![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
189 Cards in this Set
- Front
- Back
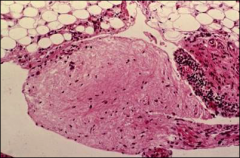
what is it
|
gonococcal infxn- worst outcome - PID leading to infertility
|
|
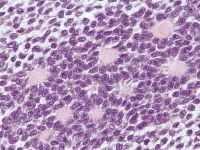
what is it, vaginal
|
vaginal adenosis
|
|
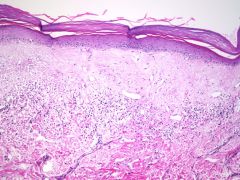
what is it, vulva
|
lichen sclerosus et atrophicus
multifocal Subepithelial homogenized zone Band of lymphocytes Not premalignant – predisposing factor |
|

what is it, vulva
|
lichen simplex chronicus
|
|
|
does lichen sclerosus et atrophicus predispose one to malignancy
|
yes
|
|
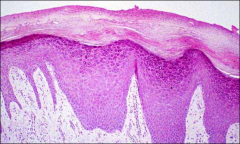
what is it, vulva
|
LSC, ddx is squamous hyperplasia, endpoint of many inflammatory dz
|
|

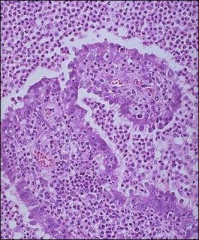
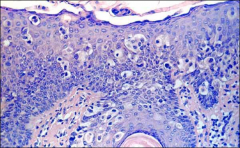
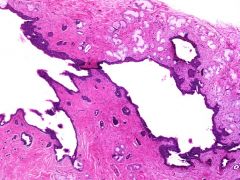
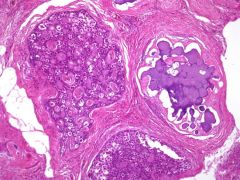
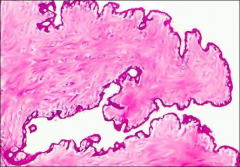
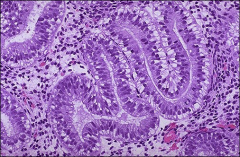
what is it, vulva
|
hidradenoma papilliferum - two cell types (with differential staining with IHC)
|
|
|
ihc for hidradenoma papilliferum
|
EMA+ (luminal layer)
Calponin, ASMA+ (basal layer) |
|
|
clinical fx of VIN (traditional)
|
HPV associated type
Younger age Multifocal associat with CIN Smoking |
|
|
simplex VIN clinical fx
|
HPV negative type
Associated with vulvar inflammatory disease (LS) Older age Unifocal Associated with p53 mutations Well differentiated simplex VIN |
|
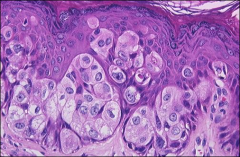
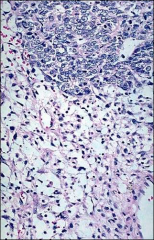
what is it, vulva
|
extramammary paget's
|
|
what is it vulva
|
melanoma
|
|
what is it vulva
|
angiomyofibroblastoma
Benign, non recurring, Well circumscribed Alternating hyper and hypocellular zones; thin-walled vessels; Stromal cells, wavy collagen strands; Rare mitoses; Mast cells cd34 and smooth muscle markers |
|
|
what age groups do angiomyofibroblastomas occur in
|
Reproductive age
|
|
|
ihc stains and EM for angiomyofibroblastoma
|
Vimentin, desmin, actin, CD 34+
EM: myofibroblasts |
|
what is it
|
aggressive angiomyxoma
Large, > 10 cm Locally infiltrative Bulky, gelatinous Hypocellular, loose stroma Numerous thin and thick-walled blood vessels (only thin in angiomyofibroblastoma) Rare mitoses Mast cells (like angiomyofibroblastoma Indolent, tendency to recur (unlike angiomyofibroblastoma) |
|
|
ihc for aggressive angiomyxoma
|
stromal cells: SMA, HHF 35, ER / PR +
|
|
|
cf angiomyofibroblastoma vs. aggressive angiomyxoma (4)
|
angiomyofibroblastoma is distinguished from aggressive angiomyxoma
by: its circumscribed border higher cellularity frequent presence of plump stromal cells lesser degree of stromal myxoid change |
|
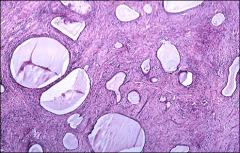
what is it, vagina
|
mesonephric/gartner's cyst - lateral wall; non
mucinous low-cuboidal epithelial cells |
|
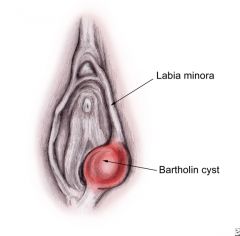
bartholin cyst location
|
just review
