![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
308 Cards in this Set
- Front
- Back
|
What diagnosis do you suspect in a patient with short limbs and normal sized head and torso (large relative to limbs)? |
Achondroplasia |
|
|
What type of bone growth is compromised in Achondroplasia? Why? |
- Failure of longitudinal bone growth (endochondral ossification) |
|
|
What causes Achondroplasia? |
- Constitutive activation of fibroblast growth factor receptor (FGFR3) |
|
|
How are the life span and fertility of a patient with Achondroplasia affected? |
Normal life span and fertility |
|
|
What type of bone is affected by Osteoporosis? What happens to it? |
Trabecular (spongy) bone loses mass and interconnections, despite normal bone mineralization and lab values (serum Ca2+ and PO4(3-)) |
|
|
What are the typical lab values for serum Ca2+ and PO4(3-) in patients with Osteoporosis? |
Ca2+ and PO4(3-) are normal |
|
|
How do you diagnose Osteoporosis? |
Bone Mineral Density test (DEXA scan) with a T-score of ≤ -2.5 |
|
|
What can cause Osteoporosis? |
- Long-term exogenous steroid use |
|
|
What are some of the potential consequences of Osteoporosis? |
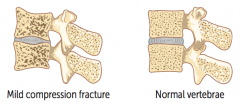
Vertebral crush fractures: |
|
|
What are the two types of Osteoporosis? |
- Type 1: post-menopausal |
|
|
What causes Type 1 Osteoporosis? Complications? |
- Post-menopausal: ↑ bone resorption due to ↓ estrogen levels |
|
|
What causes Type 2 Osteoporosis? Treatment? |
- Senile osteoporosis: affects men and women >70 years old |
|
|
Which disease is also known as Marble Bone Disease? |
Osteopetrosis |
|
|
What is wrong in Osteopetrosis? |
Failure of normal bone resorption due to defective osteoclasts → thickened dense bones that are prone to fracture |
|
|
What is the name for thickened bones due to failure of bone resorption? Consequences? |
Osteopetrosis (marble bone disease) |
|
|
What can cause Osteopetrosis? |
Mutations (eg, carbonic anhydrase II) impair ability of osteoclast to generate acidic environment necessary for bone resorption |
|
|
What is the appearance of Osteopetrosis on an x-ray? |

- Bone-in-bone appearance |
|
|
How do you treat a patient with Osteopetrosis? |
Bone marrow transplant is potentially curative because osteoclasts are derived from monocytes; the problem is defective osteoclasts |
|
|
What are the names of the diseases caused by a Vitamin D deficiency? |
- Osteomalacia in adults |
|
|
What causes osteomalacia (adults) and rickets (children)? Implications? |
Vitamin D deficiency |
|
|
What is the implication of osteoblast hyperactivity in Osteomalacia / Rickets? |
Increased Alkaline Phosphatase (ALP) because osteoblasts require an alkaline environment |
|
|
What disorder is characterized by increase in both osteoblastic and osteoclastic activity? |
Paget Disease of Bone (Osteitis Deformans) |
|
|
What are labs found in Paget Disease of Bone (Osteitis Deformans)? |
- Serum Ca2+, Phosphorus, and PTH are all normal |
|
|
What is the appearance of bone in Paget Disease of Bone (Osteitis Deformans)? |
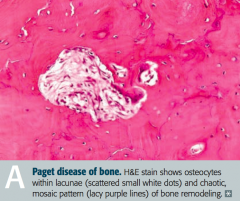
Mosaic pattern of women and lamellar bone |
|
|
What are the potential complications of Paget Disease of Bone (Osteitis Deformans)? |
- Long bone chalk-stick fractures |
|
|
In what disease is there a characteristic "increase in hat size"? Why? |
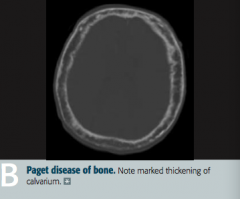
Paget Disease of Bone (Osteitis Deformans) |
|
|
What are the stages of Paget Disease? Which cells are active during these stages? |
- Lytic: osteoclasts |
|
|
What can cause Osteonecrosis (avascular necrosis)? |
Infarction of bone and marrow |
|
|
What happens in Osteonecrosis? Most common location? Why? |
- Infarction of bone and marrow, usually very painful |
|
|
In which bone disorders are the serum Ca2+, PO4(3-), ALP, and PTH all normal? Implications? |
- Osteoporosis → ↓ bone mass |
|
|
In which bone disorders are the serum Ca2+, PO4(3-), and PTH all normal, but with an elevated ALP? Implications? |
Paget Disease → abnormal mosaic bone architecture |
|
|
In which bone disorders are the serum Ca2+ and PO4(3-) decreased, but the ALP and PTH are elevated? Implications? |
Osteomalacia / Rickets → soft bones |
|
|
In which bone disorders are the serum Ca2+ and PO4(3-) increased, with a normal ALP, and decreased PTH? Implications? |
Hypervitaminosis D (caused by over-supplementation or granulomatous disease, such as sarcoidosis) |
|
|
In which bone disorders are the ALP and PTH elevated, with opposite levels of Ca2+ and PO4(3-)? |
Osteitis Fibrosa Cystica |
|
|
What are "brown tumors"? |
- Bone lesion that arises in settings of excess osteoclast activity, such as hyperparathyroidism |
|
|
What are causes of 1° hyperparathyroidism? |
- Idiopathic or parathyroid hyperplasia |
|
|
2° hyperparathyroidism is often a compensation for what? |
End-Stage Renal Disease / ESRD |
|
|
What are the types of benign primary bone tumors? |

