![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
308 Cards in this Set
- Front
- Back
|
What diagnosis do you suspect in a patient with short limbs and normal sized head and torso (large relative to limbs)?
|
Achondroplasia
|
|
|
What type of bone growth is compromised in Achondroplasia? Why?
|
- Failure of longitudinal bone growth (endochondral ossification)
- Membranous ossification is not affected - This is due to constitutive activation of fibroblast growth factor receptor (FGFR3) |
|
|
What causes Achondroplasia?
|
- Constitutive activation of fibroblast growth factor receptor (FGFR3)
- Inhibits chondrocyte proliferation - 85% of mutations occur sporadically and associated with advanced paternal age - Also associated with autosomal dominant inheritance |
|
|
How are the life span and fertility of a patient with Achondroplasia affected?
|
Normal life span and fertility
|
|
|
What type of bone is affected by Osteoporosis? What happens to it?
|
Trabecular (spongy) bone loses mass and interconnections, despite normal bone mineralization and lab values (serum Ca2+ and PO4(3-))
|
|
|
What are the typical lab values for serum Ca2+ and PO4(3-) in patients with Osteoporosis?
|
Ca2+ and PO4(3-) are normal
|
|
|
How do you diagnose Osteoporosis?
|
Bone Mineral Density test (DEXA scan) with a T-score of ≤ -2.5
|
|
|
What can cause Osteoporosis?
|
- Long-term exogenous steroid use
- Menopause: ↓ estrogen - Senile (>70 years) |
|
|
What are some of the potential consequences of Osteoporosis?
|
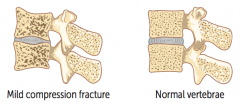
Vertebral crush fractures:
- Acute back pain - Loss of height - Kyphosis |
|
|
What are the two types of Osteoporosis?
|
- Type 1: post-menopausal
- Type 2: senile (men and women > 70 years) |
|
|
What causes Type 1 Osteoporosis? Complications?
|
- Post-menopausal: ↑ bone resorption due to ↓ estrogen levels
- Complications: femoral neck fracture, distal radius (Colles) fracture |
|
|
What causes Type 2 Osteoporosis? Treatment?
|
- Senile osteoporosis: affects men and women >70 years old
- Prophylaxis: regular weight-bearing exercise and adequate Ca2+ and Vitamin D intake throughout adulthood - Treatment: bisphosphanates, PTH, SERMs, rarely calcitonin; denosumab (monoclonal Ab against RANKL) |
|
|
Which disease is also known as Marble Bone Disease?
|
Osteopetrosis
|
|
|
What is wrong in Osteopetrosis?
|
Failure of normal bone resorption due to defective osteoclasts → thickened dense bones that are prone to fracture
|
|
|
What is the name for thickened bones due to failure of bone resorption? Consequences?
|
Osteopetrosis (marble bone disease)
- Prone to fracture - Pancytopenia and extramedullary hematopoiesis (bone fills BM space) - Cranial nerve impingement and palsies (narrowed foramina) |
|
|
What can cause Osteopetrosis?
|
Mutations (eg, carbonic anhydrase II) impair ability of osteoclast to generate acidic environment necessary for bone resorption
|
|
|
What is the appearance of Osteopetrosis on an x-ray?
|

- Bone-in-bone appearance
- Thickened, dense bones |
|
|
How do you treat a patient with Osteopetrosis?
|
Bone marrow transplant is potentially curative because osteoclasts are derived from monocytes; the problem is defective osteoclasts
|
|
|
What are the names of the diseases caused by a Vitamin D deficiency?
|
- Osteomalacia in adults
- Rickets in children |
|
|
What causes osteomalacia (adults) and rickets (children)? Implications?
|
Vitamin D deficiency
- Defective mineralization / calcification of osteoid → soft bones that bow out - ↓ Vitamin D → ↓ serum Ca2+ → ↑ PTH → ↓ serum PO4(3-) - Hyperactivity of osteoblasts → ↑ ALP (osteoblasts require alkaline environment) |
|
|
What is the implication of osteoblast hyperactivity in Osteomalacia / Rickets?
|
Increased Alkaline Phosphatase (ALP) because osteoblasts require an alkaline environment
|
|
|
What disorder is characterized by increase in both osteoblastic and osteoclastic activity?
|
Paget Disease of Bone (Osteitis Deformans)
|
|
|
What are labs found in Paget Disease of Bone (Osteitis Deformans)?
|
- Serum Ca2+, Phosphorus, and PTH are all normal
- ↑ ALP |
|
|
What is the appearance of bone in Paget Disease of Bone (Osteitis Deformans)?
|
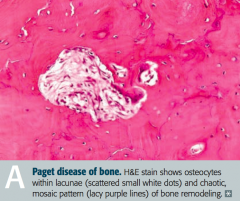
Mosaic pattern of women and lamellar bone
|
|
|
What are the potential complications of Paget Disease of Bone (Osteitis Deformans)?
|
- Long bone chalk-stick fractures
- ↑ Blood flow from ↑ AV shunts may cause high-output heart failure - ↑ Risk of Osteogenic Sarcoma - Hearing loss due to auditory foramen narrowing |
|
|
In what disease is there a characteristic "increase in hat size"? Why?
|
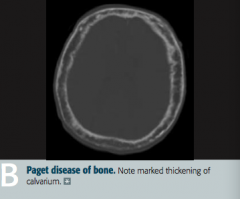
Paget Disease of Bone (Osteitis Deformans)
- Marked thickening of calvarium |
|
|
What are the stages of Paget Disease? Which cells are active during these stages?
|
- Lytic: osteoclasts
- Mixed: osteoclasts and osteoblasts - Sclerotic: osteoblasts - Quiescent: minimal osteoclast/osteoblast activity |
|
|
What can cause Osteonecrosis (avascular necrosis)?
|
Infarction of bone and marrow
- Trauma - High dose corticosteroids - Alcoholism - Sickle cell disease |
|
|
What happens in Osteonecrosis? Most common location? Why?
|
- Infarction of bone and marrow, usually very painful
- Most common site is femoral head (d/t insufficiency of medial circumflex femoral artery) |
|
|
In which bone disorders are the serum Ca2+, PO4(3-), ALP, and PTH all normal? Implications?
|
- Osteoporosis → ↓ bone mass
- Osteopetrosis → dense, brittle bones; Ca2+ ↓ in severe malignant disease |
|
|
In which bone disorders are the serum Ca2+, PO4(3-), and PTH all normal, but with an elevated ALP? Implications?
|
Paget Disease → abnormal mosaic bone architecture
|
|
|
In which bone disorders are the serum Ca2+ and PO4(3-) decreased, but the ALP and PTH are elevated? Implications?
|
Osteomalacia / Rickets → soft bones
|
|
|
In which bone disorders are the serum Ca2+ and PO4(3-) increased, with a normal ALP, and decreased PTH? Implications?
|
Hypervitaminosis D (caused by over-supplementation or granulomatous disease, such as sarcoidosis)
|
|
|
In which bone disorders are the ALP and PTH elevated, with opposite levels of Ca2+ and PO4(3-)?
|
Osteitis Fibrosa Cystica
- 1° Hyperparathyroidism: ↑ Ca2+ and ↓ PO4(3-) - 2° Hyperparathyroidism: ↓ Ca2+ and ↑ PO4(3-) |
|
|
What are "brown tumors"?
|
- Bone lesion that arises in settings of excess osteoclast activity, such as hyperparathyroidism
- It is not a true neoplasm, as the term "tumor" suggests; but, it may mimic a true neoplasm - Exhibits FIBROUS REPLACEMENT of bone, with SUBPERIOSTEAL THINNING |
|
|
What are causes of 1° hyperparathyroidism?
|
- Idiopathic or parathyroid hyperplasia
- Parathyroid adenoma - Parathyroid carcinoma |
|
|
2° hyperparathyroidism is often a compensation for what?
|
End-Stage Renal Disease / ESRD
- ↓ PO4(3-) excretion and production of activated vitamin D |
|
|
What are the types of benign primary bone tumors?
|