|
|
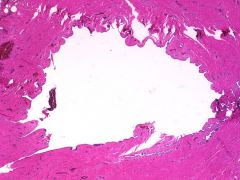
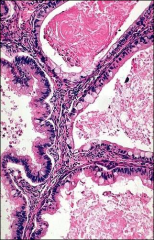
what is it, vagina
|
bartholin cyst; transitional epithelium with adjacent mucous glands
|
|
|
morphologic fx of simplex (differentiated) VIN
|
prominent parakeratosis, thickened epidermis, elongated and branched rete ridges; abnormal keratinocytes with large vesicular nuclei; focal macronucleoli; abundant eosinophilic cytoplasm; prominent intercellular bridges; mitoses common in basal layer; basal layer cells have smaller hyperchromatic nuclei with irregular contours (folded)
|
|
|
what constitutes microinvasion in scca of vulva
|
<1mm= microinvasion
|
|
|
stains for primary vulvar extramammary Paget's
|
primary vulva pagets: + for CAM 5.2, CEA, EMA, CK7, G6PD and *HER2neu, positive for muscicarmine
|
|
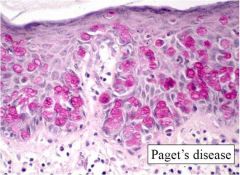
pagets what stain
|
mucicarmine
|
|
|
ddx for extramammary pagets in vulva
|
melanoma (positive melanoma markers)
extramammary pagets (mucicarmine, CAM 5.2, CEA, EMA, CK7, G6PD and *HER2neu) anorectal primary extension- CK7 (-), CK20+ urothelial primary extension - CK7 and CK20 +; uroplakin + |
|
|
distinguish between tumor thickness vs. depth of invasion in scca in vulva
|
Tumor thickness: measurement from granular layer (or surface if nonkeratinized) to deepest point of invasion
-Depth of invasion: measurement from epithelial-stromal junction of adjacent most superficial dermal papillae to deapest point of invasion |
|
|
when do a LN dissection for SCCA of vulva
|
anything over 1mm gets a LN dissection
|
|
|
hr hpv
|
HPV- 16, 18, 31, 33, 35, 45
|
|
|
lr hpv
|
HPV- 6, 11, 40, 54
|
|
|
cf depth of invasion of cervix vs. vulva
|
Vulva: DOI measured from uppermost dermal papillae, not BM; critical level= 1mm
Cervix: DOI measured from BM of adjacent surface epithelium or endocervical gland |
|
|
ais - see colposcopically or no
|
visible lesion is absent/rare
|
|
|
criteria for AIS
|
must see mitoses and apoptosis
+/- stratification and hyperchromasia |
|
|
most common hpv in ais
|
HPV 18
|
|
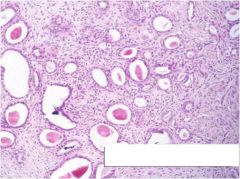
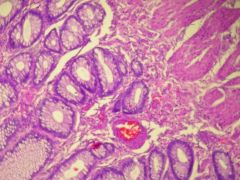
cervix, what is it
|
mesonephric remnants, more at lateral walls
|
|
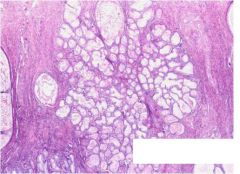
cervix, what is it
|
tunnel cluster
|
|
|
what can microglandular hyperplasia be associated with
|
pregnancy or hormone use
|
|
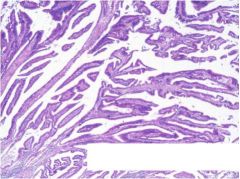
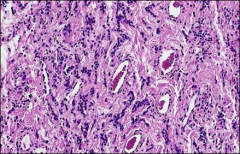
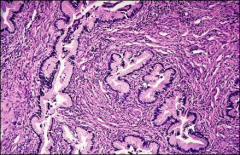
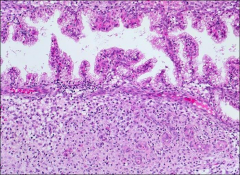
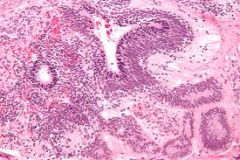
what is it, endocervix/LUS
|
villoglandular ca
|
|
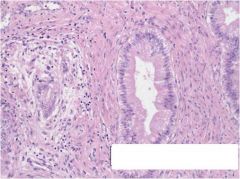
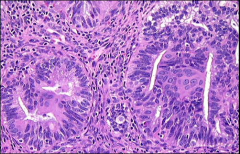
what is it, cervix
|
adenoma malignum - very well-differentiated glands, with rare nucleoli, but multiple foci of loose desmoplastic stromal reaction in multiple fields
|
|
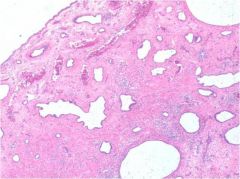
