D
A. False - term neonate would be 3.0-3.5 - preterms would be 2.5 tubes B. False - armoured tubes are thinner, so for the same internal diameter, armoured tubes are smaller C. False - this formula refers to the INTERNAL diameter. D. TRUE - albeit at different lengths of insertion E. False - they do have a Murphy eye! |
|
|
|
PP83a [Mar06]Q117 [Jul06] [Jul07]
Neonate and intubation: A. use 2.5mm internal diameter ETT B. uncuffed tube has no Murphys eye C. external diameter of a reinforced ETT is the same as a normal ETT D. use same size for oral and nasal E. Something about a 4.0 ETT has an external diameter of 4mm F. Age/4 + 4 is formula for external diameter |
ANSWER D
|
|
|
|
PP46b ANZCA version [2001-Apr] Q17, [2003-Apr] Q104, [2003-Aug] Q57, [Mar06]
The average expected depth of insertion of an oral endotracheal tube, from the lip, in a normal newborn infant is A. 7.5 cm B. 8.5 cm C. 9.5 cm D. 10.5 cm E. 11.5 cm |
ANSWER C
The approximate depth of insertion measured from the centre of the lips for an oral tube: * in a newborn is 9.5 cm, * 11.5 cm for a 6 months old infant * 12 cm for a 1 year old. * Thereafter, the approximate depth of oral insertion is given by the formula: age (years)/2 + 12 cm |
|
|
|
PP46a [Apr98] [Jul00]] (type A)
For oral intubation in a neonate, what is the best length of the ETT at the lips? A. 7 cm B. 8 cm C. 9.5 cm D. 11 cm E. Age/2 + 12 |
ANSWER C
The approximate depth of insertion measured from the centre of the lips for an oral tube: * in a newborn is 9.5 cm, * 11.5 cm for a 6 months old infant * 12 cm for a 1 year old. * Thereafter, the approximate depth of oral insertion is given by the formula: age (years)/2 + 12 cm |
|
|
|
PP80 ANZCA version [2005-Apr] Q123, [2005-Sep] Q70 [2006-Mar] Q32
A three-week-old infant presents with vomiting for 3 days and a diagnosis of pyloric stenosis. The most correct statement concerning resuscitation is that: A. alkalosis should be treated with dilute hydrochloric acid B. 5% albumin is an appropriate fluid for initial treatment of shock C. fluid deficit should be completely replaced with 5% dextrose D. hyponatraemia should be treated with 2N (twice normal) saline E. potassium replacement should begin immediately |
ANSWER B
• A. False • B. True – well documented benefits of 5% albumin for resuscitation in children – outcome benefit in surgical patients with 40ml/kg. • C. False – poor choice, min time in intravascular volume, inc. Intracellular fluid • D. False – slow rehydration/optimization better or risk hyperchloraemic metabolic acidosis and Central Pontine Myelinolysis. • E. False – slow correction after fluid resuscitated first |
|
|
|
EZ79 ANZCA Version [2006-Mar] Q115, [Jul06] Q59
An infant is anaesthetised and ventilated using an endotracheal tube and circle breathing system with CO2 absorber. The item which causes the most resistance to breathing is the A. airway pressure limiting (APL) valve B. circuit hosing C. endotracheal tube D. heat and moisture exchange filter E. inspiratory and expiratory valves |
ANSWER C
a size 3.5 ETT in a 3 month old infant has 10 times the resistance of a circle system. |
|
|
|
PP66 ANZCA version [2003-Apr] Q108, [2003-Aug] Q56, [Mar06], [Jul06] Q42, [Mar 10]
In infants with congenital pyloric stenosis A. dehydration is associated with early hyponatraemia B. plasma chloride levels seldom fall below 85 mmol.l-1 C. renal conservation of hydrogen and potassium ions occurs D. the urine is initially alkaline, then may become acidic E. vomiting causes a loss of potassium ions |
ANSWER D
* A. dehydration is associated with early hyponatraemia * B. plasma chloride levels seldom fall below 85 mmol.l-1 * C. renal conservation of hydrogen and potassium ions occurs - false: Hydrogen exchanged for potassium leading to hypokalaemia * D. the urine is initially alkaline, then may become acidic - true and most correct answer: "Vomiting normally results in equal loss of gastric acid and alkaline duodenal fluid. However, with gastric outlet obstruction, gastric acid along with a variable amount of Na+ and K+ is lost in vomitus without loss of HCO3− from the duodenum. The resultant systemic alkalosis overwhelms the capacity of the proximal convoluted tubule to reabsorb HCO3−, producing an alkaline urine. As extracellular fluid volume depletion increases, aldosterone is secreted, leading to renal conservation of Na+ in exchange for K+. Eventually hypokalaemia forces Na+ exchange preferentially with H+ instead of K+ in the renal tubules. This produces the characteristic ‘paradoxical acid urine’ in the face of systemic alkalosis." (Anaesthesia & Intensive Care Medicine Volume 9, Issue 4, April 2008, Pages 133-141) * E. vomiting causes a loss of potassium ions - true, but a variable amount: "Vomiting normally results in equal loss of gastric acid and alkaline duodenal fluid. However, with gastric outlet obstruction, gastric acid along with a variable amount of Na+ and K+ is lost in vomitus without loss of HCO3− from the duodenum" (Anaesthesia & Intensive Care Medicine Volume 9, Issue 4, April 2008, Pages 133-141) |
|
|
|
PP68b ANZCA Version [2004-Apr] Q139, [Mar06]
Separation anxiety in most infants begins at A. 2 - 4 months B. 4 - 6 months C. 6 - 8 months D. 8 - 10 months E. 10 - 12 months |
ANSWER C
|
|
|
|
PP72 ANZCA version [2004-Apr] Q97, [2004-Aug] Q92, [Mar06] Q75, [Jul06] Q63
Ventricular fibrillation in children A. if resistant to defibrillation, should be treated with amiodarone 5 mg.kg-1 B. is not associated with tricyclic antidepressant overdose C. is often associated with respiratory arrest D. is the commonest arrhythmia associated with cardiac arrest E. should be immediately defibrillated with a 5 J.kg-1 shock |
ANSWER A
DC shock is 2J/k then 4J/kg thereafter. The first line antiarrhythmic for shock-refractory VF/pulselessVT is amiodarone, 5mg/kg * The most common arrest scenario in children is bradycardia proceeding to asystole - a response to severe hypoxia and acidosis. * VF is relatively uncommon, but may complicate hypothermia, TCA poisoning, and those children with pre-existing cardiac disease |
|
|
|
PP73 ANZCA version [2004-Apr] Q133, [Mar06] Q68, [Jul06] Q39
Conditions which are more commonly associated with exomphalos, compared to gastroschisis include A. amniotic fluid peritonitis B. cardiac abnormalities C. fluid and electrolyte disturbances D. hypothermia E. prematurity |
ANSWER B
Gastroschisis involves a defect in the anterior abdominal wall (usually on the right) causing herniation of the abdominal contents without a covering sac In exomphalos there is a failure of the gut to return to the abdominal cavity during fetal embryonic development, resulting in persistent herniation through the extra embryonal part of the umbilical cord which covers it. other abdominal organs may be included. there is also an increased incidence of associated abnormalities including cardiac disease. Foetal gastrointestinal abnormalities associated with polyhydramnios are generally those with impaired/absent swallowing - ie. atresias. Exomphalos: failure to return to cavity, associated with other abnormalities particularly cardiac and renal (possibly oligohydramnios). Gastroschisis, herniation, usually to right of umbilicus. Coverings in exomphalos make a difference to fluid/heat loss. Hypovolaemia, hypothermia, infection, adhesions, irritation by amniotic fluid, blood loss during surgery. Abdo compartment syndrome on closure prediced by abdo pressure > 20mmHg or CVP increase of 4mmHg. Reoperation for ischaemic gut, anuria, staged abdo closure. Exomphalos as a central defect of abdo wall is assoc with other midline developmental anomalies - including cardiac. Gastroschesis is thought to arise from vascular disruption of the right omphalmomesenteric artery and is more commonly an isolated defect. Both may be complicated by all the problems of external bowel - infection, fluid and electrolytes, temp, prematurity |
|
|
|
PP74 ANZCA version [2004-Apr] Q148, [2004-Aug] Q62, [Mar06] Q69, [Jul06] Q36, [Jul07]
A 20 kilogram child has a haemoglobin of 60 g.l-1. The child is normovolaemic and there is no on-going blood loss. The volume of packed cells required to increase the haemoglobin level to 100 g.l-1 is A. 80 ml B. 160 ml C. 320 ml D. 500 ml E. 750 ml |
ANSWER C
A simple solution is to use Frank Shann's equation: 4ml/kg of packed cells will increase Hb by 10g/L. Thus 4x20x4 = 320 mls (which is option C). |
|
|
|
PP55 ANZCA version [2001-Apr] Q91, [2002-Mar] Q83, [2002-Aug] Q69, [2005-Apr] Q89, [2005-Sep] Q65, [Mar06] Q58, [Jul07]
A 4-year-old child with obstructive sleep disorder presenting for tonsillectomy A. is likely to suffer from daytime somnolence B. is unlikely to have a history of snoring C. is suitable for day-case surgery D. has a 40% chance of postoperative vomiting without antiemetic treatment E. is likely to lose 5% of their blood volume during surgery |
ANSWER E
• A - False . ' in contrast to adults where daytime somnolence is common, this is not typical presenting complaint in children' • B - False. 'Most common symptoms in children with sleep apnoea are nocturnal snoring and noisy breathing' • C - False. • D - True. o Miller says 70% PONV. The presence of blood in the stomach & the need for opioids are a potent stimulus to vomiting, as are swelling and inflammation of the posterior pharynx & uvular. o The incidence of emesis after tonsillectomy can be as great as 60%.’ (Cote CJ et al (2001) A Practice of Anesthesia for Infants and Children, 3rd ed, p465) ref Ferrari LR, Donlon JV: Metoclopramide reduces the incidence of vomiting after tonsillectomy in children. Anesth Analg 1992; 75:351-354. • E - ? True o Miller p2187: "Blood loss during tonsillectomy is difficult to estimate and may reach 5% of estimated blood volume. Blood loss should be replaced if this exceeds 10-15% of blood volume." o For a 4 year old: • Weight = 2x(Age + 4) = 2x(4 + 4) = 16kg • Blood volume of child = 80mls/kg = 80x16 = 1280mls • 5% blood volume = 0.05 x 1280 = 64 mls • This blood volume is entirely conceivable given surgical blood loss. o Quote from the Australian Journal of Oto-Laryngology states "Overall intra-operative blood loss was an average of 18mls (range 0-150mls) or 1% of blood volume (range 0-8%)". |
|
|
|
PP54 ANZCA version [2001-Aug] Q69 [2006-Mar] Q90, [Jul06] Q87