- Giant cell tumor
- Osteochondroma (exostosis) |
|
|
What is the most common benign bone tumor? Who is most likely to get this type of tumor?
|

Osteochondroma - males <25 years old especially
|
|

What type of bone tumor should you expect in a young patient, if present in the epiphyseal end of long bones, with a "soap bubble" appearance on x-ray? Characteristics?
|

Giant Cell Tumor
- Benign primary bone tumor - Locally aggressive, often around the knee - Multi-nucleated giant cells |
|
|
What type of bone tumor should you expect in a male <25 years that appears as an outgrowth from mature bone with a cartilaginous cap? Characteristics?
|

Osteochondroma (Exostosis)
- Most common benign tumor - Rarely transforms to chondrosarcoma |
|
|
What are the types of malignant primary bone tumors?
|
- Osteosarcoma (osteogenic sarcoma)
- Ewing sarcoma - Chondrosarcoma (Multiple Myeloma) |
|
|
What are the most common 1° malignant bone tumors?
|
1. Multiple Myeloma
2. Osteosarcoma (Osteogenic Sarcoma) |
|
|
What are the most likely malignant bone cancers by age?
|
- Boy < 15 years: Ewing Sarcoma
- 10-20 years: Osteosarcoma (1°) - 30-60 years: Chondrosarcoma - >65 years: Osteosarcoma (2°) |
|
|
What are the most common locations for the different malignant bone tumors?
|
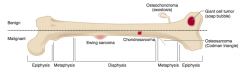
- Osteosarcoma: metaphysis of long bones, often around knee
- Ewing Sarcoma: diaphysis of long bones, pelvis, scapula, ribs - Chondrosarcoma: pelvis, spine, scapula, humerus, tibia, or femur |
|
|
Which type of bone pathology is associated with an elevation of the periosterum? What is the term for this?
|
Osteosarcoma
- Elevation of the periosterum = Codman Triangle |
|
|
Which type of bone pathology is associated with a "sunburst pattern" on x-ray?
|
Osteosarcoma
|
|
|
What are the predisposing factors for Osteosarcoma?
|
- Paget disease of bone
- Bone infarcts - Radiation - Familial retinoblastoma - Li-Fraumeni syndrome (germline p53 mutation) |
|
|
How do you treat Osteosarcoma?
|
Surgical en block resection (with limb salvage) and chemotherapy
|
|
|
Which bone pathology has an "onion skin" appearance?
|
Ewing Sarcoma
|
|
Which bone pathology is associated with anaplastic, malignant small blue cells?
|
Ewing Sarcoma
|
|
|
Which genetic change is associated with Ewing Sarcoma?
|
t(11;22) translocation
|
|
|
How do you treat Ewing Sarcoma?
|
Chemotherapy (responsive)
|
|
|
Which bone pathology typically appears as an expansile glistening mass within the medullary cavity?
|
Chondrosarcoma
|
|
|
What are the characteristics of Osteosarcoma (when is it more common? predisposing factors? location? signs on labs/imaging? treatment?)
|
- 2nd most common 1° malignant bone tumor
- Bimodal distribution: 10-20 years (1°) and >65 years (2°) - Predisposing factors: Paget disease of bone, bone infarcts, radiation, familial retinoblastoma, Li-Fraumeni syndrome (germline p53 mutation) - Location: metaphysis of long bones, often around knee - Signs: Codman triangle (from elevation of periosteum) or sunburnt pattern on x-ray - Treatment: aggressive, treat w/ surgical en bloc resection (w/ limb salvage) and chemotherapy |
|
|
What are the characteristics of Ewing Sarcoma (when is it more common? predisposing factors? location? signs on labs/imaging? treatment? other?)
|
- Boys < 15 years old
- Predisposing factors: t(11;22) translocation - Location: diaphysis of long bones, pelvis, scapula, ribs - Signs: anaplastic small blue cell malignant tumor, "onion skin" appearance in bone - Treatment: responsive to chemotherapy - Extremely aggressive w/ early metastases |
|
|
What are the characteristics of Chondrosarcoma (when is it more common? location? signs on labs/imaging? other?)
|
- Men 30-60 years old
- Location: usually in pelvis, spine, scapula, humerus, tibia, femur - Signs: expansile glistening mass within the medullary cavity - Rare, malignant, cartilaginous tumor - May be 1° origin or from osteochondroma |
|
|
What is the cause of Osteoarthritis vs Rheumatoid Arthritis?
|
- OA: mechanical - joint wear and tear destroys articular cartilage
- RA: auto-immune - inflammatory destruction of synovial joints; mediated by cytokines and type III and IV hypersensitivity reactions |
|
|
What are the findings in joints with Osteoarthritis vs Rheumatoid Arthritis?
|
- OA: subchondral cysts, sclerosis, osteophytes (bone spurs), eburnation (polished, ivory-like appearance), Heberden nodes (DIP), and Bouchard nodes (PIP); no MCP involvement
- RA: pannus formation in joints (MCP and PIP); subcutaneous rheumatoid nodules (fibrinoid necrosis), ulnar deviation of fingers, subluxation, Baker cyst (in popliteal fossa); no DIP involvement |
|
|
What joints are classically affected by Osteoarthritis vs Rheumatoid Arthritis?
|
- OA: DIP and PIP (no MCP); weight-bearing joints
- RA: MCP and PIP (no DIP) |
|
|
What are the predisposing factors for Osteoarthritis vs Rheumatoid Arthritis?
|
- OA: age, obesity, joint deformity, trauma
- RA: female, 80% are + for rheumatoid factor (anti-IgG Ab); anti-cyclic citrullinated peptide Ab is more specific; strongly associated with HLA-DR4 |
|
|
What is the classic presentation of Osteoarthritis vs Rheumatoid Arthritis?
|
- OA: pain in weight-bearing joints after use (eg, at end of day), improves with rest; knee cartilage loss begins medially (bowlegged); non-inflammatory; no systemic symptoms
- RA: morning stiffness >30 minutes improves with use; symmetric joint involvement; systemic symptoms (fever, fatigue, pleuritis, and pericarditis) |
|
|
What is the treatment for Osteoarthritis vs Rheumatoid Arthritis?
|
- OA: NSAIDs, intra-articular glucocorticoids
- RA: NSAIDs, glucocorticoids, disease-modifying agents (methotrexate, sulfasalazine, TNF-α inhibitors) |
|
|
Which type of bone pathology is associated with subchondral cysts?
|
Osteoarthritis
|
|
|
Which type of bone pathology is associated with sclerosis?
|
Osteoarthritis
|
|
|
Which type of bone pathology is associated with pannus formation in the joints (MCP, PIP)?
|
Rheumatoid Arthritis
|
|
|
Which type of bone pathology is associated with osteophytes (bone spurs)?
|
Osteoarthritis
|
|
|
Which type of bone pathology is associated with ulnar deviation of the fingers?
|
Rheumatoid Arthritis
|
|
|
Which type of bone pathology is associated with subluxation?
|
Rheumatoid Arthritis
|
|
|
Which type of bone pathology is associated with eburnation? What does this term mean?
|
Osteoarthritis - eburnation means polished, ivory-like appearance of the bone
|
|
|
Which type of bone pathology is associated with Baker cysts? Location?
|
Rheumatoid Arthritis - Baker cysts in popliteal fossa
|
|
|
Which type of bone pathology is associated with Heberden nodes and Bouchard nodes? Location?
|
Osteoarthritis
- Heberden nodes: DIP - Bouchard nodes: PIP |
|
|
What type of antibodies are associated with Rheumatoid Arthritis? Which is more specific?
|
- Rheumatoid Factor (anti-IgG antibody)
- Anti-cyclic citrullinated peptide antibody (more specific) |
|
|
What HLA is Rheumatoid Arthritis associated with?
|
HLA-DR4
|
|
|
Which type of arthritis has pain in the weight bearing joints after use (eg, at the end of the day)?
|
Osteoarthritis
|
|
|
Which type of arthritis has morning stiffness lasting >30 minutes that improves with use?
|
Rheumatoid Arthritis
|
|
|
Which type of arthritis has cartilage loss that begins medially?
|
Osteoarthritis
|
|
|
How do you treat Osteoarthritis?
|
- NSAIDs
- Intra-articular glucocorticoids |
|
|
How do you treat Rheumatoid Arthritis?
|
- NSAIDs
- Glucocorticoids - Disease-modifying agents: methotrexate, sulfasalazine, TNF-α inhibitors |
|
What type of arthritis has these features?
|
Osteoarthritis
|
|
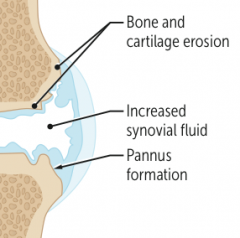
What type of arthritis has these features?
|
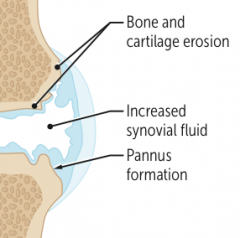
Rheumatoid Arthritis
|
|