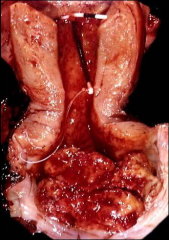
uterus, what is it, association
|
endometrium, associated w/ tamoxifen
tamoxifen polyps are large in size, typically multiple; with small, cystic glands, metaplasia, hyperplasia and myxoid changes |
|
|
criteria for calling atypia in endometrium
|
-nuclear enlargement (2-3x RBC)
Pleomorphism vesicular change Chromatin irregularity loss of polarity Prominent nucleoli Cellular stratification |
|
|
what role does PTEN play in endometrium
|
Loss of PTEN= neoplastic
|
|
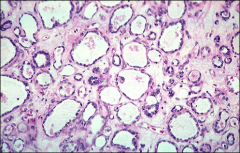
what is it, endometrium
|
cystic atrophy
|
|
|
What is Kurman and Norris' criteria for distinction between atypical hyperplasia and cancer
|
Kurman and Norris:
1. Desmoplastic stromal response (=ca, but rare to find) 2. Cribriform pattern- fused glands= CA 3. Replacement of stroma by squamous epithelium 4. Extenisive papillary pattern |
|
what is it, endometrium
|
endometrial ca, sertoliform variant
|
|
|
fx of type 1 endometrial ca
|
- Endometrioid adenocarcinoma = 80-90%
--estrogen dependent ( obesity, anovulatroy bleeding, late menopause) --good prognosis --a/w endometrial hyperplasia --Surgical stage III and IV in <20% at dx --IHC: loss of PTEN; +mut Kras and Microsatellite instability (MSI) |
|
|
fx of type II endometrial ca
|
-Serous carcinoma (<10%)
--non-estrogen-dependent --poor prognosis --usually a/w atrophy (older pts) --surgical stage III and IV in75% at dx --IHC: retains PTEN; p53+ |
|
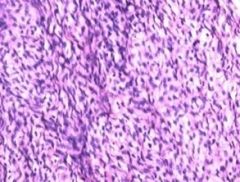
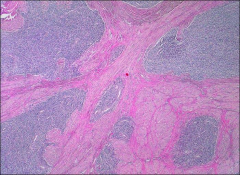
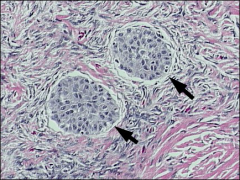
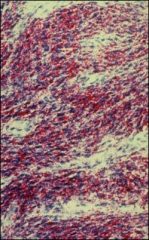
what is it, endometrium
|
Low-grade endometrial stromal sarcoma
-uniform cells, resembles proliferative stroma - must see mits - lvi common bag of worms - ddx: cellular leiomyoma |
|
|
common age for low grade endometrial stroma sarcoma
|
-75% are younger than 30 yrs old
|
|
|
ihc for low grade endometrial low grade stromal sarcoma
|
IHC: + for CD10, Vimentin, MSA, SMMT; rarely + for desmin
- ER/PR receptors, inhibin, CD99 (by contrast, leiomyoma- + for CD99 and SMA) |
|
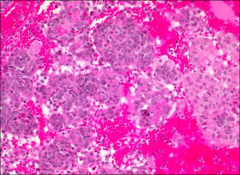
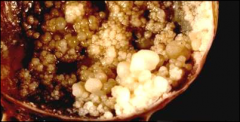
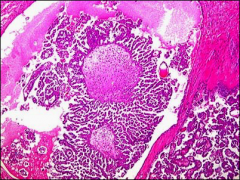
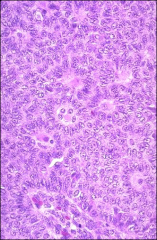
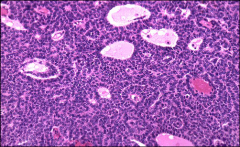
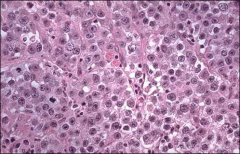
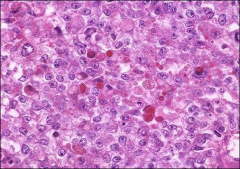
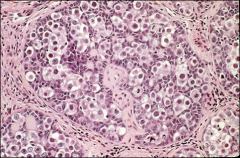
ovary
|
granulosa cell tumor
have Call-Exner bodies = spaces contain cellular debris and the nuclei around them are not making gland structures; they are found in the most common growth pattern- microfollicular; -but GCT can have many growth patterns- solid, trabecular, etc. -Adult type- has nuclear grooves (coffee-bean nuclei) -the juvenile form does not have grooves |
|
|
gross features of granulosa cell tumor
|
grossly- are cystic and solid, with areas of hemorrhage and necrosis; and may frequently rupture intraoperatively