Obstructive sleep disorder in children A. is associated with pulmonary hypertension and dysfunction of left and right ventricles B. has obesity as a major risk factor C. is rarely seen in children less than 8 years old D. is four times more prevalent in boys than girls E. does NOT usually require tonsillectomy for its management |
ANSWER A
#A. The mechanism appears to be: * Hypoxaemia and Hypercapnoea secondary to OSA lead to development of pulmonary hyperetension * PHT results in right ventricular dysfunction, remodelling and hypertrophy * Progressive tricuspid regurgitation and movement of the intra-ventricular septum lead to left ventricular outflow tract obstruction * LVOT obstruction results in left ventricular dysfunction and pulmonary oedema, which only exacerbates the hypoxaemia # B. has obesity as a major risk factor - partly true: Definitely a risk factor in the fat kiddies, but is it a major risk factor? * "Obesity, a typical feature of adults with OSA, is uncommon in children but if observed, may be associated with reduced daytime activity. More typically these children have poor weight gain and small stature." (Anaesthesia 1998; 53:571-579) # C. is rarely seen in children less than 8 years old - false: "Children usually present between 3 and 7 years of age" (Anaesthesia 1998; 53:571-579) # D. is four times more prevalent in boys than girls - false: "In contrast with adult OSA, in children there is an equal prevalence of affected boys and girls" (Anaesthesia 1998; 53:571-579) # E. does NOT usually require tonsillectomy for its management - false: "In most cases the definitive treatment of children with OSA syndrome is surgical by adenotonsillectomy" (Anaesthesia 1998; 53:571-579) |
|
|
|
PP84b ANZCA version [2005-Sep] Q141, [Mar06] Q85
Tracheo-oesophageal Fistula (TOF) A. is associated with cardiac anomalies in approximately 60% of cases B. is associated with oesophageal atresia in approximately 20% of cases C. is more common in males than females D. is usually left sided E. does not usually require contrast studies for diagnosis |
ANSWER E
# A. is associated with cardiac anomalies in approximately 60% of cases - false * Approx 27% (Table 2) # B. is associated with oesophageal atresia in approximately 20% of cases - false: * Higher association approx 96% # C. is more common in males than females - false # D. is usually left sided # E. occurs in approximately 1 in 3500 live births - true: * " The incidence of OS/TOF is 1 in 3500 live births." |
|
|
|
PP88 ANZCA Version [Jul06] Q131, [Jul07]
The glomerular filtration rate of a paediatric patient (in ml.min-1.m-2) is similar to that of an adult by the age of approximately A. 1 month B. 6 months C. 2 years D. 4 years E. 6 years |
ANSWER C
|
|
|
|
PP90 ANZCA Version [Jul06] Q142, [Apr07] Q8
A 12-year-old boy with spastic cerebral palsy and painful muscle spasms presents for multilevel osteotomies of his legs. The most effective option for post-operative analgesia would be A. a combination of NSAIDs (non-steroidal anti-inflammatory drugs) and regular tramadol B. continuous lumbar epidural analgesia with a mixture of local anaesthetic and clonidine C. regular paracetamol and oxycodone D. patient controlled morphine E. spinal morphine |
ANSWER B
Children undergoing single event multilevel surgery present specific difficulties. Our initial experience was with continuous epidural infusion of 0.125% bupivacaine and fentanyl 2 mg.ml at 0.2 – 0.3 ml.kg.h postoperatively. Analgesia was good, but spasm was frequent, necessitating 4-hourly administration of diazepam. Patients would often have postoperative nausea and vomiting resistant to anti-emetics, resulting in plain bupivacaine 0.125% replacing the combined bupivacaine/fentanyl solution. Subsequently we have been using bupivacaine 0.125% with clonidine 2.5 mg.ml at 0.2 –0.3 ml.kg.h |
|
|
|
PP91 ANZCA Version [Jul06] Q124, [Apr07] Q2
An otherwise healthy 4-year-old presenting for adenotonsillectomy develops a cough and laryngospasm during gaseous induction. At intubation clear secretions are visible at the glottis and after intubation transient wheezing is noticed. Clear fluid is aspirated from the endotracheal tube. At the end of the case, the child has a SpO2 of 96% with an FiO2 of 0.3. Airway pressures are normal. The most appropriate further management of this suspected aspiration is to A. administer broad spectrum antibiotics and otherwise manage routinely B. administer steroids and extubate after 1 hour if chest is clear on auscultation C. extubate and observe in recovery for 4-6 hours D. measure pH of tracheal aspirate and base further management on findings E. perform on-table chest X-ray and base further management on findings |
ANSWER ??? Common sense and what we do in practice is C, But the Best Practice Article refers to D and E as possible answers.
Best Practice Articles, Crisis management during anaesthesia: regurgitation, vomiting, and aspiration A chest radiograph should always be obtained if aspiration is suspected. There is no evidence that intravenous steroids have a place in treatment, and one patient convulsed after the injection of a large dose of intravenous dexamethasone. Antibiotics should not be used prophylactically but should be used if and when a specific organism is identified.11 If the patient is stable, the saturation is greater than 95% with an inspired oxygen concentration of less than 50%, the heart rate is less than 100 beats/min (in adults), the respiratory rate is less than 20/min (in adults), and the patient is apyrexial and requires minimal bronchodilators, then discharge to a general ward with appropriate monitoring is acceptable. If these criteria are not satisfied at 2 hours, the patient should be admitted to an intensive care or high dependency unit. D. "Now that children do not commonly receive an anti-cholinergic premed, seeing some secretions in the pharynx on intubation is a common occurrence and these will in most cases just be upper airway secretions. If there is any doubt about the nature of the secretions I would just sample and test with litmus paper. Similarly with any secretions aspirated from the tube. If not pink, then its not acid and "acid aspiration" is simply excluded. How could "anyone" (as in this question) proceed without doing such a simple, useful, low-cost, readily available test??" E. best practice article, management of aspiration 2006 it states that " a Chest xray should be done as soon as possible in any case of suspected pulmonary aspiration to specify the pulmonary pathology. However it must be pointed out that in approximately 25% of cases radiographic signs of aspiration are not present. |
|
|
|
PP79b ANZCA version [2005-Sep] Q143, [Jul07] [Apr 07]
Pneumonia in children A. if staphylococcal, is commonly associated with a pleural effusion B. is commonly caused by mycoplasma pneumoniae in young children C. is most commonly caused by streptococcus pneumoniae D. is rarely caused by chlamydia trachomatis in neonates E. often presents as lethargy without fever or cough |
ANSWER A
Causative bugs in paediatric pneumonia *90% viral (mostly RSV) *10% bacterial - bug depends on age of child: -Pneumococcal - older children - 90% of bacterial paediatric pneumonia -Haemophilus influenzae - all ages -Staph - younger than one, and usually sick/debilitated infants -Mycoplasma - ages 5 - 15 -Pneumocystis - immunocompromised Neonatal pneumonia * may be contracted in-utero, or aquired during birth * usually bacterial - GBS, gram neg bacilli (e coli, klebsiella, pseudomonas), listeria, staph, rarer bugs are anaerobic bacilli and chlamydia Mycoplasma causes an 'atypical pneumonia' with influenza-like respiratory illness of gradual onset with headache, malaise, fever, cough Pneumococcal pneumonia is the most common typical bacterial pneumonia in children of all ages. In one retrospective review of 254 children and young adults (age <1 month to 26 years) with pneumococcal pneumonia, the most common signs and symptoms and their approximate frequencies are listed below: • Fever: 90 percent, • Cough: 70 percent; • Productive cough: 10 percent • Tachypnea: 50 percent |
|
|
|
PP79a ANZCA version [2004-Aug] Q103, [Jul07]
Pneumonia in children A. if bacterial is commonly associated with a pleural effusion B. is often caused by Mycoplasma Pneumoniae in infants C. is rarely caused by Chlamydia Trachomatis in neonates D. is rarely fatal in developed countries E. often presents as lethargy without fever or cough |
ANSWER A
Causative bugs in paediatric pneumonia *90% viral (mostly RSV) *10% bacterial - bug depends on age of child: -Pneumococcal - older children - 90% of bacterial paediatric pneumonia -Haemophilus influenzae - all ages -Staph - younger than one, and usually sick/debilitated infants -Mycoplasma - ages 5 - 15 -Pneumocystis - immunocompromised Neonatal pneumonia * may be contracted in-utero, or aquired during birth * usually bacterial - GBS, gram neg bacilli (e coli, klebsiella, pseudomonas), listeria, staph, rarer bugs are anaerobic bacilli and chlamydia Mycoplasma causes an 'atypical pneumonia' with influenza-like respiratory illness of gradual onset with headache, malaise, fever, cough Pneumococcal pneumonia is the most common typical bacterial pneumonia in children of all ages. In one retrospective review of 254 children and young adults (age <1 month to 26 years) with pneumococcal pneumonia, the most common signs and symptoms and their approximate frequencies are listed below: • Fever: 90 percent, • Cough: 70 percent; • Productive cough: 10 percent • Tachypnea: 50 percent |
|
|
|
PP63c ANZCA Version Apr07
A six-week-old baby is booked for elective right inguinal hernia repair. An appropriate fasting time is A. 2 hours for breast milk B. 4 hours for formula C. 5 hours for breast and formula D. 6 hours for solids E. 8 hours for solids and 4 hours for all fluids |
ANSWER B
C. is also true, but a 6 week infant would not be on solids College Guidlines: Fasting Fluid : 2 hours Milk: 4 hours Solids: 6 hours |
|
|
|
PP63b ANZCA version [2005-Sep] Q121, [Apr07] Q103
A six-week-old baby is booked for elective right inguinal hernia repair. An appropriate fasting time is A. 2 hours for formula milk B. 2 hours for clear fluids C. 5 hours for breast and formula milk D. 6 hours for solids E. 6 hours for solids and 3 hours for all fluids |