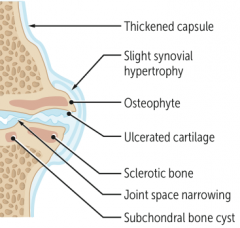
What type of arthritis has this appearance?
|

Osteoarthritis
- X-rays of the knee show joint space narrowing and sclerosis |
|

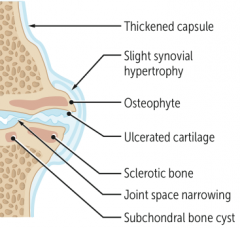
What type of arthritis has this appearance?
|

Rheumatoid Arthritis
- Note boutonnière deformities of PIP joints with ulnar deviation |
|
|
What disorder causes destruction of exocrine glands via an auto-immune process? Which glands are especially affected?
|
Sjögren Syndrome
- Especially affects lacrimal and salivary |
|
|
Which disorder causes xerophthalmia, xerostomia, and bilateral parotid gland enlargement? What do these terms mean?
|
Sjögren Syndrome
- Xerophthalmia: ↓ tear production and subsequent corneal damage - Xerostomia: ↓ saliva production |
|
|
What is the term for decreased tear production and subsequent corneal damage?
|
Xerophthalmia
|
|
|
What is the term for decreased saliva production?
|
Xerostomia
|
|
|
What antibodies are seen in Sjögren Syndrome?
|
Anti-nuclear antibodies: SS-A (anti-Ro) and/or SS-B (anti-La)
|
|
|
What can cause Sjögren Syndrome?
|
- Can be primary
- Can be secondary, associate with other auto-immune disorders (eg, rheumatoid arthritis) |
|
|
What are the potential consequences of Sjögren Syndrome?
|
- Dental caries
- Mucosa-associated lymphoid tissue (MALT) lymphoma (may present as unilateral parotid enlargement) |
|
|
What are the findings of Sjögren Syndrome?
|
- Xerophthalmia (↓ tear production and subsequent corneal damage)
- Xerostomia (↓ saliva production) - Presence of anti-nuclear antibodies: SS-A (anti-Ro) and/or SS-B (anti-La) - Bilateral parotid enlargement |
|
|
What are the characteristic findings of gout?
|
Acute inflammatory monoarthritis
|
|
|
What causes gout?
|
Precipitation of monosodium urate crystals in joints
Associated with hyperuricemia, which can be caused by: - Underexcretion of uric acid (90% of patients) - largely idiopathic, can be exacerbated by certain medications (eg, thiazide diuretics) - Overproduction of uric acid (10% of patients) - Lesch-Nyhan syndrome, PRPP excess, ↑ cell turnover (eg, tumor lysis syndrome), von Gierke disease |
|
|
What can cause underexcretion of uric acid? How often is this the cause of gout?
|
- Largely idiopathic
- Can be exacerbated by certain medications (eg, thiazide diuretics) - 90% of patients |
|
|
What can cause overproduction of uric acid? How often is this the cause of gout?
|
- Lesch-Nyhan syndrome
- PRPP excess - ↑ Cell turnover (eg, tumor lysis syndrome) - von Gierke disease - 10% of patients |
|
|
What is the characteristic of the monosodium urate crystals found in gout?
|
- Needle shaped
- Negatively birefringent (yellow under parallel light, blue under perpindicular light) |
|
|
How does gout typically present?
|

- Asymmetric joint distribution (typically a monoarthritis)
- Joint is swollen, red, and painful - Classically in the MTP joint of the big toe (podagra) - Tophus formation - Acute attacks tend to occur after a large meal or alcohol consumption |
|
|
What are tophi? Where do they form?
|
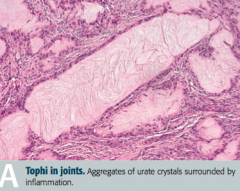
Tophus (deposit of crystalline uric acid and other substances at the surface of joints or in skin or cartilage)
- Often on external ear, olecranon bursa, or Achilles tendon |
|
|
When do acute attacks of gout often occur? Why?
|
- After a large meal
- After alcohol consumption: alcohol metabolites compete for same excretion sites in kidney as uric acid, causing ↓ uric acid secretion and subsequent buildup in blood |
|
|
What are the treatments for acute attacks of gout?
|
- NSAIDs (eg, indomethacin)
- Glucocorticoids - Colchicine |
|
|
What are the chronic preventive treatments for gout?
|
Xanthine oxidase inhibitors (Allopurinal and Febuxostat)
|
|
|
What is the mechanism of Allopurinol and Febuxostat? Uses?
|
Xanthine Oxidase inhibitors - used for chronic / preventative treatment of gout
|
|
|
What kind of crystals cause pseudogout?
|
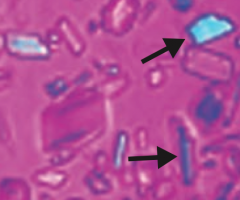
Calcium pyrophosphate crystals - basophilic, rhomboid crystals that are weakly birefringent (blue when parallel to light)
|
|
|
What is the typical presentation of pseudogout? Who is more often affected?
|
- Pain and effusion in joint
- Usually affects large joints (classically the knee) - >50 years old, both sexes affected equally |
|
|
What diseases are associated with pseudogout?
|
- Hemochromatosis
- Hyperparathyroidism - Hypoparathyroidism |
|
|
How does pseudogout appear on x-ray?
|
Chondrocalcinosis - calcium pyrophosphate cyrstals within joint space
|
|
|
How do you treat pseudogout?
|
- NSAIDS for sudden, severe attacks
- Steroids - Colchicine |
|
|
How do gout and pseudogout compare in terms of the birefringence of their crystals?
|
- Gout: crystals are yellow when parallel to light
- Pseudogout: crystals are blue when parallel to light |
|
|
What are the most common causes of infectious arthritis?
|
- S. aureus
- Streptococcus - Neisseria gonorrhoeae |
|
|
In a sexually active patient, with asymmetric migratory arthritis, what should you consider as a cause?
|
Neisseria gonorrhoeae: gonococcal arthritis (STD)
|
|
|
What are the characteristics of infectious arthritis?
|
Joint is swollen, red, and painful
|
|
|
What are the specific signs of Gonococcal Arthritis?
|
STD:
- Synovitis (eg, knee) - Tenosynovitis (eg, hand) - Dermatitis (eg, pustules) |
|
|
What is the term for arthritis without rheumatoid factor (anti-IgG Ab)? What is it associated with?
|
Seronegative Spondyloarthropathies:
- Strong association with HLA-B27 |
|
|
What are the types of Seronegative Spondyloarthropathies?
|
PAIR:
- Psoriatic arthritis - Ankylosing spondylitis - Inflammatory bowel disease - Reactive arthritis (Reiter syndrome) |
|
|
What are the characteristics of arthritis in a patient with psoriasis?
|

