![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
151 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
AC121 ANZCA Version [2003-Aug] Q146, [2004-Apr] Q72, [2005-Sep] Q62, [Mar06] Q61
The LEAST useful investigation to diagnose early myocardial RE-infarction is A. CK-MB B. CK-MB as a fraction of total CK C. echo D. ECG E. troponins |
ANSWER E
A. FALSE : CK-MB is a very good test for acute myocardial injury. It is very specific, rises in quickly : 3-4 hours, peaks at 18-24 hours, returns to normal in 72 hours, therefore good test for re-infaraction B. FALSE : Total CK to CK-MB ratio known as the cardiac index, sensitive indicator of early MI C. FALSE : D. FALSE : E. TRUE : troponins more specific for infarction (more specific than CK-MB), rise within 2 hours, peak at 12hours, elevated for 5-10 days up to weeks, therefore ppor at detecting re-infarctions |
|
|
|
AC101aa ANZCA version [2005-Sep] Q108 [March 2006 Q3]
According to the AHA (American Heart Association) Guidelines intermediate clinical predictors of increased perioperative cardiovascular risk include each of the following EXCEPT A. prior heart failure B. diabetes mellitus C. previous myocardial infarct D. renal insufficiency E. uncontrolled systemic hypertension |
ANSWER E
ACTIVE CARDIAC CONDTIONS require investigation and likely intervention unless the surgury is an emergency. 1. Unstable coronary Sx 2. Decompensated heart failure 3. Significant arrythmias 4. Severe valvular disease CLINICAL RISK FACTOR to stratify other patients 1. Hx of heart disease 2. Prior heart failure 3. Cerebrovascular disease 4. Diabetes mellitus 5. Chronic renal impairment PROCEDURE RELATED RISK 1. Vascular (>5% risk of MI and/or death). Includes all vascular surgery except carotid endarterectomy 2. Intermediate (Less than 5%, more than 1%). Carotid endarterectomy, abdominal, thoracic, neuro, head and neck, major orthopaedic, prostatic, etc. 3. Low risk (less than 1%). Ambulatory, eyes, superficial, endoscopy, breast |
|
|
|
AC101b ANZCA version [2004-Apr] Q100, [2004-Aug] Q43,
According to the American Heart Association Guidelines on Perioperative Cardiac Evaluation for Noncardiac Surgery, which of the following operations has a high risk (>5%) of cardiac death or non-fatal myocardial infarct? A. carotid endarterectomy B. trans-urethral resection of the prostate (TURP) C. total knee joint replacement D. femoral-popliteal bypass E. right hemicolectomy |
ANSWER D
PROCEDURE RELATED RISK 1. Vascular (>5% risk of MI and/or death). Includes all vascular surgery except carotid endarterectomy 2. Intermediate (Less than 5%, more than 1%). Carotid endarterectomy, abdominal, thoracic, neuro, head and neck, major orthopaedic, prostatic, etc. 3. Low risk (less than 1%). Ambulatory, eyes, superficial, endoscopy, breast |
|
|
|
MC38 ANZCA version [2002-Mar] Q10, [2002-Aug] Q49, [2005-Sep] Q9, [Mar06] Q9 (Similar reported question in [1989] [Mar90] [Sep90] [Mar93] [Aug93])
Causes of inverted P waves in Lead II of the electrocardiogram include A. transposed lower limb leads B. junctional rhythm C. hypothermia D. left axis deviation E. inferior myocardial infarction |
ANSWER B
A negative P wave in lead I may be due to 1. transposition of left and right arm electrodes 2. dextrocardia 3. abnormal atrial rhythms A. FALSE : LIMB LEADS : I, II, III -these leads are bipolar I = LA - RA II = LL - RA III = LL - LA -transposing lower limb leads should not invert P waves B. TRUE : -The presence of P waves indicates that the atria have depolarised. -If P waves are upright in lead II and aVF they have originated from the SA node -Inverted P indicates that the retrograde depolarization is occuring through atria : junctional or ventricular C. FALSE : Hypothermia -bradycardia -long QT -J waves (rounded waves above the isoelectric point that immediately follow the R wave) D. FALSE E. FALSE |
|
|
|
MC51 ANZCA version [2005-Apr] Q43, [2005-Sep] Q43, [Mar06] Q26 | Aug10
(Similar version reported in [Mar93] [Aug93] [Mar94] [Aug94] [Mar95] [Aug95] [Apr96] [Aug96]) The chief concern in the anaesthetic management of a patient with mitral stenosis is to avoid tachycardia because it A. increases the trans-mitral pressure gradient B. aggravates left ventricular ischaemia C. increases myocardial oxygen consumption D. frequently precipitates atrial fibrillation E. reduces the size of the left atrium |
ANSWER A
Mitral stenosis is characterized by mechanical obstruction to left ventricular diastolic filling secondary to a progressive decrease in mitral valve orifice size. This leads to a relatively fixed CO in combination with elevated LA pressures. Epidemiology Most common cause is rheumatic fever, and primarily affects females. These patients tend to have mixed MR / MS; a minority willl have pure MS. Patients remain asymptomatic for 15-20 years. Symptoms appear at 31 years on average with 50% mortality at 5 years if not corrected. Much less common causes of mitral stenosis include carcinoid syndrome, left atrial myxoma, severe mitral annular calcification, thrombus formation, cor triatriatum, rheumatoid arthritis, systemic lupus erythematosus, and congenital mitral stenosis. Pathophysiology * Underfilled LV with fixed CO due to stenotic valve; the LV has reduced preload reserve. With mild mitral stenosis, left ventricular filling and stroke volume are usually maintained at rest by an increase in left atrial pressure. However, stroke volume will decrease during stress-induced tachycardia (as diastolic filling is decreased) or when effective atrial contraction is lost as with atrial fibrillation. * Elevated left atrial pressure to produce a diastolic pressure gradient across stenosed mitral valve. This eventually results in elevated pulmonary venous pressures, and also pulmonary arterial hypertension. * LA dilatation initially is compensatory and keeps PAP low. However this fails eventually. Complications * atrial fibrillation occurs as a result of LA dilatation and fibrosis of the atrial wall. * Acute pulmonary oedema can occur if LAP rises suddenly (eg AF, fluid overload, autotransfusion with oxytocics). * Pulmonary venous congestion causes airway narrowing (increases work of breathing and airway resistance), transudation of fluid into pulmonary interstitial space (reducing pulmonary compliance) and redistribution of blood from bases to apices (V/Q mismatch). * Pulmonary arterial hypertension occurs 5 - 10 years after the onset of symptoms. Initially PVR elevation is reversible, but chronically elevated PVR causes pulmonary artery medial hypertrophy and fibrosis leading to an irreversible rise in PVR. * RV failure occurs as a result of PAH, when PAP are >70mmHg. * Thromboembolism occurs commonly in MS, correlating with the patient's age and size of the LA appendage. 80% of patients who develop systemic embolic are in atrial fibrillation. Presentation : History * Dyspnoea on exertion / fatigue * PND, Orthopnoea * Haemoptysis (due to rupture of bronchopulmonary varices) * Recurrent bronchitis Presentation : Examination * Mitral facies - malar flush on cheeks (dilated capillaries in combination with peripheral cyanosis) * Peripheral cyanosis - due to poor CO * AF * Signs of RVF (elevated JVP, hepatomegaly, peripheral oedema, ascites). * Tapping apex beat (due to palpable S1 - valve cusps widely apart at onset of systole) * Diastolic thrill * Pulmonary HTN (RV heave, palpable S2) * Loud S1 * Opening snap if in SR (at LSE - high LAP forcing cusps apart, but valve cone is abruptly halted) * Mid-diastolic, low pitched rumbling murmur best heard at apex |
Medical Management
* Diuretics - symptom relief in mild disease * DCR * Rate control of AF (digoxin, beta blockers, Ca channel blockers) * Anticoagulation Surgical Managment Indicated when symptoms worsen or when pulmonary hypertension develops. May be balloon valvuloplasty if suitable (in young patients with non-regurgitant valves that are not grossly affected), open mitral valvotomy/repair or replacement. Anaesthetic Management Pre-Operative *Control rate esp if in AF. Digoxin is useful in patients in chronic AF. *Operative risk correlated with the severity of the stenosis of the value Intra-Operative * Firstly, manage anti-coagulation cessation (Only applies to patients on warfarin for AF) * Secondly, antibiotic prophylaxis for bacterial endocarditis as per new guidelines (so rarely needed) * Thirdly, optimise haemodynamics (Applies mostly to patients with MV area is less than 1.5 cm2) * Haemodynamic goals are Slow, full and tight for stenotic lesions. Anaesthetic Technique * No anaesthetic technique has been demonstrated to be safer but GA may be more CVS stable. * Asymptomatic patients do not require additional monitoring. IAL, CVC, PAFC and TOE may all be considered for patients with moderate to severe disease having major surgery. * Careful induction of anaesthesia with small titrated doses of propofol or an opioid dominant technique is suitable. Ketamine should be avoided. Haemodynamic response to intubation should be adequately blunted. * Ensure deep anaesthesia - sevoflurane or opioids can be used safely. Avoid muscle relaxants with significant haemodynamic side effects (eg atracurium, mivacurium, pancuronium). Rhythm and rate * Sinus rhythm is preferred if possible for mild disease(eg preop cardioversion or drug conversion) * In moderate to severe MS atrial contraction are ineffective due to dilatation; rate control is paramount. * ensure rate is controlled (60-80/min is best) whether in sinus rhythm or in AF * avoid tachycardia (May require beta-blockers eg Esmolol if intraop tachycardia); * avoid bradycardia. (Bradycardia causes problems because of the fixed flow rate across the mitral valve. A decrease in heart rate means a decrease in cardiac output) * Cardioversion is an option if AF develops intraop Maintain Preload Margin for error is small. Avoid hypovolaemia and replace losses early and appropriately. If the preload (LA pressure) is increased the risk of pulmonary congestion is increased so excessive volume loading (IV, head down positioning) is also quite deleterious; may cause APO. Decreased preload is poorly tolerated; decreased LAP will reduce the gradient across the stenosed valve. Note that preload can be decreased by high ventilation pressures or the head-up position. (Note that the use of the term 'preload' here refers to LA pressure and not LV diastolic pressure or volume. This is because the LV is not well filled in severe MS and LVEDP will be normal or low so the preload referred to is the pressure upstream of the mitral valve ie LAP). Mantain afterload Minimal margin for errors. Vasodilatation results in reduced LA filling; the SV is fixed and cannot compensate resulting in severe hypotension. A 'pure' alpha vasopressor (eg phenylephrine) may be required. Reduce PVR Avoid hypercapnia, hypoxia, hypothermia and acidosis These are common recommendations in the literature because these factors are said to cause increased pulmonary artery pressure, and could possibly precipitate pulmonary oedema in patients with severe MS. Maintain Contractility To maximise SV from limited filling. Post Operative Optimal haemodynamics should be maintained postoperatively. This means initial ICU management if MS is severe. Mild & moderate MS is usually managed in a ward setting if the patient does not have major co-morbidities and there are no other reasons for ICU admission. Anti-coagulation may need to be recommenced as the situation allows. |
|
|
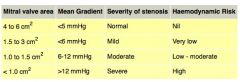
What are the operative risks when correlated to the severity of mitral stenosis?
|
|
|
|
|
MC59 ANZCA version [2001-Apr] Q43, [Jul07]
The treatment LEAST likely to be useful for torsades de pointes is A. defibrillation B. procainamide C. magnesium D. electrical pacing E. isoprenaline |
ANSWER B
Torsade de pointes -uncommon and distinctive form of polymorphic ventricular tachycardia -characterised by a gradual change in amplitude and twisting of the QRS complexes around and isoelectric line, -150-250 bpm -associated with prolong QT, usually greater than 600msec Pathophysiology -abnormality underlying both acquired and congenital long QT syndromes is the ionic current flow during repolarization : affecting the QT interval -slow inactivation of the Ca++ and Na+ during phase 3 (repolarization) leading to prolonged QT and leaves a 'window' where single or repetitive depolarizations can occur, ei early afterdepolarization (EAD) Epidemiology -unknown prevalence -QTc is longer in Caucasians than blacks -Brugada syndrome is more frequent in asians -Torsades is 2-3 more common in women : longer QTs and more sensitive to QT prolonging drugs Risk factors -Congenital long QT syndrome -Female gender -Acquired long QT syndrome (causes of which include medications and electrolyte disorders such as hypokalemia and hypomagnesemia) -Bradycardia -Baseline electrocardiographic abnormalities -Renal or liver failure Etiology Congenital - Jervell and Lange-Nielsen syndrome -Romano-Ward syndrome -Brugada syndrome is characterized by a coved ST segment in the right precordial leads. The syndrome may cause sudden death due to polymorphic VT resembling torsade -Takotsubo cardiomyopathy (stress-induced cardiomyopathy) causes a predisposition to torsade Conditions assocaited - Electrolyte abnormalities - Hypokalemia, hypomagnesemia, hypocalcemia - Endocrine disorders - Hypothyroidism, hyperparathyroidism, pheochromocytoma, hyperaldosteronism -Cardiac conditions - Myocardial ischemia, myocardial infarction, myocarditis, bradyarrhythmia, complete atrioventricular (AV) block, takotsubo cardiomyopathy[6] -Intracranial disorders - Subarachnoid hemorrhage, thalamic hematoma, cerebrovascular accident, encephalitis, head injury -Nutritional disorders - Anorexia nervosa, starvation, liquid protein diets, gastroplasty and ileojejunal bypass, celiac disease Drug Causes -antiarrhythmic drugs : Class 1A (quinidine, procainamide, dispyramide) Class 1C (encainide, flecainide) Class 3 (sotalol, amiodarone) -Antihistamines : astemizole and terfenadine -Antibiotics - Erythromycin, clarithromycin, azithromycin, levofloxacin, moxifloxacin, gatifloxacin, trimethoprim-sulfamethoxazole, clindamycin, pentamidine, chloroquine - Antifungals - Ketoconazole, itraconazole -Antivirals – Amantadine -Antipsychotics - Haloperidol, phenothiazines, thioridazine, trifluoperazine, sertindole[9] , zimeldine, ziprasidone[7] -Tricyclic and tetracyclic antidepressants -Antihistamines (histamine1-receptor antagonists) - Terfenadine, astemizole, diphenhydramine, hydroxyzine -Cholinergic antagonists - Cisapride, organophosphates (pesticides) -Diuretics - Indapamide, hydrochlorothiazide, furosemide -Antihypertensives - Bepridil, lidoflazine, prenylamine, ketanserin -Lithium -Anticonvulsants - phenytoin, carbamazepine (possible) -Oral hypoglycemic -Citrate (massive blood transfusions) - Cocaine -Vasopressin (possible) - Fluoxetine (possible) |
Acute Treatment
Short Term -same for acquired and congenital long QT syndrome except Beta1-adrenergic stimulation may be tried in acquired but contraindicated in congential 1. Remove offending agent 2. DC cardioversion if unstable 3. Predisposing conditions such as electrolyte disturbances corrected Pharmcological *magnesium is the drug of choice -1-2g IV over 30-60 seconds -repeated 5-15 minutes -OR continuous infusion at 3-10mg/min *Lidocaine has no effect in torsades, initial benefit but torsade will always reoccur *Isoprenaline can be used, accelerated AV conduction and decrease QT but increasing the heart rate (contraindicated in congenital) -Lignocaine and phenytoin provide inconsistent benefit. Amiodarone should be avoided because it can precipitate torsardes. Temporary transvenous pacing -same as isoprenaline -maintain HR 90-110 -atrial pacing is preferred to maintain a narrow QRS and short QT -however in AV block, ventricular pacing can be used -overdrive to 140bpm may be required Longterm treatment -Beta-adrenergic antagonists at maximally tolerated doses are used as a first-line long-term therapy in congenital long QT syndrome. -Propranolol -esmolol or nadolol also can be used. -Beta-blockers should be avoided in those congenital cases in which bradycardia is a prominent feature. Insertion of AICD -Permanent pacing benefits patients who remain symptomatic despite receiving the maximally tolerated dose of beta-blockers and can be used adjunctively with beta-blockers. It decreases the QT interval by enhancing the repolarizing potassium currents and suppressing EADs. High left thoracic sympathectomy, another antiadrenergic therapy, is effective in patients who remain refractory to beta-blockade and pacing. Accidental ablation of ocular efferent sympathetic nerves may result in Horner syndrome. Implantable cardioverter-defibrillators (ICDs) are useful in instances when torsade recurs despite treatment with beta-blockers, pacing, and possibly left thoracic sympathectomy. Beta-blockers should be used along with ICDs because shock can further precipitate torsade by adrenergic stimulation. In the United States, an ICD for refractory cases may often precede sympathectomy. Long-term treatment in acquired long QT syndrome usually is not required because the QT interval returns to normal once the inciting factor or predisposing condition has been corrected. Pacemaker implantation is effective in cases that are associated with heart block or bradycardia. ICDs are indicated in cases that cannot be managed by avoidance of the offending agent. The boundary between acquired and congenital may not always be clear. Additive factors are often present, and individuals may show increased susceptibility to QT effects. |
|
|
MC81 ANZCA version [2001-Aug] Q45, [2002-Mar] Q43, [2004-Apr] Q48, [2004-Aug] Q23, [Jul06] Q1 (Similar reported question in [Jul97] [Apr98] [Jul98] [Mar06])
A low ejection fraction is most likely to be seen in a patient with A. poor left ventricular (LV) systolic function B. poor LV systolic function and severe mitral regurgitation C. poor LV diastolic function D. septic shock E. a post myocardial infarct ventricular septal defect |
ANSWER A
A. TRUE : EF = (EDV-ESV) / EDV, as EDV will be normal, but ESV will be high, EF is low B. FALSE : MR will decrease ESV as blood will flow retrograde to atria, therefore EF will be high C. FALSE : EDV high with ESD normal, therefore EF will be high D. FALSE : high output state E. FALSE : same as B |
|
|
|
MC59b ANZCA version [2003-Apr] Q125, [2003-Aug] Q85, [2005-Sep] Q69, [Mar06] Q48 [Mar10] [Aug10]
In the management of torsades de pointes (polymorphic ventricular tachycardia), all the following drugs may be useful EXCEPT A. amiodarone B. isoprenaline C. [[lignocaine] D. magnesium E. phenytoin |
ANSWER A
5 minute cardiac consult says that magnesium and isoprenaline are recognised treatments. Lignocaine and phenytoin provide inconsistent benefit. Amiodarone should be avoided because it can precipitate torsardes. |
|
|
|
AZ77 ANZCA Version [Jul06] Q149
With regard to peri-operative cardiac risk reduction there is evidence that all of the following reduce perioperative cardiac morbidity EXCEPT A. intra-operative use of nitrous oxide B. peri-operative use of alpha-two agonists C. perioperative use of diltiazem D. peri-operative use of statins E. tight peri-operative glycaemic control (blood sugar between 3.5 and 6mmol.l-1) |
ANSWER A
A. TRUE : N2O has limited potency, used as adjunct with volatile agents or TIVA. -N2O interferes with vitamin B12 and folate metabolism -impairs production of methionine (from homocysteine), -megaloblastic anaemia, immunosuppression, myocardial ischaemia, nerve and spinal cord toxicity, carcinogenicity, teratogenicity (esp. with occupational exposure); as well as postoperative nausea and vomiting, and increased risk of hypoxia. -ENIGMA trialpatients receiving N2O had a significant increased risk of postoperative wound infection, severe vomiting, pneumothorax or atelectasis, and pneumonia. Additionally nitrous oxide patients recorded lower QoR scores, and for ICU patients (but not others), a greater length of stay. There was a nonsignificant reduction in AMI, mortality and awareness. B. FALSE : large meta analysis, highlighted 31 RCT's, poor as only 6 studies clearly reported blinding and randomization, showed a reduction in mortality, non fatal MI, but also hypotension and bradycardia C. FALSE : meta analysis of 11 studies shows a reduction in myocardial ischemia and SVT. And a tread towards reduction in mortality. Mainly observed with diltiazem. Dihydropiridone and verapramil has no effect. D. FALSE : Plaque stablization, oxidative stress reduction and decreased vascular inflammation. E. FALSE : shown to reduce wound infection |
|
|
|
Discuss the ENIGMA TRIAL.
|
More than 1 million Australians and New Zealanders undergo anaesthesia with nitrous oxide (N2O) each year, but there has yet to be a large trial of its safety and effectiveness.