ANSWER B
C. is also true, but a 6 week infant would not be on solids |
|
|
|
SZ25 [Apr07]
A six year old boy requires return to theatre for arrest of post-tonsillectomy haemorrhage. When anaesthetising for this procedure it is important to: A. avoid sedative premedication prior to induction B. avoid volatile anaesthesic agents C. have duplicate suction apparatus and ETTs available D. use an uncuffed endotracheal tube in this age group E. RSI |
ANSWER C
A. Truish B. False C. True - CCEAP article "Before induction, in addition to the standard equipment, a selection of laryngoscope blades, smaller than expected tracheal tubes, and two suction catheters should be immediately available" D. False. Not necessarily. E. False - can do RSI or SV gas induction on side |
|
|
|
PP31 ANZCA version [Aug93] [Apr96] [Aug96] [Apr97] [Jul97] [2005-Apr] Q77, [2005-Sep] Q78, [Jul07], [Mar10]
In congenital diaphragmatic hernia A. there is hyperplasia of pulmonary arterioles in the hypoplastic lung B. right-sided lesions are more pathologically significant C. vasodilator drugs are contraindicated D. right-sided lesions through the foramen of Bochdalek are the most common E. intrapulmonary shunts are the major cause of cyanosis |
ANSWER A
A TRUE B. FALSE. Left sides lesions are larger and associated with more pulmonary hypoplasia C. FALSE D. FALSE: 90% are left posteriorlateral E. FALSE extrapulmonary Right to Left shunting is more common due to the pulmonary hypertension, and consequent shunting via a patent DA. |
|
|
|
MN44 ANZCA version [2005-Sep] Q99
Cerebral palsy is associated with each of the following EXCEPT A. gastro-oesophageal reflux B. increased sensitivity to non-depolarising muscle relaxants C. malnutrition D. recurrent aspiration E. scoliosis |
ANSWER B
Cerebral Palsy associated with increased sensitivity to depolarising NMBDs and resistance to non-depolarising NMBDs. (Morgan & Mikhail) |
|
|
|
PP93 [Apr07] Q124
The Neonatal Facial Coding Scale (NFCS) used to assess pain in neonates includes all of the following except A. Brow bulge B. Chin quiver C. Closed mouth D. Deep nasolabial fold E. Eyes squeezed shut |
ANSWER C
Neonatal Facial Coding System (NFCS) actions monitored: * (1) brow lowering (lowering and drawing together of the brow can result in brow bulge) * (2) eyes squeezed shut * (3) deepening of the naso-labial furrow (fold) * (4) open lips (any separation of the lips is an occurrence) * (5) vertical mouth stretch * (6) horizontal mouth stretch * (7) taut tongue (cupping of the tongue) * (8) chin quiver (high frequency vibration of the chin and lower jaw) * (9) lip pursing (tightening the muscles around the lips to form an "oo") In addition a tenth activity was monitored in preterm infants: * (10) tongue protrusion (this is a "no pain" response in full term infants) |
|
|
|
PP92 [Apr07]
5yo 35kg child having repair of leg laceration. gas induction with sevo N2O and oxygen. Can't get in drip. Put in LMA and immediately get stridor and airway obstruction and desaturate to 90%. Next step after increase FiO2 to 100% is: A Remove LMA and deepen with sevoflurane B Leave LMA and deepen with sevoflurane C Intralingual Suxamethonium D IM Atropine E IM Suxamethonium |
ANSWER A
|
|
|
|
PP58a ANZCA version [2002-Mar] Q74
Spinal anaesthesia in infants A. often causes hypotension if the infant is awake B. has a lower failure rate than in adults C. eliminates the risk of postoperative apnoea D. lasts for a longer time than in adults E. may be performed at a higher spinal level than in adults |
ALL FALSE
|
|
|
|
PP58b ANZCA version [2003-Aug] Q114, [2004-Apr] Q32, [2005-Apr] Q24, [2005-Sep] Q38, [Jul07]
Spinal anesthesia in infants A. eliminates the risk of postoperative apnea B. has a lower failure rate than in adults C. lasts for a shorter time than in adults D. may be performed at a higher level than in adults E. often causes hypotension if the infant is awake |
ANSWER C
* Proven to reduce risk of apnoeas * Failure rate of 20% * Duration 20-60 minutes (the answer) * Spinal cord terminates more inferiorly (L3) |
|
|
|
A 25 kilogram child has a haemoglobin of 65 g.l-1. The child is normovolaemic and there is no on-going blood loss. The volume of packed cells required to increase the haemoglobin level to 90 g.l-1 is
A. 100 ml B. 150 ml C. 250 ml D. 350 ml E. 450 ml |
ANSWER C
Frank Shan 4 x 2.5 x25 = 250ml |
|
|
|
ANZCA Version [Jul07]
You are commencing general anaesthesia for a 2-year-old child to allow biopsy of an anterior mediastinal mass, A pre-operative CT scan demonstrated compression of the lower trachea and the carina by Ihe mass. During inhalational induction, the child desaturates to 70% due to airway compression by the mass. You should A. apply continuous positive airway pressure (CPAP) via facemask B. arrange urgent median sternotomy C. intubate the patient and allow spontaneous ventilation D. intubate the patient and provide positive pressure ventilation E. place the patient in the prone position |
ANSWER E
|
|
|
|
ANZCA Version [Jul07]
With respect to gastric volumes and fasting in children, A. casein-predominant milks empty faster than whey-predominant milks B. children have a higher incidence of aspiration than adults C. solids rely on first order kinetics for gastric emptying but liquids follow zero order kinetics D. the rate of gastric emptying is NOT related to the energy content of the meal E. unlimited clear fluid ingestion 2 hours before surgery does NOT affect volume, but does affect the pH of stomach contents |
ANSWER B
A: FALSE: Human milk and whey predominant formula empty faster than casein predominant formular and cow's milk. Probably due to lower protein content in human and whey based milk. B. Paediatric aspiration is slightly more common than in adults (1 per 1200–2600 compared to 1 per 2000–3000 in adults) C. FALSE: Solids follow zero order (linear decay) kinetics and liquids first order (exponentail decay) D. FALSE E. FALSE: Clear fluids up to 2 hrs preop do not increase gastric volume or signiicantly change gastric pH (there may be an increase in pH with clear fluids up to 2 hrs) |
|
|
|
PP95 [Jul07]
A one year old child arrests with VT. Has had 2x DC shocks, and 100 mcg adrenaline. Further 1x DC shock given. What is next step? A. 20 J DC shock B. 40 J DC shock C. 50 mg amiodarone D. 100 mcg adrenaline E. 1000 mcg adrenaline |
ANSWER C
|
|
|
|
PP96 [Jul07]
Newborn with diaphragmatic hernia. Initially sats 95% on RA. Now beginning to develop respiratory distress. Next appropriate step: A. Awake intubation B. Trial NO prior to intubation and ventilation C. Rapid sequence induction D. Mask ventilation throughout case with CPAP E. Gas down with CPAP |
ANSWER A
Miller, Yao and Artusio, and Morgan Mikhail all say awake intubation Assumption: this occurs immediately post delivery Problems 1. pt has pulmonary hypoplasia and pulmonary HTN with a transitional circulation apnoea, hypoxia and hypercarbia will lead to reversal of shunts If this neonate is desaturating, it needs to be intubated immediately. Waiting for IV access (difficult in a neonate) may not be possible. However, awake intubations due increase risk of ICH (neonates are already at risk of this, this increases the risk further) |
|
|
|
PP99 ANZCA version [Jul07] q128
A 6-year-old child is referred via the orthopaedic clinic for closed reduction under general anaesthesia of a forearm fracture, sustained 2 days earlier. He is an asthmatic, usually well controlled, but has a current upper respiratory tract infection. He is on salbutamol 2 puffs twice a day, and on auscultation his chest is clear. He is adequately fasted and can proceed to theatre immediately. The best choice for airway management of this child is A. endotracheal intubation and controlled ventilation B. endotracheal intubation and spontaneous ventilation C. facemask and spontaneous ventilation D. laryngeal mask airway and spontaneous ventilation E. ProsealTM laryngeal mask airway and spontaneous ventilation |
ANSWER C
|
|
|
|
PP100 ANZCA version [Jul07] q135
Regarding the normal term infant A. foetal haemoglobin (HbF) comprises approximately one-third the total haemoglobin at birth and falls to negligible levels by 3 months of age B. foetal haemoglobin (HbF) comprises approximately 70% of the total haemoglobin at birth and falls to negligible levels by 6 months of age C. haemoglobin level below 90g.l-1 at 9-12 weeks (physiological anaemia) is common and does NOT require investigation D. normal haemoglobin at birth should be greater than 200g.l-1 unless there has been delay in umbilical cord clamping E. total blood volume is approximately 70 ml.kg-1 body weight |
ANSWER B
|
|
|
|
ANZCA Version [Jul 07] Q.147
A 4y.o. boy presents for insertion of grommets. His maternal great-grandfather is know to have had an episode of malignant hyperthermia. Which of the following is the strongest evidence that the boy is NOT susceptible to MH? A. the boy was exposed to halothane at age 2 with no sequelae B. the boy has recently been shown to have a normal serum creatinine kinase C. the boy's grandfather has had a negative muscle contracture test for MH D. the boy's mother has had negative molecular genetic testing for MH E. there have been NO other episodes of MH in the family despite exposure to known triggers on multiple occasions |
ANSWER C
|
|
|
|
ANZCA Version [Jul 07] Q.147
A 4y.o. boy presents for insertion of grommets. His maternal great-grandfather is know to have had an episode of malignant hyperthermia. Which of the following is the strongest evidence that the boy is NOT susceptible to MH? A. the boy was exposed to halothane at age 2 with no sequelae B. the boy has recently been shown to have a normal serum creatinine kinase C. the boy's grandfather has had a negative muscle contracture test for MH D. the boy's mother has had negative molecular genetic testing for MH E. there have been NO other episodes of MH in the family despite exposure to known triggers on multiple occasions |
ANSWER D
The ideal anaesthestic if you decide to do the child with URTI is "minimally invasive". I.e. if you can use a face mask use one, if you can use an LMA use one as instrumentation of the reactive airway can get you into trouble. |
|
|
|
PP When using a T piece for a small child, which is not an advantage?