- Joint pain and stiffness
- Asymmetric and patchy involvement - Dactylitis ("sausage fingers") - "Pencil-in-cup" deformity on x-ray |
|
|
How common is arthritis in patients with psoriasis?
|
1/3 of patients with psoriasis
|
|
|
What is the name of the chronic inflammatory disease of the spine and sacroiliac joints? Implications?
|
Ankylosing Spondylitis
- Ankylosis (stiff spine d/t fusion of joints) - Uveitis - Aortic regurgitation |
|

In what condition do you see "bamboo spine"? Cause?
|

Ankylosing spondylitis
- Vertebral fusion |
|
|
What are the characteristics of arthritis in patients with Inflammatory Bowel Disease?
|
Crohn disease and ulcerative colitis are often accompanied by ankylosing spondylitis or peripheral arthritis
|
|
|
What is the classic triad of findings in Reactive Arthritis (Reiter Syndrome)?
|
"Can't see, can't pee, can't bend my knee":
- Conjunctivitis (and anterior uveitis) - Urethritis - Arthritis |
|
|
What is Reactive Arthritis (Reiter Syndrome) in response to?
|
Post-GI (Shigella, Salmonella, Yersinia, Campylobacter) or Chlamydia infections
|
|
|
What disease has the classic presentation of rash, joint pain, and fever?
|
Systemic Lupus Erythematosus
|
|
|
What mnemonic can help you remember the characteristics of Systemic Lupus Erythematosus?
|
RASH OR PAIN:
- Rash (malar or discoid) - Arthritis - Soft tissues / Serositis - Hematologic disorders (eg, cytopenias) - Oral / nasopharyngeal ulcers - Renal disease, Raynaud phenomenon - Photosensitivity, Positive VDRL/RPR - Anti-nuclear antibodies - Immunosuppressants - Neurologic disorders (eg, seizures, psychosis) |
|
|
What are the common causes of death in patients with Systemic Lupus Erythematosus?
|
- Cardiovascular disease
- Infections - Renal disease |
|
|
What kind of cardiac disease is associated with Systemic Lupus Erythematosus?
|
Libman-Sacks Endocarditis: wart-like vegetations on boths ides of valve
|
|
|
What kind of renal disease is associated with Systemic Lupus Erythematosus?
|
Lupus Nephritis (Type III hypersensitivity reaction):
- Nephritic: diffuse proliferative glomerulonephritis - Nephrotic: membranous glomerulonephritis |
|
|
What kinds of antibodies are associated with Systemic Lupus Erythematosus?
|
- Anti-nuclear antibodies (ANA)
- Anti-dsDNA antibodies - Anti-Smith antibodies - Anti-histone antibodies - Anti-cardiolipin antibodies |
|
|
What antibody is sensitive, but not specific for Systemic Lupus Erythematosus?
|
Anti-nuclear antibodies (ANA)
|
|
|
What antibody is specific and indicates a poor prognosis (renal disease) for Systemic Lupus Erythematosus?
|
Anti-dsDNA antibodies
|
|
|
What antibody is specific, but does not offer prognostic information?
|
Anti-Smith antibodies (directed against snRNPs)
|
|
|
What antibody is sensitive for drug-induced lupus?
|
Anti-histone antibodies
|
|
|
What antibody shows false positives for patients with syphilis and prolongs the PTT in patients with Systemic Lupus Erythematosus? Implications?
|
Anti-Cardiolipin antibody
- Pardoxically prolonged PTT, increases risk for arteriovenous thromboembolism |
|
|
What antibody increases the risk of arteriovenous thromboembolism?
|
Anti-cardiolipin antibodies
|
|
|
How is complement affected in Systemic Lupus Erythematosus?
|
Decreased C3, C4, and CH50 due to immune complex formation
|
|
|
How do you treat patients with Systemic Lupus Erythematosus?
|
- NSAIDs
- Steroids - Immunosuppressants - Hydroxychloroquine |
|
|
What mnemonic can help you remember the characteristics of Systemic Lupus Erythematosus?
|
RASH OR PAIN:
- Rash (malar or discoid) - Arthritis - Soft tissues / Serositis - Hematologic disorders (eg, cytopenias) - Oral / nasopharyngeal ulcers - Renal disease, Raynaud phenomenon - Photosensitivity, Positive VDRL/RPR - Anti-nuclear antibodies - Immunosuppressants - Neurologic disorders (eg, seizures, psychosis) |
|
|
What disease is characterized by immune-mediated, widespread non-caseating granulomas and elevated serum ACE levels?
|
Sarcoidosis
|
|
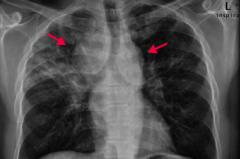
If your patient is a black female with enlarged lymph nodes and bilateral hilar adenopathy or reticular opacities incidentally found on CXR, what diagnosis should you consider? Why?
|
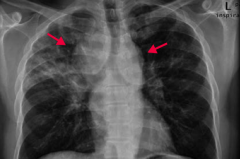
Sarcoidosis
- CXR shows bilateral suprahilar adenopathy (arrows) and right upper lung reticular opacity (often incidental findings on CXR) - Common in black females - Often asymptomatic except for enlarged lymph nodes |
|
|
What is sarcoidosis associated with?
|
- Restrictive lung disease (interstitial fibrosis)
- Erythema nodosum (inflammation of the fat cells under the skin, resulting in tender red nodules or lumps that are usually seen on both shins) - Lupus pernio (chronic raised indurated (hardened) lesion of the skin, often purplish) - Bell palsy - Epithelioid granulomas - Uveitis - Hypercalcemia |
|
|
What are the characteristics of the granulomas in Sarcoidosis?
|
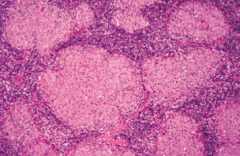
- Non-caseating
- Epithelioid - Contain Schaumann and asteroid bodies |
|
|
What electrolyte abnormality is associated with sarcoidosis? Cause?
|
Hypercalcemia - due to ↑ 1α-hydroxylase-mediated Vitamin D activation in macrophages
|
|
|
How do you treat sarcoidosis?
|
Steroids
|
|
|
What are the characteristics of Sarcoidosis?
|
- Immune-mediated, widespread non-caseating granulomas
- Elevated serum ACE levels - Common in black females - Often asymptomatic except for enlarged lymph nodes - Incidental findings on CXR: bilateral hilar adenopathy and/or reticular opacities |
|
|
What diagnosis should you consider in a patient with pain and stiffness in their shoulders and hips, with fever, malaise, and weight loss?
|
Polymyalgia Rheumatica
|
|
|
What symptoms occur in patients with Polymyalgia Rheumatica?
|
- Pain and stiffness in shoulders and hips
- Fever, malaise, weight loss - No muscular weakness |
|
|
Who is more likely to have Polymyalgia Rheumatica?
|
- More common in women >50 years old
- Associated with Temporal (Giant Cell) Arteritis |
|
|
What are the lab findings in a patient with Polymyalgia Rheumatica?
|
- ↑ ESR
- ↑ C-reactive protein - Normal CK |
|
|
How do you treat a patient with Polymyalgia Rheumatica?
|
Rapid response to low-doe corticosteroids
|
|
|
Which disease is most commonly seen in females 20-50 years old with chronic widespread musculoskeletal pain, stiffness, paresthesias, poor sleep, and fatigue? How should you treat?
|
Fibromyalgia
- Regular exercise - Antidepressants (TCAs, SNRIs) - Anti-convulsants |
|
|
What are the symptoms of Fibromyalgia?
|
- Chronic, widespread musculoskeletal pain
- Associated with stiffness, paresthesias, poor sleep, and fatigue - Most commonly in females 20-50 years old |
|
|
How do you treat Fibromyalgia?
|
- Regular exercise
- Antidepressants (TCAs, SNRIs) - Anti-convulsants |
|
|
What is the cause of progressive symmetric proximal muscle weakness, characterized by endomysial inflammation with CD8+ T cells? Most common location?
|
Polymyositis - most often involves shoulders
|
|
|
What disease can cause present similarly to polymyositis (progressive symmetric proximal muscle weakness) with the addition of malar rash (similar to SLE), Gottron papules (on knuckles), heliotrope (erythematous periorbital) rash, "shawl and face" rash, and/or "mechanic's hands" appearance? What type of inflammation causes this presentation?
|