N2O has limited potency. The usual practice is to administer 70% N2O in oxygen along with a volatile agent (eg. sevoflurane) or propofol in order to produce a depth of anaesthesia sufficient for surgery. This is despite knowledge that N2O interferes with vitamin B12 and folate metabolism. This impairs production of methionine (from homocysteine), used to form tetrahydrofolate and thymidine during DNA synthesis. This raises the possibility of: megaloblastic anaemia, immunosuppression, myocardial ischaemia, nerve and spinal cord toxicity, carcinogenicity, teratogenicity (esp. with occupational exposure); as well as postoperative nausea and vomiting, and increased risk of hypoxia. The prevailing view is that N2O is a cheap, relatively "safe" drug that can reduce the exposure to other anaesthetic drugs. However, the development of many new (safer?) anaesthetic drugs has led to calls for a re-evaluation of the role of N2O in current anaesthetic practice. The aim of the ENIGMA Trial was investigate the effectiveness and safety of nitrous oxide (N2O) in anaesthesia (1). Design Large, multi-centre, prospective, randomised, double blind, parallel-group, effectiveness trial. Patients will be randomly allocated to either 70% N2O in oxygen (FiO2 0.3) or oxygen with or without nitrogen (FiO2 0.8-1.0). Patients, surgeons, and nursing staff, and all individuals responsible for all outcome assessments were blinded to group identity. Primary End Point Hospital length of stay (LOS). LOS is a marker of serious morbidity and has direct healthcare resource implications. Secondary End Points Wound infection, myocardial infarction, pneumonia, stroke, severe vomiting, awareness, blood transfusion, pneumothorax, quality of recovery, and mortality Sample size 2000 patients (alpha 0.05, beta 0.10), to detect a ½-day (or greater) reduction in hospital length of stay Preliminary Results The ENIGMA Trial concluded November 2004 after 19 months of recruitment and 2050 patients' randomised across 19 hospitals both nationally and internationally. Data from 2012 patients were analysed, with 1015 patients randomised to the N2O group and 997 patients randomised to the Oxygen only group. We found that patients receiving N2O had a significant increased risk of postoperative wound infection, severe vomiting, pneumothorax or atelectasis, and pneumonia. Additionally nitrous oxide patients recorded lower QoR scores, and for ICU patients (but not others), a greater length of stay. There was a non-significant reduction in AMI, mortality and awareness. Further details and results of sub-group analyses will be presented at the meeting. |
|
|
|
EM58 ANZCA version [2003-Aug] Q120, [Jul06] Q62
During a transoesophageal echocardiography (TOE) examination the end-diastolic area is found to be 15 cm2 and the end-systolic area 10 cm2 . Based on these measurements one could calculate this patient's A. area ejection fraction to be 33% B. area ejection fraction to be 67% C. ejection fraction to be 50% D. ejection fraction to be 67 % E. fractional area change to be 50% |
ANSWER A
Ejection fraction = (end-diastolic volume - end-systolic volume ) / end-diastolic volume] x 100 (%) Ejection fraction area = (EDV area - ESV area) / EDV area x 100 (%) |
|
|
|
EM37 ANZCA version [2001-Aug] Q57, [2002-Mar] Q52, [Jul06] Q81, [Apr07] (Similar reported question in [Apr96] [Aug96] [Apr97])
Systemic vascular resistance index (SVRI) is calculated from A. systemic vascular resistance multiplied by body surface area B. systemic vascular resistance divided by body surface area C. mean aortic and central venous pressure difference divided by cardiac output D. cardiac index divided by the mean aortic and central venous pressure difference E. none of the above |
ANSWER A
Since SVR = ((MAP-CVP)*80)/CO And CI = CO/BSA SVRI is calculated by substituting CI for CO in the equation for SVR, i.e. SVRI = ((MAP-CVP)*80)/CI Therefore SVRI = ((MAP-CVP)*80)/(CO/BSA) SVRI = ((MAP-CVP)*80)*(BSA/CO) SVRI = (((MAP-CVP)*80)/CO)*BSA SVRI = SVR * BSA |
|
|
|
List the Primary measured haemodynmic data.
|
Arterial Systolic BP
Arterial Diastolic BP Mean arterial pressure Rigth atrial pressure Right Ventricular systolic pressure Right ventricular diastolic pressure Pulmonary artery systolic pressure Pulmonary Artery Systolic Pressure Mean Pulmonary Artery Systolic Pressure Pulmonary Artery Wedge Pressure Left Atrial Pressure Cardiac Output |
Primary measured haemodynamic data
Arterial blood pressure (BP) systolic (SBP) = 90 - 140 mmHg Diastolic (DBP) = 60 - 90 mmHg Mean arterial pressure (MAP): [SBP + (2 x DBP)]/3 = 70 - 105 mmHg Right atrial pressure (RAP) = 2 - 6 mmHg Right ventricular pressure (RVP) systolic (RVSP) = 15 - 25 mmHg Diastolic (RVDP) = 0 - 8 mmHg Pulmonary artery pressure (PAP) systolic (PASP) = 15 - 25 mmHg Diastolic (PADP) = 8 - 15 mmHg Mean pulmonary artery pressure (MPAP): [PASP + (2 x PADP)]/3 = 10 - 20 mmHg Pulmonary artery wedge Pressure (PAWP) = 6 - 12 mmHg Left atrial pressure (LAP) = 6 - 12 mmHg Cardiac output (CO): HR x SV/1000 = 4.0 - 8.0 L/min |
|
|
List the Derived haemodynamic Data
|
Cardiac index (CI): CO/BSA
Stroke volume (SV): CO/HR x 1000 Stroke volume index (SVI): CI/HR x 1000 Systemic vascular resistance (SVR): 80 x (MAP - RAP)/CO Systemic vascular resistance index (SVRI): 80 x (MAP - RAP)/CI Pulmonary vascular resistance (PVR): 80 x (MPAP - PAWP)/CO Pulmonary vascular resistance index (PVRI): 80 x (MPAP - PAWP)/CI |
Derived haemodynamic data
Cardiac index (CI): CO/BSA = 2.5 - 4.0 L/min/m2 Stroke volume (SV): CO/HR x 1000 = 60 - 100 ml/beat Increased SV is associated with bradycardia and positive inotropic agents which increase contractility. Stroke volume index (SVI): CI/HR x 1000 = 33 - 47 ml/m2/beat Systemic vascular resistance (SVR): 80 x (MAP - RAP)/CO = 1000 - 1500 dyne s/cm5 SVR: Systemic vascular resistance. Represents the load applied to the left ventricular muscle during ejection. Systemic vascular resistance index (SVRI): 80 x (MAP - RAP)/CI = 1970 - 2390 dyne s/cm5/m2 Pulmonary vascular resistance (PVR): 80 x (MPAP - PAWP)/CO = <250 dyne s/cm5 PVR is an index of the resistance offered by the pulmonary capillaries to the systolic effort of the right ventricle. Pulmonary vascular resistance index (PVRI): 80 x (MPAP - PAWP)/CI = 255 - 285 dyne s/cm5/m2 |
|
|
EM40 ANZCA Version [2001-Aug] Q35, [2002-Mar] Q15, [2004-Aug] Q31, [2005-Sep] Q11, [Jul06] Q27 (Similar reported question in [Aug96] [Apr97] [Jul97])
A Swan-Ganz catheter can be unreliable for measuring pulmonary artery systolic and diastolic pressures because the length and compliance of the tubing affects the measuring system by A. reducing its resonant frequency B. reducing its frequency response C. reducing its damping coefficient D. inducing a zero error E. inducing baseline drift |
ANSWER A
|
|
|
|
MC55 ANZCA version [2001-Apr] Q45, [2001-Aug] Q34, [2004-Apr] Q34, [2004-Aug] Q7, [Jul06] Q14, [Apr07] Q9 (Similar reported question in [Aug93] [Mar94] [Aug94] [Jul97] [Jul98] [Aug99])
The J-point of the ECG waveform is altered by all of the following EXCEPT A. hypothermia B. tachycardia C. myocardial ischaemia D. calcium channel blockers E. digoxin |

ANSWER D
The "J-point" is the end of the QRS complex and serves at the take-off point of the ST segment. The J Wave deflection, aka Osborn Wave. It represents the approximate end of depolarization and the beginning of repolarization as determined by the surface ECG. J point elevation is very common in young healthy individuals. Has no pathological implications whatsoever. But must be distinguished from ST elevation (J point elevation, the P wave maintains its own shape) Causes of J point depression from baseline 1. hypothermia 2. hypercalcaemia 3. brain injury, SAH 4. early repolarization, tachycardia 5. epicardial or endocardial ischemia 6. percarditis 7. RBBB/LBBB 8. RVH / LVH 9. Digitialis Clinical Significance? Early sign of tachyarrthmias has been reported |
|
|
|
MC114 ANZCA version [2002-Aug] Q133, [2003-Apr] Q37, [2006-Mar] Q50, [Jul06] Q4
In Wolff-Parkinson-White (WPW) syndrome, A. the delta wave is caused by a delay in conduction in the accessory pathway B. the PR interval is of normal duration but the QRS complex is widened C. a narrow complex supraventricular tachycardia (SVT) is the most common form of arrhythmia D. central venous cannulation is unlikely to trigger SVT E. cardioversion of arrhythmias is seldom effective |
ANSWER C
A : False. Accessory pathway is not delayed, it is fast (ventricular preexcitation) B : False. Short PR. Apparent long QRS as P wave slurs into the QRS complex via delta wave C : True. So-called 'orthodromic' tachycardia via the rapid normal pathway (with retrograde conduction via the accessory pathway) is commonest. D : FALSE. CVC insertion is not likely to cause SVT but it could "theoretically predispose" to the the arrhythmia according to Stoelting's textbook. E : False. Cardioversion or procainamide are standard therapies for antidromic (broad-complex) tachycardia. Can also be used for orthodromic tachycardia. |
|
|
|
Wolff-Parkinson-White Syndrome
|
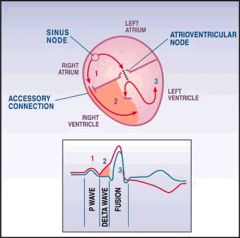
WPW syndrome is currently defined as a congenital abnormality involving the presence of abnormal conductive tissue between the atria and the ventricles in association with supraventricular tachycardia (SVT).
A form of pre-excitation characterized by 3 ECG features: * a short PR interval (<120ms) * long QRS interval (due to fusion of delta wave & QRS) (>120ms) with presence of a delta wave (not seen in all leads, slurred onset due to onset of early part of QRS) *secondary ST-T wave changes * Occurs in 1 out of 10,000 people * Can be asymptomatic or associated with tachycardia & palpitations * Concern that individuals with WPW are at risk of ventricular fibrillation if they were to go into AF * When WPW is present the ST segments cannot be used to identify ischemia and Q waves are actually negative delta-waves and not due to infarction. * One of the ECG patterns where the R wave can be greater than S wave in V1 and V2. Acute Management ACLS guidelines -BAC's -IV access, cardiac monitoring -O2 is hypoxic -DC cardioversion if unstable -chemical cardioversion if stable -ACLS support if cardiac arrest DC cardioversion -minimum effective energy should be used and energy should be titrated -synchronised 100J should terminate most SVT, second shock at 200J -watch out for a. rarely shock can cause VT b. embolic episodes (1-3%) especially when in association with AF > 48 hours, consider TOE to exclude left atrial thrombus Chemical Cardioversion -adenosine -verapramil Atrial Filbrillation -principle is to prolong the antegrade refractory period of the accessory pathway relative to the AV node. -which is different to non-WPW AF where the aim to prolong the refractory period of the AV node -the use of AV nodal blockers in atrial fibrillation (eg Beta-blockers, Digoxin, Ca Channel Blockers) in theory may increase the risk of ventricular fibrillation by relatively increasing conductance through anterograde accessory pathways and increasing ventricular rate. -thus must be avoided, primary synchronized cardioversion should be first line treatment if unstable -Class Ic Antiarrythmics, flecainide and procainamide, may be tried -Procainamide : 17mg/kg IV, not exceeeding 50mg/min : blocks the AP but increases transmission through AV Further Management 1. AP ablation 2. ongoing pharmacological prophylaxis |
|
|
|
MC135 [Jul06] Q122 ANZCA Version
You are called to the cardiac catheter lab to assist when a 55-year-old man with unstable angina becomes restless during difficult placement of a right coronary artery stent. When you arrive he is conscious and responding to voice. He is sweating with a pulse of 60 beats per minute in sinus rhythm, blood pressure measured from arterial catheter of 80/50 mmHg and Sp02 of 97%. The arterial pressure wave has an exaggerated fall with inspiration. The most appropriate next clinical intervention would be to A. administer atropine B. commence an adrenalin infusion C. perform a quick transthoracic echocardiograph D. sedate and intubate E. transfer to operating theatre immediately |
ANSWER C
Likely diagnosis is tamponade secondary to RCA rupture with ?AV node bradycardia? Differential * Cardiac Causes -Tamponade/effusion secondary to RCA rupture, although would expect a higher CVP -Cardiogenic shock due to infarction or ischaemia - Pericarditis/cardiomyopathy -Pulmonary embolism * Pulmonary Causes -Tension Pneumothorax -Severe Asthma * Non-cardiac causes -Hypovolaemic shock -Diuretic overdose -Occult haemorrhage -Anaphylaxis (rare, but would explain low CVP and tachycardia may be blocked by beta-blockers) -Drug error (but not an anaesthetic overdose, because he's anxious) |
|
|
|
MC137 [Jul06] Q104 ANZCA Version
A common finding in hereditary prolonged QT syndrome is A. bifid T waves B. inverted P waves C. prolonged QRS complex D. R axis deviation E. short PR interval |
ANSWER A
QT interval is generally measured in lead II, as the T-wave ending is usually discrete and the QT interval in lead II has a good correlation with the maximal QT measurement from the whole 12-lead ECG. In many LQTS, the QT interval is not prolonged but have increased variability known as QT dispersion. QTD is significantly increased in symptomatic LQTS patients, but may not be signifcantly different to control values in asymptomatic LQTS patients. T wave and U wave abnormalities are common in LQTS. T waves may be larger, prolonged, or have a notched, bifid or biphasic appearance. A pathognomonic feature of LQTS is so-called T wave alternans, where there is beat-tobeat variation in T wave amplitude. Exercise testing of patients with LQTS may provoke prolongation of the QTc. A notched T wave during the recovery phase of exercise is highly suggestive of LQTS. Head up tilt testing may also provoke abnormal QT prolongation and arrhythmias. |
|
|
|
Long QT syndrome
|
"Long QT syndrome (LQTS) is a congenital disorder characterized by a prolongation of the QT interval on electrocardiogram (ECG) and a propensity to ventricular tachyarrhythmias, which may lead to syncope, cardiac arrest, or sudden death".