A. Can use low gas flows B. Feel compliance C. Assess tidal volume D. Can rapidly change levels of CPAP E. low resistance |
ANSWER A
|
|
|
|
PP Haemoglobin in infants:
A. 30% fetal Hb at birth, adult levels by 3 months B. 70% fetal Hb at birth, negligible amounts by 6 months C. Hb 90 at 6 months normal doesn't need Ix D. Hb 200 at birth unless delayed cord clamping E. ? |
ANSWER B
|
|
|
|
PP (Q139 Aug 2008) Arrest in a 10 year old. Has ventricular tachycardia after a near drowning accident. Patient is intubated and is being ventilated with 100% O2 and has IV access. A single DC monophasic shock of 60J has been given. The next step is to give
A adrenaline 10mcg/kg and DC shock 60J B adrenaline 10mcg/kg and DC shock 120J C amiodarone 5mg/kg D DC shock 60J E DC shock 120J |
ANSWER B
|
|
|
|
PP (Q150 Aug 2008) 6 month old baby for VSD repair. Induced with 50% N2O, O2, sevoflurane 8%. While obtaining IV access, the patient desaturates to 85%. The manouevre to increase the O2 saturations is to
A give a fluid bolus B change from sevoflurane to isoflurane C institute CPAP D decrease the FiO2 E reduce the sevoflurane concentration |
ANSWER E
PVR/SVR ratio determining R-->L shunt |
|
|
|
Neonate if febrile with rash and periodic breathing. which is likely ABG?
a) metab acidosis resp acidosis b) metab acidosis compensated c) resp acidosis d) alkalosis e) alkalosis |
ANSWER A
|
|
|
|
2 month old systolic murmur heard at apex no change with posture, now on 5th centile for weight after being on 30th at birth, mother states has difficulty feeding. Peripheral pulses reduced femoral more than upper body. Most likely cause:
A. HOCM B. VSD C. PDA D. venous hum E. ASD |
ANSWER C
PDA - collapsing pulse with sharp upstroke from ejection of large volume of blood into empty aorta during systole, low diastolic pressure due to rapid decompression of aorta, hyperkinetic apex, single S2 if large or even reversed splitting of S2, continous loud "machinary murmur at 1st LIC space. sometimes associated with flow murmur through left heart eg. mitral mid diastolic murmur. |
|
|
|
18/12 old undergoing routine SV GA under LMA. Sudden onset SVT with HR 220 BP 84/60 ETCO2 32 SpO2 98.Management:
A. Adenosine 100mcg B. DCR 2J/kg C. DCR 4J/kg D. Amiodarone 5mg/kg E. CPR |
ANSWER A
Management of SVT in a child: • Attempt valsalva maneuvers as able by child, ie; forceful cough, cold packs on face and neck, or blow through a straw • Establish IV/IO NS. Do not withhold IO if unable to start IV promptly and child is unstable • If unable to maintain airway, consider endotracheal Intubation • If child is rapidly deteriorating perform immediate synchronized cardioversion at 0.5J/kg. Consider pain management or sedation • If time allows may try Adenosine first at 0.1mg/kg IV or IO, being sure to administer rapidly and follow with a rapid fluid flush. During administration, record a rhythm strip. • Consider Amiodarone. |
|
|
|
36.
4 yr old presents for elective surgery, otherwise fit healthy, murmur at left sternal edge on auscultation heard in systole and diastole, disappears on lying down. Most likely cause: A. HOCM B. VSD C. PDA D. venous hum E. ASD |
ANSWER D
Venous Hum - systolic + diastolic components, not really a murmur. Benign medical condition where 20% of the blood flow travels to the brain and back to the heart. Due to the large amount of blood it can move quite fast causing the vein walls to vibrate which can create a humming noise to be heard by the patient.The murmur disappears when the patient is in the supine position. |
|
|
|
What is the appropriate LMA size for an 8kg child:
A. 1 B. 1.5 C. 2 D. 2.5 E. 3 |
ANSWER B
LMA sizes (Drug Doses Frank Shann Book) <5kg = 1, 5-10kg = 1.5, 10-20kg = 2, 20-30kg = 2.5, 30-50kg = 3.0, 50-70kg = 4.0, 70-100kg = 5.0, >100kg = 6 |
|
|
|
Neonate born to known drug abusing mother brought to emergency department by grandmother, unwell lethargic, slightly jaundiced, ABG shows following:
pH 7.52 Na 135 Cl 87 K 3 pCO2 38 Which of the following is the Diagnosis? A) Septicaemia B) Hepatitis C) Pyloric stenosis D) Pneumonia E) Opioid withdrawl |
ANSWER C
Hypokalaemic, hypochloraemic metabolic alkalosis; classic for pyloric stenosis. The other stuff is probably a distraction. |
|
|
|
15kg child found fitting on paeds ward ?24h ?48h postop while on infusion of 60ml/h ½ NS + Dextrose. Now intubated. Na is 119, next management step:
A) frusemide B) hypertonic saline C) Normal saline at 20ml/hr D) Water restrict E) Phenytoin |
ANSWER B
Acute symptomatic hyponatraemia. Aim to raise serum Na by 2mmol/hr until symptom resolve. Complete correction is unnecessary, although not unsafe. Infuse hypertonic saline (3% NaCl) at a rate of 1.2-2.4ml/kg/hr through a large vein... If there are severe neurological symptoms, eg seizure, coma, 3%NaCl may be infused at 4-6ml/kg/hr. Electrolyte should be carefully monitored. |
|
|
|
17. (Variation of old Question). Paediatric ALS – 20 kg, VF has had 2 shocks only. Next step
a. Adrenaline b. Amiodarone c. Shock 50J d. Shock 100J |
ANSWER A
|
|
|
|
35. (NEW) Emergence delirium in a kid in recovery. NOT used to treat
a. Fentanyl 1mc/kg b. Midazolam 0.1 mg/kg c. Propofol d. Clonidine 1mc/kg e. Sucrose |
ANSWER E
Fentanyl IV 1–2 µg/kg (22), propofol IV 0.5–1.0 mg/kg (39), and midazolam IV 0.02–0.10 mg/kg (12,84) have all been used for the treatment of ED. A single bolus dose of dexmedetomidine 0.5 µg/kg was also shown to be efficient in the PACU for ED (85). Perhaps in the age group likely to get ED, sucrose probably isn't going to do the trick as usually that's reserved for the neonates. |
|
|
|
AZ73 ANZCA version [2004-Apr] Q127, [2005-Apr] Q52, [2005-Sep] Q7 [2009-Aug]q76
A fourteen-year-old girl is scheduled to have a termination of pregnancy. With regard to consent for this procedure, which of the following statements most truly reflects the law in Australasia? A. A fourteen-year-old girl is able to give consent independently of her parents/guardians if she is considered, by her treating doctors, to be of sufficient maturity to understand the issues. B. A fourteen-year-old girl is able to give consent independently of her parents/guardians only if a court deems her sufficiently mature. C. Minors are not able to give consent, independently of parents/guardians, until sixteen years of age. D. Minors are not able to give consent, independently of parents/guardians, until eighteen years of age. E. Only life-saving treatment may be administered to a fourteen-year-old without parental/ guardian consent. |
ANSWER A
The Gillick-competence test 2.7 A young person under 18 years of age is legally competent to consent to medical treatment if he or she is capable of understanding the nature and consequences of that treatment. The High Court of Australia settled this common law test for determining a young person’s competence in a case commonly known as Marion’s case. The majority of the Court held that: A minor is capable of giving informed consent when he or she achieves a sufficient understanding and intelligence to enable him or her to understand fully what is proposed.10 The majority in Marion’s case followed a decision of the English House of Lords in Gillick v West Norfolk and Wisbech Area Health Authority.11 In Gillick, it was held that a young girl was competent to consent to contraceptive advice and treatment if she had a sufficient understanding and intelligence to enable her to understand fully what was proposed.12 2.8 The test focuses on an assessment of the individual young person’s level of maturity and understanding in relation to the treatment proposed. This means that, before the age of 18 (when a young person legally becomes an adult), there is no fixed age at which it is possible to say, in advance of such an assessment, that a young person is automatically capable of consenting to medical treatment generally, or to specific types of medical treatment. Thus, while a young person of, say, 10 years of age may have the necessary intelligence and understanding of what is proposed to consent to the administration of a course of antibiotics to treat a sore throat, he or she may not, at the same time, possess sufficient understanding to consent to the removal of his or her tonsils in the case of acute tonsillitis. In short, before the age of majority, competence to consent operates on a continuum which ranges from the point at which a young person is clearly able to consent to the medical treatment proposed to that at which he or she is clearly unable to do so. 2.9 The test may prove difficult for medical practitioners, with whom the assessment of Gillick-competence initially rests, to apply in practice. The imprecision of the test places a significant onus on that assessment.13 Medical practitioners sued for providing medical treatment to a young person without consent bear the onus of proving that they believed that the young person was of sufficient maturity and understanding to consent to the treatment in question. |