Dermatomyositis: perimysial inflammation and atrophy with CD4+ T cells
|
|
|
How does Polymyositis compare to Dermatomyositis in terms of location of symptoms?
|

- Polymyositis: symmetric, progressive, proximal muscle weakness, especially in shoulders
- Dermatomyositis: same muscle weakness + malar rash, Gottron papules (knuckles), shawl and face rash |
|
|
What type of inflammation is responsible for Polymyositis and Dermatomyositis?
|
- Polymyositis: endomysial inflammation with CD8+ T cells
- Dermatomyositis: perimysial inflammation and atrophy with CD4+ T cells |
|
|
What lab findings are associated with polymyositis and dermatomyositis?
|
- ↑ CK
- (+) ANA Abs - (+) anti-Jo-1 Abs - (+) anti-SRP Abs - (+) anti-Mi-2 Abs |
|
|
How do you treat a patient with polymyositis or dermatomyositis?
|
Steroids
|
|
|
What is the most common neuromuscular junction disorder?
|
Myasthenia Gravis
|
|
|
What is the pathophysiology responsible for Myasthenia Gravis?
|
Auto-Abs to post-synaptic ACh receptor
|
|
|
What are the symptoms of Myasthenia Gravis?
|
- Ptosis
- Diplopia - Weakness - Worsens with muscle use |
|
|
What is Myasthenia Gravis associated with?
|
- Thymoma
- Thymic hyperplasia |
|
|
How do you treat Myasthenia Gravis?
|
AChE Inhibitor - reverses symptoms
|
|
|
Which neuromuscular junction disease is more rare than Myasthenia Gravis?
|
Lambert-Eaton Myasthenic Syndrome
|
|
|
What is the pathophysiologic cause of Lambert-Eaton Myasthenic Syndrome?
|
Auto-antibodies to presynaptic Ca2+ channels → ↓ ACh release
|
|
|
What are the symptoms of Lambert-Eaton Myasthenic Syndrome?
|
- Proximal muscle weakness
- Autonomic symptoms (dry mouth, impotence) - Improves with muscle use |
|
|
What is Lambert-Eaton Myasthenic Syndrome associated with?
|
Small cell lung cancer
|
|
|
What is the effect of AChE inhibitors in patients with Lambert-Eaton Myasthenic Syndrome?
|
Minimal effect
|
|
|
What are the two neuromuscular junction diseases and how do they compare in terms of the cause?
|
- Myasthenia Gravis: auto-Abs to post-synaptic ACh receptor
- Lambert-Eaton Myasthenic Syndrome: auto-Abs to presynaptic Ca2+ channel which decreases ACh release |
|
|
What are the two neuromuscular junction diseases and how do they compare in terms of the symptoms they cause?
|
- Myasthenia Gravis: ptosis, diplopia, weakness, worsens with muscle use
- Lambert-Eaton Myasthenic Syndrome: proximal muscle weakness, autonomic symptoms (dry mouth, impotence), improves with muscle use |
|
|
What are the two neuromuscular junction diseases and how do they compare in terms of associated conditions?
|
- Myasthenia Gravis: thymoma, thymic hyperplasia
- Lambert-Eaton Myasthenic Syndrome: small cell lung carcinoma |
|
|
If a patient has a suspicious "mass" at a site of trauma to their bone/muscle, what should you think of?
|
Myositis Ossificans: metaplasia of skeletal muscle to bone (muscle becomes calcified) following muscular trauma
|
|
|
Where is Myositis Ossificans more commonly found?
|
Most often in upper or lower extremity
|
|
|
What are the clinical findings in a patient with Myositis Ossificans?
|

May present as a suspicious mass at a site of known trauma or as incidental finding on radiography
|
|

What diagnosis should you consider in a patient with puffy and taut skin with an absence of wrinkles? Cause?
|

Scleroderma (systemic sclerosis): excessive fibrosis and collagen deposition throughout the body
|
|
|
Sclerosis can affect what organs?
|
- Skin
- Renal - Pulmonary (most common cause of death) - Cardiovascular - GI |
|
|
Who is more commonly affected by Scleroderma?
|
Females (75%)
|
|
|
What are the two types of Scleroderma (systemic sclerosis)?
|
- Diffuse Scleroderma
- Limited Scleroderma |
|
|
What are the symptoms of diffuse scleroderma? Cause?
|
- Widespread skin involvement, rapid progression
- Early visceral involvement (eg, renal, pulmonary, CV, GI) - Associated with anti-Scl-70 Ab (anti-DNA topoisomerase I antibody) |
|
|
What are the symptoms of limited scleroderma? Cause?
|
- Limited skin involvement confined to fingers and face
- Also with CREST involvement: Calcinosis, Raynaud phenomenon, Esophageal dysmotility, Sclerodactyly, and Telangiectasia - More benign - Associated with anti-Centromere Ab |
|
|
Which antibodies are associated with the two types of Scleroderma?
|
- Diffuse Scleroderma: anti-DNA topoisomerase I antibody
- Limited Scleroderma: anti-Centromere antibody |
|
|
What are the symptoms of CREST involvement? What is it associated with?
|
CREST:
- Calcinosis - Raynaud phenomenon - Esophageal dysmotility - Sclerodactyly - Telangiectasia - Associated with Limited Scleroderma |
|