|
|
|
other malignancy a/w granulosa cell tumor of ovary and why
|
** They produce estrogen- causing stimulation of endometrium with hyperplasia or carcinoma possible.
|
|
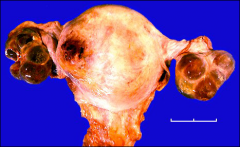
what is it, ovary
|
gonadoblastoma; composed of nests of germ cells and sex cord cells
|
|
|
what can gonadoblastoma be associated with
|
most often a/w mixed gonadal dysgenesis, with some Y chromosome material present
|
|
|
what can gonadoblastoma most commonly transform into
|
a benign entity- but MAY undergo malignant transformation--> malignant germ cell tumor
-most commonly- will become dysgerminoma |
|
|
cf depth of invasion of vulva melanoma to scca
|
vulva: surface of the epithelium to deepest portion of tumor
* different from squamous cell ca- which is measured from the adjacent dermal papillae to the deepest portion of tumor. |
|

what, ovary
|
fibrothecoma;
if ascites/right hydrothorax, called meig's syndrome |
|
what, ovary
|
fibrothecoma
|
|
|
what extraovarian malignancy can be assoc with fibrothecoma
|
they have endocrine function- commonly estrogen--> unopposed estrogen stimulation of the endometrium--> hyperplasia or carcinoma
|
|
|
most common type of malignant ovary histologic type
|
serous
frequently bilateral (60%) |
|
|
ihc for serous ovarian ca
|
-IHC: CK7 and WT-1 + (to determine if primary or secondary- ie from endometrium)
-p53 + (high-grade have p53 mutations) |
|
|
morphologic appearance of implant of serous borderline tumor (invasive implant)
|
Invasive: irregular infiltration; fibrotic, edematous or myxoid stroma; solid or cribriform nests; substantial atypia
|
|
|
morphologic appearance of implant of serous borderline tumor (non-invasive)
|
Non-invasive: sharp demarcation from normal tissue; fibrotic or inflammatory response; glands, papillary clusters or single cells; moderate atypia
|
|
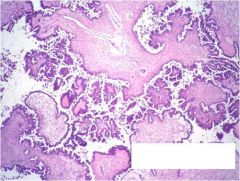
what, ovary
|
serous borderline tumor
|
|
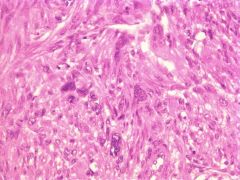
what, uterus, no mits, no necrosis
|
symplastic leiomyoma
|
|
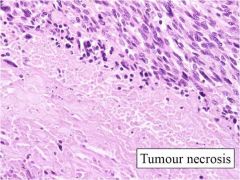
significance, uterus
|
tumor necrosis in smooth muscle tumor (real not infarction type)
tumor cells abut necrosis |
|
|
important mit counts in stratifying leiomyomas, atypical leiomyomas and leiomyosarcomas
|
mit>10/10hpf; if only focal atypia, criteria of >20/10 can be used to call atypical leio in absence of tumor necrosis
|
|
|
what is HHF35
|
muscle specific actin
|
|
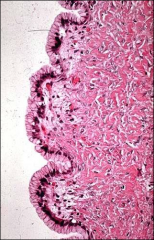
what, vagina
|
adenosis
Benign glandular epithelium with metaplasia |
|
|
associations/causes adenosis; at risk for
|
DES exposure
at risk for: clear cell carcinoma |
|
|
location at which adenosis is most likely found
|
upper 1/3, anterior wall
|
|
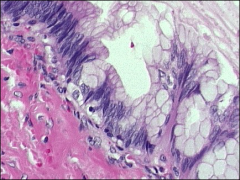
what, vagina, what associations, what 3 fx are favorable for prognosis
|
clear cell carcinoma, vagina