|
|
|
MC157 [Mar10] [Aug10]
An 18 yo with Fontan circulation undergoing exploratory laparotomy. On ICU ventilation, saturation is 70%. Which ventilator parameter would you INCREASE to improve his saturation? A. Bilevel pressure B. Expiratory time C. Inspiratory time D. Peak inspiratory pressure E. PEEP |
ANSWER B
During IPPV a DECREASE in inspiratory time (which means an INCREASE in expiratory time) will improve pulmonary blood flow - despite the increased peak airway pressures. |
|
|
|
SC33 [Mar10] [Aug10]
A 7 kg Infant with tetralogy of Fallot, post Blalock-Taussig shunt. Definitive repair at later date. Paralysed and vetilated. Baseline saturation 85%, now 70%, BEST treatment: A. Increase FiO2 from 50 to 100% B. Esmolol 70 mcg C. Phenylephrine 35 mcg D. Morphine 1 mg E. 1/2 NS with 2.5% dextrose 70 mls |
ANSWER C
Frank Shann's dose recommendation for phenylephrine is 2-10 mcg/kg as a bolus, which would fit nicely with C (5mcg/kg). It'd be nice to do A too, but I'd say C is more effective. |
|
|
|
TMP-107 [Mar10] [Aug10]
Baby with Tracheo-oesophageal fistula found by bubbling saliva and nasogastric tube coiling on Xray. BEST immediate management? A. Bag and mask ventilate B. Intubate and ventilate C. position head up, insert suction catheter in oesophagus (or to stomach?) D. Place prone, head down to allow contents to drain E. Insert gastrostomy |
ANSWER C
* A - FALSE. Not unless the baby is in respiratory distress and/or hypoxic. May inflate stomach by ventilating through fistula. * B - FALSE. Just because the baby has been diagnosed with TOF is not an immediate indication for intubation in and of itself. * C - TRUE. Neonates with TOF should have a "nasogastric" tube inserted into the oesophageal stump to drain secretions and prevent accumulation in the blind-end pouch. The NGT should be connected to continuous suction. The infant should be nursed prone or in the lateral position with 30 degrees head up tilt to decrease the risk of aspiration. See A Practice of Anesthesia for Infants and Children - 4th edition by Cote, Lerman, Todres; p.755. Saunders (2009) * D - FALSE. Can nurse prone, but lateral with head up tilt seems to be the recommended and most commonly cited method. * E - FALSE. Initial management as above (see C - TRUE), and then repair. Gastrostomy may be performed, but not best immediate management. |
|
|
|
PP69 ANZCA version [2003-Aug] Q93, [2004-Apr] Q3
The commonest congenital cardiac defect is A. coarctation of the aorta B. patent ductus arteriosus C. pulmonic stenosis D. transposition of the great vessels E. ventricular septal defect |
ANSWER E
VSD 32% PDA 12% ASD 6% TGA 5% |
|
|
|
PN48 [Mar10] [Aug10]
Why is codeine not used in paediatrics? A. Poor taste B. High inter-individual pharmacokinetic variability C. Not licensed for children < 10 years old D. Not as effective as adult when given in ?weight adjusted dose? E. ? |
ANSWER B
* A - As far as I am aware it doesn't have a particularly nasty taste, and is used in cough suppressants, so FALSE. * B - TRUE. Variations in CYP2D6 function affect how much codeine is converted to morphine, and therefore how effective it is, but also how "sensitive" patients are to codeine. * C - Painstop was used in children when I was an RMO a few years ago and contains codeine, and as far as I know it is still used, but I don't know the specific licensing info for codeine in paeds. It is not used in our hospital, but mostly because we use oxycodone instead.- You can still buy it OTC. We have some at home. (Because you can't buy oxycodone OTC!) * D - ? False. It's crap in children just like it's crap in adults isn't it! |
|
|
|
TMP-128 [Aug09] [Mar10] [Aug10]
Indication for percutaneous closure of ASD A. Ostium primum < 3cm B. Ostium primum > 3cm C. Ostium secundum < 3 cm D. Ostium secundum > 3cm E. Sinus venosus ASD |
ANSWER C
|
|
|
|
TMP-Jul10-020
Thermoneutral zone in 1 month old infant ? A. 26 – 28 degrees Celcius B. 28 – 30 degrees Celcius C. 30 – 32 degrees Celcius D. 32 – 34 degrees Celcius E. 34-36 degrees celcius |
ANSWER D
|
|
|
|
TMP-Jul10-022 A 4 year old child with VSD (repaired when 2 years old) for dental surgery. What antibiotic prophylaxis do the guidelines recommend?
A. Amoxycillyn orally B. Amoxycillin IV C. Cephazolin IV D. Amoxycillin / gentamicin E. No antibiotics required |
ANSWER E
|
|
|
|
TMP-Jul10-023 A 4 year old child with Arthrogrophysis multiplex congenita for dental surgery. Jaw rigidity post induction. Likely cause ?
A. Temporomandibular joint involvement/ TMJ rigidity B. Inadequate depth of anaesthesia C. Inadequate muscle relaxation/ inadequate sux D. Masseter spasm E. ? |
ANSWER ??
Any condition that impairs in utero movement for > 3 wk can result in AMC. Causes may involve * Physical limitation of movement (eg, due to uterine malformations, multiple gestations, oligohydramnios) * Maternal disorders (eg, multiple sclerosis, impaired uterine vascularity) * Fetal disorders (eg, neuropathies; myopathies, including muscular dystrophies; connective tissue abnormalities; impaired fetal vascularity; anterior horn cell disease) Patients with arthrogryposis have micrognathia, a high arched palate, and a short and rigid neck making tracheal intubation difficult and at times impossible. The primary concern to the anesthesiologist is the potential for airway involvement thereby making direct laryngoscopy and endotracheal intubation difficult. Direct laryngoscopy and intubation become more difficult as the patient ages because craniofacial involvement often progresses with growth. Alternatives to direct laryngoscopy and tracheal intubation, such as the use of the laryngeal mask airway, with or without the use of a tube exchanger, or fiberoptics, have been used successfully in this disorder. In such difficult airway scenario we decided to avoid intubation and maintained her on spontaneous ventilation. We kept difficult intubation cart ready in case required to secure airway in emergency. The extensive contractures, tense skin, and minimal muscle mass and subcutaneous tissue pose challenges for intraoperative positioning and intravenous access. Children with arthrogryposis may have altered responses to neuromuscular relaxants and are akin to other patients with anterior horn cell diseases. Response to nondepolarizing relaxants has been reported to be extremely variable, the use of short-acting nondepolarizing agents in association with careful monitoring of neuromuscular function has been advocated in these patients. |
|
|
|
PP86 ANZCA version [2005-Sep]Q118 | Aug10
A three-week old infant presents with pyloric stenosis and 3 days of vomiting. A typical electrolyte profile would be A. Na+ 130 mmol.l-1 K+ 5.8 mmol.l-1 Cl- 98 mmol.l-1 HCO3- 17 mmol.l-1 B. Na+ 148 mmol.l-1 K+ 4.1 mmol.l-1 Cl- 108 mmol.l-1 HCO3- 13 mmol.l-1 C. Na+ 135 mmol.l-1 K+ 4.5 mmol.l-1 Cl- 90 mmol.l-1 HCO3- 30 mmol.l-1 D. Na+ 130 mmol.l-1 K+ 2.8 mmol.l-1 Cl- 90 mmol.l-1 HCO3- 28 mmol.l-1 E. Na+ 130 mmol.l-1 K+ 3.9 mmol.l-1 Cl- 98 mmol.l-1 HCO3- 17 mmol.l-1 |