What type of lesion is this? Characteristics? Other examples?
|

Macule
- Flat lesion with well-circumscribed change in skin color <1 cm - Ex: freckles, labial macule (picture) |
|

What type of lesion is this? Characteristics? Other examples?
|

Patch
- Macule that is >1 cm (flat lesion with well-circumscribed change in skin color) - Ex: large birthmark (congenital nevus) - picture |
|

What type of lesion is this? Characteristics? Other examples?
|

Papule
- Elevated solid skin lesion < 1cm - Ex: mole (nevus) - picture, acne |
|

What type of lesion is this? Characteristics? Other examples?
|

Plaque
- Papule >1 cm (elevated solid skin lesion) - Ex: psoriasis (picture) |
|

What type of lesion is this? Characteristics? Other examples?
|

Vesicle
- Small fluid containing blister <1 cm - Ex: Chickenpox (varicella), Shingles (zoster) |
|

What type of lesion is this? Characteristics? Other examples?
|

Bulla
- Large fluid-containing blister >1cm - Ex: bullous pemphigoid |
|

What type of lesion is this? Characteristics? Other examples?
|

Pustule
- Vesicle containing pus - Ex: pustular psoriasis |
|

What type of lesion is this? Characteristics? Other examples?
|

Wheal
- Transient smooth papule or plaque - Ex: hives (urticaria) |
|

What type of lesion is this? Characteristics? Other examples?
|

Scale
- Flaking off of stratum corneum - Ex: eczema, psoriasis, SCC |
|

What type of lesion is this? Characteristics? Other examples?
|

Crust
- Dry exudate - Ex: impetigo |
|
|
What are the microscopic dermatologic term?
|
- Hyperkeratosis
- Parakeratosis - Spongiosis - Acantholysis - Acanthosis |
|
|
What lesion causes an increased thickness of the stratum corneum? Example?
|
Hyperkeratosis - eg, psoriasis or calluses
|
|
|
What lesion causes hyperkeratosis with retention of nuclei in the stratum corneum? Example?
|
Parakeratosis - eg, psoriasis
|
|
|
What lesion causes an epidermal accumulation of edematous fluid in the intercellular spaces? Example?
|
Spongiosis - eg, eczematous dermatitis
|
|
|
What lesion causes separation of epidermal cells? Example?
|
Acantholysis - eg, pemphigus vulgaris
|
|
|
What lesion causes epidermal hyperplasia (↑ spinosum)? Example?
|
Acanthosis - eg, acanthosis nigricans
|
|
|
What are the characteristics of hyperkeratosis? Examples?
|
Increased thickness of the startum corneum
- Eg, psoriasis and calluses |
|
|
What are the characteristics of parakeratosis? Examples?
|
Hyperkeratosis (↑ thickness of stratum corneum) with retention of nuclei in stratum corneum
- Eg, psoriasis |
|
|
What are the characteristics of spongiosis? Examples?
|
Epidermal accumulation of edematous fluid in intercellular spaces
- Eg, eczematous dermatitis |
|
|
What are the characteristics of acantholysis? Examples?
|
Separation of epidermal cells
- Eg, Pemphigus Vulgaris |
|
|
What are the characteristics of acanthosis? Examples?
|
Epidermal hyperplasia (↑ spinosum)
- Eg, acanthosis nigricans |
|
|
What are the types of pigmented skin disorders?
|
- Albinism
- Melasma (chloasma) - Vitiligo |
|
|
What disorder has a normal melanocyte number with ↓ melanin production? Cause?
|

Albinism
- Due to ↓ tyrosinase activity or defective tyrosine transport - Can also be caused by failure of neural crest cell migration during development |
|
|
What causes Albinism?
|
- Due to ↓ tyrosinase activity or defective tyrosine transport
- Can also be caused by failure of neural crest cell migration during development |
|
|
What is albinism associated with increased risk of?
|
Skin cancer
|
|

What disorder causes hyperpigmentation associated with pregnancy or OCP use?
|

Melasma (Chloasma
|
|

What disorder causes irregular areas of complete depigmentation? Cause?
|

Vitiligo
- Caused by auto-immune destruction of melanocytes |
|
|
What are the common skin disorders?
|
- Verrucae
- Melanocytic nevus - Urticaria - Ephelis - Atopic dermatitis (eczema) - Allergic contact dermatitis - Psoriasis - Seborrheic keratosis |
|

Which common skin disorder causes soft, tan-colored, cauliflower-like papules? Cause?
|

Verrucae / warts - caused by HPV
|
|
|
Which common skin disorder causes epidermal hyperplasia, hyperkeratosis, and koilocytosis?
|
Verrucae / warts
|
|

Which common skin disorder causes condyloma acuminatum on genitals? Cause?
|

Verrucae / warts (caused by HPV)
|
|

What common skin finding is this?
|

Melanocytic Nevus - intradermal nevi are papular
- AKA common mole |
|

What common skin finding is this?
|

Melanocytic Nevus - junctional nevi are flat macules
|
|
|
What can melanocytic nevi lead to?
|
They are benign, but melanoma can arise in congenital or atypical moles
|
|

What common skin finding is this? Cause?
|

Urticaria / hives - pruritic wheals form after mast cell degranulation
|
|
|
How is urticaria characterized?
|

Superficial dermal edema and lymphatic channel dilation, leading to pruritic wheals
|
|

What common skin finding is this? Cause?
|

Ephelis - freckles
- Normal number of melanocytes, with ↑ melanin pigment |
|

What common skin finding is this? Cause?
|

Atopic Dermatitis (Eczema)
- Pruritic eruption, commonly on skin flexures |
|
|
What is the other name for Atopic Dermatitis? What is it associated with?
|
Eczema
- Associated with other atopic diseases: asthma, allergic rhinitis |
|
|
What is the typical location of Atopic Dermatitis (Eczema)?
|

- Usually starts on face in infancy (G)
- Often appears in antecubital fossae thereafter (H) |
|

What common skin finding is this? Cause?
|

Atopic Dermatitis (Eczema)
- Pruritic eruption, commonly on skin flexures |
|

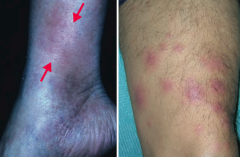
What common skin finding is this? Cause?
|

Allergic Contact Dermatitis
- Type IV hypersensitivity reaction - Follows exposure to allergen - Lesions occur at site of contact (eg, NICKEL) |
|

What common skin finding is this? Cause?
|

Allergic Contact Dermatitis
- Type IV hypersensitivity reaction - Follows exposure to allergen - Lesions occur at site of contact (eg, NEOMYCIN) |
|
|
What are common allergens that cause allergic contact dermatitis? What type of reaction?
|
- Nickel
- Poison Ivy - Neomycin - Causes a type IV hypersensitivity reaction |
|

What common skin finding causes papules and plaques with silver scaling, especially on the knees and elbows?
|

Psoriasis
|
|

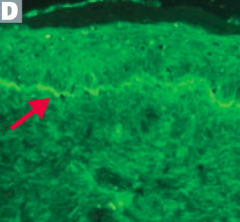
What common skin finding is this? What sign is this arrow pointing at?
|