from adenosis (associated with DES) could also occur in cervix Favorable prognosis: low stage, low mitotic activity, mild nuclear atypia |
|
|
in whom does clear cell carcinoma of vagina/cervix occur in
|
<40, associated with DES exposure
|
|
what, vagina
|
fibroepithelial stromal polyp
|
|
|
risk factors CIN (5)
|
Early age at first intercourse
Multiple partners (multiple partners!) Smoking Immunodeficiency Poor hygiene, STDs |
|
|
morphologic fx of microglandular hyperplasia
|
Closely packed glands with mucin and
mixed inflammation; subnuclear vacuoles, rare mitoses |
|
|
how often see CIN if have AIS
|
CIN in 50 to 70% cases, 20% have history of CIN
|
|
what, cervix
|
adenoma malignum
|
|
|
associated syndrome adenoma malignum
|
Peutz jeghers
|
|
vagina
|
barrel shaped cervix; adenosquamous cell carcinoma, glassy cell variant (eos) - more aggressive
|
|
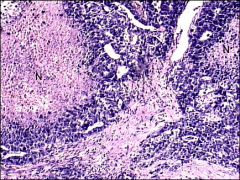
what, uterus, associations
|
chronic endometritis, IUD, actinomyces
|
|
|
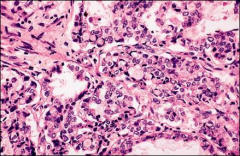
what, endometrium
|
granulomatous endometritis - most often TB, rarely fungal (eg.coccidiomycosis), viral (CMV)
|
|
endometrium
|
early secretory day 17 (pod 3)
decidualization around arteries pod9-10 |
|
endometrium
|
secretory - supranuclear vacuoles
|
|
endometrium
|
menstrual phase - exodus is 6-10 of menstrual cycle
|
|
|
endometrium 1:1 gland stroma ratio - 3 "causes"
|
Normal cycling endometrium
Dysfunctional uterine bleeding Infertility |
|
|
endometrium >1:1 gland stroma ratio - 2 "causal spectrums"
|
- hyperplasia/carcinoma
-late secretory/menstrual |
|
|
endometrium <1:1 gland stroma ratio - 3 "causes"
|
- atrophy
- stromal proliferation/tumors - decidua |
|

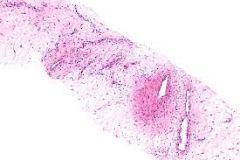
uterus, what
|
adenomyosis
|
|
|
risks for EM hyperplasia
|
Nulliparity
unopposed estrogen stimulation (exogenous, endogenous) PCO – Stein Leventhal syndrome Diabetes mellitus Hypertension – related to obesity Obesity |
|
uterus, what
|
atypical polypoid adenomyoma (if lots of fibrosis could call atypical polypoid adenofibroma)
features - Endometrial glands -Squamous morules - Myofibromatous stroma |
|
|
where are atypical polypoid adenomyomas most commonly found
|
LUS
|
|
|
in what age group can you find atypical polypoid adenomyomas
|
reproductive age
|
|
|
what syndrome can atypical polypoid adenomyomas be found
|
turners
|
|
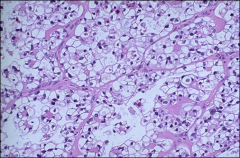
uterus, what
|
clear cell carcinoma
|
|
|
uterus, what
|
villoglandular endometrial ca
|
|
|
what histological fx is essential in an endometrial stromal nodule to distinguish it from a sarcoma
|
pushing border
|
|
|
in an undifferentiated endometrial sarcoma, which two of the three following features are most important, necrosis, mitoses or nuclear pleomorphism
|
necrosis and nuclear pleomorphism
|
|
what, uterus
|
endometrial stromal sarcoma
|
|
|
ihc for endometrial stromal sarcoma
|
Vimentin +
CD 10 + Actin – focally + Desmin – ER / PR +, low grade ESS |
|
|