- Giant cell tumor |
|
|
What is the most common benign bone tumor? Who is most likely to get this type of tumor? |

Osteochondroma - males <25 years old especially |
|

What type of bone tumor should you expect in a young patient, if present in the epiphyseal end of long bones, with a "soap bubble" appearance on x-ray? Characteristics? |

Giant Cell Tumor |
|
|
What type of bone tumor should you expect in a male <25 years that appears as an outgrowth from mature bone with a cartilaginous cap? Characteristics? |

Osteochondroma (Exostosis) |
|
|
What are the types of malignant primary bone tumors? |
- Osteosarcoma (osteogenic sarcoma) |
|
|
What are the most common 1° malignant bone tumors? |
1. Multiple Myeloma |
|
|
What are the most likely malignant bone cancers by age? |
- Boy < 15 years: Ewing Sarcoma |
|
|
What are the most common locations for the different malignant bone tumors? |
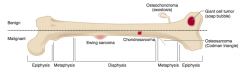
- Osteosarcoma: metaphysis of long bones, often around knee |
|
|
Which type of bone pathology is associated with an elevation of the periosterum? What is the term for this? |
Osteosarcoma |
|
|
Which type of bone pathology is associated with a "sunburst pattern" on x-ray? |
Osteosarcoma |
|
|
What are the predisposing factors for Osteosarcoma? |
- Paget disease of bone |
|
|
How do you treat Osteosarcoma? |
Surgical en block resection (with limb salvage) and chemotherapy |
|
|
Which bone pathology has an "onion skin" appearance? |
Ewing Sarcoma |
|
Which bone pathology is associated with anaplastic, malignant small blue cells? |
Ewing Sarcoma |
|
|
Which genetic change is associated with Ewing Sarcoma? |
t(11;22) translocation |
|
|
How do you treat Ewing Sarcoma? |
Chemotherapy (responsive) |
|
|
Which bone pathology typically appears as an expansile glistening mass within the medullary cavity? |
Chondrosarcoma |
|
|
What are the characteristics of Osteosarcoma (when is it more common? predisposing factors? location? signs on labs/imaging? treatment?) |
- 2nd most common 1° malignant bone tumor |
|
|
What are the characteristics of Ewing Sarcoma (when is it more common? predisposing factors? location? signs on labs/imaging? treatment? other?) |
- Boys < 15 years old |
|
|
What are the characteristics of Chondrosarcoma (when is it more common? location? signs on labs/imaging? other?) |
- Men 30-60 years old |
|
|
What is the cause of Osteoarthritis vs Rheumatoid Arthritis? |
- OA: mechanical - joint wear and tear destroys articular cartilage |
|
|
What are the findings in joints with Osteoarthritis vs Rheumatoid Arthritis? |
- OA: subchondral cysts, sclerosis, osteophytes (bone spurs), eburnation (polished, ivory-like appearance), Heberden nodes (DIP), and Bouchard nodes (PIP); no MCP involvement |
|
|
What joints are classically affected by Osteoarthritis vs Rheumatoid Arthritis? |
- OA: DIP and PIP (no MCP); weight-bearing joints |
|
|
What are the predisposing factors for Osteoarthritis vs Rheumatoid Arthritis? |
- OA: age, obesity, joint deformity, trauma |
|
|
What is the classic presentation of Osteoarthritis vs Rheumatoid Arthritis? |
- OA: pain in weight-bearing joints after use (eg, at end of day), improves with rest; knee cartilage loss begins medially (bowlegged); non-inflammatory; no systemic symptoms |
|
|
What is the treatment for Osteoarthritis vs Rheumatoid Arthritis? |
- OA: NSAIDs, intra-articular glucocorticoids |
|
|
Which type of bone pathology is associated with subchondral cysts? |
Osteoarthritis |
|
|
Which type of bone pathology is associated with sclerosis? |
Osteoarthritis |
|
|
Which type of bone pathology is associated with pannus formation in the joints (MCP, PIP)? |
Rheumatoid Arthritis |
|
|
Which type of bone pathology is associated with osteophytes (bone spurs)? |
Osteoarthritis |
|
|
Which type of bone pathology is associated with ulnar deviation of the fingers? |
Rheumatoid Arthritis |
|
|
Which type of bone pathology is associated with subluxation? |
Rheumatoid Arthritis |
|
|
Which type of bone pathology is associated with eburnation? What does this term mean? |
Osteoarthritis - eburnation means polished, ivory-like appearance of the bone |
|
|
Which type of bone pathology is associated with Baker cysts? Location? |
Rheumatoid Arthritis - Baker cysts in popliteal fossa |
|
|
Which type of bone pathology is associated with Heberden nodes and Bouchard nodes? Location? |
Osteoarthritis |
|
|
What type of antibodies are associated with Rheumatoid Arthritis? Which is more specific? |
- Rheumatoid Factor (anti-IgG antibody) |
|
|
What HLA is Rheumatoid Arthritis associated with? |
HLA-DR4 |
|
|
Which type of arthritis has pain in the weight bearing joints after use (eg, at the end of the day)? |
Osteoarthritis |
|
|
Which type of arthritis has morning stiffness lasting >30 minutes that improves with use? |
Rheumatoid Arthritis |
|
|
Which type of arthritis has cartilage loss that begins medially? |
Osteoarthritis |
|
|
How do you treat Osteoarthritis? |
- NSAIDs |
|
|
How do you treat Rheumatoid Arthritis? |
- NSAIDs |
|
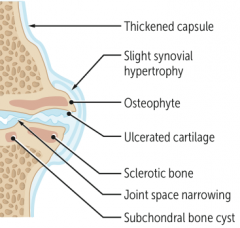
What type of arthritis has these features? |
Osteoarthritis |
|
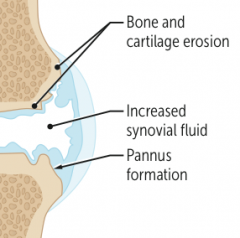
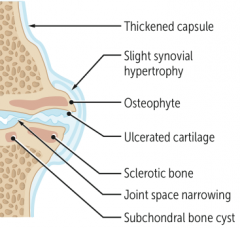
What type of arthritis has these features? |
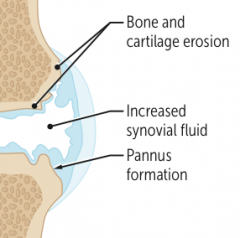
Rheumatoid Arthritis |
|