Pathophysiology A malfunction of cardiac ion channels results in impaired ventricular repolarization that can lead to a characteristic polymorphic ventricular tachycardia known as torsades de pointes. Epidemiology -30% of patients present with unexplained syncope or aborted sudden death. -Only about 60% are symptomatic at time of diagnosis. -Many are identified when family members are screened after episodes of syncope or cardiac death. -The prevalence may be as high as 1 per 1100-3000 Diagnosis -QTc = Measured QT / Square root of RR interval (all measured in seconds). QTc of >440ms is considered prolonged, but about 6% of patients with symptomatic LQTS will have a normal QTc. -Diagnostic criteria include ECG findings, clinical history and family history. -ECG findings includes length of QTc, Torsades, T wave alterans, Notched / bifid / biphasic T waves and low heart rate for age. Long Term Management -Untreated, symptomatic LQTS has a mortality exceeding 20% in the first year after diagnosis and approaches 50% within 10 years. -Asymptomatic patients with incidental LQTS (<0.5% mortality per year) and asymptomatic family members (0.5% mortality per year) have a very low risk of syncope or sudden death. -Beta blockade, anti-bradycardia pacing, implantation of cardioverter defibrillators, and left cardiac sympathetic denervation are used in the treatment of these patients. However, these treatment modalities do not guarantee the prevention of sudden cardiac death. Certain drugs, including anesthetic agents, are known to contribute to QT prolongation. |
Anaesthesia management
-Anaesthesia in patients carries a very high risk of malignant ventricular arrythmias, however despite beta blockade patients remain at risk. -Patients should be on maintenance beta blocker therapy and this much be continued throughout the perioperative period, including IV replacement if enteral intake is not possible. Electrolytes must be normal (especially K+, Mg++ and Ca++) Intraoperative management should focus on prevention of excessive sympathetic activity and avoidance of factors that can prolong the QT interval. * Have pacing apparatus, defibrillator and drugs available. * Consider induction and maintenance with propofol (which may shorten the QTc interval) * Response to intubation must be adequately blunted * Avoid high intra-thoracic pressures and PEEP which simulates a Valsalva and can prolong the QT. * Extubate deep * Avoid reversal * Manage Torsades de pointes Drugs which prolong QTc * Volatile anaesthetic agents all prolong the QT interval * Thiopentone * Atropine, Glycopyrrolate * Class Ia antiarrythmics (Disopyramide, Quinidine, Procainamide) * Class Ic antiarrythmics * Class III antiarrythmics * Butyrophenones (Droperidol, haloperidol) * Phennothiazine and atypical anti-psychotics * SSRIs * Macrolide antibiotics * Cisapride |
|
|
MC138 ANZCA Version [Jul06] Q144
Ebstein's abnormality describes a congenital defect of the A. aortic valve B. mitral valve C. pulmonary valve D. pulmonary veins E. tricuspid valve |
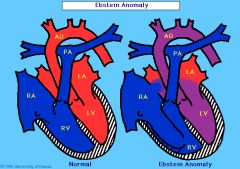
ANSWER E
Ebstein's anomaly is a rare congenital heart defect where there is apical displacement of the septal and posterior tricuspid valve leaflets with to atrialization of the right ventricle with a variable degree of malformation and displacement of the anterior leaflet. Usually associated with ASD. The leaflets are unusually deep in the right ventricle. The leaflets are often larger than normal. Leading to large TR and RHF. SVT and thrombus formation is common. |
|
|
|
MC139 ANZCA Version [Jul06] Q119 Apr07 Q12
A diagnosis of pulmonary embolism is most strongly suggested by A. intraluminal filling defects or vascular cutoffs on angiography B. PaO2 less than 85 mmHg and an abnormal lung perfusion scan C. PaO2 less than 85 mmHg and an elevated PaCO2 D. right ventricular hypertrophy with right ventricular strain and right axis deviation on electrocardiography E. "unmatched" ventilation-perfusion defects |
ANSWER A
|
|
|
|
MC140 [Mar06] Q119 [Jul06] Q42 ANZCA VERSION
Regarding a 75-year-old female patient with moderate aortic stenosis presenting for an elective hip replacement, A. atrial systole has an increased contribution to stroke volume (compared to a patient with no aortic stenosis) B. beta-blockers are poorly tolerated in this degree of aortic stenosis C. hypotension is better tolerated than hypertension D. rheumatic heart disease is the commonest aetiology in this age group in Western Society E. single shot spinal anaesthesia is the preferred method of anaesthesia |
ANSWER A
A. TRUE : hypertrophied ventricle is stiff, causing diastolic dysfunction and reduced compliance. . Consequently, left ventricular filling becomes dependent on atrial contraction with atrial systole contributing 40%, instead of the usual 20%, of left ventricular end-diastolic volume. The left atrium hypertrophies to maintain left ventricular filling. Preservation of sinus rhythm becomes vital for the maintenance of cardiac output. B. FALSE : LV is dependent on preload and filling pressures, a normal to high HR is preferred. Tachy and bradycardia should be avoided C. FALSE : Avoidance of systemic hypotension is essential. Hypotension leads to myocardial ischaemia and a downward spiral of reduced contractility causing further falls in blood pressure and coronary perfusion. D. FALSE : Degenerative calcific aortic stenosis: This is now the most common form of aortic stenosis in the UK and tends to occur over the age of 70 yr. E. FALSE : Anaesthetic techniques that reduce systemic vascular resistance (e.g. regional neuroaxial techniques) must be used with extreme caution although successful cases of carefully titrated epidural and spinal blocks using catheters have been reported. Slow titration of epidural anaesthesia may be done with caution. |
|
|
|
MC151 ANZCA Version [Jul06] Q132, [Apr07]
The QT interval may be prolonged by each of the following EXCEPT A. high intra-thoracic pressure B. hypothermia C. magnesium sulphate D. suxamethonium E. volatile anaesthetic agents |
ANSWER C
MgSO4 does not prolong the QTI, it is treatment for Torsades (30mg/kg). |
|
|
|
MC19b ANZCA Version [Jul06] Q17, [Apr07]
A 50 year old patient is admitted with acute chest pain. An ECG shows tall R waves in lead V1. The most likely diagnosis is A. occlusion of the anterior descending coronary artery B. a lateral myocardial infarction C. pulmonary infarction D. posterior myocardial infarction E. occlusion of the circumflex artery |
ANSWE D
Tall R in V1 is defined as R/S ratio equal to or greater than 1. This is normal in ONLY 1% of presentations. Causes include 1. RBBB 2. left ventricular ectopy 3. Posterior MI (tall R V1-3, ST depression V2/3, TWI V1-3. Tall T V2) 4. Right ventricular hypertrophy 5. Right ventricular strain, dilation eg PE 6. WPW syndrome with left sided accessory pathway 7. HOCM 8. Dextrocardia 9. Normal Variant 10. Misplaced electrodes |
|
|
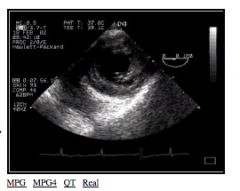
Label the structures on this Transgastric View on TEE
|

These are acquired by advancing probe into the stomach.
Used for assessment of 1. LV fucntion 2. Myocardial ischmia PM = Posteromedial papillary muscle AL = Anterolateral papillary muscle RV = Right ventricle LV = Left ventricle IVS = interventricular septum -IW = inferior wall LV -PW = posterior wall LV -AW = anterior wall of LV GREEN : LAD supplies AW RED : CIRC supplies PW BLUE : RCA supplies IV and IW |
|
|
Label the structures on this Four Chamber View in TOE
|
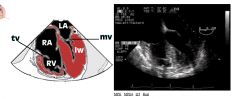
This is a mid-oesophageal view.
This is obtained 35-37cm from the incisor teeth. Uses include assessments of 1. Atria 2. Ventricular Septum 3. Ventricles 4. Both AV valves Good view of the mitral valve and interatrial septum. It is poor at assessing the function of the LV. RA = right atrium RV = right ventricle IW = inferior wall TV = tricuspid valve MV = mitral valve |
|
|
|
MC149 ANZCA Version [Apr07]
Reverse splitting of the 2nd heart sound is caused by A. acute pulmonary embolism B. ASD C. complete LBBB D. severe MR E. pulmonary HT |
ANSWER D
Physiology of the Second Heart Sound -Audible component of the closure of aortic and pulmonary valves -A2 followed by P2, separated only by 0.02 - 0.08 seconds. -Although contraction of both ventricles occurs at the same time, difference in opening and closure are due to differences in impedance of each vascular bed -as PVR is low, PV opens sooner and closes later -as SVR is high, AV opens later and closes sooner -therefore A2-P2 -this interval is widened by deep inspiration, known as Physiological Splitting. Abnormal Splitting of Second Heart Sound (1) persistently single; -S2 remains single throughout respiratory cycle -most commonly due to inaudibility -in setting of CHD : absence of PV : Fontans (pulmonary atresia, severe PV stensosis, dysplastic PV, transposition of great arteries) (2) persistent (audible expiratory) splitting, with normal respiratory variation; -most common cause if RBBB (3) persistent splitting without respiratory variation (fixed splitting); -A2 and P2 is constantly wide and remains unchanged during respiratory cycle -Hallmark of ASD (4) reversed (paradoxical) splitting. -Reversed sequence of semilunar valve closure P2-A2 -Common causes : LBBB and Right ventricular PPM (activation of the RV before LV) -Other causes : RV ectopic beats, prolonged LV mechanical systole, HOCM, Severe hypertension, PDA - |
|
|
|
MC42 ANZCA version [2004-Apr] Q75
Abnormal Q waves are NOT a feature of the ECG in A. an old myocardial infarction B. left bundle branch block C. recent transmural myocardial infarction D. digitalis toxicity E. Wolff-Parkinson-White syndrome |
ANSWER D
Q waves transmural MI, LBBB, hyperkalaemia, WPW, amyloid, HOCM, cardiac contusion, myocarditis, dextrocardia, reverse limb leads |
|
|
|
MC146 ANZCA version [2005-Sep] Q113, [Apr07]
In the diagnosis of postoperative myocardial infarction A. echocardiography has little role to play B. infarct size can be judged from cumulative enzyme release C. new left bundle branch block on ECG confirms acute infarction D. serum troponins have high sensitivity and are detectable for up to 5 days E. ST segment elevation is extremely common |
ANSWER D
|
|
|
|
ANZCA Version [APR07]
Regarding atrial fibrillation A. aspirin is as effective as warfarin for the prevention of embolic stroke in elderly patients B. patients should not receive warfarin therapy unless they have risk factors for embolic stroke C. patients who are converted to sinus rhythm should be placed on rhythm maintenance therapy D. rhythm control has NOT been shown to be superior to rate control E. the best drug for rate control during exercise is digoxin |
ANSWER B and D
Embolic Risk of AF : Application of the CHADS2 CHF - 1 HT - 1 Age > 75 - 1 DM - 1 CVA - 2 Score of *0 : 0.5-1.7% Risk per year of stroke, Commence Aspirin only *1 : Unsure if stroke benefit outweights bleeding risk if patient is female; greater >65 OR has any artherosclerotic disease (PVD/CAD) they should be started on warfarin (CHA2S2VASc score) *>2 : 4-18% Risk per year of stroke, commence warfarin AFFIRM, PIAF, RACE, STAF which show that rate control is at least as effective as rhythm control in improving symptoms and functional capacity, particularly in those over 65yrs. AFFIRM -the Atrial Fibrillation Follow-up Investigation of Rhythm Management -designed to determine whether restoration and maintenance of SR is associated with a lower all-cause mortality when compared to the alternative strategy of anticoagulation and rate control in patients with AF -The sample size for this trial was calculated at 5300, but after screening 7400 patients, enrollment was stopped at just over 4000 -Sotalol and amiodarone (for rhythm control) -ventricular rate control was achieved with digoxin, beta-blockers, and rate-lowering calcium-channel blockers -no difference in the all cause mortality Rhythm Control Limb -at least 80% of the patients could be stabilized into sinus rhythm, and 60% remained in sinus rhythm after 5 years -strangely, a larger number were hospitalized -all cause mortality was greater when analyzed with intention to treat |
|
|
|
MC160 ANZCA Version [Jul 2007]
The strongest indication for the use of transoesophageal echocardiography during major non-cardiac surgery is A. recent myocardial infarction (less than six weeks old) B. acute significant intra-operative ST segment depression on ECG C. massive intraoperative blood loss D. a history of severe valvular heart disease E. unexplained significant intraoperative hypotension |
ANSWER E
Practice Guidelines for TOE from ASA 2010 1. Known heart disease which would cause hemodynamic, pulmonary or neurological compromise eg. ASD, AS, HOCM, MI 2. Unexplained hypotension 3. Unexplained hypoxemia 4. Where life threatening hypotension is anticipated |
|
|
MC143 ANZCA version [2003-Aug] Q138, [2004-Apr] Q37, [2005-Sep] Q14, [Jul07], [Apr08]q1
This ECG (Lead V5) most likely represents A. Wolff-Parkinson-White (WPW) syndrome B. atrial fibrillation C. complete heart block D. atrio-ventricular junctional rhythm E. sinoatrial block |
ANSWER D
* Regular rate -> so not AF B * Rate 75/min -> too fast for complete heart block - so not C * No delta wave (so not WPW (option A)) * Narrow QRS -> Supraventricular rhythm PLUS (no P wave before QRS) ->AV junctional rhythm (D) |
|
|
|
MC100 ANZCA version [Jul00] [2001-Apr] Q41, [Jul07]
A 24 year old female with mitral valve prolapse develops atrial flutter during a diagnostic laparoscopy. The drug most likely to revert this arrhythmia is A. Digoxin B. Amiodarone C. Verapamil D. Esmolol E. Adenosine |
None of them?
With regard to Atrial Flutter (not AF): Reversion best achieved with DC Cardioversion Reversion rate for pharmacological agents: * Ibutilide 38-76% * Sotalol 19% * Flecanide 13% * Verapamil 5% * Adenosine/Amiodarone -not of use in cardioverting Atrial Flutter ( but useful for rate control) |
|
|
|
MN40 ANZCA version [2002-Mar] Q91, [2005-Sep] Q83, [Jul07], [Mar10]
An INCORRECT statement regarding the autonomic nervous system is that A. autonomic dysfunction is a predictor for worse long term survival after myocardial infarction B. heart rate responses are primarily mediated through the sympathetic nervous system C. inhalation anaesthetics all impair autonomic reflex responses D. autonomic dysfunction is a predictor for haemodynamic instability following anaesthetic induction E. low heart rate variability is associated with worse cardiac outcomes following non-cardiac surgery |
ANSWER B
A. FALSE : There also is strong evidence in patients that autonomic balance and vagal reflexes influence morbidity and mortality after MI. Patients surviving MI who had either low HRV or low baroreflex sensitivity had an increased risk of subsequent sudden cardiac death B. TRUE : The sympathetic component is primarily involved in adjusting peripheral vascular tone and plays a lesser role in the reflex regulation of HR and cardiac output. The vagal component is primarily involved in regulating HR. C. FALSE : All inhalational agents impair the autonomic nervous system D. FALSE : it is well documented that patients with impaired autonomic reflexes (e.g., patients with diabetes) have greater intraoperative BP lability compared with autonomically intact patients. [2,3] In addition, it now is clear that many of the sedative, hypnotic drugs used for induction of anesthesia and all of the potent inhaled anesthetic gases in clinical use impair autonomic reflex responses. E. FALSE : low HR variability (HRV), an index of impaired cardiac-vagal tone, is an independent predictor of mortality after non-cardiac surgery |
|
|
|
SG65 [Jul07]
To improve oxygenation in a patient intubated and ventilated for a laparotomy you adjust the ventilator settings to apply 10 cm H2O of PEEP (positive end-expiratory pressure). The patient's blood pressure falls from 130/80 to 90/50 mmHg. The addition of PEEP may result in a fall in blood pressure because PEEP causes A. decreased myocardial contractility B. decreased venous return C. increased left ventricular afterload D. increased left ventricular compliance E. increased right ventricular afterload |
ANSWER B
PEEP may reduce cardiac output by reducing venous return, by increasing pulmonary vascular resistance, and by shifting the interventricular septum to the left, thus reducing the left ventricular end diastolic volume. |
|
|
|
MC156 ANZCA Version [Jul07]
Regarding patients aged 65 years or older with recurrent atrial fibrillation (AF) A. amiodarone and digoxin have similar efficacy in restoring sinus rhythm B. patients who have been reverted to sinus rhythm should still remain on warfarin therapy C. patients who remain in atrial fibrillation with heart rates less than 80 beats per minute do NOT require long term warfarin therapy D. peri-operative therapy with a beta-blocker will commonly lead to restoration of sinus rhythm E. restoration of sinus rhythm with electrical DC cardioversion improves long-term survival in comparison to controlling heart rate alone |
ANSWER B
A. FALSE : Amiodarone and sotolol are used for chemical cardioversion, digoxin is used for rate control B. TRUE : a patient who undergoes cardioversion should at least remain on anticoagulative therapy for a short while after DC reversion because of the risk of atrial thrombus formation in the stunned atrium. C. FALSE : not part f CHADS2 Score or HAS-BLED D. FALSE : perioperative beta blockers will not restore SR with recurrent AF, beta blockers are mainly used for rate control E. FALSE : AFFIRM trial showed no survival benefit |
|
|
|
MC76 [Jul97] [Apr98] (type A)
Which new change on ECG is most likely to indicate acute ischaemia? (Type A) A. 2mm horizontal ST depression in 60yr old male undergoing TURP with spinal B. 2mm ST depression in previously fit 20yr old female GA caesarean C. 0.7mm ST depression in a 60 yr old male undergoing TURP with spinal D. 2mm downsloping ST depression in 30yr old male craniotomy for SAH E. T-wave inversion in 60yr old male TURP under spinal |
ANSWER A
|
|
|
|
MC162 ANZCA version [Jul07] Q140
In acute coronary syndromes with ST elevation on ECG A. aspirin should be administered only after reperfusion strategies have commenced B. patients can wait up to 24 hours from onset of ischaemic symptoms before implementation of a reperfusion strategy C. patients should have elevated cardiac enzymes before proceeding to reperfusion strategies D. patients undergoing reperfusion strategies should have aspirin or clopidogrel but NOT both E. percutaneous coronary intervention is preferable to fibrinolytic therapy |
ANSWER E
|
|
|
|
PH61 ANZCA version [Jul07]
A morbidly obese 140kg, 40-year-old male is scheduled for cholecystectomy. He has no history of cardiac disease. His ideal body weight is 70kg. Compared to his resting cardiac output at ideal body weight, his resting cardiac output at his weight of 140 kg would be A. decreased by 20% or more B. decreased by 10% C. unchanged D. increased by 10% E. increased by 20% or more |
ANSWER D
Miller 6th edition says CO increases by 0.01L/min for each kg of adipose tissue. If this is true, a 10% increase in CO represents 50kg extra adipose tissue, whilst a 20% increase in CO represents 100kg extra adipose tissue (ie, more than 140kg!). Furthermore, not all the extra weight in the 140kg person is adipose tissue, some will be due to increased plasma, red cells and interstitial fluid. |
|
|
|
TMP-127 [Apr08]
When considering an acute myocardial infarction: A. Aspirin and clopidogrel should not be given together B. PCI is better than thrombolysis C. Aspirin should not be given prior to MI confirmed with cardiac enzyme rise D. Reperfusion can be delayed for 24hrs E. something about confirming cardiac enzyme elevation before instituting reperfusion strategies |
ANSWER B
A. FALSE : All patients with AMI should be loaded with aspirin and continued life long. Clopidogrel loading depends on whether the institution offers CABGs, if CABGs are not offered then clopidogrel is commenced. Clopidogrel is continued 1. Angioplasty no clopidogrel 2. BMS 1 month 3. DES 1 year |
|
|
|
MM Carcinoid syndrome - finding on examining heart:
A. Fine inspiratory crepitations B. Systolic murmur at apex C. Systolic murmur at left sternal edge D. Murmur at apex with opening snap E. Pericardial rub |
ANSWER C
A carcinoid tumor is a tumor that secretes large amounts of the hormone serotonin. These tumors usually: * arise in the gastrointestinal tract and * from there may migrate (metastasize)to the liver. Carcinoid tumors also sometimes develop in the lung. Only about 10% of the people with carcinoid tumors will develop the carcinoid syndrome. Major symptoms of this syndrome include: * hot, red facial flushing, * diarrhea and * wheezing. Carcinoid syndrome occurs when the tumors produce excessive amounts of serotonin or other substances. The presence of carcinoid syndrome suggests: * the presence of liver secondaries * a non-GI carcinoid tumour * massive mediator release by tumour The liver normally breaks down the mediators (vasoactive compounds) secreted by the tumour. As most carcinoid tumours are in the GIT, the mediators are released into the portal veins, and broken down in the liver. To cause carcinoid syndrome then indicates the liver is being bypassed or overwhelmed. Carcinoid Heart Disease * Develops in 50% of patients with carcinoid syndrome o hence in about 5% of people with a carcinoid tumour * It results in fibrosis of myocardial tissues, especially on the Right side of the heart o tricuspic regurgitation is the most common finding o pulmonary regurg and/or stenosis also occurs o less than 10% of patients with carcinoid have mitral or aortic regurg o constrictive pericarditis has also been described |
|
|
|
MM13 ANZCA version: [2003-Aug] Q39 (Similar reported question in [Aug96] [Apr97])
Carcinoid tumours A. arise in the gastrointestinal tract in approximately 40% of cases B. result in the carcinoid syndrome in approximately 50% of cases C. release vasoactive agents including histamine, kallikrein and prostaglandins D. are NOT associated with hypergylcaemia E. do not usually result in intraoperative hypotensive episodes |
ANSWER
A. FALSE : Gastrointestinal carcinoids are slow growing neuroendocrine tumors that may arise anywhere in the gastrointestinal tract. *small intestine (30%) *rectum (12%) *colon (8%) *appendix (8%) *stomach (10–30%) B. FALSE : Carcinoid syndrome occurs in less than 10%; hepatic metastases are generally present. C. TRUE : Carcinoid tumors can contain numerous GI peptides including gastrin, insulin, somatostatin, motilin, neurotensin, tachykinins (substance K, substance P, neuropeptide K), glucagon, gastrin-releasing peptide, vasoactive intestinal peptide, pancreatic peptide, other biologically active peptides (corticotropin, calcitonin, growth hormone), prostaglandins, and bioactive amines (serotonin). D. E. FALSE : manipulation of the tumour you may get carcinoid hypotnesive crises no matter where the tumour lies |
|
|
|
MC (Q132 Aug 2008) DC cardioversion - LEAST likely indicated for
A atrial fibrillation B atrial flutter C multifocal atrial tachycardia D paroxysmal atrial tachycardia E ventricular tachycardia |
ANSWER C