carcinosarcoma
|
Mixture of malignant epithelium and sarcomatous stroma (latter usually predominating)
Homologous component is usually high grade (spindle cells, roundcells or giant cells). May resemble FS or LMS Heterologous - chondrosarcoma, osteosarcoma or RMS |
|
|
of a carcinosarcoma, which component is most likely to metastasize
|
Epithelial component of the tumor usually shows the most capability for invasion and metastases
|
|
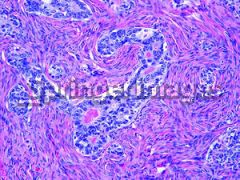
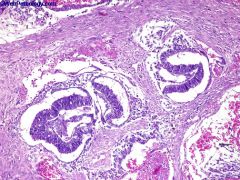
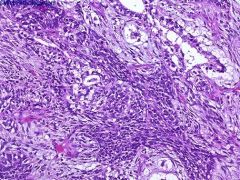
what, uterus
|
adenosarcoma - Epithelial and stromal elements with stromal hypercellularity
● Epithelial component appears benign; glands are usually large and dilated with periglandular stromal cuffing, 80% have cambium layer (stromal condensation) beneath surface epithelium and adjacent to glands (most characteristic histologic feature); mitotic activity and cytologic atypia are more common in this zone ● Epithelium is usually endometrioid but also ciliated, mucinous and even squamous ● Stroma has polypoid or leaf-like projections into glandular lumina, resembling phyllodes tumor of breast |
|
|
prognosis of verrucous ca
|
locally invasive, rarely distant metastases, better prognosis,
|
|
|
for cervix, depth of invasion for scca
|
recall, 3mm/5mm/7 mm review
|
|
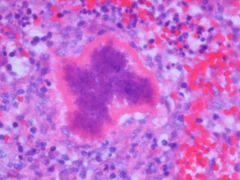
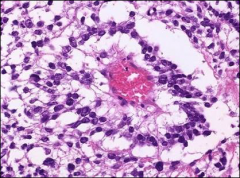
what is this
|
splendore-hoeppli phenomenon - assoc with ab-ag rxn.
means its causing infection |
|
|
really ugly cells - wondering about serous, what stain
|
p53
|
|
|
in heterologous elements of carcinosarcoma, what is the most common type
|
rhabdomyosarcoma
|
|
|
msot common site emosis
|
ovary
|
|
|
how does tb get to ft
|
hematogenous
|
|
fallopian tube
|
adenomatoid tumor
|
|
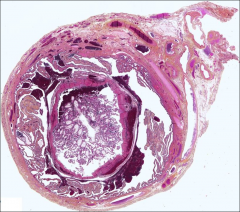
fallopian tube, where most common
|
ectopic pregnancy, ampulla
|
|
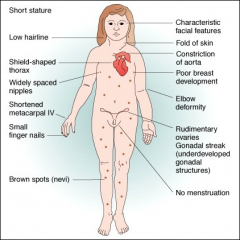
turners for review
|
for review
|
|
|
most common cancers from emosis
|
clear cell
secondary endometrioid low grade ESS |
|
explain ovarian cysts in choriocarcinoma of uterus
|
lutein cysts bilateral
|
|

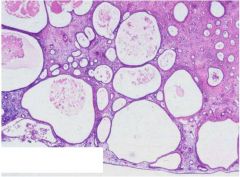
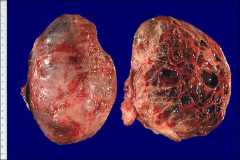
ovary
|
PCOS, stein leventhal
|
|

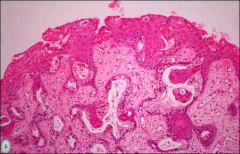
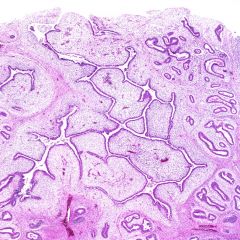
ovary
|
papillary serous cystadenoma
|
|
ovary
|
serous borderline
|
|
|
microinvasion for serous borderline
|
<3 mm (10mm length?)
|
|
ovary, significance
|
micropapillary serous carcinoma, medusa head; very elongated papillary structures
more likely bilateral, more likely to have surface involvement, more likely to have invasive implants |
|
|
peritoneum
|
noninvasive serous papillary implant - superficial, stuck on
|
|
|
peritoneum
|
desmoplastic, noninvasive implant - still superficial
|
|
peritoneum
|
invasive serous papillary implant
|
|
ovary
|
at least borderline (at least!!)