ANSWER D
|
|
|
|
31. NEW. Which of the following causes the most heat loss in a neonate?
A: conduction B: convection C: evaporation D: radiation E: vasodilation |
ANSWER D
|
|
|
|
37. New (?). Eisenmengers syndrome:
A: decrease Hb to <180 with venesection B: Give high FiO2 C: Pulmonary vasodilators will treat the pulmonary hypertension D: terminal RV failure usually occurs in the 3rd-4th decade |
MEDICAL CARE
1. Avoid sudden fluids shift or dehydration -> increase R->L shunt 2. Avoid very hot or humid climited -> exacerbate vasodilation causing syncope 3. Oxygen therapy: no impact on exercise capacity and survival 4. Pulmonary vasodilators: similar to idiopathic PAH. -shown to improve oxygenation -improve 6MWT -improve NYHA class -no improvement in mortality 5. Anticoagulation -incidence of PE 21% -however, increased bleeding risk due to dysfunctional platelets -Hct>65% should have preop venesection 6. Pregnacy -avoidance, tubual ligation strongly recommeded -fetal mortality 25% -maternal mortality 50% |
|
|
|
38. NEW. Your registrar gives a Duchenne patient 1mg/kg of suxamethonium. What are you most worried about?
A: hyperkalaemia B: rhabomyolysis C: MH |
ANSWER A and B
o Sux: Hyperkalaemia, rhabdo o NDMR: safe but reduced dose, prolonged block |
|
|
|
PP94 [Apr07]
A 25kg child is having liver resection and is rapidly given 1 unit of blood. Her CVP is 8. The cause most likely to be responsible for any haemodynamic instability she experiences is: A. coagulopathy B. hyperkalaemia C. ABO incompatability D. Hypocalcaemia E. Hypothermia |
ANSWER B
|
|
|
|
PP89 ANZCA Version [Jul06] Q115
An 8-year-old boy who is wheelchair bound with cerebral palsy and spastic quadriplegia is booked for an MRI (magnetic resonance imaging), under general anaesthesia for a rapid deterioration in his epilepsy control. On arrival to the MRI suite (with no premedication) he is distressed and inconsolable. Immediate management of this situation should include A. an inhalation induction with parental/carer presence B. cancellation and rescheduling with sedative premedication C. cancellation of procedure until epilepsy is better controlled D. detailed discussion with parents/carer regarding anaesthetic options E. intramuscular or oral ketamine induction |
ANSWER D
|
|
|
|
PP87 ANZCA Version [Jul06] Q107
The weight of a child can be estimated using the formula A. (age + 2) x 3 B. (age + 4) x 2 C. (age x 2) + 4 D. (age x 3) + 2 E. age x 4 |
ANSWER B
The "standard" anaesthetic formula are: * From age 1-8: wt= (age in years x 2) + 8 [which is equal to (age+4)x2] * From age 8-12 wt = (age in years) x 3 For practical use though, a simple easy-to-remember guide that I made up is the "1-6-10 rule": * At age 1 yrs -> 10kgs * At age 6 yrs -> 20kgs * At age 10yrs -> 30kgs And for the in-between years: * From 1->6, add 2kgs/yr * From 6->10, add 2.5kgs/yr Another rule of thumb for >1yr old is (2x Age)+9 until 9yrs old, and 3x Age thereafter. |
|
|
|
PP85 [2004-Aug] Q149
Signs of severe dehydration in an infant include each of the following EXCEPT A. elevated pulse rate B. marked oliguria C. pale skin colour D. parched mucous membranes E. reduced blood pressure |
ANSWER E
From BJA review, ref below on assessment of dehydration Appearance: * Mild - Thirsty, restless, alert. * Moderate - Thirsty, restless or lethargic but rousable, pale (BP - Normal/low) * Severe - Drowsy to comatose, limp, cold, sweaty, grey, cyanosed ( BP - Low) Hypotension is very late sign. |
|
|
|
PP82 ANZCA version [2004-Aug] Q143
Post-dural puncture headaches (PDPH) in children A. are less effectively treated by a blood patch (compared to adults) B. are rare in children under 10 years of age C. have an incidence of approximately 5% to 12% following spinal anaesthesia D. have an incidence which is independent of needle gauge E. presents with signs which are not posturally related |
ANSWER B
* A. are less effectively treated by a blood patch (compared to adults) - probably false * B. are rare in children under 10 years of age - controversial in literature but possibly best answer of a bad lot o " Postspinal headache is one of the most common complications of lumbar puncture (LP). Limited evidence suggests that the incidence in children is lower than in adults [22-25]. However, in a prospective study of LP in 112 children and adolescents (age 2 to 16 years), postspinal headache occurred in 18 and 40 percent of children <10 years and ≥10 years, respectively [26]." (Uptodate) * C. have an incidence of approximately 5% to 12% following spinal anaesthesia - false o Note the numbers for B are post LP. * D. have an incidence which is independent of needle gauge - false o Bigger needle, more likely * E. presents with signs which are not posturally related - false |
|
|
|
PP81 ANZCA version [2005-Apr] Q137
An eight-year-old boy presents with bleeding one week after a tonsillectomy. When you see him in the emergency room, he is conscious but restless, tachypnoeic, pale and cool peripherally, with a pulse rate of 135 and blood pressure of 80/60. What percentage of his blood volume is he most likely to have lost? A. 10 -15% B. 15-25% C. 25 - 45% D. 45-55% E. more than 55% |
ANSWER C
An 8 yr old is expected to have a systolic BP = 80 + (2 x age in yrs). So for this child expect SBP=95 The APLS guidelines suggest that a child with greater than 40% blood loss will be "responsive only to pain", clearly not this child. In fact, an agitated child falls into the <25% blood loss group. Also of note is that HR=135. A child of 8 years will have a HR in the range of 80-120. ATLS manual only has three (<25, 25-45, >45). Other references have different grading: * <15% will have mild tachycardia * <25% decreased pulse pressure but normal-ish BP * <35% decreased BP * >40% coma and severe decrease BP. |
|
|
|
PP78 ANZCA version [2004-Apr] Q150, [2004-Aug] Q4
In children with upper respiratory tract infections (URTIs) presenting for general anaesthesia A. airway events are less likely if an endotracheal tube is used B. oxygen desaturation to under 90% is more likely (compared to children without URTIs) C. parental smoking does NOT affect the incidence of airway events D. peri-operative breath holding is NOT more likely (compared to children without URTIs) E. the site of surgery has no effect on the incidence of airway events |
ANSWER B
"Results showed that children with active and recent URIs (in the last 4 wk) had significantly more episodes of overall respiratory events, breath-holding, major arterial oxygen desaturation (Spo2 <90%), and severe coughing compared with children with no URIs." "Independent risk factors for adverse respiratory events in children with active URIs included use of an ETT in a child <5 yr old, prematurity (<37 wk), history of reactive airway disease, paternal smoking, surgery involving the airway, presence of copious secretions, and presence of nasal congestion." |
|
|
|
PP76 ANZCA version [2004-Apr] Q134, [2004-Aug] Q57
Post-operative nausea and vomiting in children A. is more common in females (than males) before puberty B. is more common in children under two years of age (than older) C. is rare following orchidopexy D. is twice as frequent in children over the age of three, compared to adults E. should not be treated with ondansetron |
ANSWER D
The incidence of PONV above preschool age is higher than in adults. It depends on age: * 34-50% in school children * 20% in preschool children * 5% (lowest incidence) in infants There is a greater incidence in girls but this only begins after 13 years of age |
|
|
|
PP75 ANZCA version [2004-Apr] Q101
In the management of pain for children A. a linear analogue scale is rarely used in assessment of pain B. non-steroidal anti-inflammatory drugs (NSAIDS) often cause renal dysfunction C. opioids are contraindicated under one month of age D. paracetamol is effective orally at a dose of 10 mg.kg-1 E. rectal paracetamol is recommended at doses of 20-30 mg.kg-1 |
ANSWER E
VAS scores ARE useful in children, but probably limited to children seven years of age and older NSAIDs are clearly in widespread use, no reference seems necessary to prove this point. Morphine is relatively contraindicated in neonates due to increased risk of apnoeas, but if the neonate is being discharged from theatre to NICU for monitoring/ventilation, morphine would not be contraindicated. In small doses morphine is used in neonates. * A - "Older children (>5yo) with an understanding of numerical concepts may be able to use these; vertical formats such as ladders and thermometers seem to be most successful" * B - "Adequate hydration is required in the postoperative period. Consequently, after major surgery, oral NSAIDs are usally only started once the child is eating and drinking adequately, and prescribed for a set time period, eg 3 days" * C - "caution in infants under 6 months of age, as dose reduction may be required". Premature infants listed as CI in MIMS * D - "A dose of 10mg/kg is no more effective than placebo for minor pain in children" * E - "The recommended dose in children is...20mg/kg rectally every 6 hours" |
|
|
|
PP70 ANZCA version [2003-Aug] Q140, [2004-Apr] Q82
The normal haemoglobin (g.dl-1) for age during infancy is A. 16 at 3 months B. 12 at 3 months C. 10 at 3 months D. 8 at 3 months E. 9 at 12 months |