Multifocal AT are resistent to DC cardioversion Indications for DC 1. narrow or wide QRS complex tachycardia (ventricular rate >150) who is unstable (eg, chest pain, pulmonary edema, lightheadedness, hypotension) should be immediately treated with synchronized electrical cardioversion 2. Synchronized electrical cardioversion may be used to treat stable VT that does not respond to a trial of intravenous medications 3. In hemodynamically stable patients with atrial fibrillation, atrial flutter, or other supraventricular tachycardia (SVT), synchronized electrical cardioversion can also be used to electively restore sinus rhythm. Contraindications 1. known digitalis toxicity -associated tachycardia. 2. Atrial Tachycardias (including multifocal) 3. AF with risk of developing or known left sided thrombus |
|
|
|
MC03 ANZCA version [2004-Aug] Q39, [2005-Apr] Q2 (Similar reported question in [1986] [1988] [1989] [Mar90] [Sep90] [Mar91] [Aug91] [Mar92] [Jul98])
The proportion of adult patients with a probe-patent foramen ovale is A. 0-10% B. 10-20% C. 20-35% D. 35-50% E. greater than 50% |
ANSWER C
Anatomic closure of the foramen ovale occurs between 3 months and 1 year of age, although 20% to 30% of adults have probe-patent foramen ovales. -Stoelting |
|
|
|
MC03b ANZCA version [2002-Mar] Q79, [2002-Aug] Q30
An INCORRECT statement regarding patent foramen ovale (PFO) in adults is that: A. it is found in 5% of patients at postmortem examination B. it can cause hypoxaemia C. it is best seen using transoesphageal echocardiography D. an asymptomatic PFO requires no intervention E. the sitting position should be avoided in patients with a PFO |
ANSWER A
A : False - 30% have a probe PFO on autopsy, and in vivo, 20% can detect on sensitive tests e.g colour Doppler B : True - minor R-> L shunt occurs commonly with a large ASD -> mild decrease in SpO2 to 93-95%, and any increase in right sided pressure (e.g Valsalva, PE, volume overload) -> shunt C : True - "Transesophageal contrast echocardiography provides superior visualization of the atrial septum and therefore is preferred to transthoracic contrast echocardiography for detecting patent foramen ovale." EMedicine D : True - "Most patients with a patent foramen ovale as an isolated finding receive no special treatment" EMedicine E : True a relative C/I as risk of air embolism is high -> risk of paradoxical embolism with a PFO, |
|
|
|
MC20b ANZCA version [2002-Aug] Q111, [2003-Apr] Q65, [2004-Aug] Q83, [2005-Apr] Q51
Electrocardiographic changes in acute hyperkalaemia include A. the appearance of a J wave B. loss of P waves C. flattening of the T wave D. a prominent U wave E. a prolonged QT interval |
ANSWER B
In orders of appearance 1. Tall peaked T waves with shortened QT 2. Lengthening of PR and QRS 3. Loss of P wave 3. Lengthening of QRS to Torsades J-wave mainly with hypothermia and hypercalaemia U-wave seen in mainly precordial leads V2-V4. -?early repolarization of the His-Purkinje system -typically less than 0.2mV and is clearly separate from the T wave -Prominent U waves are most often seen in hypokalemia, but may be present in hypercalcemia, thyrotoxicosis, or exposure to digitalis, epinephrine, and Class 1A and 3 antiarrhythmics, as well as in congenital long QT syndrome and in the setting of intracranial hemorrhage. |
|
|
|
MC20a [Aug91]
What are the ECG changes of hyperkalaemia? A. Prolonged PR interval B. Prolonged QRS C. Peaked T wave D. Shortened PR interval E. Deep S wave |
ANSWER A, B, C
|
|
|
|
MC65 ANZCA version [2002-Mar] Q53, [2002-Aug] Q63, [2004-Apr] Q59, [2004-Aug] Q84, [2005-Sep] Q58, [Mar06] Q38, [Jul07] (Similar reported question in [Apr96] [Apr97] [Jul97])
Characteristic cardio-pulmonary effects of pulmonary thrombo-embolism include A. hypoxaemia due to excess perfusion of lung units with a low V/Q ratio B. hypercarbia due to an increase in physiological dead-space C. reverse splitting of the second heart sound D. an increase in compliance of the left ventricle E. an increase in coronary blood flow to the right ventricle during systole |
ANSWER A
|
|
|
|
MC59b ANZCA version [2003-Apr] Q125, [2003-Aug] Q85, [2005-Sep] Q69, [Mar06] Q48 [Mar10] [Aug10]
In the management of torsades de pointes (polymorphic ventricular tachycardia), all the following drugs may be useful EXCEPT A. amiodarone B. isoprenaline C. [[lignocaine] D. magnesium E. phenytoin |
ANSWER A
|
|
|
|
MC59 Black Bank version [Aug94] [Aug95] [Apr96] [Aug96] [Mar00] [Jul00] (type A)
The least useful treatment in torsades de pointes is: A. Lignocaine B. Diisopyramide C. Magnesium D. Overdrive pacing E. Isoprenaline F. Defibrillation G. Digoxin H. Adrenaline I. Procainamide |
ANSWER A
|
|
|
|
MC84c ANZCA version [2005-Apr] Q49, [2005-Sep] Q67 (Similar version reported in [Apr98] [Aug99] [Mar00] [Jul00])
In providing anaesthesia for a patient with Eisenmenger's syndrome, it is NOT true that A. an important goal is to maintain an optimal shunt, by preventing changes to pulmonary vascular resistance (PVR) or systemic vascular resistance (SVR) B. the patient's high haemoglobin should be maintained and blood loss monitored closely C. a gaseous induction with sevoflurane presents an effective method for anaesthesia and avoids cardiovascular compromise D. if general anaesthesia is required, ketamine is an - appropriate choice of drug E. careful attention to intravenous infusions and drug administration is needed to prevent paradoxical air embolism |
ANSWER B
A. FALSE : fine balance of PVR and SVR to maintain the optimal shunt. B. TRUE : Compensate for hypoxia by erythrocytosis with increase in Hct. HCT>65% should have vensection before to minimize risk of thromboembolism. Blood loss should be closely monitored. C. FALSE : Even though gaseous induction theoretically will drop SVR and increase R to L shunt. D. FALSE : Ketamine has been the most popular agent for anesthetic induction in patients with cyanotic conditions because it increases SVR and cardiac output, thereby diminishing the magnitude of R-L shunting. E. FALSE : care should be taken to avoid iatrogenic air emoblism as there is a clear right to left shunt Eisenmenger's syndrome -patients who left to right shunt has been reversed resulting from increased PVR -explosure of pulmonary vasculature to increased blood flow and pressure (VSD or ASD) results in pulmonary obstructive disease -obliteration of pulmonary vascular bed progresses with increases in PVR -when PVR = SVR : eisenmenger's syndrome -shunt reversal in 50% untreated VSD and 10% untreated ASD Signs and symptoms -cyanosis -decreased exercise tolerance -paplitations are common due to AF/AFlu -arterial hypoemia resulting in polycythemia : visual disturbances, headache, dizziness, paresthesia -hemoptysis -thrombosis -CVA and brain abscess -sudden death Treatment -mainly prevention -phlebotomy with isovolmetric replacement to reduces risks of hyperviscosity -lung transplant with repair of heart defect in selected cases Anaesthetic Management * Preop assessment: Cardiac function ? failure, degree of shunt (SpO2, echo), rhythm, antiarrhythmics, hyperviscosity syndrome (HCT > 65% ie Hb 210), associated congenital problems. * Monitoring: Art, CVL, ? TOE, ? PICCO. ? Monitor sats in both arms (PDA). * Preinduction: antibiotic prophylaxis(amoxycillin and gentamicin), ? phlebotomy (haemodilution). * Physiological goals: maintain SVR:PVR ratio, maintain cardiac output. Prevent air/paradoxical embolus. * Induction: anything is OK, maintain SVR. * Maintenance: anything is OK except N2O. Consider selective pulm vasodilator (NO, PGI2). * Neuraxial: slow onset and watch SVR. * Postop: ICU. DVT prophylaxis. Effective analgesia. |
|
|
|
MC109 ANZCA version [2001-Aug] Q89, [2002-Mar] Q57, [2005-Apr] Q97, [2005-Sep] Q32
In patients with mitral regurgitation A. left ventricular damage does NOT occur before the onset of symptoms B. mitral valve replacement has a lower operative mortality and incidence of late adverse outcomes compared to mitral valve repair C. an ejection fraction of less than 60% may be an indication for surgery, even in the absence of symptoms D. long term vasodilators have been shown to delay the need for surgery E. the presence of a third heart sound always indicates heart failure |
ANSWER C
A. FALSE : Unlike stenotic cardiac valve lesions, regurgitant cardiac valve lesions often progress insidiously, causing left ventricular damage and remodeling before symptoms have developed B. FALSE : Mitral valve repair is preferred to mitral valve replacement because it restores valve competence, maintains the functional aspects of the mitral valve apparatus, and avoids insertion of a prosthesis C. TRUE : Survival may be prolonged if surgery is performed before the ejection fraction is less than 60% or before the left ventricle is unable to contract to an end-systolic dimension of 45 mm (normal < 40 mm). Symptomatic patients should undergo mitral valve surgery even if they have a normal ejection fraction D. FALSE : Although vasodilators are useful in the medical management of acute mitral regurgitation, there is no apparent benefit to long-term use of these drugs in asymptomatic patients with chronic mitral regurgitation E. FALSE : S3 can be heard and recorded in healthy young adults. However, it is usually abnormal in patients over the age of 40 years, suggesting an enlarged ventricular chamber |
|
|
|
MC118 ANZCA version [2004-Apr] Q110
An elective surgical patient with hypertrophic obstructive cardiomyopathy becomes hypotensive (systolic pressure 70 mmHg and heart rate 60 beats.min-1) during intravenous induction of anaesthesia. The most appropriate initial therapy would be aimed at increasing A. blood volume B. degree of myocardial depression C. heart rate D. myocardial contractility E. vasoconstriction |
ANSWER E
Aims with HOCM are the same as AS 1. Slow 2. Full 3. Tight 4. Avoid increases in contactility |
|
|
|
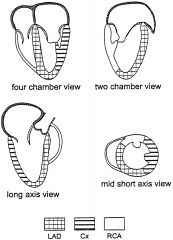
Draw the 4 views in a TOE.
4 chamber view 2 chamber view Long Axis View Mid Short Axis View Indicate the territories of the LAD, Cx and RCA |
|
|
|
|
What are the indication for PPM?
|
Two major indications :
1. Failure of impulse formation 2. Failure of cardiac conduction The following are common indications -SA node : sick sinus syndrome, tachy-brady syndrome, symptomatic sinus bradycardia, hypersensitive carotid sinus syndrome -AV node : 2nd and 3rd degree AV block -Trifasicular block -RBBB with left anterior hemiblock -RBBB with left posterior hemiblock -Alternating LBBB and RBBB -High risk patients with congenital long QT -cardiomyopathy : HOCM or dilated CM despite optimal medical therapy (biventricular pacing) Sick Sinus Syndrome is most common cause |
|
|
|
What is sick sinus syndrome?
|
An array of clinical disorders resulting from irreversible sinus node dysfunction.
Inadequate sinus node automaticity results in : -sinus arrest -sinus pause -sinus bradycardia -ectoptic tachyarhythmias |
|
|
|
MC65 ANZCA version [2002-Mar] Q53, [2002-Aug] Q63, [2004-Apr] Q59, [2004-Aug] Q84, [2005-Sep] Q58, [Mar06] Q38, [Jul07] (Similar reported question in [Apr96] [Apr97] [Jul97])
Characteristic cardio-pulmonary effects of pulmonary thrombo-embolism include A. hypoxaemia due to excess perfusion of lung units with a low V/Q ratio B. hypercarbia due to an increase in physiological dead-space C. reverse splitting of the second heart sound D. an increase in compliance of the left ventricle E. an increase in coronary blood flow to the right ventricle during systole |
ANSWER A
A. TRUE : Impaired gas exchange due to PE cannot be explained solely on the basis of mechanical obstruction of the vascular bed and alterations in the ventilation to perfusion ratio. Gas exchange abnormalities are also related to the release of inflammatory mediators, resulting in surfactant dysfunction, atelectasis, and functional intrapulmonary shunting B. FALSE : Arterial blood gases usually reveal acute respiratory alkalosis due to hyperventilation. The arterial PO2 and the alveolar-arterial oxygen difference (A–a–DO2) are usually abnormal in patients with PE compared with healthy, age-matched controls. However, arterial blood gases are not diagnostic: among patients who were evaluated in the PIOPED I study, neither the PO2 nor the A–a–DO2 differentiated between those with and those without pulmonary emboli. Profound hypoxia with a normal chest radiograph in the absence of preexisting lung disease is highly suspicious for PE. C. FALSE : P2 before A2 in delayed LV ejection eg severe AS or coarctation or ↑ LV load eg large PDA. P2 is LOUD in pulm hypertension and is not typically described as being earlier (enough to reverse the splitting). D. FALSE : ↑ PVR → ↑ RV size → deviates septum → ↓ LV compliance (TeOh p281) E. FALSE : TeOH p351 - acute pulmonary hypertension increases right ventricular afterload and wall tension, with coronary ischaemia PE physiology (Nunn p551) * ↑ PVR 1. Physical occlusion 2. Platelet activation in thrombus → 5HT and TXA2 release → vasoconstriction → ↑ PVR * Respiratory lesion o ↑ alveolar deadspace o ↑ A-a gradient + Normal to low PaCO2 (in SV) because ↑ RR ? due to J-receptor stimulation + hypoxia * ↓ PaO2 o Deranged V/Q relationships o ↓ CO → low mixed venous O2 * Bronchospasm due to 5HT release from platelets * ↓ pulmonary compliance (still unknown mechanism) |
|
|
|
MC134 ANZCA Version [Mar06] Q135
Correct statements regarding Hypertrophic Cardiomyopathy include each of the following EXCEPT that it A. results in a left ventricular wall thickness of greater than 12 mm B. is a condition where the left ventricle is hypertrophied and dilated C. is predominantly a non-obstructive disease D. is most easily and reliably diagnosed with 2-dimensional echocardiography E. the hypertrophy is characteristically asymmetrical |
ANSWER B
A: True. usually >15mm (12mm or less is considered normal) B: False. hypertrophic yes, dilated no C: True. "75%" have no outflow obstruction D: This is an excellent way to diagnose. E: True. Asymmetric septal hypertrophy. |
|
|
|
MC148 ANZCA Version [Mar06] Q46
The most useful finding to confirm the diagnosis of aortic stenosis in an adult with a systolic murmur is: A. increasing murmur intensity with inspiration B. decreasing murmur intensity with passive leg elevation C. increased second heart sound D. effort syncope E. a slow rate of rise of the carotid pulse |
ANSWER D
A. FALSE : RILE, louder with expiration B. FALSE : with most murmurs passive leg raising causes them to get louder (except HOCM and MVP) C. FALSE : A soft or absent A2 or reversed splitting of S2 may denote severe AS D. TRUE : this is a cardinal symptoms of AS E. TRUE : A slow-rising, diminished arterial pulse suggests severe AS in a patient with a grade 2/6 midsystolic murmur at the upper intercostal spaces, however has a poor sensitivity. |
|
|
|
MC146 ANZCA version [2005-Sep] Q113, [Apr07]
In the diagnosis of postoperative myocardial infarction A. echocardiography has little role to play B. infarct size can be judged from cumulative enzyme release C. new left bundle branch block on ECG confirms acute infarction D. serum troponins have high sensitivity and are detectable for up to 5 days E. ST segment elevation is extremely common |
ANSWER D
|
|
|
|
AC146 [Mar06]
A 35-year-old woman with a history of palpitations has the following ECG at rest: * 1st ECG pre-op with possible delta wave and big R wave in V1 She pressents for laparoscopic appendicectomy for suspected acute appendicitis. Prior to induction she feels faint and you feel a very rapid irregular brachial pulse. A portion of her 12 lead ECG now is shown below * 2nd ECG 12 lead at time of event HR>240 bpm ?irreg AF/SVT/VT wide-complex VT Your treatment of this arrhythmia should be A. carotid sinus massage B. DC cardioversion C. IV lignocaine D. IV verapamil E. IV adenosine |
ANSWER B
Haemodynamically unstable : SHOCK * orthodromic AVRT (narrow QRS)- want to block conduction thru AV node. -Try vagal manouvre -then adenosine -then verapamil * antidromic AVRT (wide QRS) - want to block conduction thru accessory pathway. -procainamide 10mg/kg -blocking AV conduction (ie vagal/adenosine) not effective -verapamil contraindicated as won't stop the AVRT but has v/d effect so may worsen haemodynamics. * AF - again want to block conduction via accessory pathway. -procainamide -verapamil &digoxin contraindicated as they block AV node and may cause preferential conduction down accessory pathway, causing faster ventricular rate |
|
|
|
MC101 ANZCA version [2001-Apr] Q128, [2001-Aug] Q104
Atrial fibrillation 1. of less than 24 hours duration will usually revert to sinus rhythm spontaneously 2. is contributed to by alcohol excess, pericarditis and chronic lung disease 3. of long duration has lower success rates for both pharmacological and electrical conversion 4. has a risk of atrial thrombus and embolic stoke which decreases with time |
ANSWER 1, 2, 3
Atrial Fibrillation 1. Incidence of AF doubles each decade 2. It is an independant RF for death, most commonly due to heart failure 3. Spontaneous conversion to SR within 24 hours in 2/3 of patients -likelihood decreases after 24 hours -after one week, spontaneous reversion is rare Risk factors -age -valvular heart disease -CCF -hypertension -diabetes -LVH -IHD -COPD -alcohol **'lone AF in 30% of cases |
|
|
|
MC102 ANZCA version [2001-Apr] Q143
A permanent pacemaker is indicated in the asymptomatic patient with 1. complete heart block following acute inferior myocardial infarction 2. sick sinus syndrome 3. Wenckebach atrioventricular block 4. Mobitz Type II atrioventricular block |
ANSWER 1, 2, 3, 4
Class 1 - (most persuasive) 1. . Asystole. 2. . Symptomatic bradycardia (includes sinus bradycardia with hypotension and type I second-degree AV block with hypotension not responsive to atropine). 3. . Bilateral BBB (alternating BBB or RBBB with alternating LAFB/LPFB) (any age). 4. . New or indeterminate age bifascicular block (RBBB with LAFB or LPFB, or LBBB) with first-degree AV block. 5. . Mobitz type II second-degree AV block. Class 2a 1. . RBBB and LAFB or LPFB (new or indeterminate). 2. . RBBB with first-degree AV block. 3. . LBBB, new or indeterminate. 4. . Incessant VT, for atrial or ventricular overdrive pacing. 5. . Recurrent sinus pauses (greater than 3 seconds) not responsive to atropine. Class 2b 1. . Bifascicular block of indeterminate age. 2. . New or age-indeterminate isolated RBBB. Class 3 1. . First-degree heart block. 2. . Type I second-degree AV block with normal hemodynamics. 3. . Accelerated idioventricular rhythm. 4. . Bundle branch block or fascicular block known to exist before acute MI. |
|
|
|
ANZCA Version [Apr 08]
A 65 -year-old female patient with known chronic renal disease and a normal resting preoperative electrocardiogram (ECG) has undergone total hip replacement. Three days postoperatively she complains of chest pain and breathlessness. Her pulse rate is 110 min-1 and blood pressure 130/90 mmHg. The following ECG is recorded. The diagnosis is most likely to be: (RBBB, R wave in VI, S wave in I, Q wave in III, t wave inversion in III A. Atrial fibrillation B. hyperkalaemia C. myocardial infarction D. pericarditis E. pulmonary embolus |
ANSWER E
S1Q3T3 |
|
|
|
MC104 ANZCA Version [Apr 08]
It is MOST important to re-program a patient's implanted cardiac pacemaker prior to: A. electroconvulsive therapy (ECT) B. laser therapy to a laryngeal papilloma C. lithotripsy of a renal calculus D. magnetic resonance imaging of the thorax E. percutaneous transhepatic cholangiography |
ANSWER A, C, D
Although C is best, as you PPM is absolute contraindication for MRI. Situations Probably Requiring Pacemaker Reprogramming *Any rate-responsive device *Special pacing indication (hypertrophic obstructive cardiomyopathy, dilated cardiomyopathy, pediatric patients) *Pacemaker-dependent patients *Major procedure in the chest or abdomen *Rate enhancements present that should be disabled *Lithotripsy *Transurethral resection *Hysteroscopy *Electroconvulsive therapy *Succinylcholine use *Magnetic resonance imaging (generally contraindicated by device manufacturers) In some situations and for certain patients, a pacemaker should be reprogrammed either to avoid potential patient injury or to prevent a pacemaker rhythm that could be confused with pacemaker malfunction. |
|
|
|
MC106a ANZCA version [2001-Apr] Q132
A patient with pulmonary hypertension secondary to lung disease presents for laparotomy. To avoid exacerbating pulmonary hypertension, the anaesthetist could employ 1. total intravenous anaesthesia 2. ketamine as the primary anaesthetic agent 3. volatile anaesthetic agents 4. N2O as an adjunct to volatile anaesthetic agents |
ANSWER 1 and 2
* Hypercapnoea is bad for pulmonary hypertension * Ketamine is bad for PHT * N2O is bad for PHT * TIVA is acceptable * Volatiles are also acceptable |
|
|
|
MC106c ANZCA version [2002-Mar] Q66, [2002-Aug] Q22, [2004-Aug] Q19
A patient with pulmonary hypertension secondary to lung disease presents for laparotomy. The anaesthetic technique LEAST likely to exacerbate the pulmonary hypertension is endotracheal intubation and A. controlled ventilation with isoflurane, N2O and O2 B. spontaneous breathing with isoflurane and O2 / air C. controlled ventilation with total intravenous anaesthesia and O2 / air D. controlled ventilation with ketamine and O2 / air E. controlled ventilation with high dose opioids, N2O and O2 |
ANSWER C
A. FALSE : addition of N2O increases PVR and RAP B. FALSE : aim to prevent hypoxia and hypercarbia, spontaneous ventilation will not achieve this C. TRUE : TIVA is acceptable, controlled ventilation is important D. FALSE : ketamine increases PVR especially in spontaneous ventilation E. FALSE |
|
|
|
MC106d ANZCA version [2004-Apr] Q109
A patient with pulmonary hypertension secondary to lung disease presents for laparotomy. The anaesthetic technique LEAST likely to exacerbate the pulmonary hypertension is endotracheal intubation and controlled ventilation with A. high dose opioids, N2O and O2 B. isoflurane and O2 / air C. isoflurane, N2O and O2 D. ketamine and O2 / air E. propofol and O2 / air |
ANSWER B and E
MEDICAL MANAGEMENT of PPHN 1) Minimize Pulmonary Hypertension/Vasoconstriction AVOID: HYPOXIA, HYPOTHERMIA, ACIDOSIS, ANEMIA, HYPOTENSION AND STIMULATION ! 2) Maximize Pulmonary Vasodilatation (Decrease pulmonary vascular resistance) a) OXYGEN (FiO2 = 1.0) b) ALKALINIZATION - METABOLIC ALKALOSIS (pH > 7.55) 3) Support Cardiac Output and Blood Pressure a) VOLUME b) INOTROPIC AGENTS: Dobutamine, Dopamine and Epinephrine 4) Relieve Pain and Anxiety a) ANALGESIA: Morphine or Fentanyl b) SEDATION: Lorazepam, Chloral Hydrate, Phenobarbital, Midazolam and Thorazine c) PARALYSIS: Pavulon 5) Administer Pulmonary Vasodilating Agents a) "INHALED NITRIC OXIDE" b) TOLAZOLINE c) PROSTAGLANDIN E1 d) ISOPROTERENOL 6) Avoid Barotrauma a) Small tidal volumes with high rates (i.e., HFOV) b) Avoid hyperventilation (pCO2 ² 30) to minimize barotrauma |
|
|
|
MC106e ANZCA version [2005-May] Q55
A patient with pulmonary hypertension secondary to lung disease presents for laparotomy. Regarding this patient's anaesthetic management: A. an alpha-agonist is the inotrope of choice B. hypothermia is protective against rises in pulmonary artery pressure C. isoflurane will tend to decrease pulmonary artery pressure D. ketamine is an appropriate anaesthetic agent E. right heart failure is not a concern |
ANSWER C?