|
|
ovary
|
cystadenofibroma
|
|
ovary
|
mucinous cystadenoma, can be among the largest tumors you can get in ovary, intestinal type (more common; worse prognosis if malignancy)
|
|
ovary
|
mucinous cystadenoma, endocervical more often associated with emosis
|
|
ovary how far would you go
|
mucinous low malignant potential/borderline
|
|
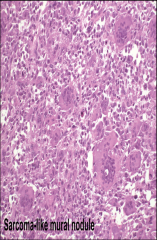
when do you see these
|
mucinous tumors - can have sarcomas (elderly, aggressive behavior) or sarcoma-like mural nodules (young, no impact on course, can be osteoclast-like giant cells, spindle cells or histiocytic)
|
|
|
pseudomyxoma peritoneum source
|
extraovarian, look at apx
|
|
|
keratins in helping with ddx for mucinous tumor in peritoneum
|
ck7+CK20+ mucinous ovary
CK7+CK20- other ovarian epithelial CK20+ colon/apx |
|
|
what does pseudomyx. peritonei usually spare
|
small intestine
|
|
|
what does borderline endometrial tumor look like
|
complex hyperplasia
|
|
|
fx of ovarian clear cell ca
|
Cells with abundant, pale, vacuolated cytoplasm
Hyaline cytoplasmic inclusions pleomorphic macronucleoli |
|
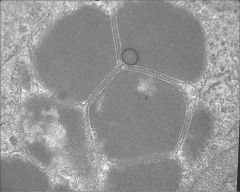
em of what
|
clear cell carcinoma, ovary
|
|
ovary
|
brenner tumor
groove nuclei/coffee bean borderline: like low grade papillary ue malignant: transitional - if classic brenner, then malignant otherwise transitional - TCC has worse prognosis |
|

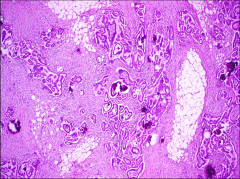
ovary, note some yellow color
|
granulosa cell tumor (malignant)
|
|
ovary
|
granulosa cell tumor; malignant, can have mets up to twenty years later
|
|
|
what in the ddx for granulosa cell tumor
|
sertoli leydig cell tumor
|
|
|
ihc for granulosa cell tumor
|
inhibin, CD99, maybe Ck but EMA-
|
|
|
significance of juvenile granulosa
|
no grooves, excellent prognosis, looks scary
|
|
ovary
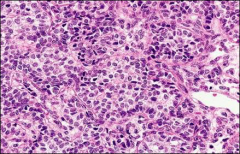
|
granulosa cell tumor
|
|
|
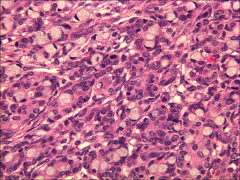
ovary
|
juvenile granulosa cell - scary, no grooves
|
|
ovary
|
juvenile granulosa cell tumor
|
|
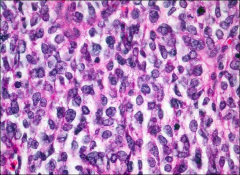
ovary
|
juvenile granulosa cell tumor
|
|

syndrome, ovary
|
meigs, fibroma (could have thecoma component - test with oil red o stain)
|
|
oil red o stain, ovary
|
looking for thecoma component in fibrothecoma
|
|
ovary
|
sertoli-leydig: Leydig cells have abundant eosinophilic or light pink cytoplasm. The Sertoli cells have a pale/clear cytoplasm
most typical is composed of tubules lined by Sertoli cells and interstitial clusters of Leydig cells. |
|
|
ihc in sertoli-leydig
|
inhibin-alpha
|
|
ovary, tumor type, what is shown
|
leydig cell tumor, reinke's crystals
|
|
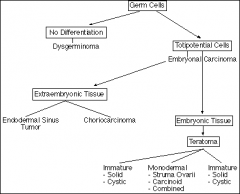
germ cell tumor chart
|
just for review
|
|
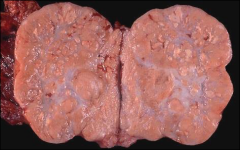
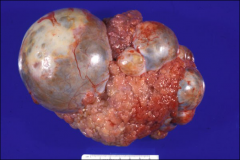
ovary, classic gross
|
cerebriform appearance, dysgerminoma/seminoma
|
|
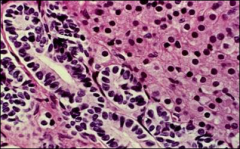
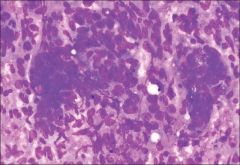
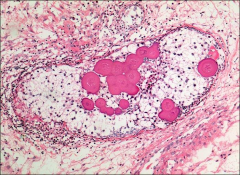
ovary
|
dysgerminoma
|
|
|
ihc for dysger
