![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
41 Cards in this Set
- Front
- Back
|
What problems are there in renal failure?
|
Inadequate excretion
Excessive water losses |
|
|
What 3 things do you require for normal renal function?
|
Normal perfusion of kidneys
Normal glomerulus Normal (efficient) output of urine |
|
|
What are the 3 types of kidney failure?
|
Pre-renal
Intrinsic Post-renal |
|
|
What can cause defective perfusion to the kidneys?
|
Hypovolemia
Low effective circulating volume due to cardiac failure Vascular occlusion - due to shock from Gram-neg bacteria |
|
|
What is oliguria?
|
Small volume of concentrated urine
|
|
|
What are the consequences of poor perfusion to the kidneys?
|
Lowered GFR
Lowered SNGFR (single nephron GFR) Leads to: Azataemia (urea and creatinine) Hyperkalaemia Hyperphosphataemia Acidaemia Oliguria |
|
|
How does the kidney try and compensate for poor blood perfusion to the glomerulus?
|
Angiotensin-II mediated constriction of efferent arteriole
|
|
|
How does the medulla react to poor perfusion?
|
Prostaglandin release causes vasodilation
(blocked by NSAIDS) |
|
|
Why is the medulla vulnerable to defective perfusion?
|
It is already hypoxic and when full perfusion is restored there may be a wash out of the medulla and its osmotic gradient and dilute urine produced
|
|
|
Why is the cortex vulnerable when exposed to poor perfusion?
|
Poor perfusion causes oxidative stress - mitochondria produce reactive oxygen species - causes damage to cell membranes
Further damage when perfusion is brought back to normal |
|
|
How may prerenal failure be reversible and irreversible?
|
Reversible if blood supply restored
Irreversible if kidney damage |
|
|
Significance of azotaemia and uraemia?
|
Azotaemia - urea and creatinine - only a measure of blood rather than a condition
Uraemia - causes polysystemic toxicity - due to urea and other peptide hormones such as insulin |
|
|
What are 3 types of intrinsic renal failure?
|
Glomerulonephritis
Inherited disease Amyloidosis |
|
|
What are the consequences of glomerulonephritis?
|
Accumulation of immune complexes and complement in the basal lamina of glomerulus
Leads to neutrophil recruitment, oxidative reactive generation, damage of cells and their matrices Proliferation of mesangial cells, thickening of GBM and glomerulosclerosis |
|
|
What inherited condition may lead to glomerulosclerosis?
|
Type IV collagen gene mutation
Leads to thickening of basement membrane and abnormal podocyte foot processes (Common in Samoyeds) |
|
|
How does amyloidosis come about?
|
Antigenic stimulation of the immune system
Leads to excessive production of serum protein AA Leads to reactive systemic amyloidosis - deposition of amyloid |
|
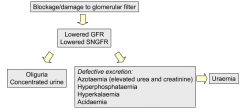
Remember this diagram
|
rpoij
|
|
|
What other consequence is seen with intrinsic renal failure?
|
Proteinuria
Damage to filter but some parts remain very open and protein leaks out |
|
|
What can cause corticol insult?
|
Nephrotoxicity
Ischaemia |
|
|
What are the consequences of cortical insult?
|
Necrosis of proximal tubular epithelium
Flattened epithelium and cellular debris in tubules |
|
|
What does the regeneration of the cortex depend on?
|
Whether the basement membrane is intact or not
Also ischaemic damage more severe |
|
|
What leads to the lowered GFR in defective reabsorption (i.e. cortical insult)?
|
Proximal tubule is damaged so less Na taken up, macula densa senses high Na, lowers GFR
Also debris in the tubules leads to back pressure in Bowman's capsule |
|
|
Which infectious agent can cause this defective reabsorption?
|
Leptospirosis
Bacteria form reservoir in tubule and |
|
|
What kind of infection is leptospirosis?
|
Descending infection, from blood to tubules
|
|
|
What is an ascending infection?
|
E.g. E coli or summat
|
|
|
What are the effects of hypoaldosteronism?
|
Poor Na uptake in proximal tubule
Leads to hypovolaemia Poor K excretion Leads to hyperkalaemia |
|
|
What are the effects of diabetes mellitus?
|
Glucosuria -> polyuria (as water follows the glucose)
Diabetic nephropathy - proteins in the blood become modified by glucose - glycosylation - vasculature becomes damaged |
|
|
What are the effects of diabetes insipidus?
|
Lack of ADH secretion or resistance to ADH
Leads to lack of recruitment of aquaporin-2 in collecting duct epithelium Loss of water through urine Polyuria |
|
|
What are 3 reasons for urinary tract blockage?
|
Congenital developmental problems
Stones - calculi Compression of ureter |
|
|
What are the effects of defective flow in the urinary tract?
|
Back-pressure in kidney
Leads to necrosis of epithelial tissue and dilation of the tubules Compression of the blood vessels -> ischaemia Inflammatory response -> fibrosis |
|
|
What leads to oliguria with a blockage in the urinary tract?
|
Back pressure in the tubules leads to Bowman's capsule
Loss of net filtration pressure leads to reduced GFR |
|
|
What is chronic renal failure?
|
The slow, progressive, irreversible loss of nephrons and kidney function
|
|
|
What are some causes of chronic renal failure?
|
Diabetic nephropathy
Hydronephritis Hypertension Infective damage in hypoperfusion |
|
|
At what stage of nephron loss does chronic renal failure occur?
|
70%
Less than 70% - no clinical signs |
|
|
Describe the changes to GFR and SNGFR with chronic renal failure
|
Decreased GFR
Increased SNGFR |
|
|
Why with a chronic loss of nephrons is there a rise in SNGFR?
|
Because many nephrons have died, the remaining ones have more blood to deal with, and thus more filtrate
|
|
|
What are the consequences of chronic nephron loss?
|
Polyuria -> polydypsia
Insufficient time to reabsorb Na and K -> hyponatraemia and hypokalaemia Plus azotaemia and hypophosphataemia leading to uraemia and hypocalcaemia Hyperfiltration leads to GBM permeability problems and mesangial cell proliferation + non-functional nephrons |
|
|
Describe the differences between acute and chronic renal failure
|
Chronic - polyuria, hypokalaemia and progressive damage to kidney
(instead of oliguria and hyperkalaemia) |
|
|
What is another name for calcitriol?
|
Vitamin D
|
|
|
How does chronic renal failure lead to hypocalcaemia?
|
Increased phosphate in the blood
Decreased calcium in blood as deposited in tissues Renal failure also leads to reduced 1-alpha hydroxylase -> reduced calcitriol levels -> further reduced calcium in the blood |
|
|
What is the effect of lowered plasma Ca?
|
Secondary hyperparathyroidism
As PTH is trying to correct lowered Ca |