|
|
|
|
MC107 ANZCA version [2001-Aug] Q71
A permanent dual-chamber transvenous pacemaker set to a DDDR mode will A. NOT be affected by diathermy B. increase the ventricular pacing rate if the minute volume is increased C. usually require reprogramming to VVO mode for surgery D. revert to DDD mode if a magnet is placed over the generator site E. result in a tachyarrhyrthmia if the patient develops atrial flutter |
ANSWER B
A. FALSE : XXDX will both sense and therefore trigger or inhibit based on the detected rhythm. Only in VOO or DOO (asynchronous pacing) B. TRUE : XXXR Rate Responsive Pacemakers -detect increases in metabolic rate by movement via piezoelectric crystals, minute ventilation via thoracic impedance, QT interval and stroke volume C. FALSE : depends if the patient is pacemakers dependent -yes? then set to VOO -no? leave it alone or disable but put on pacing pads -if the patient has an underlying rhythm, there is a risk of R on T. D. FALSE : PPM revert to VOO or DOO, AICD turns off shock function E. FALSE : This is a dual chamber pacing and sensing pacemaker. Whilst the atrial pacing may increase, the ventricular pacing will still function. Hence a tachyarrhythmia is only possible if all atrial impulses are conducted normally. Often this is not the case as the AV node aids to slow down conduction. |
|
|
|
MC110 ANZCA version [2002-Mar] Q78, [2004-Apr] Q27, [2004-Aug] Q3 | Aug10
Left bundle branch block (LBBB) on the ECG is A. commonly a normal variant B. associated with a delay in atrio-ventricular conduction C. demonstrated by a notched R wave in chest lead V1 D. associated with right axis deviation E. a relative contra-indication to flotation of a pulmonary artery catheter |
ANSWER E
A False - due to IHD or LVH (RBBB can be normal variant) B ?False - bundle branch blocks are after the AV node C False - LBBB has notched R in I,III,VL,VF,V5 (Hampton ECG in Practice p272) D False - but RBBB associated with right axis deviation E True - 5% of IHD patients get RBBB on PAC insertion ∴ relative contraindication |
|
|
|
MC112 ANZCA version [2002-Aug] Q120
In patients undergoing vascular surgery, myocardial ischaemia is most likely to occur A. in the pre-operative period B. during induction of anaesthesia C. intra-operatively, prior to revascularisation D. in the first 48 hours post-operatively E. 48 to 72 hours post-operatively |
ANSWER D
2/3 of myocardial ishcemia begins in the first 24 hours post operatively. |
|
|
|
MC113 ANZCA version [2002-Aug] Q85, [2003-Apr] Q79
When assessing a patient with unstable angina, the clinical feature most predictive of an adverse short-term outcome (death or myocardial infarction within 6 months) is A. increased angina frequency or severity B. angina provoked at a lower threshold of exercise C. new onset angina on effort D. an angina episode lasting more than 10 minutes E. age less than 65 years |
ANSWER A
Coronary syndrome I no Sx with ordinary activity II slight limitation of ordinary activity III marked limitation of ordinary activity IV inabilty to carry on any physical activity without discomfort- anginal symptoms may be present at rest. high risk of death/ MI are History -acceleration tempo of ischaemic symptoms in preceding 24 hours Character of pain -prolonged ongoing rest pain (>20 mins) Clinical findings -Pulm Oedema most likely due to ischaemia -New or worsening MR murmur -Hypotension, bradycardia or tachycardia -Age > 75 years -ECG Angina at rest with transient ST changes > 0.05mV, -New or presumed new BBB -Sustained VT Cardiac markers -elevated TnT or TnI >0.1 ng/ml |
|
|
|
MC115 ANZCA version [2001-Aug] Q88
With respect to acute myocardial infarction A. true posterior infarcts manifest on the ECG as a tall R wave in Lead V3 B. aspirin should NOT be given unless myocardial infarction is confirmed C. regional anaesthesia is NOT recommended if thrombolytic therapy has been used within the previous 2 weeks D. Angiotensin Converting Enzyme (ACE) inhibitors may be indicated in the acute period E. Troponin I testing is unsuitable in the perioperative period |
ANSWER D
A. FALSE : Dominant R in V1 B. FALSE : AHA/ACC guidelines suggest aspirin within 10 minutes of acute chest pain C. ??? ASRA guidelines : Patients who have received fibrinolytic and thrombolytic drugs "should be cautioned against receiving spinal or epidural anesthetics except in highly unusual circumstances. Data are not available to clearly outline the length of time neuraxial puncture should be avoided after discontinuation of these drugs. But regional anaesthesia does not necessarily include neuroaxial blockade D. TRUE : ACC suggest all AMI's if no hypotension. "Start ACE inhibitor orally in patients with anterior infarction, pulmonary congestion, or LVEF less than 0.40 if the following are absent: hypotension (SBP less than 100 mm Hg or less than 30 mm Hg below baseline) or known contraindications to this class of medications." E. FALSE |
|
|
|
MC117 ANZCA version [2003-Aug] Q118, [2004-Apr] Q78, [Mar06]
The medical therapy for unstable angina which is most effective in reducing progression to myocardial infarction is A. aspirin B. beta-blockers C. calcium channel blockers D. glyceral trinitrate E. thrombolytic therapy |
ANSWER A
See ACC/AHA guidelines .The recommendations of medical therapy ('to prevent death and MI') include: Class 1. (level of evidence) * Aspirin (A) * Clopidogrel if ASA not tolerated (A) * ASA and clopidogrel for 9 months post UA/STEMI (B) * Beta-blockers if not contraindicated (B) * Lipid lowering agents (A or B depending on patient) * ACEI for pts with CCF, LV dysfunction (EF <0.4), HTN or DM (A). |
|
|
|
MC121 ANZCA version [2004-Apr] Q96, [2004-Aug] Q91
Correct statements regarding atrial fibrillation include all of the following EXCEPT A. A history of hypertension, associated with atrial fibrillation, increases stroke risk. B. A history of poor left ventricular systolic function, associated with atrial fibrillation, increases stroke risk. C. Anticoagulation should be continued for one month following successful cardioversion of atrial fibrillation. D. Anticoagulation therapy (to an INR of 2.0) decreases the risk of stroke by up to 50%. E. Atrial fibrillation becomes an increasingly important cause of stroke with advancing age. |
ANSWER D
A. TRUE : CHADSII B. TRUE : CHADSII C. TRUE : The first is to anticoagulate for at least 3 weeks before and 4–6 weeks after elective cardioversion. The second strategy obviates the need for prior anticoagulation, and involves a pre-procedure transoesophageal echo (TOE) to exclude the presence of LA/LAA thrombus. After cardioversion, patients must be anticoagulated with heparin or enoxaparin followed by warfarin or enoxaparin as above (IIa/B). D. FALSE : therapeutic range is 2.0-3.0 E. TRUE : increasing ages increases the annual risk of stroke from 1.5% at 50yo to 23% at 80yo. |
|
|
|
MC123 ANZCA version [2004-Aug] Q117
The first heart sound on auscultation is A. characteristically quiet in mitral stenosis B. due equally to mitral and tricuspid valve closure C. louder than usual with a premature beat D. loudest at the left sternal edge E. unchanged in mitral regurgitation |
ANSWER C
A - false Loud S1 in MS because ↓ valve orifice → impaired LV filling ∴ mitral valve wide open when systole starts → valve snaps shut loudly B - false - with the higher L-sided pressures the mitral valve closure contributes more to S1, than does tricuspid closure C - true - akin to MS, the early arrival of ventricular contraction before ventricular filling tapers off means the valve is widely open and will make a louder sound upon closure with the VEB D - false - fitting w the MV contributing more to the S1, the ideal place to auscultate is the apex (MCL, 5th ICS) E - false - soft or absent |
|
|
|
MC125a ANZCA version [2002-Apr] Q86
In a patient with aortic stenosis, A. aortic regurgitation is rarely seen B. the characteristic compensation of the left ventricle is dilatation C. presentation is usually with a cerebrovascular accident D. a valve area of < 0.8 cm2 represents severe disease E. atrial arrhythmias are commonly seen |
ANSWER D
Maintenance of sinus rhythm and adequate intravascular volume is vital to ensure ventricular filling. Arrhythmias must be treated promptly. New onset atrial fibrillation may require cardioversion Degenerative calcific aortic stenosis - This is now the most common form of aortic stenosis in the UK and tends to occur over the age of 70 yr. Mechanical stress over time leads to progressive fibrosis and calcification of a previously normal tri-leaflet valve Anaesthetic techniques that reduce systemic vascular resistance (e.g. regional neuroaxial techniques) must be used with extreme caution although successful cases of carefully titrated epidural and spinal blocks using catheters have been reported |
|
|
|
MC125b ANZCA version [2004-Apr] Q116, [2004-Aug] Q27 [note different options]
In a patient with aortic stenosis, A. aortic regurgitation is rarely seen B. loss of sinus rhythm is poorly tolerated C. presentation is usually with a cerebrovascular accident D. the characteristic compensation of the left ventricle is dilatation E. the most common aetiology is rheumatic calcification |
ANSWER B
Maintenance of sinus rhythm and adequate intravascular volume is vital to ensure ventricular filling. Arrhythmias must be treated promptly. New onset atrial fibrillation may require cardioversion Degenerative calcific aortic stenosis - This is now the most common form of aortic stenosis in the UK and tends to occur over the age of 70 yr. Mechanical stress over time leads to progressive fibrosis and calcification of a previously normal tri-leaflet valve Anaesthetic techniques that reduce systemic vascular resistance (e.g. regional neuroaxial techniques) must be used with extreme caution although successful cases of carefully titrated epidural and spinal blocks using catheters have been reported |
|
|
|
MC126 ANZCA version [2002-Mar] Q135 [2010- August] Q66
Left ventricular diastolic dysfunction 1. can be diagnosed with transoesophageal echocardiography. 2. is improved by propofol anaesthesia. 3. is suggested by an early to late (atrial) mitral inflow velocity ratio (E/A) of less than one 4. following an old myocardial infarction is mainly due to delayed ventricular relaxation |
ANSWER 1 and 3
Diastolic dysfunction -very common -2 components a. poor relaxation b. decreased compliance Diagnsosis 1. Clinical features of heart failure 2. Normal EF >50% 3. Increased left diastolic filling pressure (this is invasive, therefore non-invasive surrogates are used) a. Isovolumic Relaxation Time : time from AV closure to MV opening -IRT >110ms (60-80ms is normal) b. Transmitral inflow : E/A ratio -E is the early and A (atrial) is late ventricular filling velocity -E wave related to LV 'suction' and LA pressure -E wave acceleration will be higher with high LA pressure; and lowered with impaired relaxation -as DD progresses, the atrial component becomes more important in maintaining preload c. Pulmonary Venous Inflow : TOE Categorising DD i. Mild dysfunction (E/A <1, IRT>100ms, normal E wave deceleration, atrial reversal of pulmonary venous inflow ii. Mild-Mod (same E/A and ITR but atrial reversal >35ms) iii. Moderate ('pseudonormalization' with normal E/A iv. Severe ('restrictive' large E small A, short IRT, reduced pukmonary systolic wave) Management The following agents may be of value: * calcium channel blockers (but beware of some with associated ischaemic heart disease) * beta blockers * ACE inhibitors and AT-II receptor antagonists. |
|
|
|
MC127 ANZCA version [2002-Mar] Q147
A 28 yr old patient with hypertrophic obstructive cardiomyopathy (HOCM) presents for an emergency laparotomy for suspected ectopic pregnancy. In anaesthetising this patient it is important to 1. maintain a pulse rate of at least 100 beats.min-1 2. increase cardiac contractility 3. reduce preload 4. maintain sinus rhythm. |
ANSWER 4
Haemodynamics with HOCM Hypertrophic obstructive cardiomyopathy is a dynamic condition, which is associated with the following: * Hypertrophy in an asymmetrical manner, with the septum and aortic outflow tract being hypertrophied to a greater extent than the rest of the LV * Dynamic motion of the hypertrophied portion of the heart leading to a function outflow resistance * Systolic anterior motion of the mitral valve, leading to a functional mitral regurgitation due to the Bernoulli effect on the mitral valve. Haemodynamic aims with HOCM * Slow heart rate * Normal to mildly reduced contractility * Sinus rhythm * Maintain afterload to ensure good coronary perfusion pressure * Full preload |
|
|
|
MC128 ANZCA version [2005-Apr] Q145, [Jul06] Q25
The normal range of the QRS axis in the ECG is A. 0 to +180 degrees B. 0 to +90 degrees C. -30 to +90 degrees D. -90 to +90 degrees E. -90 to +30 degrees |
ANSWER C
|
|
|
|
MC125a ANZCA version [2002-Apr] Q86
In a patient with aortic stenosis, A. aortic regurgitation is rarely seen B. the characteristic compensation of the left ventricle is dilatation C. presentation is usually with a cerebrovascular accident D. a valve area of < 0.8 cm2 represents severe disease E. atrial arrhythmias are commonly seen |
ANSWER D
Maintenance of sinus rhythm and adequate intravascular volume is vital to ensure ventricular filling. Arrhythmias must be treated promptly. New onset atrial fibrillation may require cardioversion Degenerative calcific aortic stenosis - This is now the most common form of aortic stenosis in the UK and tends to occur over the age of 70 yr. Mechanical stress over time leads to progressive fibrosis and calcification of a previously normal tri-leaflet valve Anaesthetic techniques that reduce systemic vascular resistance (e.g. regional neuroaxial techniques) must be used with extreme caution although successful cases of carefully titrated epidural and spinal blocks using catheters have been reported |
|
|
|
MC125b ANZCA version [2004-Apr] Q116, [2004-Aug] Q27 [note different options]
In a patient with aortic stenosis, A. aortic regurgitation is rarely seen B. loss of sinus rhythm is poorly tolerated C. presentation is usually with a cerebrovascular accident D. the characteristic compensation of the left ventricle is dilatation E. the most common aetiology is rheumatic calcification |
ANSWER B
Maintenance of sinus rhythm and adequate intravascular volume is vital to ensure ventricular filling. Arrhythmias must be treated promptly. New onset atrial fibrillation may require cardioversion Degenerative calcific aortic stenosis - This is now the most common form of aortic stenosis in the UK and tends to occur over the age of 70 yr. Mechanical stress over time leads to progressive fibrosis and calcification of a previously normal tri-leaflet valve Anaesthetic techniques that reduce systemic vascular resistance (e.g. regional neuroaxial techniques) must be used with extreme caution although successful cases of carefully titrated epidural and spinal blocks using catheters have been reported |
|
|
|
MC126 ANZCA version [2002-Mar] Q135 [2010- August] Q66
Left ventricular diastolic dysfunction 1. can be diagnosed with transoesophageal echocardiography. 2. is improved by propofol anaesthesia. 3. is suggested by an early to late (atrial) mitral inflow velocity ratio (E/A) of less than one 4. following an old myocardial infarction is mainly due to delayed ventricular relaxation |
ANSWER 1 and 3
Diastolic dysfunction -very common -2 components a. poor relaxation b. decreased compliance Diagnsosis 1. Clinical features of heart failure 2. Normal EF >50% 3. Increased left diastolic filling pressure (this is invasive, therefore non-invasive surrogates are used) a. Isovolumic Relaxation Time : time from AV closure to MV opening -IRT >110ms (60-80ms is normal) b. Transmitral inflow : E/A ratio -E is the early and A (atrial) is late ventricular filling velocity -E wave related to LV 'suction' and LA pressure -E wave acceleration will be higher with high LA pressure; and lowered with impaired relaxation -as DD progresses, the atrial component becomes more important in maintaining preload c. Pulmonary Venous Inflow : TOE Categorising DD i. Mild dysfunction (E/A <1, IRT>100ms, normal E wave deceleration, atrial reversal of pulmonary venous inflow ii. Mild-Mod (same E/A and ITR but atrial reversal >35ms) iii. Moderate ('pseudonormalization' with normal E/A iv. Severe ('restrictive' large E small A, short IRT, reduced pukmonary systolic wave) Management The following agents may be of value: * calcium channel blockers (but beware of some with associated ischaemic heart disease) * beta blockers * ACE inhibitors and AT-II receptor antagonists. |
|
|
|
MC127 ANZCA version [2002-Mar] Q147
A 28 yr old patient with hypertrophic obstructive cardiomyopathy (HOCM) presents for an emergency laparotomy for suspected ectopic pregnancy. In anaesthetising this patient it is important to 1. maintain a pulse rate of at least 100 beats.min-1 2. increase cardiac contractility 3. reduce preload 4. maintain sinus rhythm. |
ANSWER 4
Haemodynamics with HOCM Hypertrophic obstructive cardiomyopathy is a dynamic condition, which is associated with the following: * Hypertrophy in an asymmetrical manner, with the septum and aortic outflow tract being hypertrophied to a greater extent than the rest of the LV * Dynamic motion of the hypertrophied portion of the heart leading to a function outflow resistance * Systolic anterior motion of the mitral valve, leading to a functional mitral regurgitation due to the Bernoulli effect on the mitral valve. Haemodynamic aims with HOCM * Slow heart rate * Normal to mildly reduced contractility * Sinus rhythm * Maintain afterload to ensure good coronary perfusion pressure * Full preload |
|
|
|
MC128 ANZCA version [2005-Apr] Q145, [Jul06] Q25
The normal range of the QRS axis in the ECG is A. 0 to +180 degrees B. 0 to +90 degrees C. -30 to +90 degrees D. -90 to +90 degrees E. -90 to +30 degrees |