ANSWER C
|
|
|
|
PP67 ANZCA version [2003-Apr] Q126, [2003-Aug] Q75
The most appropriate intravenous fluid volume to administer to a one-year-old 10 kilogram infant, fasted for five hours having minor peripheral surgery of two hours duration (with minimal blood loss) is A. 200 ml B. 260 ml C. 320 ml D. 410 ml E. 490 ml |
ANSWER C
Fluid requirements per hour: * 4ml/kg/hr first 10 kg * 2ml/kg/hr next 10 kg * 1ml/kg/hr each further kg 10kg child 7hr x 40ml/hr = 280ml Third space losses = 0-2ml/kg/hr for relatively atraumatic surgery or 6-8ml/kg/hr for traumatic procedures, so 2ml/kg/hr x 10kg x 2hr = 40ml Total = 320ml = C |
|
|
|
PP65 ANZCA version [2003-Apr] Q130
In a child with NO history of epilepsy the commonest cause of post-operative convulsions is A. hyperthermia B. hyponatraemia C. hypoxia D. local anaesthetic toxicity E. pethidine toxicity |
ANSWER B
|
|
|
|
PP64 ANZCA version [2002-Aug] Q131, [2003-Apr] Q78
Changes in the fetal circulation following birth include A. an immediate increase in pulmonary vascular resistance B. functional closure of the foramen ovale at one hour C. physical closure of the foramen ovale at several weeks D. a decrease in systemic vascular resistance E. closure of the ductus arteriosus in the first few hours |
ANSWER B
A. An immediate decrease in pulmonary vascular resistance occurs with the first breaths. The entry of air (with oxygen) into the lungs with onset of breathing results in removal of hypoxic pulmonary vasoconstriction so PVR falls markedly. B. Foramen ovale functional closure is generally in place at one hour; it occurs as pulmonary venous return increases, causing a rise in left atrial pressure compared to right atrial pressure C. Total physical closure of the foramen ovale (when it occurs) takes up to a year D. An Increase in systemic vascular resistance occurs as the cord is clamped E. The actual closure of the ductus takes place in two stages. In healthy full term newborns, functional ductal closure occurs by 96 h. This functional closure is followed later by anatomical closure via endothelial and fibrous tissue proliferation |
|
|
|
PP62 ANZCA version [2002-Aug] Q113, [2003-Apr] Q74
Propofol for induction and maintenance of anaesthesia in healthy children, compared to healthy adults, has A. a larger central volume of distribution B. a lower total body clearance C. the same context sensitive half-time D. a more rapid awakening time E. a lower infusion rate requirement |
ANSWER A
|
|
|
|
PP61a ANZCA version [2002-Aug] Q119
The peak effect of oral midazolam as a premedication in children occurs after A. 10 - 20 minutes B. 20 - 30 minutes C. 30 - 40 minutes D. 40 - 50 minutes E. 50 - 60 minutes |
ANSWER C
"The dose of oral midazolam... usually results in a satisfactorily sedated child in approximately 10-15 min with a peak effect occurring at approximately 20-30 min, with minimal to no delay in recovery, even for brief procedures." |
|
|
|
PP61c ANZCA version [2004-Apr] Q131
Satisfactory sedation after 0.5 mg.kg-1 of oral midazolam as a premedication in children usually occurs after A.5 minutes B.15 minutes C.25 minutes D.35 minutes E.45 minutes |
ANSWER C
"The dose of oral midazolam... usually results in a satisfactorily sedated child in approximately 10-15 min with a peak effect occurring at approximately 20-30 min, with minimal to no delay in recovery, even for brief procedures." |
|
|
|
PP61d ANZCA version [2004-Aug] Q141, [2005-Apr] Q61
Which of the following statements regarding pre-operative oral midazolam in children (in appropriate dosage) is INCORRECT? A. Distress at induction is reduced by approximately one half B. Peak effect is at 20 - 30 minutes C. Pre-operative anxiety is reduced D. Post-operative maladaptive behaviour is reduced E. Significantly delays recovery and discharge |
ANSWER E
|
|
|
|
PP60 ANZCA version [2002-Aug] Q116
A one-month-old infant requires analgesia following simple inguinal hernia repair. The most appropriate paracetamol dosing regimen for the first 48 hours is Route Loading Subsequent Maximum daily dose doses dose (mg.kg-1) (mg.kg-1) (mg.kg-1.day-1) A. Oral 20 15 45 B. Oral 20 20 90 C. Oral 20 20 60 D. Rectal 20 20 90 E. Rectal 40 20 90 |
ANSWER C
According to ANZCA APM (2nd ed) p210: * Max daily dose for infants less than 6 months is 60mg/kg/day - so answer is C * Over 6 months: 90 mg/kg/day * Under 6 months: 60 mg/kg/day * 34 wk prem: 45 mg/kg/day |
|
|
|
PP59 ANZCA version [2002-Mar] Q95, [2002-Aug] Q35
A child weighing 8 kg would be expected to need a Laryngeal Mask Airway of size: A. 0 B. 1 C. 1.5 D. 2 E. 2.5 |
ANSWER B
LMA Size Weight 1 <5kg 1.5 5-10kg 2 10-20kg 2.5 20-30kg 3 >30kg |
|
|
|
PP56 ANZCA version [2002-Mar] Q143
The Pierre Robin syndrome is characterised by 1. smaller than normal mandible 2. cervical spine synostosis 3. cleft palate 4. maxillary hypoplasia |
ANSWER 1 and 3
* Pierre Robin syndrome has mandibular hypoplasia. * There are no cervical spine abnormalities. * Cleft palate in 50% of cases. |
|
|
|
PP53a ANZCA version [2001-Aug] Q85
Intraoperative hypoglycaemia in children is LEAST likely in A. small-for-age children B. Beckwith-Wiedeman Syndrome C. infants following an overnight fast D. infants on propanolol peri-operatively E. intra-operative interruption of pre-operative total parenteral nutrition (TPN) |
ANSWER C
Small for age, young, prolong fasting, propranolol, Beckwith (organomegaly, glossomegaly, hypoglycaemia), Silver-Russell (small for age, failure to thrive, poor feeding) all associated with hypoglycaemia. Overnight fast causes less hypo than a daytime fast because of morning cortisol, maybe this is the answer. Interruption of preop TPN may cause hypo but add the stress of surgery and I think that they'd probably be OK. All that's required to prevent hypoglycaemia is 2% glucose at the maintenance rate. |
|
|
|
PP53b ANZCA version [2002-Mar] Q88, [2002-Aug] Q67
Intraoperative hypoglycaemia in children is LEAST likely in A. small-for-age children B. Beckwith-Wiedeman Syndrome C. infants following an overnight fast D. infants treated with propanolol E. Russell-Silver syndrome |
ANSWER C
Small for age, young, prolong fasting, propranolol, Beckwith (organomegaly, glossomegaly, hypoglycaemia), Silver-Russell (small for age, failure to thrive, poor feeding) all associated with hypoglycaemia. Overnight fast causes less hypo than a daytime fast because of morning cortisol, maybe this is the answer. Interruption of preop TPN may cause hypo but add the stress of surgery and I think that they'd probably be OK. All that's required to prevent hypoglycaemia is 2% glucose at the maintenance rate. |
|
|
|
PP53c ANZCA version [2001-Apr] Q82
The most correct statement regarding intra-operative glucose management in children is that A. 5% dextrose should be used B. there is a higher incidence of hypoglycaemia in children following overnight fasting than in children fasting during the daytime C. blood glucose monitoring is mandatory D. hyperglycaemia is harmless E. most children do not require glucose intra-operatively |
ANSWER E
* A: False - 5% dextrose should NOT be used due to risk of hyperglycaemia and hyponatraemia * B: False - due to diurnal variation in cortisol, daytime fast result in higher incidence of hypoglycaemia * C: False - NOT mandatory * D: False - hyperglycaemia results in diuresis, dehydration, electrolyte disturbances, increase risk of hypoxic brain injury etc * E: True - can use either low glucose solutions or glucose free solutions for most kids. |
|
|
|
PP52 ANZCA version [2001-Aug] Q66, [2002-Mar] Q34
A 16 kilogram, 3 year old boy for unilateral inguinal herniotomy has general anaesthesia and a caudal with 8 mls of 0.25% plain bupivacaine. The LEAST correct statement regarding this anaesthetic management is that A. the required level of the block is T12 B. the volume of local anaesthetic used is inadequate C. the block duration is the same for all segments D. peripheral nerve blocks are safer than neural axis blocks in children E. use of adrenaline in the local anaesthetic would prolong the block |
ANSWER C
The question is asking about the least correct or probably better rephrased, the most false. D is clearly contentious so could be either T/F in a debate. E is probably true but causes spinal ischaemia and so is not ideal in a practical sense. B is correct. The volume is inadequate. (should be 1ml/kg) A is sort of correct. The caudal is for post op analgesia as the child is having a GA, so T12 block height is probably just OK. This leaves C as being 'the most false' |
|
|
|
PP51 [Jul00]
At what age in children is the Hb level at its lowest? A. Neonate B. 3 months C. 6 months D. 12 months E. 24 months |
ANSWER B
The Children's Hospital Westmead Handbook says lowest at 3-12 months. The Children's Hospital notes emphasise that 3 months is the lowest value. * The nadir is at 3 months where the Hb is 10g/dl. |
|
|
|
PP49 [Apr99] [Mar00]
A 5kg baby loses 65mls of blood at operation. Which of the following is correct? A. Transfuse as blood loss >20% B. Don’t transfuse as loss is <10% C. Transfuse if further blood loss anticipated D. >25% blood volume lost E. Definitely do not give blood |
ANSWER C
Weight = 5kg Blood volume = 80 mls/kg = 80 x 5 = 400mls Blood loss = 65/400 = 16% |
|
|
|