Psoriasis
- Auspitz sign - pinpoint bleeding spots from exposure of dermal papillae when scales are scraped off |
|
|
What are the skin findings in psoriasis?
|
- Papules and plaques with silvery scaling (K), especially on knees and elbows
- Acanthosis (epidermal hyperplasia, ↑ spinosum) with parakeratotic scaling (nuclei still in stratum corneum) - ↑ Stratum spinosum and ↓ stratum granulosum - Auspitz sign: pinpoint bleeding spots from exposure of dermal papillae when scales are scraped off - Can be associated with nail pitting and psoriatic arthritis |
|

What common skin finding appears as a flat, greasy, pigmented squamous epithelial proliferation with keratin-filled cysts and has an appearance of being "stuck on"? Cause? Where do these lesions occur?
|

Seborrheic Keratosis
- Occurs on head, trunk, and extremities |
|

What common skin finding appears as a flat, greasy, pigmented squamous epithelial proliferation with keratin-filled cysts and has an appearance of being "stuck on"? Cause? Where do these lesions occur?
|

Seborrheic Keratosis
- Occurs on head, trunk, and extremities |
|

What common skin finding appears as a flat, greasy, pigmented squamous epithelial proliferation with keratin-filled cysts and has an appearance of being "stuck on"? Cause? Where do these lesions occur?
|

Seborrheic Keratosis
- Occurs on head, trunk, and extremities |
|
|
What is a common benign neoplasm of older persons?
|

Seborrheic Keratosis
|
|

What is the name of the sign for the sudden appearance of multiple seborrheic keratoses? What does this indicate?
|

Leser-Trélat Sign: indicates an underlying malignancy (eg, GI, lymphoid)
|
|
|
What are the types of infectious skin disorders?
|
- Impetigo
- Cellulitis - Necrotizing Fasciitis - Staphylococcal Scalded Skin Syndrome - Hairy Leukoplakia |
|

What skin disorder is characterized by "honey-colored crusting"? Most common causes?
|

Impetigo
- Usually from S. aureus or S. pyogenes |
|
|
What kind of infection is Impetigo? Characteristics?
|

- Very superficial skin infection
- Usually from S. aureus or S. pyogenes - Highly contagious - Honey-colored crusting |
|

What skin disorder is this? Most common causes?
|

Bullous Impetigo - has bullae and is usually caused by S. aureus
|
|

What skin disorder is this? Most common causes?
|

Cellulitis
- Acute, painful, spreading infection of dermis and subcutaneous tissues - Usually from S. pyogenes or S. aureus |
|
|
What often precipitates a Cellulitis infection?
|

Often starts with a break in the skin from trauma or another infection
|
|

What skin disorder causes bullae and a purple color to the skin? Most common causes?
|

Necrotizing Fasciitis
- Deeper tissue injury, usually from anaerobic bacter or S. pyogenes - Flesh eating bacteria |
|

What does Necrotizing Fasciitis lead to?
|

Results in crepitus from methane and CO2 production
|
|

What skin disorder causes fever and generalized erythematous rash with sloughing of the upper layers of the epidermis that heals completely? Cause?
|

Staphylococcal Scalded Skin Syndrome
- Exotoxin destroys the keratinocyte attachments in the stratum GRANULOSUM only |
|
|
What happens if a patient is exposed to a staphylococcal exotoxin that can destroy keratinocyte attachments to the stratum granulosum?
|

Staphylococcal Scalded Skin Syndrome
- Fever - Generalized erythematous rash - Sloughing of layers of epidermis - Heals completely - Seen in newborns and children |
|

What skin disorder causes white, painless plaques on the tongue that cannot be scraped off? Most common cause?
|

Hairy Leukoplakia
- EBV mediated - Occurs in HIV positive patients |
|
|
Who gets Hairy Leukoplakia? Appearance?
|

- Seen in HIV-positive patients with EBV
- Causes a white, painless plaque on the tongue that cannot be scraped off |
|
|
What are the blistering skin disorders?
|
- Pemphigus vulgaris
- Bullous pemphigoid - Dermatitis herpetiformis - Erythema multiforme - Stevens-Johnson Syndrome |
|
|
What skin disorder is caused by IgG antibody against desmoglein (component of desmosomes)?
|
Pemphigus Vulgaris
|
|
|
What skin disorder is caused by IgG antibody against hemidesmosomes?
|
Bullous Pemphigoid (think: antibodies are "BULLOW" the epidermis)
|
|

Which skin disorder causes flaccid intraepidermal bullae and affects the oral mucosa? Cause?
|

Pemphigus Vulgaris
- Auto-immune: IgG antibody against desmoglein (part of desmosomes) - Caused by acantholysis (keratinocytes in stratum spinosum are connected by desmosomes) |
|
|
How can you diagnose Pemphigus Vulgaris?
|
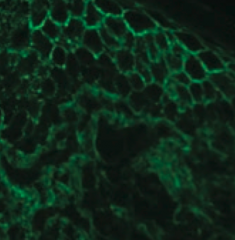
- Immunofluorescence reveals Abs (IgG against Desmoglein) against epidermal cells in a reticular (net-like) pattern
- Nikolsky sign (+) - separation of epidermis upon manual stroking of skin |
|

Which skin disorder causes tense blisters on the skin but spares the oral mucosa? Cause?
|

Bullous Pemphigoid
- Auto-immune: IgG against hemidesmosomes |
|
|
How can you diagnose Bullous Pemphigoid?
|
- Immunofluorescence reveals linear pattern at epidermal-dermal junction
- Tense blisters contain eosinophils - Nikolsky sign (-) = separation of epidermis upon manual stroking of skin |
|

Which skin disorder causes pruritic papules, vesicles, and bullae (often on the elbows)? Cause / associations?
|

Dermatitis Herpetiformis
- Deposits of IgA at the tips of the dermal papillae - Associated with celiac disease |
|
|
Which skin disorder is associated with infections, drugs , cancers, and auto-immune diseases?
|
Erythema Multiforme
|
|
|
What infections can cause Erythema Multiforme?
|

- Mycoplasma pneumoniae
- HSV |
|
|
What drugs can cause Erythema Multiforme?
|
- Sulfa drugs
- β-lactams - Phenytoin |
|
|
What type of lesions are associated with Erythema Multiforme?
|

- Macules
- Papules - Vesicles - Target lesions (look like targets with multiple rings and a dusky center showing epithelial disruption) |
|
|
What skin disorder is characterized by fever, bulla, necrosis, sloughing of skin, and a high mortality rate?
|
Stevens Johnson Syndrome
|
|
|
Are mucus membranes affected in Stevens Johnson Syndrome?
|

Yes - typically at least 2 mucus membranes are involved
|
|
|
In what skin disorders ma you see target lesions?
|
- Erythema Multiforme
- Stevens Johnson Syndrome |
|
|
What is the more severe form of Stevens Johnson Syndrome? How do you distinguish them?
|

Toxic Epidermal Necrolysis
- >30% of the body surface area is affected |
|

Which skin disorder is associated with a hyperpigmented, velvety thickening of the skin? Cause?
|

Acanthosis Nigricans
- Epidermal hyperplasia - Associated with hyperinsulinemia (eg, diabetes, obesity, Cushing syndrome) and visceral malignancies (eg, gastric adenocarcinoma) |
|
|
What skin changes occur in Acanthosis Nigricans?
|

Epidermal hyperplasia causes symmetrical, hyperpigmented, velvety thickening of skin, especially on neck or in axilla
|
|
What premalignant lesion is caused by sun exposure, leading to a small, rough, erythamtous or brownish papule or plaque? What can it progress to?
|
Actinic Keratosis: risk of squamous cell carcinoma is proportional to degree of epithelial dysplasia
|
|
|
What is the appearance of the skin changes in Actinic Keratosis?
|
Small, rough, erythematous or brownish papules or plaques
|
|
|
What is there a risk of if you have Actinic Keratosis? What determines risk?
|