ANSWER C
|
|
|
|
MC129 ANZCA version [2005-Apr] Q149
In providing general anaesthesia for patients with congenital Long QT syndromes, which of the following statements is correct? A. a priming dose of a non-depolarising muscle relaxant protects against succinylcholine induced arrhythmias B. beta-blocking drugs are relatively contra-indicated C. low dose droperidol is safe D. pre-induction infusion of magnesium sulphate should NOT be used E. thiopentone leaves the QT interval unchanged |
ANSWER A
* A. a priming dose of a non-depolarising muscle relaxant protects against succinylcholine induced arrhythmias - true: o "The ideal muscle relaxant should avoid bradycardia, vagal stimulation, and potassium shifts. It should have little or no histamine release and be short acting to avoid the use of reversal agents. Accordingly, succinylcholine, because of its autonomic effects and potassium release, is far from ideal. It prolongs the QT interval in patients with c-LQTS unless pretreatment with a priming dose of tubocurarine is used." (Anesthesiology. 2005 Jan;102(1):204-10.) * B. beta-blocking drugs are relatively contra-indicated - false: o "The mainstay of treatment of congenital LQTS since 1975 has been ß-block. Schwarz reported a decrease in mortality from 71% in untreated historical controls to 6% in those treated" (Br J Anaesth 2003; 90: 349–66) * C. low dose droperidol is safe - probably false: o "Although the data that led to the 2001 black box warning resulted from case reports and surveillance data rather than scientific publications in medical journals, it seems prudent to avoid using droperidol in the perioperative setting in patients with c-LQTS." (Anesthesiology. 2005 Jan;102(1):204-10.) * D. pre-induction infusion of magnesium sulphate should NOT be used - false: o "Magnesium sulfate is the treatment of choice for prevention of recurrence in patients with drug-induced TdP even with normal magnesium concentrations." (Anesthesiology. 2005 Jan;102(1):204-10.) o "It has been suggested that pretreatment with magnesium (30 mg/kg) may be beneficial, even in patients with normal serum magnesium concentration. Magnesium is very unlikely to cause toxicity, and may block the inward sodium and potassium currents implicated in generating early after-depolarizations" (Anesthesiology. 2005 Jan;102(1):204-10.) * E. thiopentone leaves the QT interval unchanged - false o "Thiopental prolongs the QT interval in healthy patients. 45 Despite this effect, thiopental has been used safely in patients with c-LQTS" (Anesthesiology. 2005 Jan;102(1):204-10.) Long QT syndrome -congential disorder characterized prolongation of QT invertal on ECG -Propensity to ventricular tachyarrythmias which may leave to syncope, cardiac arrest and sudden death 30% of patients present with unexplained syncope or aborted sudden death -60% are symptomatic at time of diagnosis. -prevalence may be as high as 1 per 1100-3000. Diagnosis -QTc >440ms -QTc = QT/ sq root of RR interval Management -Beta blockade -anti-bradycardia pacing -implantation of cardioverter defibrillators -left cardiac sympathetic denervation are used in the treatment of these patients. -However, these treatment modalities do not guarantee the prevention of sudden cardiac death. Anaesthesia management Anaesthesia in patients carries a very high risk of malignant ventricular arrythmias, however despite beta blockade patients remain at risk. Patients should be on maintenance beta blocker therapy and this much be continued throughout the perioperative period, including IV replacement if enteral intake is not possible. Electrolytes must be normal (especially K+, Mg++ and Ca++) Intraoperative management should focus on prevention of excessive sympathetic activity and avoidance of factors that can prolong the QT interval. * Have pacing apparatus, defibrillator and drugs available. * Consider induction and maintenance with propofol (which may shorten the QTc interval) * Response to intubation must be adequately blunted * Avoid high intra-thoracic pressures and PEEP which simulates a Valsalva and can prolong the QT. * Extubate deep * Avoid reversal (see below) * Manage Torsades de pointes Drugs which prolong QTc Note that not all of these have been associated with Torsades de pointes. * Volatile anaesthetic agents all prolong the QT interval * Thiopentone * Atropine, Glycopyrrolate * Class Ia antiarrythmics (Disopyramide, Quinidine, Procainamide) * Class Ic antiarrythmics * Class III antiarrythmics * Butyrophenones (Droperidol, haloperidol) * Phennothiazine and atypical anti-psychotics * SSRIs * Macrolide antibiotics * Cisapride |
|
|
|
MC130 [Apr05] Q139 ANZCA version
A patient with known ischaemic heart disease undergoes percutaneous coronary artery stenting (with a non drug-eluting stent) prior to major elective surgery. Ideally the surgery should be postponed for A. 1-4 weeks B. 4-8 weeks C. 8-12 weeks D. 12-24 weeks E. over 24 weeks |
ANSWER B
ACC/AHA guidelines [1] (http://www.americanheart.org/downloadable/heart/1013454973885perio_update.pdf) (see page 31) * case series show significant incidence of perioperative death and major bleed for patients who had surgery within 14 days of stent placement. * recommend waiting a minimum of 2 weeks, but 4 weeks is preferable. * waiting longer than 6 to 8 weeks puts you into the time period when restenosis [if it is to occur] will begin occuring. * pts are usually on antiplatelet rx for 4 weeks, so optimal time period seems to be 4-6 weeks, allowing time for stoppage of antiplatelet agent preop if surgeon desires [but ideally not stopping before the 4 week mark. |
|
|
|
MC131 ANZCA version [2005-Apr] Q141
The cardiac valvular lesion identified as the MOST significant risk factor for non-cardiac surgery is severe A. aortic incompetence B. aortic stenosis C. mitral incompetence D. mitral stenosis E. tricuspid incompetence |
ANSWER B
Consider that most general anaesthesia results in a decrease in cardiac contractility, which can be detrimental to cardiac output with severe AS. From ACC/AHA Guideline Update on Perioperative Cardiovascular Evaluation for Noncardiac Surgery [1] (http://www.acc.org/clinical/guidelines/perio/clean/perio_index.htm) "Severe aortic stenosis poses the greatest risk for noncardiac surgery. If the aortic stenosis is severe and symptomatic, elective noncardiac surgery should generally be postponed or canceled. Such patients require aortic valve replacement before elective but necessary noncardiac surgery. On the other hand, in patients with severe aortic stenosis who refuse cardiac surgery or are otherwise not candidates for aortic valve replacement, noncardiac surgery can be performed with a mortality risk of approximately 10%. In rare instances, percutaneous balloon aortic valvuloplasty may be justified when the patient is not a candidate for valve replacement." |
|
|
|
MC132 ANZCA version [2005-Apr] Q131
Ischaemic preconditioning limits myocardial damage during a subsequent ischaemic insult. This process is inhibited by A. alpha-2 agonists B. insulin C. isoflurane D. opioids E. sulfonylureas |
ANSWER E
* Cardiac preconditioning is thought to be due to action of ATP K+ channels. * These are typically blocked by sulphonylureas, hence these agents would negate preconditioning. * Therefore option E is correct. |
|
|
|
MC136 ANZCA version [2005-Sep] Q111
During controlled ventilation of a neonate prior to repair of a truncus arteriosus which of the following is MOST likely to be deleterious? A. controlled hypoventilation B. ventilation with air C. ventilation with an FiO2 of 0.18 D. ventilation with nitric oxide E. ventilation with PEEP of 3 cmH2O |
ANSWER D
Truncus arteriosis results from failure of division of pulmonary artery from the aorta -resulting in too much blood flow to the lungs Anaesthetic Management -involves maintaining a high PVR to reduce the gradient across the truncus -minimise further pulmonary shunting -PVR/SVR ratio 1. Minimise SVR -heart failure medication -mainly diuretics 2. Maximise PVR -hypoventilation -hypoxia -PEEP |
|
|
|
MC141 ANZCA Version [APR07]
Regarding atrial fibrillation A. aspirin is as effective as warfarin for the prevention of embolic stroke in elderly patients B. patients should not receive warfarin therapy unless they have risk factors for embolic stroke C. patients who are converted to sinus rhythm should be placed on rhythm maintenance therapy D. rhythm control has NOT been shown to be superior to rate control E. the best drug for rate control during exercise is digoxin |
ANSWER D
AFFIRM, PIAF, RACE, STAF : -this RCT have shown rate control is at least effective as rhythm control in improving symptoms and fucntional capacity |
|
|
|
MC142 ANZCA version [2004-Apr] Q138
The following statements regarding prolonged QT syndrome are true EXCEPT A. all patients with the syndrome have a prolonged QTc (QT interval corrected for heart rate) B. a QTc greater than 500 msec is considered prolonged C. exercise testing may provoke a prolongation of the QTc D. T and U wave abnormalities are common E. T wave alternans is pathognomonic of the syndrome |
ANSWER A
# A - False (therefore answer) --> "6% of patients with symptomatic LQTS have a normal QTc interval." # B - True --> "QTc interval of >440 ms is considered prolonged", therefore > 500 msec is definitely prolonged # C - True --> "Exercise testing of patients with LQTS may provoke prolongation of the QTc" # D - True --> "T wave and U wave abnormalities are common in LQTS" # E - True --> "A pathognomonic feature of LQTS is so-called T wave alternans, where there is beat-to-beat variation in T wave amplitude." |
|
|
|
MC144 ANZCA version [2004-Aug] Q114
Early features of pulmonary hypertension include each of the following EXCEPT A. a narrowly split second heart sound (S2) B. an early diastolic murmur C. decreased oxygen saturation D. dyspnoea on exertion E. hyperlucent lung periphery on chest Xray |
ANSWER B
A. TRUE : a narrowly split second heart sound (S2) B. FALSE :an early diastolic murmur - this is a late sign of PHT C. TRUE decreased oxygen saturation - d/t V/Q mismatch, R>L via PFO, and decr CO w decr PvO2 D.TRUE : dyspnoea on exertion - cardinal sign E. TRUE : hyperlucent lung periphery on chest Xray - classic finding thus true |
|
|
|
MC145 ANZCA version [2005-Sep] Q125
Each of the following are causes of right axis deviation on the ECG (electrocardiogram) EXCEPT A. chronic lung disease B. lateral myocardial infarction C. left anterior hemiblock D. left posterior hemiblock E. right ventricular hypertrophy |
ANSWER C
Conditions associated with right axis deviation * Right ventricular hypertrophy * Left posterior hemiblock * Lateral myocardial infarction * Acute right heart strain |
|
|
|
MC152 [Jul07]
60 y.o with acute aortic regurgitation. In pulmonary oedema. BP 160/90. HR was about 90. What is the best treatment pre-op: A. Intra aortic balloon pump B. Dobutamine infusion C. Sodium nitroprusside infusion D. Beta blocker E. Dopamine infusion |
ANSWER C
the systolic blood pressure remains above 100 mmHg with good mentation and renal function, intravenous sodium nitroprusside should be added. The initial dose is 0.25 to 0.5 microg/kg per minute. Nitroprusside should not be used without beta blockade since vasodilation alone induces reflex activation of the sympathetic nervous system leading to enhanced ventricular contraction and increased aortic shear stress. Aim should be to augment forward flow as a temporising treatment -patient needs a new AV |
|
|
|
MC153 [Jul07] ANZCA version
When viewing the central venous pressure trace: A. an accentuated "a" wave supports the diagnosis of atrial fibrillation B. a steeper than normal "x" descent supports the diagnosis of tricuspid regurgitation C. blunted "a" and "v" waves are associated with extensive right ventricular infarction D. flattened "x" and "y" descents are associated with pericardial constriction E. a monophasic pattern with obliteration of the "y" descent supports the diagnosis of pericardial tamponade |
ANSWER E
A - False * In atrial fibrillation, a waves will be absent, and in atrioventricular dissociation, a waves will be dramatically increased ("cannon waves") as the atrium contracts against a closed tricuspid valve. B - False * In tricuspid regurgitation, the c wave and x descent will be replaced by a large positive wave of regurgitation as the blood flows back into the right atrium during ventricular contraction C - False * Prom a and v waves with RV infarction due to (a wave) increased atrial pressure from contraction into stiff RV (kind of like increased RA afterload) and v waves increased as often assoc TR hence increased filling RA. D - False * Pericardial constriction – tall a and v waves, steep x and y descents E - True In cardiac tamponade, all pressure will be elevated, and the y descent will be nearly absent |
|
|
|
MC154 ANZCA version [Jul07] Q90
Clinical features supporting the diagnosis of cardiac tamponade include all of the following EXCEPT A. equal diastolic pressures of all heart chambers B. ST segment abnormalities C. increased venous pressure and cardiac output with fluid loading D. increased patient comfort in the sitting position E. impalpable apex beat and soft heart sounds |
ANSWER B
|
|
|
|
MC155 ANZCA version [Jul07] Q148
The LEAST desirable position for the tip of a central venous catheter which has been inserted into the left internal jugular vein is A. mid-way along the left brachiocephalic vein B. at the junction of the left brachiocephalic vein and the superior vena cava (SVC) C. in the SVC at the level of the carina D. at the junction of the SVC and the right atrium E. in the right atrium |
ANSWER B
Whenever the catheter negotiates a sharp bend, the catheter must be passed a reasonable distance beyond the bend such that the axes of the catheter and vein are aligned. In the case of insertion from the left side, this may be achievable only by siting the tip in the right atrium. 'The carina as a radiological landmark for central venous catheter tip position' P. A. Stonelake and A. R. Bodenham British Journal of Anaesthesia 2006 96(3):335-340 * Zone A represents the lower SVC and upper RA. In this zone CVCs placed from the left side are likely to lie parallel to the vessel walls. However, a part of this zone lies within the RA and therefore within the pericardial reflection. This may represent a necessary compromise for left-sided CVCs to ensure they lie parallel to the vessel wall. * Zone B represents the area around the junction of the left and right innominate veins and the upper SVC. This is a suitable area for CVCs placed from the right side, however left-sided CVCs will enter this area at a steep angle and are at risk of abutting the lateral wall of the SVC and should ideally be advanced into zone A. * Zone C represents the left innominate vein proximal to the SVC. CVCs in zone C are probably suitable for short-term fluid therapy and CVP monitoring, but not for inotrope infusions or long-term use. * A high proportion of left-sided lines above the carina had a steep (≥40°) angle to the vertical...These can be further divided into two groups: those lying within the left innominate vein proximal to the SVC (zone C) and those where the tip abuts the right internal wall of the SVC (zone B). The latter group has a higher chance of vessel wall perforation and associated morbidity. |
|
|
|
ANZCA Version [Jul07]
Regarding patients aged 65 years or older with recurrent atrial fibrillation (AF) A. amiodarone and digoxin have similar efficacy in restoring sinus rhythm B. patients who have been reverted to sinus rhythm should still remain on warfarin therapy C. patients who remain in atrial fibrillation with heart rates less than 80 beats per minute do NOT require long term warfarin therapy D. peri-operative therapy with a beta-blocker will commonly lead to restoration of sinus rhythm E. restoration of sinus rhythm with electrical DC cardioversion improves long-term survival in comparison to controlling heart rate alone |
ANSWER B
A. FALSE : digoxin is used for rate control not for cardioversion B. TRUE : must remain on warfarin for 3-6 months, unless a thrombus has been excluded by TOE C. FALSE D. FALSE E. FALSE |
|
|
|
MC157 [Mar10] [Aug10]
An 18 yo with Fontan circulation undergoing exploratory laparotomy. On ICU ventilation, saturation is 70%. Which ventilator parameter would you INCREASE to improve his saturation? A. Bilevel pressure B. Expiratory time C. Inspiratory time D. Peak inspiratory pressure E. PEEP |
ANSWER B
Fontan circulation Main determinants of success -SVR -PVR -AV valve function -sinus rhythm -ventricular function (preload, SVR, contractility) |
|
|
|
MC159 ANZCA Version [Apr 07]
The American Heart Association guidelines for pre-operative cardiac risk assessment define poor functional capacity as being only able to exercise at a level of less than 4 METS. An exercise capacity of 4 METS would correspond to: A. Light housework such as dishwashing B. heavy work around the house such as moving heavy objects C. jogging for 2 kms D. walking briskly on level ground (6kph) E. walking slowly on level ground (3kph) |
ANSWER A
|
|
|
|
MC160 ANZCA Version [Jul 2007]
The strongest indication for the use of transoesophageal echocardiography during major non-cardiac surgery is A. recent myocardial infarction (less than six weeks old) B. acute significant intra-operative ST segment depression on ECG C. massive intraoperative blood loss D. a history of severe valvular heart disease E. unexplained significant intraoperative hypotension |
ANSWER E
TOE here is indicated as it will assist diagnosis, e.g. PE, AMI, CCF, underfilling |
|
|
|
MC162 ANZCA version [Jul07] Q140