What type of arthritis has this appearance? |

Osteoarthritis |
|

What type of arthritis has this appearance? |

Rheumatoid Arthritis |
|
|
What disorder causes destruction of exocrine glands via an auto-immune process? Which glands are especially affected? |
Sjögren Syndrome |
|
|
Which disorder causes xerophthalmia, xerostomia, and bilateral parotid gland enlargement? What do these terms mean? |
Sjögren Syndrome |
|
|
What is the term for decreased tear production and subsequent corneal damage? |
Xerophthalmia |
|
|
What is the term for decreased saliva production? |
Xerostomia |
|
|
What antibodies are seen in Sjögren Syndrome? |
Anti-nuclear antibodies: SS-A (anti-Ro) and/or SS-B (anti-La) |
|
|
What can cause Sjögren Syndrome? |
- Can be primary |
|
|
What are the potential consequences of Sjögren Syndrome? |
- Dental caries |
|
|
What are the findings of Sjögren Syndrome? |
- Xerophthalmia (↓ tear production and subsequent corneal damage) |
|
|
What are the characteristic findings of gout? |
Acute inflammatory monoarthritis |
|
|
What causes gout? |
Precipitation of monosodium urate crystals in joints |
|
|
What can cause underexcretion of uric acid? How often is this the cause of gout? |
- Largely idiopathic |
|
|
What can cause overproduction of uric acid? How often is this the cause of gout? |
- Lesch-Nyhan syndrome |
|
|
What is the characteristic of the monosodium urate crystals found in gout? |
- Needle shaped |
|
|
How does gout typically present? |

- Asymmetric joint distribution (typically a monoarthritis) |
|
|
What are tophi? Where do they form? |
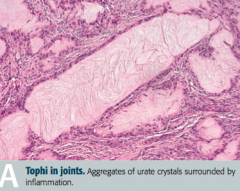
Tophus (deposit of crystalline uric acid and other substances at the surface of joints or in skin or cartilage) |
|
|
When do acute attacks of gout often occur? Why? |
- After a large meal |
|
|
What are the treatments for acute attacks of gout? |
- NSAIDs (eg, indomethacin) |
|
|
What are the chronic preventive treatments for gout? |
Xanthine oxidase inhibitors (Allopurinal and Febuxostat) |
|
|
What is the mechanism of Allopurinol and Febuxostat? Uses? |
Xanthine Oxidase inhibitors - used for chronic / preventative treatment of gout |
|
|
What kind of crystals cause pseudogout? |
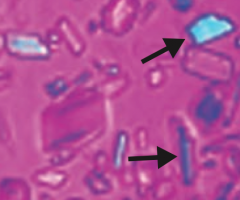
Calcium pyrophosphate crystals - basophilic, rhomboid crystals that are weakly birefringent (blue when parallel to light) |
|
|
What is the typical presentation of pseudogout? Who is more often affected? |
- Pain and effusion in joint |
|
|
What diseases are associated with pseudogout? |
- Hemochromatosis |
|
|
How does pseudogout appear on x-ray? |
Chondrocalcinosis - calcium pyrophosphate cyrstals within joint space |
|
|
How do you treat pseudogout? |
- NSAIDS for sudden, severe attacks |
|
|
How do gout and pseudogout compare in terms of the birefringence of their crystals? |
- Gout: crystals are yellow when parallel to light |
|
|
What are the most common causes of infectious arthritis? |
- S. aureus |
|
|
In a sexually active patient, with asymmetric migratory arthritis, what should you consider as a cause? |
Neisseria gonorrhoeae: gonococcal arthritis (STD) |
|
|
What are the characteristics of infectious arthritis? |
Joint is swollen, red, and painful |
|
|
What are the specific signs of Gonococcal Arthritis? |
STD: |
|
|
What is the term for arthritis without rheumatoid factor (anti-IgG Ab)? What is it associated with? |
Seronegative Spondyloarthropathies: |
|
|
What are the types of Seronegative Spondyloarthropathies? |
PAIR: |
|
|
What are the characteristics of arthritis in a patient with psoriasis? |