Risk of squamous cell carcinoma is proportional to degree of epithelial dysplasia
|
|
What is the skin disorder characterized by painful inflammatory lesions of the subcutaneous fat, usually on the anterior shins? Possible causes?
|

Erythema Nodosum
- Often idiopathic - Can be associated with sarcoidosis, coccidioidomycosis, histoplasmosis, TB, streptococcal infections, leprosy, and Crohn disease |
|
|
What is the appearance of Erythema Nodosum?
|

Painful, inflammatory lesions of subcutaneous fat, usually on anterior shins
|
|

What can cause Erythema Nodosum?
|
- Often idiopathic
- Can be associated with sarcoidosis, coccidioidomycosis, histoplasmosis, TB, streptococcal infections, leprosy, and Crohn disease |
|
|
Which skin disorder is associated with the 6 P's: pruritic, purple, polygonal planar papules and plaques?
|

Lichen Planus
|
|
|
Which skin disorder manifests as Wickham striae (reticular white lines) on mucosal surfaces? What is it associated with?
|
Lichen Planus
- Associated with Hepatitis C |
|
|
Which skin disorder is associated with a sawtooth infiltrate of lymphocytes at the dermal-epidermal junction?
|
Lichen Planus
|
|
|
What are the features of Lichen Planus?
|

6 P's:
- Pruritic - Purple - Polygonal Planar Papules and Plaques Mucosal involvement manifests as Wickham striae (reticular white lines) Sawtooth infiltrate of lymphocytes at dermal-epidermal junction Associated with Hepatitis C |
|
|
Which skin disorder is known as a "Herald patch" followed days later by a "Christmas tree" distribution of plaques with a collarette scale? How long does this last?
|

Pityriasis Rosea
- Self-resolves in 6-8 weeks |
|

What is this finding? What is it a sign of?
|

Herald Patch - sign of Pityriasis Rosea
|
|

What is this finding? What is it a sign of?
|

Christmas tree distribution - sign of Pityriasis Rosea
|
|
|
What causes a sunburn?
|
Acute cutaneous inflammatory reaction due to excessive UV irradiation
|
|
|
What is the mechanism of damage causing sunburn?
|
Causes DNA mutations, inducing apoptosis of keratinocytes
|
|
|
What are the types of UV rays? How do they differ in the skin changes they cause?
|
- UVA: causes tanning and photoaging
- UVB: causes sunburn |
|
|
What are the potential complications of sunburns?
|
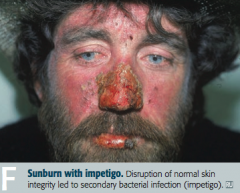
- Impetigo
- Skin cancers: basal cell carcinoma, squamous cell carcinoma, and melanoma |
|
|
What are the types of skin cancers?
|
- Basal cell carcinoma
- Squamous cell carcinoma - Melanoma |
|
|
What is the most common skin cancer?
|
Basal Cell Carcinoma
|
|

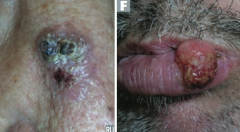
What kind of skin lesion is this? Characteristic appearance?
|

Basal Cell Carcinoma
- Pink, pearly nodules - Commonly with telangiectasias, rolled borders, and central crusting or ulceration |
|

What kind of skin lesion is this? Characteristic appearance?
|

Basal Cell Carcinoma
- Non-healing ulcer with infiltrating growth |
|

What kind of skin lesion is this? Characteristic appearance?
|

Basal Cell Carcinoma
- Scaling plaque (superficial BCC) |
|
|
What is the classic histologic appearance of a Basal Cell Carcinoma?
|
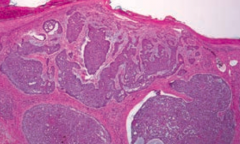
- Palisading nuclei
- Nests of basaloid cells in dermis |
|
|
Where are most Basal Cell Carcinomas located?
|
Found in sun-exposed areas of body
|
|
|
What is the prognosis of Basal Cell Carcinoma?
|
Locally invasive, but almost never metastasizes
|
|
|
How can Basal Cell Carcinomas appear?
|

- Pink pearly nodules, commonly with telangiectasis, rolled borders, and central crusting or ulceration
- Also can appear as non-healing ulcers with infiltrating growth - Scaling plaque (superficial) |
|
|
What is the second most common skin cancer?
|
Squamous Cell Carcinoma
|
|
|
What is Squamous Cell Carcinoma associated with?
|
- Excessive exposure to sunlight
- Immunosuppression - Occasionally arsenic exposure |
|
|
What are the most common locations for Squamous Cell Carcinoma?
|
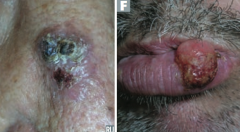
- Face
- Lower lip - Ears - Hands |
|
|
What is the prognosis of Squamous Cell Carcinoma?
|
Locally invasive, but may spread to lymph nodes and will rarely metastasize
|
|
Which type of skin cancer causes ulcerative red lesions with frequent scales, and is associated with chronic draining sinuses?
|
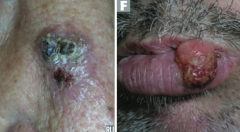
Squamous Cell Carcinoma
|
|
|
What does Squamous Cell Carcinoma look like histologically?
|
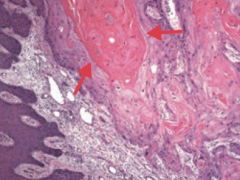
Keratin pearls
|
|
|
What is the name of the scaly plaque, that is a precursor to Squamous Cell Carcinoma?
|
Actinic Keratosis
|
|
|
What is the name of the Squamous Cell Carcinoma variant that grows rapidly and may regress spontaneously? Timeline?
|

Keratoacanthoma: grows rapidly over 4-6 weeks and regresses over months
|
|
|
Which type of skin cancer has a significant risk for metastasis? What determine the risk of this?
|
Melanoma - depth of tumor correlates with risk of metastasis
|
|
|
What tumor marker is there for Melanoma?
|
S-100 tumor marker
|
|
|
What is Melanoma associated with?
|
- Sunlight exposure
- Fair-skinned persons are at ↑ risk |
|
|
What are the key things to look for when evaluating a patient you think may have a Melanoma?
|
ABCDEs:
- Asymmetry - Border irregularity - Color variation - Diameter >6 mm - Evolution over time |
|
|
What are the types of Melanoma?
|

- Superficial spreading melanoma (I)
- Nodular melanoma (J) - Lentigo maligna melanoma (K) - Acrolentiginous melanoma (L) |
|

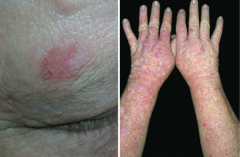
What skin lesion is this?
|

Superficial Spreading Melanoma
|
|

What skin lesion is this?
|

Nodular Melanoma
|
|

What skin lesion is this?
|

Lentigo Maligna Melanoma
|
|

What skin lesion is this?
|

Acrolentiginous Melanoma
|
|
|
What genetic abnormality often drives melanoma?
|
BRAF kinase activating mutation (V600E)
|
|
|
How do you treat Melanoma?
|
- Primary treatment: excision with appropriately wide margins
- Metastatic or unresectable melanoma in patients with BRAF V600E mutation may benefit from Vemurafenib, a BRAF kinase inhibitor |