In acute coronary syndromes with ST elevation on ECG A. aspirin should be administered only after reperfusion strategies have commenced B. patients can wait up to 24 hours from onset of ischaemic symptoms before implementation of a reperfusion strategy C. patients should have elevated cardiac enzymes before proceeding to reperfusion strategies D. patients undergoing reperfusion strategies should have aspirin or clopidogrel but NOT both E. percutaneous coronary intervention is preferable to fibrinolytic therapy |
ANSWER E
|
|
|
|
AC90b ANZCA version [2001-Aug] Q17, [2002-Aug] Q83
In a patient undergoing a femoro-popliteal bypass, the most predictive independent risk factor for the development of post-operative myocardial infarction would be A. a previous history of coronary artery bypass grafts B. diabetes mellitus C. an episode of intra-operative myocardial ischaemia D. hypercholesterolaemia E. an episode of post-operative myocardial ischaemia lasting over 60 minutes |
ANSWER C
Most (>80%) Perioperative MIs occur early after surgery, are asymptomatic, of the non-Q-wave type (60–100%), and are most commonly preceded by ST-segment depression rather than ST-segment elevation |
|
|
|
AC90c ANZCA version [2003-Apr] Q98, [2003-Aug] Q14, [2005-Apr] Q7, [2005-Sep] Q22, [Mar06] [Mar10] [Aug10]
In a patient undergoing a femoro-popliteal bypass, the most predictive independent risk factor for the development of post-operative myocardial infarction would be A. an acute myocardial infarct 3 months ago B. an episode of intra-operative myocardial ischaemia C. an episode of post-operative myocardial ischaemia D. 50% blood volume blood loss intra-operatively E. poorly controlled diabetes mellitus |
ANSWER B
Most (>80%) Perioperative MIs occur early after surgery, are asymptomatic, of the non-Q-wave type (60–100%), and are most commonly preceded by ST-segment depression rather than ST-segment elevation |
|
|
|
AZ63 ANZCA version [2002-Aug] Q123, [Mar06] Q59 [Apr07] Q10
Regarding extracorporeal shockwave lithotripsy (ESWL) for renal calculi in patients with a permanent pacemaker in situ, A. ESWL is contraindicated B. ESWL pulses should be timed to coincide with the ST interval C. rate modulation of the pacemaker should be deactivated during the ESWL procedure D. there is a risk that the ESWL pulse will reprogramme the pacemaker E. regional anaesthesia is relatively contraindicated |
ANSWER C
Pacemakers relatively contraindicated * Dual chamber pacemakers o Reprogram to VVI o Turn rate response off * Continuous ECG monitoring * Keep lithotripter more than 15cm from pacemaker * Time shock wave with R wave Reprogramming a pacemaker to asynchronous pacing at a rate greater than the patient's underlying rate usually ensures that no over- or undersensing during EMI will take place, protecting the patient. Miller p1422 |
|
|
|
SC25 [Mar06] Q99 ANZCA Version
When anaesthetising a patient with a ventricular assist device (VAD) for noncardiac surgery A. anticoagulation should be temporarily discontinued during surgery B. electrocautery is well tolerated by these devices C. malignant arrhythmias should be treated with defibrillation if indicated D. the most important causes of decreased pump output are hypovolaemia and increased afterload E. volatile anaesthetic agents should be avoided. |
ANSWER D
A. FALSE : With the exception of the Heartmate, maintenance of therapeutic levels of anticoagulation is imperative for extracorporeal circulation through these devices (because of the risk of thromboembolism), and both the surgeon and anesthesiologist must be prepared for increased intraoperative bleeding...At no time should anticoagulation ever be fully reversed in a VAD-supported patient B. FALSE : Extracorporeal devices (the Abiomed and the Thoratec) and the well shielded Novacor will not be affected by defibrillation or the electrocautery. Unfortunately, the Heartmate is not well shielded and may be reset to a fixed-rate mode by the electrocautery and potentially damaged by external defibrillation. When feasible, the use of bipolar electrocautery is recommended. C. FALSE : patients on biventricular support will often remain hemodynamically stable in the face of otherwise malignant arrhythmias. Regardless, malignant ventricular arrhythmias should be terminated whenever possible. D. TRUE : The two most important factors leading to decreased pump output are hypovolemia and increased afterload E. |
|
|
|
SF73 ANZCA Version [Jul06] Q146, [Apr07] Q145
Drugs that may be used for the management of heart failure, secondary to dilated cardiomyopathy in pregnancy, include each of the following EXCEPT A. ACE (angiotensin-converting enzyme) inhibitor B. beta-blockers C. digoxin D. loop diuretics E. nitrates |
ANSWER A
A. TRUE : Category D B. FALSE : labetolol is routinely used metoprolol and esmolol is preferred as it is beta selective -reserved for later pregnancy -caused IUGR, bradycardias and hypoglycaemia C. FALSE : Cat A D. FALSE : Cat C E. FALSE : Cat B2 |
|
|
|
Black Bank April 2009
MC 60 year old vascular patient. ECG given. Showed large positive R waves in lateral leads, large negative S waves in anterior leads. ST depression laterally ie LVH with strain; bicuspid p waves A. LVH with strain B. Enlarged RA C. Lateral ischaemia D. LBBB E. L posterior hemiblock |
ANSWER A
|
|
|
|
Black Bank April 2009
Pulsus paradoxus is: A. Reduced BP on inspiration unlike normal (ie normally increased on insp) B. Reduced BP on inspiration exaggerated from normal C. Reduced BP on expiration unlike normal D. Reduced BP on expiration exaggerated from normal E. ? |
ANSWER B
|
|
|
|
Black Bank April 2009
What antibiotics are required for bacterial endocarditis prophylaxis in a woman with MV prolapse for cholecystectomy. A. None B. gentamicin C. ampicillin and gentamicin D. ampicillin E. cephazolin |
ANSWER A
|
|
|
|
Black Bank 2009
Male 60’s sudden onset of chest pain , L arm weakness and hoarse voice, ECG is unchanged from old (T inversion laterally), CXR normal, BP135/80, Pulse 110/min. Next step in management: A)Aspirin B)SNP infusion C)GTN infusion D)Metoprolol E)Heparin |
Stupid question : next step would be to diagnose
Sounds like aortic dissection therefore D |
|
|
|
TMP-130 [Aug09]
Essential diagnostic criteria on ECG for LBBB A. Loss of septal Q's in V5 and V6 B. RSR in V1 C. Large slurred S in V6 D. T-waves opposite to direction of QRS E. QRS duration minimum 0.2 s |
ANSWER A
* A TRUE * B FALSE o This represents RBBB * B FALSE o Also RBBB * D FALSE o An associated finding, not essential * E FALSE Diagnostic criteria for LBBB: * QRS duration of 120 ms * Dominant S wave in V1 * Broad monophasic R wave in lateral leads (I, aVL, V5-V6) * Absence of Q waves in lateral leads (I, V5-V6; small Q waves are still allowed in aVL) * Prolonged R wave peak time > 60ms in left precordial leads (V5-6) * About » o Authors o Affiliates o Awards o Archives o Analytics o Legal Disclaimer * Blog * Exams » o ACEM Primary o ACEM Fellowship o CICM Fellowship o Utopian College o ACTM Fellowship o Conference * Education » o Clinical Cases o Toxicology o History o Clinical Examination o Investigations [tests] o Procedures o Lecture Notes o Medicine 2.0 o Oslerisms * Resources » o Stuff We Read o Image DATABASE o Emergency Medicine Blogs o Podcasts o ANZ MedBloggers o International Emergency Medicine o Eponymous Fractures o Glossary of terms o Paediatrics o Medical Humour * ECG Library » o ECG Basics o ECG Clinical Cases o Cardiology Eponyms o A-Z by Diagnosis o ECG References o ECG Exam Template * Books » o On Call Principles o Emergency Medicine o Toxicology Handbook o Critical Care Drug Manual o EMA Journal o Reviews * November 1, 2011 LITFL » ECG Library » ECG Basics » Left Bundle Branch Block Left Bundle Branch Block LBBB@ 590x246 Left Bundle Branch Block Background * Normally the septum is activated from left to right, producing small Q waves in the lateral leads. * In LBBB, the normal direction of septal depolarisation is reversed (becomes right to left), as the impulse spreads first to the RV via the right bundle branch and then to the LV via the septum. * This sequence of activation extends the QRS duration to > 120 ms and eliminates the normal septal Q waves in the lateral leads. * The overall direction of depolarisation (from right to left) produces tall R waves in the lateral leads (I, V5-6) and deep S waves in the right precordial leads (V1-3), and usually leads to left axis deviation. * As the ventricles are activated sequentially (right, then left) rather than simultaneously, this produces a broad or notched (‘M’-shaped) R wave in the lateral leads. LBBB M and W Left Bundle Branch Block Dominant S wave in V1 with broad, notched ('M'-shaped) R wave in V6 Diagnostic Criteria * QRS duration of 120 ms * Dominant S wave in V1 * Broad monophasic R wave in lateral leads (I, aVL, V5-V6) * Absence of Q waves in lateral leads (I, V5-V6; small Q waves are still allowed in aVL) * Prolonged R wave peak time > 60ms in left precordial leads (V5-6) Associated Features * Appropriate discordance: the ST segments and T waves always go in the opposite direction to the main vector of the QRS complex * Poor R wave progression in the chest leads * Left axis deviation QRS Morphology in the Lateral Leads The R wave in the lateral leads may be either: * ‘M’-shaped * Notched * Monophasic * RS complex Causes * Aortic stenosis * Ischaemic heart disease * Hypertension * Dilated cardiomyopathy * Anterior MI * Primary degenerative disease (fibrosis) of the conducting system (Lenegre disease) * Hyperkalaemia * Digoxin toxicity Diagnostic Criteria RBBB 1. Broad QRS > 120 ms 2. RSR’ pattern in V1-3 (‘M-shaped’ QRS complex) 3. Wide, slurred S wave in the lateral leads (I, aVL, V5-6 Associated Features * ST depression and T wave inversion in the right precordial leads (V1-3) Variations * Sometimes rather than an RSR’ pattern in V1, there may be a broad monophasic R wave or a qR complex. Causes of RBBB # Right ventricular hypertrophy / cor pulmonale # Pulmonary embolus # Ischaemic heart disease # Rheumatic heart disease # Myocarditis or cardiomyopathy # Degenerative disease of the conduction system # Congenital heart disease (e.g. atrial septal defect) |
|
|
|
[TMP-131]] [Aug09]
Troponin is elevated post-infarct A. 1-2 days B. 2-5 days C. 5-14 days D. 7-21 days E ? |
ANSWER D
|
|
|
|
Black Bank August 2009
12. (NEW) Fit lady for elective laparoscopic cholecystectomy seen in PreAdmission Clinic. ECG shows LAD, RSR in V1, wide slurred S in V6 and QRS duration 0.2 msec. Your options a. Refer to cardiology b. Crack on c. Place permanent pacemaker d. Place temporary pacing wires e. Give atropine premedication |
ANSWER B
LAD and RBBB = bifascicular block. As per AHA/ACC go forth. Unless patient described intermittent syncope, indicating an intermittent trifasicular (complete) heart block. |
|
|
|
Diagnostic Criteria for LBBB
|
Left Bundle Branch Block
Background * Normally the septum is activated from left to right, producing small Q waves in the lateral leads. * In LBBB, the normal direction of septal depolarisation is reversed (becomes right to left), as the impulse spreads first to the RV via the right bundle branch and then to the LV via the septum. * This sequence of activation extends the QRS duration to > 120 ms and eliminates the normal septal Q waves in the lateral leads. * The overall direction of depolarisation (from right to left) produces tall R waves in the lateral leads (I, V5-6) and deep S waves in the right precordial leads (V1-3), and usually leads to left axis deviation. * As the ventricles are activated sequentially (right, then left) rather than simultaneously, this produces a broad or notched (‘M’-shaped) R wave in the lateral leads. Diagnostic Criteria * QRS duration of 120 ms * Dominant S wave in V1 * Broad monophasic R wave in lateral leads (I, aVL, V5-V6) * Absence of Q waves in lateral leads (I, V5-V6; small Q waves are still allowed in aVL) * Prolonged R wave peak time > 60ms in left precordial leads (V5-6) Associated Features * Appropriate discordance: the ST segments and T waves always go in the opposite direction to the main vector of the QRS complex * Poor R wave progression in the chest leads * Left axis deviation QRS Morphology in the Lateral Leads *The R wave in the lateral leads may be either: * ‘M’-shaped * Notched * Monophasic * RS complex QRS Morphology in V1 *The QRS complex in V1 may be either: * rS complex (small R wave, deep S wave) * QS complex (deep Q/S wave with no preceding R wave) Causes * Aortic stenosis * Ischaemic heart disease * Hypertension * Dilated cardiomyopathy * Anterior MI * Primary degenerative disease (fibrosis) of the conducting system (Lenegre disease) * Hyperkalaemia * Digoxin toxicity |
|
|
|
Diagnostic Criteria for RBBB
|
Right Bundle Branch Block
Background * In RBBB, activation of the right ventricle is delayed as depolarisation has to spread across the septum from the left ventricle. * The left ventricle is activated normally, meaning that the early part of the QRS complex is unchanged. * The delayed right ventricular activation produces a secondary R wave (R’) in the right precordial leads (V1-3) and a wide, slurred S wave in the lateral leads. * Delayed activation of the right ventricle also gives rise to secondary repolarization abnormalities, with ST depression and T wave inversion in the right precordial leads. * In isolated RBBB the cardiac axis is unchanged, as left ventricular activation proceeds normally via the left bundle branch. ECG changes in RBBB Diagnostic Criteria * Broad QRS > 120 ms * RSR’ pattern in V1-3 (‘M-shaped’ QRS complex) * Wide, slurred S wave in the lateral leads (I, aVL, V5-6) Associated Features * ST depression and T wave inversion in the right precordial leads (V1-3) Variations * Sometimes rather than an RSR’ pattern in V1, there may be a broad monophasic R wave or a qR complex. Causes of RBBB # Right ventricular hypertrophy / cor pulmonale # Pulmonary embolus # Ischaemic heart disease # Rheumatic heart disease # Myocarditis or cardiomyopathy # Degenerative disease of the conduction system # Congenital heart disease (e.g. atrial septal defect) Incomplete RBBB * Incomplete RBBB is defined as an RSR’ pattern in V1-3 with QRS duration < 120ms. * It is a normal variant, commonly seen in children (of no clinical significance). |
|
|
|
Diagnostic Criteria for left anterior hemiblock
|
Background
* In left anterior fascicular block (aka left anterior hemiblock), impulses are conducted to the left ventricle via the left posterior fascicle, which inserts into the infero-septal wall of the left ventricle along its endocardial surface. * On reaching the left ventricle, the initial electrical vector is therefore directed downwards and rightwards (as excitation spreads outwards from endocardium to epicardium), producing small R waves in the inferior leads (II, III, aVF) and small Q waves in the left-sided leads (I, aVL). * The major wave of depolarisation then spreads in an upwards and leftwards direction, producing large positive voltages (tall R waves) in the left-sided leads and large negative voltages (deep S waves) in the inferior leads. * This process takes about 20 milliseconds longer than simultaneous conduction via both fascicles, resulting in a slight widening of the QRS. * The impulse reaches the left-sided leads later than normal, resulting in a increased R wave peak time (the time from onset of the QRS to the peak of the R wave) in aVL. Diagnostic Criteria for LAFB * Left axis deviation (usually between -45 and -90 degrees) * Small Q waves with tall R waves (= ‘qR complexes’) in leads I and aVL * Small R waves with deep S waves (= ‘rS complexes’) in leads II, III, aVF * QRS duration normal or slightly prolonged (80-110 ms) * Prolonged R wave peak time in aVL > 45 ms * Increased QRS voltage in the limb leads Handy Tips * In LAFB, the QRS voltage in lead aVL may meet voltage criteria for LVH (R wave height > 11 mm), but there will be no LV strain pattern. |
|
|
|
Diagnostic Criteria for left posterior hemiblock
|
Left Posterior Fascicular Block
Background * In left posterior fascicular block (aka left posterior hemiblock), impulses are conducted to the left ventricle via the left anterior fascicle, which inserts into the upper, lateral wall of the left ventricle along its endocardial surface. * On reaching the ventricle, the initial electrical vector is therefore directed upwards and leftwards (as excitation spreads outwards from endocardium to epicardium), causing small R waves in the lateral leads (I and aVL) and small Q waves in the inferior leads (II, III and aVF). * The major wave of depolarisation then spreads along the free LV wall in a downward and rightward direction, producing large positive voltages (tall R waves) in the inferior leads and large negative voltages (deep S waves) in the lateral leads. * This process takes up to 20 milliseconds longer than simultaneous conduction via both fascicles, resulting in a slight widening of the QRS. * The impulse reaches the inferior leads later than normal, resulting in a increased R wave peak time (= the time from onset of the QRS to the peak of the R wave) in aVF. Diagnostic Criteria for LPFB * Right axis deviation (> +90 degrees) * Small R waves with deep S waves (= ‘rS complexes’) in leads I and aVL * Small Q waves with tall R waves (= ‘qR complexes’) in leads II, III and aVF * QRS duration normal or slightly prolonged (80-110ms) * Prolonged R wave peak time in aVF * Increased QRS voltage in the limb leads * No evidence of right ventricular hypertrophy * No evidence of any other cause for right axis deviation Handy Tips * LPFB is much less common than LAFB, as the broad bundle of fibres that comprise the left posterior fascicle are relatively resistant to damage when compared with the slim single tract that makes up the left anterior fascicle. * It is extremely rare to see LPFB in isolation. It usually occurs along with RBBB in the context of a bifascicular block. * Do not be tempted to diagnose LPFB until you have ruled out more significant causes of right axis deviation: i.e. acute PE, tricyclic overdose, lateral MI, right ventricular hypertrophy. |
|
|
|
What is a U wave?