- Joint pain and stiffness |
|
|
How common is arthritis in patients with psoriasis? |
1/3 of patients with psoriasis |
|
|
What is the name of the chronic inflammatory disease of the spine and sacroiliac joints? Implications? |
Ankylosing Spondylitis |
|

In what condition do you see "bamboo spine"? Cause? |

Ankylosing spondylitis |
|
|
What are the characteristics of arthritis in patients with Inflammatory Bowel Disease? |
Crohn disease and ulcerative colitis are often accompanied by ankylosing spondylitis or peripheral arthritis |
|
|
What is the classic triad of findings in Reactive Arthritis (Reiter Syndrome)? |
"Can't see, can't pee, can't bend my knee": |
|
|
What is Reactive Arthritis (Reiter Syndrome) in response to? |
Post-GI (Shigella, Salmonella, Yersinia, Campylobacter) or Chlamydia infections |
|
|
What disease has the classic presentation of rash, joint pain, and fever? |
Systemic Lupus Erythematosus |
|
|
What mnemonic can help you remember the characteristics of Systemic Lupus Erythematosus? |
RASH OR PAIN: |
|
|
What are the common causes of death in patients with Systemic Lupus Erythematosus? |
- Cardiovascular disease |
|
|
What kind of cardiac disease is associated with Systemic Lupus Erythematosus? |
Libman-Sacks Endocarditis: wart-like vegetations on boths ides of valve |
|
|
What kind of renal disease is associated with Systemic Lupus Erythematosus? |
Lupus Nephritis (Type III hypersensitivity reaction): |
|
|
What kinds of antibodies are associated with Systemic Lupus Erythematosus? |
- Anti-nuclear antibodies (ANA) |
|
|
What antibody is sensitive, but not specific for Systemic Lupus Erythematosus? |
Anti-nuclear antibodies (ANA) |
|
|
What antibody is specific and indicates a poor prognosis (renal disease) for Systemic Lupus Erythematosus? |
Anti-dsDNA antibodies |
|
|
What antibody is specific, but does not offer prognostic information? |
Anti-Smith antibodies (directed against snRNPs) |
|
|
What antibody is sensitive for drug-induced lupus? |
Anti-histone antibodies |
|
|
What antibody shows false positives for patients with syphilis and prolongs the PTT in patients with Systemic Lupus Erythematosus? Implications? |
Anti-Cardiolipin antibody |
|
|
What antibody increases the risk of arteriovenous thromboembolism? |
Anti-cardiolipin antibodies |
|
|
How is complement affected in Systemic Lupus Erythematosus? |
Decreased C3, C4, and CH50 due to immune complex formation |
|
|
How do you treat patients with Systemic Lupus Erythematosus? |
- NSAIDs |
|
|
What mnemonic can help you remember the characteristics of Systemic Lupus Erythematosus? |
RASH OR PAIN: |
|
|
What disease is characterized by immune-mediated, widespread non-caseating granulomas and elevated serum ACE levels? |
Sarcoidosis |
|
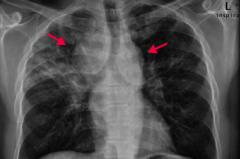
If your patient is a black female with enlarged lymph nodes and bilateral hilar adenopathy or reticular opacities incidentally found on CXR, what diagnosis should you consider? Why? |
Sarcoidosis |
|
|
What is sarcoidosis associated with? |
- Restrictive lung disease (interstitial fibrosis) |
|
|
What are the characteristics of the granulomas in Sarcoidosis? |
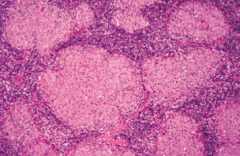
- Non-caseating |
|
|
What electrolyte abnormality is associated with sarcoidosis? Cause? |
Hypercalcemia - due to ↑ 1α-hydroxylase-mediated Vitamin D activation in macrophages |
|
|
How do you treat sarcoidosis? |
Steroids |
|
|
What are the characteristics of Sarcoidosis? |
- Immune-mediated, widespread non-caseating granulomas |
|
|
What diagnosis should you consider in a patient with pain and stiffness in their shoulders and hips, with fever, malaise, and weight loss? |
Polymyalgia Rheumatica |
|
|
What symptoms occur in patients with Polymyalgia Rheumatica? |
- Pain and stiffness in shoulders and hips |
|
|
Who is more likely to have Polymyalgia Rheumatica? |
- More common in women >50 years old |
|
|
What are the lab findings in a patient with Polymyalgia Rheumatica? |
- ↑ ESR |
|
|
How do you treat a patient with Polymyalgia Rheumatica? |
Rapid response to low-doe corticosteroids |
|
|
Which disease is most commonly seen in females 20-50 years old with chronic widespread musculoskeletal pain, stiffness, paresthesias, poor sleep, and fatigue? How should you treat? |
Fibromyalgia |
|
|
What are the symptoms of Fibromyalgia? |
- Chronic, widespread musculoskeletal pain |
|
|
How do you treat Fibromyalgia? |
- Regular exercise |
|
|
What is the cause of progressive symmetric proximal muscle weakness, characterized by endomysial inflammation with CD8+ T cells? Most common location? |
Polymyositis - most often involves shoulders |
|
|
What disease can cause present similarly to polymyositis (progressive symmetric proximal muscle weakness) with the addition of malar rash (similar to SLE), Gottron papules (on knuckles), heliotrope (erythematous periorbital) rash, "shawl and face" rash, and/or "mechanic's hands" appearance? What type of inflammation causes this presentation? |