PP47 [Apr98] (type A)
A 34 week prem neonate in recovery post hernia. At 90 seconds after extubation, HR is 75. Most important intervention: A. CPR B. Atropine C. Ensure oxygenation D. Reintubate E. ? |
ANSWER C
Preterm infant post GA, bradycardia most likely due to hypoxia, either apnea or obstruction - therefore ensuring oxygenation is most important, |
|
|
|
PP45 [Apr98] [Jul98] [Apr99] (type A)
Tracheo-oesophageal fistula in a neonate is associated with all of the following EXCEPT: A. VSD B. Vertebral column abnormalities. C. Anal atresia (or: imperforate anus) D. Pulmonary hypoplasia. E. Renal abnormalities. F. ? Radial abnormalities |
ANSWER D
"VACTERL Association" V stands for vertebral anomalies, like hemi or block vertebrae. A stands for imperforate anus or anal atresia. C denotes cardiac anomalies such as VSD. TE stands for tracheoesophageal fistula. R stands for renal or anomalies and radial or arm anomalies. L is often added to stand for limb anomalies in case you forget. |
|
|
|
PP40 [Aug95] [Jul97]
A 9 year old boy for an appendix operation is induced with thiopentone, fentanyl, suxamethonium. Two minutes after induction, he is pulseless & ECG shows sinus arrest. The most likely cause is: A. Allergy to suxamethonium B. Bradycardia secondary to suxamethonium C. Duchenne muscular dystrophy (?undiagnosed) D. Dystrophica myotonia E. Malignant hyperthermia |
ANSWER C
|
|
|
|
PP38 [Aug94] [Jul97]
An HIV-positive mother gives birth to a baby. What is the percentage chance of the baby being HIV antibody positive? A. 5-10% B. 20-30% C. 50% D. 70-85% E. 95-99% |
ANSWER E
The question asks about the baby being HIV ANTIBODY positive (NOT HIV positive) Almost all babies will have antibodies to HIV from the mother and will test positive for 6-18months. During pregnancy, the mother's antibodies (part of the immune system that fights germs) are passed on to her baby. So all babies of women with HIV will test positive for HIV antibodies at first. This doesn't mean the baby is infected, though. Babies keep the mother's antibodies until they can make their own, which happens between 6 and 18 months of age. An HIV positive woman can transmit the virus to her baby during pregnancy, labour and delivery, and through breastfeeding. If she takes no preventive drugs and breastfeeds then the chance of her baby becoming infected is around 20-45%. Risk is decreased to 2-3% if mother is compliant with antivirals, viral load low, LUSCS, avoid breast milk. |
|
|
|
PP37 [Aug94] [Apr96] (Type A MCQ)
A child with an inhaled foreign body. What is the characteristic radiological sign? A. Hyperinflation of the affected lung on expiration B. Opacity in the right upper lobe C. Evidence of interstitial oedema D. Collapse of the affected lobe E. Right middle lobe collapse F. Radiopaque shadow superimposed on bronchi G. Mediastinal shift |
ANSWER A and D
* A. Hyperinflation of the affected lung on expiration - true and has best detail: "If the chest is normal, a ball-valve phenomenon may still exist, and on the expiration view, air will be trapped on the affected side, whereas the unaffected lung will decrease in volume." (Mettler: Essentials of Radiology 2E Ch 9) * B. Opacity in the right upper lobe - likely false * C. Evidence of interstitial oedema - likely false * D. Collapse of the affected lobe - true: "In this case (of a completely impacted foreign body), the air distally will become resorbed, and postobstructive atelectasis or a focal infiltrate with associated volume loss will be found." (Mettler: Essentials of Radiology 2E Ch 9) * E. Right middle lobe collapse - possible but not a cardinal feature of the CXR * F. Radiopaque shadow superimposed on bronchi - false: "Most foreign bodies consist of vegetable material (such as peanuts) or plastic. Remember that vegetable and plastic items are usually not visible on a plain x-ray." (Mettler: Essentials of Radiology 2E Ch 9) * G. Mediastinal shift - true but only on expiratory film: "If the chest is normal, a ball-valve phenomenon may still exist, and on the expiration view, air will be trapped on the affected side, whereas the unaffected lung will decrease in volume. When this happens, a resultant shift of the mediastinum toward the normal unaffected side will be seen." (Mettler: Essentials of Radiology 2E Ch 9) |
|
|
|
PP04 [1985] [1986] [Mar91] [Apr96] [Aug96] [Apr97] [Jul97]
A 5kg baby is 5% dehydrated. The body water deficit: A. 150mls B. 200mls C. 250mls D. 300mls E. 350mls |
ANSWER C
The % dehydrated is a % of total body weight. Five percent of 5,000g is 250g. One ml of water weighs one gram, so 250 grams is 250mls of water. A general description of dehydration signs & symptoms: * Mild dehydration produces thirst and mild oliguria but no detectable physical signs; it equates with 5% acute weight loss. * Moderate dehydration (5-10%) : tachycardia, slightly sunken eyes, reduced skin turgor and peripheral perfusion/capillary return, some loss of ocular tension and sunken fontanelles, and more thirst and oliguria * Severe dehydration (>10%): marked tachycardia, obvious loss of skin tone and tissue turgor, sunken eyes, loss of ocular tension, severe oliguria/anuria, restlessness or apathy. Also circulatory collapse, delirium, coma, fever and cyanosis |
|
|
|
PP05a
What is the fluid replacement for maintenance of a 3kg neonate in the first 24 hours of life? A. 50mls B. 100mls C. 150mls D. 200mls E. 250mls |
ANSWER D
60 mls/kg/day for first 24 hrs so 180 mls/day for a 3 kg newborn Maintenance Water Requirements Age ml/kg/day 1st day of life 60 2nd day 90 3rd day 120 up to 9 months 120–140 12 months 90–100 2 years 80–90 4 years 70–80 8 years 60–70 12 years 50-60 [edit] Factors modifying water requirements Extra Required * Fever (add 12% for each °c above 37°C) * Hyperventilation * High ambient temperature * Extreme activity * Any other abnormal losses e.g. diarrhoea, polyuria Less required * Hypothermia (subtract 12% for each°c below 37°C) * Very high humidity * Oliguria or anuria * Extreme inactivity * Fluid retention e.g. cardiac failure |
|
|
|
PP09 [1985] [1986] [1987] [1988] [Aug91] [Mar92] [Aug92]
Retrolental fibroplasia: A. Is prevented by control of FIO2 B. Is a common cause of myopia C. Causes retinal detachment leading to blindness D. May recover if mild E. Occurs more commonly in premature babies F. Is more common in premature infants |
ANSWER C
A. Is prevented by control of FIO2 - Not prevented, but high FiO2 increases risk B. Is a common cause of myopia - No C. Causes retinal detachment leading to blindness - Yes, it can do, due to fibrous scar tissue; the key disease element is fibrovascular proliferation. D. May recover if mild - Well, it may not progress to retinal detahcment, but recover?? E. Occurs more commonly in premature babies - It ONLY occurs in premature babies F. Is more common in premature infants - as (E) |
|
|
|
PP15 [1986]
Polyhydramnios is associated with: A. Diaphragmatic hernia B. TOF C. Pulmonary hypoplasia D. CNS abnormalities E. Renal agenesis |
ANSWER A and B
* A True * B True, the tracheo-oesophageal fistula in 86% of cases has atresia of the oesophagus proximally and the trachea fistulates to the distal oesophagus. As such, the fetus is unable to swallow amniotic fluid and polyhydramnios results. * C False * D False non-specific * E False causes oligohydramnios as no urine is produced. TOFistula also cause polyhydramnios, but pulmonary hypoplasia is caused by oligohydramnios. |
|
|
|
PP16
The condition of a neonate deteriorates twelve hours after repair of a diaphragmatic hernia. The most likely cause for deterioration: A. Hypoglycaemia B. Gastric dilatation C. Tension pneumothorax D. Haemorrhage E. None of the above |
ANSWER E
Pulmonary hypoplasia still exists and PTH is still sensitive to stressors (hypercarbia, hypoxia, acidosis, hypothermia, pain). The postoperative course, after surgical reduction of congenital diaphragmatic hernias, is often characterized by rapid improvement, followed by sudden deterioration with profound arterial hypoxemia, hypercapnia, and acidosis, resulting in death. The mechanism for this deterioration is the reappearance of fetal circulation patterns, with right-to-left shunting through the foramen ovale and ductus arteriosus. If shunting occurs through the ductus arteriosus, there is a 20-mm Hg or more difference in the PaO2 measured in samples obtained simultaneously from preductal and postductal arteries. If the shunting is predominantly through the foramen ovale, no such gradient exists. Proper sedation is necessary as any stressful stimulus can further exacerbate already elevated pulmonary pressures with resultant increases in shunt flow and further desaturation. |
|
|
|
PP18 [1987] [Mar91] [Aug91]
Best fluid replacement in pyloric stenosis: A. Hartmanns solution B. N/2 saline C. N/5 saline D. Dextrose 4% in N/5 saline E. 10% Dextrose |
NONE OF THESE
Oxford Handbook (p800): 5%D + 0.45% saline (with 20 mmol/l KCl) RCH Guidelines (http://www.rch.org.au/clinicalguide/cpg.cfm?doc_id=8402): *Fluid resuscitation may be necessary with 10-20ml/kg boluses of normal saline, for patients with moderate to severe dehydration *Commence IV Fluids (0.45% Saline / 5% Dextrose + 10mmol KCl / 500mls) at 100mls/kg/day initially *Review after 4-6 hours |
|