|
plap
|
|
|
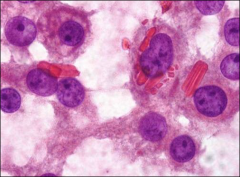
cytology for dysgerminoma
|
tigroid background, fragile
|
|
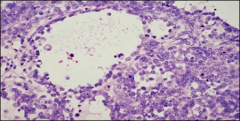
cytology
|
dysgerminoma, tigroid background
|
|
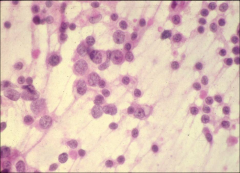
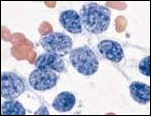
cytology, ovary
|
dysgerminoma, tigroid background
|
|
lace like reticular network, neoplasm, ovary
|
yolk sac
|
|
schillar duvall bodies
|
yolk sac tumor
|
|
ovary
|
yolk sac tumor
|
|
|
ihc yolk sac
|
afp
|
|
|
when pure yolk sac
|
young
|
|
|
when embryonal pue
|
really rare
|
|
ovary
|
embryonal - necrosis, epithelioid/glandular features
|
|
|
stains for embryonal
|
beta hcg, afp, keratin and CD30 (!)
|
|
what, ovary or testis
|
polyembryoma - yolk sac tumour and undifferentiated teratoma/embryonal carcinoma, with a characteristic finding of embryoid bodies lying in a loose mesenchymal stroma
|
|
|
associated syndrome - polyembryoma
|
klinefelters
|
|
|
what % of thyroid tissue is necessary to call struma ovarii
|
50%
|
|
|
what is struma ovarii assoc
|
pseudoMeigs - most common cause
|
|
|
what else do you see associated with ovarian teratomas (outside of thyroid)
|
carcinoids
|
|
what, peritoneum, associted with
|
gliomatosis peritonei, teratoma of ovary but not coming "from"
|
|
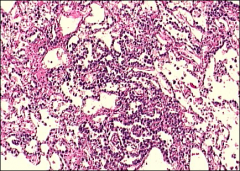
if this is a teratoma, what should you think
|
not likely benign, most common malignancy in IMMATURE teratoma; neuroectodermal component
in MATURE: scca |
|

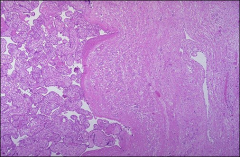
what, ovary
|
immature teratoma
|
|
what ovary/testis
|
immature teratoma
|
|
ovary/testis
|
immature teratoma
|
|
ovary, syndrome
|
gonadoblastoma - mixture of teratoma/sex cord stromal tumors
benign but propensity to malignant transformation |
|
ovary
|
gonadoblastoma, propensity for malignant transformation
|
|
|
what is a gynandroblastoma
|
mix of sex cord stromal tumors containing at least 10% of both male and female sex cord stromal elements (aka sertoli-leydig and granulosa cells)
|
|
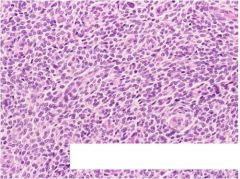
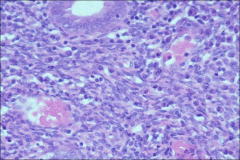
ovary, association, age clue
|
small cell carcinoma
hypercalcemia YOUNG (like 20s) if associated with hypercalcemia can be older if not hypercalcemic (postmenopausal) |
|
ovary
|
small cell carcinoma
|
|
|
hypercalcemia in malignancy
|
lung - squamous cell, clear cell
small cell carcinoma, young, ovary |
|
|
if get carcinosarcoma in ovary, what is the most common heterologous element
if get carcinosarcoma in uterus, what is the most common heterologous element |
in ovary: cartilage
in uterus: rhabdo component |
|
ovary
|
carcinosarcoma
|
|
ovary
|
krukenberg tumor, premenopausal, primary gastric/breast/gi tract, pancreas
often bilateral |
|
|
when see amnion nodusum
|
any cause of oligohydramnius
|
|
what, placenta
|
placenta accreta - no intervening endometrium
|
|
|
syncytiotrophoblastic proliferation in complete mole
|
all the way around the villi
|
|
|
where is scalloping seen partial or complete moles or both
|
partial
|