Dermatomyositis: perimysial inflammation and atrophy with CD4+ T cells |
|
|
How does Polymyositis compare to Dermatomyositis in terms of location of symptoms? |

- Polymyositis: symmetric, progressive, proximal muscle weakness, especially in shoulders |
|
|
What type of inflammation is responsible for Polymyositis and Dermatomyositis? |
- Polymyositis: endomysial inflammation with CD8+ T cells |
|
|
What lab findings are associated with polymyositis and dermatomyositis? |
- ↑ CK |
|
|
How do you treat a patient with polymyositis or dermatomyositis? |
Steroids |
|
|
What is the most common neuromuscular junction disorder? |
Myasthenia Gravis |
|
|
What is the pathophysiology responsible for Myasthenia Gravis? |
Auto-Abs to post-synaptic ACh receptor |
|
|
What are the symptoms of Myasthenia Gravis? |
- Ptosis |
|
|
What is Myasthenia Gravis associated with? |
- Thymoma |
|
|
How do you treat Myasthenia Gravis? |
AChE Inhibitor - reverses symptoms |
|
|
Which neuromuscular junction disease is more rare than Myasthenia Gravis? |
Lambert-Eaton Myasthenic Syndrome |
|
|
What is the pathophysiologic cause of Lambert-Eaton Myasthenic Syndrome? |
Auto-antibodies to presynaptic Ca2+ channels → ↓ ACh release |
|
|
What are the symptoms of Lambert-Eaton Myasthenic Syndrome? |
- Proximal muscle weakness |
|
|
What is Lambert-Eaton Myasthenic Syndrome associated with? |
Small cell lung cancer |
|
|
What is the effect of AChE inhibitors in patients with Lambert-Eaton Myasthenic Syndrome? |
Minimal effect |
|
|
What are the two neuromuscular junction diseases and how do they compare in terms of the cause? |
- Myasthenia Gravis: auto-Abs to post-synaptic ACh receptor |
|
|
What are the two neuromuscular junction diseases and how do they compare in terms of the symptoms they cause? |
- Myasthenia Gravis: ptosis, diplopia, weakness, worsens with muscle use |
|
|
What are the two neuromuscular junction diseases and how do they compare in terms of associated conditions? |
- Myasthenia Gravis: thymoma, thymic hyperplasia |
|
|
If a patient has a suspicious "mass" at a site of trauma to their bone/muscle, what should you think of? |
Myositis Ossificans: metaplasia of skeletal muscle to bone (muscle becomes calcified) following muscular trauma |
|
|
Where is Myositis Ossificans more commonly found? |
Most often in upper or lower extremity |
|
|
What are the clinical findings in a patient with Myositis Ossificans? |

May present as a suspicious mass at a site of known trauma or as incidental finding on radiography |
|

What diagnosis should you consider in a patient with puffy and taut skin with an absence of wrinkles? Cause? |

Scleroderma (systemic sclerosis): excessive fibrosis and collagen deposition throughout the body |
|
|
Sclerosis can affect what organs? |
- Skin |
|
|
Who is more commonly affected by Scleroderma? |
Females (75%) |
|
|
What are the two types of Scleroderma (systemic sclerosis)? |
- Diffuse Scleroderma |
|
|
What are the symptoms of diffuse scleroderma? Cause? |
- Widespread skin involvement, rapid progression |
|
|
What are the symptoms of limited scleroderma? Cause? |
- Limited skin involvement confined to fingers and face |
|
|
Which antibodies are associated with the two types of Scleroderma? |
- Diffuse Scleroderma: anti-DNA topoisomerase I antibody |
|
|
What are the symptoms of CREST involvement? What is it associated with? |
CREST: |
|