|
U Wave
The U wave is a small (0.5 mm) deflection immediately following the T wave, usually in the same direction as the T wave. It is best seen in leads V2 and V3. Normal U Wave Source of the U wave The source of the U wave is unknown. Three common theories regarding its origin are: * Delayed repolarisation of Purkinje fibres * Prolonged repolarisation of mid-myocardial “M-cells” * After-potentials resulting from mechanical forces in the ventricular wall Features of Normal U waves * The U wave normally goes in the same direction as the T wave * U -wave size is inversely proportional to heart rate: the U wave grows bigger as the heart rate slows down * U waves generally become visible when the heart rate falls below 65 bpm * The voltage of the U wave is normally < 25% of the T-wave voltage: disproportionally large U waves are abnormal * Maximum normal amplitude of the U wave is 1-2 mm Abnormalities of the U wave * Prominent U waves * Inverted U waves Prominent U waves * U waves are prominent if > 1-2mm or 25% of the height of the T wave * The most common cause of prominent U waves is bradycardia * Abnormally prominent U waves are characteristically seen in severe hypokalaemia Prominent U waves may also be seen with: * Hypomagnesaemia * Hypocalcaemia * Hypothermia * Raised intracranial pressure * Left-ventricular hypertrophy / HOCM The following drugs may cause prominent U waves: * Digoxin * Phenothiazines (thioridazine) * Class Ia antiarrhythmics (quinidine, procainamide) * Class III antiarrhythmics (sotalol, amiodarone) Note that many of the conditions causing prominent U waves will also cause a long QT. Inverted U waves * U-wave inversion is abnormal (in leads with upright T waves) * A negative U wave is highly specific for the presence of heart disease The main causes of inverted U waves are: * Coronary artery disease * Hypertension * Valvular heart disease * Congenital heart disease * Cardiomyopathy * Hyperthyroidism In patients presenting with chest pain, inverted U waves: * Are a very specific sign of myocardial ischaemia * May be the earliest marker of unstable angina and evolving myocardial infarction * Have been shown to predict a ≥ 75% stenosis of the LAD / LMCA and the presence of left ventricular dysfunction |
|
|
|
What is a Osborn Wave?
|
Osborn Wave (J Wave)
* The Osborn wave (J wave) is a positive deflection at the J point (negative in aVR and V1) (ie. positive deflection following immediately following QRS) * It is usually most prominent in the precordial leads * Characteristically seen in hypothermia (typically T<30C), but they are not pathognomonic. * J waves may be seen in a number of other conditions: o normal variant o hypercalcemia o medications o neurological insults such as intracranial hypertension, severe head injury and subarachnoid hemorrhage o Le syndrome d’Haïssaguerre (idiopathic VF) The height of the J wave is roughly proportional to the degree of hypothermia |
|
|
|
Describe LVH.
|
Left Ventricular Hypertrophy
Background * The left ventricle hypertrophies in response to pressure overload secondary to conditions such as aortic stenosis and hypertension. * This results in increased R wave amplitude in the left-sided ECG leads (I, aVL and V4-6) and increased S wave depth in the right-sided leads (III, aVR, V1-3). * The thickened LV wall leads to prolonged depolarization (increased R wave peak time) and delayed repolarization (ST and T-wave abnormalities) in the lateral leads. Criteria for Diagnosing LVH * There are numerous criteria for diagnosing LVH, some of which are summarised below. * The most commonly used are the Sokolov-Lyon criteria (S wave depth in V1 + tallest R wave height in V5-V6 > 35 mm). * Voltage criteria must be accompanied by non-voltage criteria to be considered diagnostic of LVH. Voltage Criteria Limb Leads * R wave in lead I + S wave in lead III > 25 mm * R wave in aVL > 11 mm * R wave in aVF > 20 mm * S wave in aVR > 14 mm Precordial Leads * R wave in V4, V5 or V6 > 26 mm * R wave in V5 or V6 plus S wave in V1 > 35 mm * Largest R wave plus largest S wave in precordial leads > 45 mm Non Voltage Criteria * Increased R wave peak time > 50 ms in leads V5 or V6 * ST segment depression and T wave inversion in the left-sided leads: AKA the left ventricular ‘strain’ pattern Additional ECG changes seen in LVH * There may be associated signs of left atrial enlargement * There is commonly a left axis deviation * ST depression and T wave inversion in the left precordial leads may be accompanied by reciprocal ST elevation (‘high take off’) in the right precordial leads Causes of LVH * Hypertension (most common cause) * Aortic stenosis * Aortic regurgitation * Mitral regurgitation * Coarctation of the aorta * Hypertrophic cardiomyopathy Handy Tips * Voltage criteria alone are not diagnostic of LVH * ECG changes are an insensitive means of detecting LVH (patients with clinically significant left ventricular hypertrophy seen on echocardiography may still have a relatively normal ECG) |
|
|
|
Describe RVH.
|
Right ventricular hypertrophy
Electrocardiographic Features Diagnostic criteria * Right axis deviation of +110° or more * Dominant R wave in V1 (> 7mm) * QRS duration < 120ms (i.e. changes not due to RBBB) Supporting criteria * ST depression / T wave inversion in the right precordial (V1-4) and inferior (II, III, aVF) leads * Deep S waves in the lateral leads (I, aVL, V5-V6) Causes * Pulmonary hypertension * Mitral stenosis * Acute pulmonary embolism * Chronic lung disease (cor pulmonale) * Congenital heart disease (e.g. Tetralogy of Fallot, pulmonary stenosis) |
|
|
|
What is a Delta wave?
|
Delta Wave
The characteristic ECG findings in the Wolff-Parkinson-White syndrome are: * short PR interval (< 120ms) * broad QRS (> 100ms) * a slurred upstroke to the QRS complex (the delta wave) |
|
|
|
Describe the ECG changes which maybe seen with PE.
|
ECG changes in PE are related to:
* dilation of the right atrium and right ventricle with consequent shift in the position of the heart * right ventricular ischaemia * increased catecholamine levels (which drives the tachyarrhythmias) The following ECG changes may be seen in acute pulmonary embolism: * Sinus tachycardia * SI QIII TIII – deep S wave in I, Q wave in III, inverted T wave in III * Complete or incomplete RBBB * Right axis deviation * Right ventricular strain pattern: T wave inversions in V1-3, sometimes extending to V4 * Simultaneous T wave inversions in the inferior (II, III, aVF) and right precordial leads (V1-3). * Right atrial enlargement (“P pulmonale”): peaked P wave in lead II > 2mm in height * Clockwise rotation: shift of the R/S transition point towards V6, persistent S wave in V6 * Atrial tachyarrhythmias: AF, flutter, atrial tachycardia |
|
|
|
Black Bank August 2009
18. (NEW) Patient with known severe aortic regurgitation. Auscultation reveals loud mid diastrolic murmur in aortic area. You also hear a quiet mid diastolic murmur in the apex. This is a. Functional mitral stenosis b. Mitral valve incompetence c. Impaired LV function d. Papillary muscle dysfunction |
ANSWER A
|
|
|
|
Black Bank August 2009
29. (NEW) Which patients do not get pulmonary hypertension a. ASD b. Chronic thromboembolism c. Tetralogy d. MR e. MS |
ANSWER C
Must be C as you have some degree of RVOT obstruction thus pulmonary blood flow is decreased, and your mitral valve is competent so there is no increase in LA pressure. |
|
|
|
Black Bank August 2009
66. 70 y old patient with AF (rate 80/min) in pre-admission clinic booked for ant resection. (it was not mentioned if AF was old or new or if on patient was on any medication) What management? A. Crack on B. Echocardiography and Cardioversion C. Immediate Cardioversion D. ? E. ? |
This patient should undergo evaluation and treatment before non-cardiac surgery.
This can be considered an active cardiac condition. 1. Unstable coronary syndromes Unstable or severe angina* (CCS class III or IV)† Recent MI‡ 2. Decompensated HF (NYHA functional class IV; worsening or new-onset HF) 3. Significant arrhythmias -High-grade atrioventricular block -Mobitz II atrioventricular block -Third-degree atrioventricular heart block -Symptomatic ventricular arrhythmias -Supraventricular arrhythmias (including atrial fibrillation) with uncontrolled ventricular rate (HR greater than 100 bpm at rest) -Symptomatic bradycardia -Newly recognized ventricular tachycardia 5. Severe valvular disease -Severe aortic stenosis (mean pressure gradient greater than 40 mm Hg, aortic valve area less than 1.0 cm2, or symptomatic) -Symptomatic mitral stenosis (progressive dyspnea on exertion, exertional presyncope, or HF) |
|
|
|
MC161 [Mar10][Aug10]
Drug eluting stent 6 months old. On aspirin and prasugrel 10mg. Elective lap cholecystectomy for biliary colic. A. Do case while taking both B. Do case while stopping both C. Stop Prasugrel for 7 days, keep taking aspirin D. Stop Prasugrel for some other different time E. Post-pone for 6 months |
ANSWER E
As per AHA/ACC Guidelines, recommended to continue dual anti-platelet therapy for 365 days, and I would consider prasugrel the same as clopidogrel. Given that this is an elective procedure, and the potential for blood loss (while usually minimal) is significant (especially given dual anti-platelet therapy), the procedure should be delayed for another 6 months (i.e. 12 months from time of stent placement). The risk of an in-stent thrombosis is high if both anti-platelet drugs are not continued for the full 12 months. |
|
|
|
MC161 [Mar10][Aug10]
Drug eluting stent 6 months old. On aspirin and prasugrel 10mg. Elective lap cholecystectomy for biliary colic. A. Do case while taking both B. Do case while stopping both C. Stop Prasugrel for 7 days, keep taking aspirin D. Stop Prasugrel for some other different time E. Post-pone for 6 months |
ANSWER E
As per AHA/ACC Guidelines, recommended to continue dual anti-platelet therapy for 365 days, and I would consider prasugrel the same as clopidogrel. Given that this is an elective procedure, and the potential for blood loss (while usually minimal) is significant (especially given dual anti-platelet therapy), the procedure should be delayed for another 6 months (i.e. 12 months from time of stent placement). The risk of an in-stent thrombosis is high if both anti-platelet drugs are not continued for the full 12 months. |
|
|
|
TMP-106 [Mar10] [Aug10]
A 75yo male with moderate aortic stenosis (valve area 1.1cm2). Gets mild dyspnoea on exertion but otherwise asymptomatic. Needs hip replacement. A. Continue with surgery B. Beta block then continue C. Get myocardial perfusion scan D. Postpone surgery awaiting AVR E. Postpone surgery awaiting balloon valvotomy |
ANSWER D
|
|
|
|
Black Bank March 2010
50.POISE trial showed A. Increase CVA B. Anaphylaxis C. renal failure D. Increased AMI |
ANSWER A
|
|
|
|
TMP-112 [Mar10]
Patient for fempop bypass (i believe it said "angioplasty"), history of CCF. Also has diabetes on oral hypoglycaemics, controlled hypertension and atrial fibrillation at rate of 80bpm. A. Medium risk surgery, medium risk patient B. Medium risk surgery, high risk patient C. High risk surgery low risk patient D. High risk surgery, medium risk patient E. High risk surgery, high risk patient |
ANSWER D
Fem-pop bypass is HIGH risk surgery This patient has 2 intermediate risk factors: a history of prior CCF, and diabetes. The controlled HT and AF<80bpm are minor risk factors * High risk pt = An "active cardiac condition" - Unstable coronary syndromes - Unstable or severe angina (CCS class III or IV) - Recent MI - Decompensated HF - NYHA class IV - Worsening or new-onset HF - Significant arrhythmias - High-grade A-V block - Mobitz type II A-V block - 3rd degree A-V block - Symptomatic ventricular arrhythmias - SVT (incl AF) with uncontrolled ventricular rate (HR>100bpm @ rest) - Symptomatic bradycardia - Newly recognised VT - Severe valvular disease - Severe AS (mean P gradient > 40mmHg; valve area < 1.0cm2; symptomatic) - Symptomatic mitral stenosis (progressive SOBOE, exertional presyncope, or HF) * Medium risk pt = Presence of "clinical risk factors" (presumably 1 or more) - ischaemic heart disease - compensated or prior heart failure - diabetes mellitus - renal insufficiency (creatinine >2mg/dL, which is >177umol/L) - cerebrovascular disease * Low risk pt = Minor predictors - Age >70 - Abnormal ECG (LVH; LBBB; ST-T abnormalities) - Rhythm other than sinus - Uncontrolled systemic hypertension |
|
|
|
TMP-109 [Mar10] [Aug10]
The MAIN indication for biventricular pacing is A. complete heart block B. congestive cardiac failure C. VF D. ? E. ? |
ANSWER B
Biventricular pacing is defined as a lead in the RV to pace the interventricular septum, and a lead in the coronary sinus which can pace the LV lateral free wall. This is apparently most commonly used in patients with LBBB which can cause dyssynchronous contraction of the LV leading to impaired systolic function. The biventricular pacing "resynchronises" LV contraction and improves systolic function. Indications: (i) severe cardiomyopathy (EF<35%), and (ii) LBBB with NYHA class III or IV symptoms despite maximal medical therapy. |
|
|
|
TMP-128 [Aug09] Indication for percutaneous closure of ASD
A. Ostium primum < 3cm B. Ostium primum > 3cm C. Ostium secundum < 3 cm D. Ostium secundum > 3cm E. Sinus venosus ASD |
ANSWER C
Of these, only an ostium secundum ASD is suitable for percutaneous closure. |
|
|
|
Black Bank 2010
109.Reverse splitting of the second heart sound occurs with: A. LBBB B. Pulmonary hypertension C. Acute pulmonary embolus D. ASD E. Severe MR |
ANSWER A and D
Physiology of the Second Heart Sound -Audible component of the closure of aortic and pulmonary valves -A2 followed by P2, separated only by 0.02 - 0.08 seconds. -Although contraction of both ventricles occurs at the same time, difference in opening and closure are due to differences in impedance of each vascular bed -as PVR is low, PV opens sooner and closes later -as SVR is high, AV opens later and closes sooner -therefore A2-P2 -this interval is widened by deep inspiration, known as Physiological Splitting. Abnormal Splitting of Second Heart Sound (1) persistently single; -S2 remains single throughout respiratory cycle -most commonly due to inaudibility -in setting of CHD : absence of PV : Fontans (pulmonary atresia, severe PV stensosis, dysplastic PV, transposition of great arteries) (2) persistent (audible expiratory) splitting, with normal respiratory variation; -most common cause if RBBB (3) persistent splitting without respiratory variation (fixed splitting); -A2 and P2 is constantly wide and remains unchanged during respiratory cycle -Hallmark of ASD (4) reversed (paradoxical) splitting. -Reversed sequence of semilunar valve closure P2-A2 -Common causes : LBBB and Right ventricular PPM (activation of the RV before LV) -Other causes : RV ectopic beats, prolonged LV mechanical systole, HOCM, Severe hypertension, PDA |
|
|
|
Black Bank March 2010
110. Atrial fibrillation: A. Cardioversion results in longer life expectency than rate control B. Need to stay on warfarin following cardioversion C. Pt with HR <80 generally do not require anticoagulation D. |
ANSWER B
|
|
|
|
Black Bank August 2010
81. Patient with diastolic dysfunction. Is it caused by: a. Restrictive cardiomyopathy b. Dilated cardiomyopathy c. d. e. |
ANSWER A
|
|
|
|
TMP-Jul10-014 Patient with aortic dissection. Blood pressure 150/90. Best drug to control BP:
A. Captopril B. Esmolol C. GTN D. Hydralazine E. SNP |
ANSWER B
B-blockade has most desired effects -reduce the force of LV ejection (dP/dt) SNP/GTN can be used, but always need to be combined with beta blockers, as a reflex tachycardia and contractility can result in increased sheer damage to the dissection. |
|
|
|
TMP-Jul10-015
Type of aortic dissection – which classically NON-operative management: A. DeBakey Type I B. DeBakey Type II C. Stanford A D. Stanford B E. Stanford C |
The Stanford classification divides dissections into 2 types, type A and type B.
* Type A involves the ascending aorta (DeBakey types I and II); type B does not (DeBakey type III). * This system also helps delineate treatment. Usually, type A dissections require surgery, while type B dissections may be managed medically under most conditions. Type A ->Surgery Type B -> Medical The DeBakey classification divides dissections into 3 types. * Type I involves the ascending aorta, aortic arch, and descending aorta. * Type II is confined to the ascending aorta. * Type III is confined to the descending aorta distal to the left subclavian artery. o Type III dissections are further divided into IIIa and IIIb. o Type IIIa refers to dissections that originate distal to the left subclavian artery but extend both proximally and distally, mostly above the diaphragm. o Type IIIb refers to dissections that originate distal to the left subclavian artery, extend only distally and may extend below the diaphragm. |
|
|
|
TMP-Jul10-010
The BEST clinical indicator of SEVERE aortic stenosis is: A. Presence of thrill B. Mean Gradient 30mmHg C. Valve area of 1.2 cm2 D. Slow rising pulse and ESM radiating to carotids E. Shortness of breath |
ANSWER E
|
|
|
|
Black Bank March 2011
6. NEW: ECG- which does NOT have abnormal Q waves: A: Digoxin toxicity B: Anterior myocardial infartion C: Previous AMI D: LBBB E: Wolff-Parkinson-White syndrome |
ANSWER A
Q Wave * A Q wave is any negative deflection that precedes an R wave Normal Q wave Origin of the Q Wave * The Q wave represents the normal left-to-right depolarisation of the interventricular septum * Small ‘septal’ Q waves are typically seen in the left-sided leads (I, aVL, V5 and V6) Q waves in different leads * Small Q waves are normal in most leads * Deeper Q waves (>2 mm) may be seen in leads III and aVR as a normal variant * Under normal circumstances, Q waves are not seen in the right-sided leads (V1-3) Pathological Q Waves Q waves are considered pathological if: * > 40 ms (1 mm) wide * > 2 mm deep * > 25% of depth of QRS complex * Seen in leads V1-3 Pathological Q waves usually indicate current or prior myocardial infarction. Differential diagnosis: * myocardial infarction * cardiomyopathies — hypertrophic (HOCM), infiltrative * rotation of the heart — extreme clockwise or counter-clockwise rotation * lead placement errors — e.g. upper limb leads placed on lower limbs Loss of normal Q waves The absence of small septal Q waves in leads V5-6 should be considered abnormal. Absent Q waves in V5-6 is most commonly due to LBBB. |
|
|
|
8. NEW. TMP-Jul10-010?? Long stem about an old #NOF patient with aortic stenosis. What is a sign/ investigation/ symptom that shows the most severity? (ie Which one of these would indicate that the lesion was severe?)
A: Thrill in Aortic area B: Murmur in lower left sternal edge C: Murmur radiating to carotids D: History of ischaemic heart disease or coronary artery disease E: history of angina/ syncope |
ANSWER E
|
|
|
|
Black Bank March 2011
9. NEW. You get a TOE on a patient with aortic stenosis. What is the finding most likely to indicate that the valve needs replacement? possibly same as TMP-Jul10-010 A: Average pressure gradient 30mmHg B: Valve area 1.2cm(squared) C: dyspnoea |
ANSWER C
|
|
|
|
Black Bank March 2011
32. NEW. 75 year old with non-valvular AF usually on warfarin has their warfarin stopped for one week. What is their daily risk of stroke? A: 1% B: 0.1% C: 0.01% D: 4% E: 10% |
ANSWER C
Embolic Risk of AF : Application of the CHADS2 CHF - 1 HT - 1 Age > 75 - 1 DM - 1 CVA - 2 Score of *0 : 0.5-1.7% Risk per year of stroke, Commence Aspirin only *1 : Unsure if stroke benefit outweights bleeding risk if patient is female; greater >65 OR has any artherosclerotic disease (PVD/CAD) they should be started on warfarin (CHA2S2VASc score) *2 = 4% *3 = 6% *4 = 8.5% *5 = 12.5% *6 = 18% 2%/365 = 0.005% |
|
|
|
Black Bank March 2011
34. NEW. Patient with Marfan's and 2 hours of severe chest pain, mild hypertension and ECG showing ischaemia. The next best step is urgent: A: CT B: TOE C: ? D: Angiography and PCI E: Thrombolysis |
ANSWER A
|
|