What type of lesion is this? Characteristics? Other examples? |

Macule |
|

What type of lesion is this? Characteristics? Other examples? |

Patch |
|

What type of lesion is this? Characteristics? Other examples? |

Papule |
|

What type of lesion is this? Characteristics? Other examples? |

Plaque |
|

What type of lesion is this? Characteristics? Other examples? |

Vesicle |
|

What type of lesion is this? Characteristics? Other examples? |

Bulla |
|

What type of lesion is this? Characteristics? Other examples? |

Pustule |
|

What type of lesion is this? Characteristics? Other examples? |

Wheal |
|

What type of lesion is this? Characteristics? Other examples? |

Scale |
|

What type of lesion is this? Characteristics? Other examples? |

Crust |
|
|
What are the microscopic dermatologic term? |
- Hyperkeratosis |
|
|
What lesion causes an increased thickness of the stratum corneum? Example? |
Hyperkeratosis - eg, psoriasis or calluses |
|
|
What lesion causes hyperkeratosis with retention of nuclei in the stratum corneum? Example? |
Parakeratosis - eg, psoriasis |
|
|
What lesion causes an epidermal accumulation of edematous fluid in the intercellular spaces? Example? |
Spongiosis - eg, eczematous dermatitis |
|
|
What lesion causes separation of epidermal cells? Example? |
Acantholysis - eg, pemphigus vulgaris |
|
|
What lesion causes epidermal hyperplasia (↑ spinosum)? Example? |
Acanthosis - eg, acanthosis nigricans |
|
|
What are the characteristics of hyperkeratosis? Examples? |
Increased thickness of the startum corneum |
|
|
What are the characteristics of parakeratosis? Examples? |
Hyperkeratosis (↑ thickness of stratum corneum) with retention of nuclei in stratum corneum |
|
|
What are the characteristics of spongiosis? Examples? |
Epidermal accumulation of edematous fluid in intercellular spaces |
|
|
What are the characteristics of acantholysis? Examples? |
Separation of epidermal cells |
|
|
What are the characteristics of acanthosis? Examples? |
Epidermal hyperplasia (↑ spinosum) |
|
|
What are the types of pigmented skin disorders? |
- Albinism |
|
|
What disorder has a normal melanocyte number with ↓ melanin production? Cause? |

Albinism |
|
|
What causes Albinism? |
- Due to ↓ tyrosinase activity or defective tyrosine transport |
|
|
What is albinism associated with increased risk of? |
Skin cancer |
|

What disorder causes hyperpigmentation associated with pregnancy or OCP use? |

Melasma (Chloasma |
|

What disorder causes irregular areas of complete depigmentation? Cause? |

Vitiligo |
|
|
What are the common skin disorders? |
- Verrucae |
|

Which common skin disorder causes soft, tan-colored, cauliflower-like papules? Cause? |

Verrucae / warts - caused by HPV |
|
|
Which common skin disorder causes epidermal hyperplasia, hyperkeratosis, and koilocytosis? |
Verrucae / warts |
|

Which common skin disorder causes condyloma acuminatum on genitals? Cause? |

Verrucae / warts (caused by HPV) |
|

What common skin finding is this? |

Melanocytic Nevus - intradermal nevi are papular |
|

What common skin finding is this? |

Melanocytic Nevus - junctional nevi are flat macules |
|
|
What can melanocytic nevi lead to? |
They are benign, but melanoma can arise in congenital or atypical moles |
|

What common skin finding is this? Cause? |

Urticaria / hives - pruritic wheals form after mast cell degranulation |
|
|
How is urticaria characterized? |

Superficial dermal edema and lymphatic channel dilation, leading to pruritic wheals |
|

What common skin finding is this? Cause? |

Ephelis - freckles |
|

What common skin finding is this? Cause? |

Atopic Dermatitis (Eczema) |
|
|
What is the other name for Atopic Dermatitis? What is it associated with? |
Eczema |
|
|
What is the typical location of Atopic Dermatitis (Eczema)? |

- Usually starts on face in infancy (G) |
|

What common skin finding is this? Cause? |

Atopic Dermatitis (Eczema) |
|

What common skin finding is this? Cause? |

Allergic Contact Dermatitis |
|

What common skin finding is this? Cause? |

Allergic Contact Dermatitis |
|
|
What are common allergens that cause allergic contact dermatitis? What type of reaction? |
- Nickel |
|

What common skin finding causes papules and plaques with silver scaling, especially on the knees and elbows? |

Psoriasis |
|

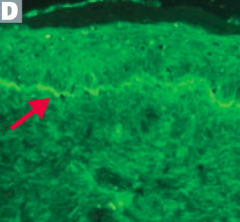
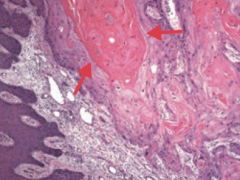
What common skin finding is this? What sign is this arrow pointing at? |

Psoriasis |
|
|
What are the skin findings in psoriasis? |
- Papules and plaques with silvery scaling (K), especially on knees and elbows |
|

What common skin finding appears as a flat, greasy, pigmented squamous epithelial proliferation with keratin-filled cysts and has an appearance of being "stuck on"? Cause? Where do these lesions occur? |

Seborrheic Keratosis |
|

What common skin finding appears as a flat, greasy, pigmented squamous epithelial proliferation with keratin-filled cysts and has an appearance of being "stuck on"? Cause? Where do these lesions occur? |

Seborrheic Keratosis |
|

What common skin finding appears as a flat, greasy, pigmented squamous epithelial proliferation with keratin-filled cysts and has an appearance of being "stuck on"? Cause? Where do these lesions occur? |

Seborrheic Keratosis |
|
|
What is a common benign neoplasm of older persons? |

Seborrheic Keratosis |
|

What is the name of the sign for the sudden appearance of multiple seborrheic keratoses? What does this indicate? |

Leser-Trélat Sign: indicates an underlying malignancy (eg, GI, lymphoid) |
|
|
What are the types of infectious skin disorders? |
- Impetigo |
|

What skin disorder is characterized by "honey-colored crusting"? Most common causes? |

Impetigo |
|
|
What kind of infection is Impetigo? Characteristics? |

- Very superficial skin infection |
|

What skin disorder is this? Most common causes? |

Bullous Impetigo - has bullae and is usually caused by S. aureus |
|

What skin disorder is this? Most common causes? |

Cellulitis |
|
|
What often precipitates a Cellulitis infection? |

Often starts with a break in the skin from trauma or another infection |
|

What skin disorder causes bullae and a purple color to the skin? Most common causes? |

Necrotizing Fasciitis |
|

What does Necrotizing Fasciitis lead to? |

Results in crepitus from methane and CO2 production |
|

What skin disorder causes fever and generalized erythematous rash with sloughing of the upper layers of the epidermis that heals completely? Cause? |

Staphylococcal Scalded Skin Syndrome |
|
|
What happens if a patient is exposed to a staphylococcal exotoxin that can destroy keratinocyte attachments to the stratum granulosum? |

Staphylococcal Scalded Skin Syndrome |
|

What skin disorder causes white, painless plaques on the tongue that cannot be scraped off? Most common cause? |

Hairy Leukoplakia |
|
|
Who gets Hairy Leukoplakia? Appearance? |

- Seen in HIV-positive patients with EBV |
|
|
What are the blistering skin disorders? |
- Pemphigus vulgaris |
|
|
What skin disorder is caused by IgG antibody against desmoglein (component of desmosomes)? |
Pemphigus Vulgaris |
|
|
What skin disorder is caused by IgG antibody against hemidesmosomes? |
Bullous Pemphigoid (think: antibodies are "BULLOW" the epidermis) |
|

Which skin disorder causes flaccid intraepidermal bullae and affects the oral mucosa? Cause? |

Pemphigus Vulgaris |
|
|
How can you diagnose Pemphigus Vulgaris? |
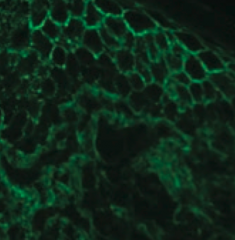
- Immunofluorescence reveals Abs (IgG against Desmoglein) against epidermal cells in a reticular (net-like) pattern |
|

Which skin disorder causes tense blisters on the skin but spares the oral mucosa? Cause? |

Bullous Pemphigoid |
|
|
How can you diagnose Bullous Pemphigoid? |
- Immunofluorescence reveals linear pattern at epidermal-dermal junction |
|

Which skin disorder causes pruritic papules, vesicles, and bullae (often on the elbows)? Cause / associations? |

Dermatitis Herpetiformis |
|
|
Which skin disorder is associated with infections, drugs , cancers, and auto-immune diseases? |
Erythema Multiforme |
|
|
What infections can cause Erythema Multiforme? |

- Mycoplasma pneumoniae |
|
|
What drugs can cause Erythema Multiforme? |
- Sulfa drugs |
|
|
What type of lesions are associated with Erythema Multiforme? |

- Macules |
|
|
What skin disorder is characterized by fever, bulla, necrosis, sloughing of skin, and a high mortality rate? |
Stevens Johnson Syndrome |
|
|
Are mucus membranes affected in Stevens Johnson Syndrome? |

Yes - typically at least 2 mucus membranes are involved |
|
|
In what skin disorders ma you see target lesions? |
- Erythema Multiforme |
|
|
What is the more severe form of Stevens Johnson Syndrome? How do you distinguish them? |

Toxic Epidermal Necrolysis |
|

Which skin disorder is associated with a hyperpigmented, velvety thickening of the skin? Cause? |

Acanthosis Nigricans |
|
|
What skin changes occur in Acanthosis Nigricans? |

Epidermal hyperplasia causes symmetrical, hyperpigmented, velvety thickening of skin, especially on neck or in axilla |
|

What premalignant lesion is caused by sun exposure, leading to a small, rough, erythamtous or brownish papule or plaque? What can it progress to? |
Actinic Keratosis: risk of squamous cell carcinoma is proportional to degree of epithelial dysplasia |
|
|
What is the appearance of the skin changes in Actinic Keratosis? |
Small, rough, erythematous or brownish papules or plaques |
|
|
What is there a risk of if you have Actinic Keratosis? What determines risk? |

Risk of squamous cell carcinoma is proportional to degree of epithelial dysplasia |
|

What is the skin disorder characterized by painful inflammatory lesions of the subcutaneous fat, usually on the anterior shins? Possible causes? |

Erythema Nodosum |
|
|
What is the appearance of Erythema Nodosum? |

Painful, inflammatory lesions of subcutaneous fat, usually on anterior shins |
|

What can cause Erythema Nodosum? |
- Often idiopathic |
|
|
Which skin disorder is associated with the 6 P's: pruritic, purple, polygonal planar papules and plaques? |

Lichen Planus |
|
|
Which skin disorder manifests as Wickham striae (reticular white lines) on mucosal surfaces? What is it associated with? |
Lichen Planus |
|
|
Which skin disorder is associated with a sawtooth infiltrate of lymphocytes at the dermal-epidermal junction? |
Lichen Planus |
|
|
What are the features of Lichen Planus? |

6 P's: |
|
|
Which skin disorder is known as a "Herald patch" followed days later by a "Christmas tree" distribution of plaques with a collarette scale? How long does this last? |

Pityriasis Rosea |
|

What is this finding? What is it a sign of? |

Herald Patch - sign of Pityriasis Rosea |
|

What is this finding? What is it a sign of? |

Christmas tree distribution - sign of Pityriasis Rosea |
|
|
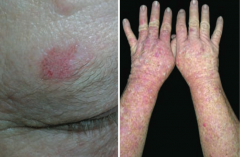
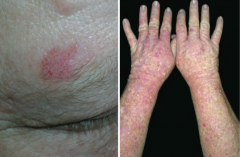
What causes a sunburn? |
Acute cutaneous inflammatory reaction due to excessive UV irradiation |
|
|
What is the mechanism of damage causing sunburn? |
Causes DNA mutations, inducing apoptosis of keratinocytes |
|
|
What are the types of UV rays? How do they differ in the skin changes they cause? |
- UVA: causes tanning and photoaging |
|
|
What are the potential complications of sunburns? |
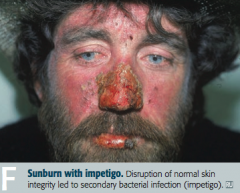
- Impetigo |
|
|
What are the types of skin cancers? |
- Basal cell carcinoma |
|
|
What is the most common skin cancer? |
Basal Cell Carcinoma |
|

What kind of skin lesion is this? Characteristic appearance? |

Basal Cell Carcinoma |
|

What kind of skin lesion is this? Characteristic appearance? |

Basal Cell Carcinoma |
|

What kind of skin lesion is this? Characteristic appearance? |

Basal Cell Carcinoma |
|
|
What is the classic histologic appearance of a Basal Cell Carcinoma? |
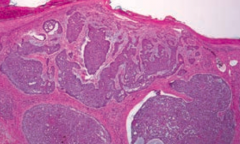
- Palisading nuclei |
|
|
Where are most Basal Cell Carcinomas located? |
Found in sun-exposed areas of body |
|
|
What is the prognosis of Basal Cell Carcinoma? |
Locally invasive, but almost never metastasizes |
|
|
How can Basal Cell Carcinomas appear? |

- Pink pearly nodules, commonly with telangiectasis, rolled borders, and central crusting or ulceration |
|
|
What is the second most common skin cancer? |
Squamous Cell Carcinoma |
|
|
What is Squamous Cell Carcinoma associated with? |
- Excessive exposure to sunlight |
|
|
What are the most common locations for Squamous Cell Carcinoma? |
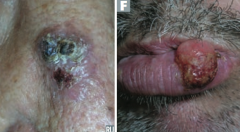
- Face |
|
|
What is the prognosis of Squamous Cell Carcinoma? |
Locally invasive, but may spread to lymph nodes and will rarely metastasize |
|
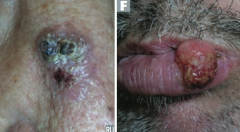
Which type of skin cancer causes ulcerative red lesions with frequent scales, and is associated with chronic draining sinuses? |
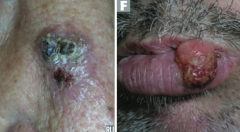
Squamous Cell Carcinoma |
|
|
What does Squamous Cell Carcinoma look like histologically? |
Keratin pearls |
|
|
What is the name of the scaly plaque, that is a precursor to Squamous Cell Carcinoma? |
Actinic Keratosis |
|
|
What is the name of the Squamous Cell Carcinoma variant that grows rapidly and may regress spontaneously? Timeline? |

Keratoacanthoma: grows rapidly over 4-6 weeks and regresses over months |
|
|
Which type of skin cancer has a significant risk for metastasis? What determine the risk of this? |
Melanoma - depth of tumor correlates with risk of metastasis |
|
|
What tumor marker is there for Melanoma? |
S-100 tumor marker |
|
|
What is Melanoma associated with? |
- Sunlight exposure |
|
|
What are the key things to look for when evaluating a patient you think may have a Melanoma? |
ABCDEs: |
|
|
What are the types of Melanoma? |

- Superficial spreading melanoma (I) |
|

What skin lesion is this? |

Superficial Spreading Melanoma |
|

What skin lesion is this? |

Nodular Melanoma |
|

What skin lesion is this? |

Lentigo Maligna Melanoma |
|

What skin lesion is this? |

Acrolentiginous Melanoma |
|
|
What genetic abnormality often drives melanoma? |
BRAF kinase activating mutation (V600E) |
|
|
How do you treat Melanoma? |
- Primary treatment: excision with appropriately wide margins |

