![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
100 Cards in this Set
- Front
- Back
|
Which bacteria form long, branching filaments resembling fungi? |
- Actinomyces
- Nocardia |
|
Which bacteria causes oral/facial abscesses that drain through sinus tracts forming yellow "sulfur" granules? How do you treat?
|
Actinomyces - treat with Penicillin
|
|
|
Characteristics of Actinomyces?
|
- G+ anaerobe
- Forms long-branching filaments that resemble fungi - Not acid fast - Normal oral flora - Causes oral/facial abscesses that drain through sinus tracts forming yellow "sulfur granules" - Treat with Penicillin |
|
|
Which bacteria causes pulmonary infections in immunocompromised patients and cutaneous infections after trauma in immunocompromised patients? How do you treat?
|
Nocardia - treat with Sulfonamides
|
|
|
Characteristics of Nocardia?
|
- G+ aerobe
- Forms long, branching filaments resembling fungi - Acid fast (weak) - Found in soil - Causes pulmonary infections in immunocompromised patients - Causes cutaneous infections after trauma in immunocompromised patients - Treat with Sulfonamides |
|
|
What causes Tuberculosis? Different forms of infection?
|
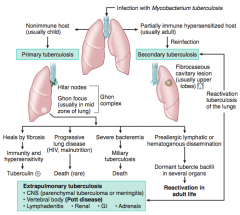
Infection with Mycobacterium tuberculosis
- Primary infection: non-immune host (usually a child) - Secondary infection: partially immune hyper-sensitized host (usually adult) |
|
|
What are the signs of a Primary Tuberculosis?
|
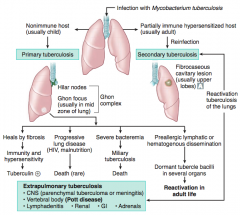
Occurs in a non-immune host (usually a child)
- Ghon Complex: Hilar nodes & Ghon focus (usually in mid zone of lung) |
|
|
What can Primary Tuberculosis lead to?
|
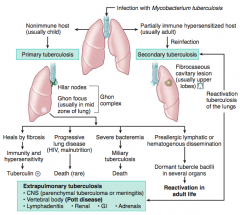
- Heals by fibrosis → immunity and hypersensitivity → Tuberculin (+)
- Progressive lung disease (HIV, malnutrition) → death (rare) - Severe bacteremia → miliary tuberculosis → death - Pre-allergic lymphatic or hematogenous dissemination → dormant tubercle bacilli in several organs → REACTIVATION in adult life |
|
|
What are the signs of a Secondary Tuberculosis?
|
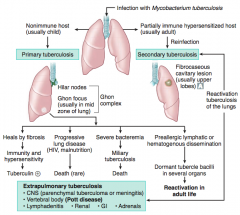
Fibrocaseous cavitary lesion (usually in upper lobes)
|
|
|
What can Secondary Tuberculosis lead to?
|
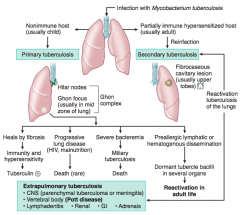
Extrapulmonary Tuberculosis |
|
|
What does a positive PPD test mean?
|
Either:
- Current infection with Mycobacterium tuberculosis - Past exposure to Mycobacterium tuberculosis - BCG vaccinated |
|
|
What does a negative PPD test mean?
|
Either:
- No infection - Anergic (steroids, malnutrition, immunocompromise) and in sarcoidosis |
|
|
Which test is more specific than PPD for Mycobacterium tuberculosis infection?
|
Interferon-γ Release Assay (IGRA)
- More specific - Fewer false positives from BCG vaccination |
|
|
Which vaccine is used to prevent Tuberculosis?
|
BCG vaccine
|
|
|
What is the appearance of a caseating granuloma in tuberculosis infection?
|
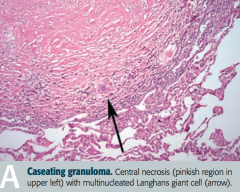
- Central necrosis (pinkish region in upper left) |
|
|
What are the symptoms of TB?
|
- Fever
- Night sweats - Weight loss - Hemoptysis |
|
|
What are the species of Myocbacterium? What disease do they cause?
|
- M. tuberculosis (TB, often resistant to multiple drugs)
- M. kansasii (pulmonary TB-like symptoms) - M. avium-intracellulare (causes disseminated, non-TB disease in AIDS; often resistant to multiple drugs; prophylactic tx with azithromycin) - M. leprae (Leprosy / Hansen disease) |
|
|
What are the characteristics of all Mycobacteria?
|
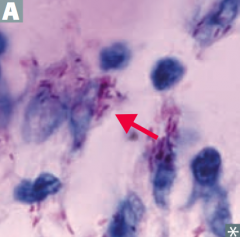
All are acid-fast organisms
|
|
|
Which bacteria causes disseminated, non-TB disease in AIDS patients? Treatment / prevention?
|
Mycobacterium avium-intracellulare
- Often resistant to multiple drugs - Prophylactic treatment with Azithromycin |
|
|
What is released by virulent strains of Mycobacteria? Implication?
|
Cord fator is found in virulent strains
- Inhibits macrophage maturation - Induces release of TNF-α Sulfatides (surface glycolipids) - Inhibit phagolysosomal fusion |
|

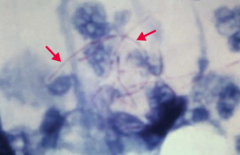
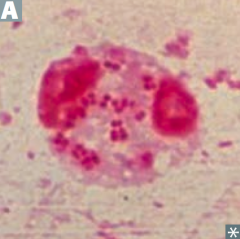
Which bacteria causes this appearance?
|
Mycobacterium leprae (Leprosy / Hansen disease)
|
|
|
Characteristics of Mycobacterium leprae?
|
- Acid-fast bacillus
- Likes cool temperatures - Cannot be grown in vitro - Reservoir in US: armadillos |
|
|
What does Mycobacterium leprae infect?
|
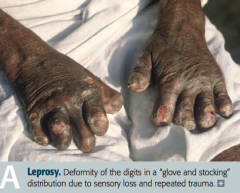
- Skin
- Superficial nerves: "glove and stocking" loss of sensation - Armadillos (reservoir) |
|
|
What are the forms of Leprosy / Hansen disease? Characteristics?
|

Lepromatous:
- Diffuse presentation over skin - Leonine (lion-like) facies - Communicable - Characterized by low cell-mediated immunity w/ a humoral Th2 response Tuberculoid: - Limited to a few hypoesthetic, hairless skin plaques - Characterized by high cell-mediated immunity with a largely Th1 type immune response |
|
|
Which form of Leprosy has a LOW cell-mediated immunity with a humoral Th2 response?
|
Lepromatous form
|
|
|
Which form of Leprosy has a HIGH cell-mediated immunity with a largely Th1-type immune response?
|
Tuberculoid form
|
|
|
How do you treat the two forms of Leprosy / Hansen disease?
|
Lepromatous form:
- Dapsone, Rifampin, and Clofazimine for 2-5 years Tuberculoid form: - Dapsone and Rifampin for 6 months |
|
|
How should you first distinguish G- (pink) bacteria?
|
Shape
- Diplococci - "Coccoid" rods - Rods - Oxidase (+) comme shaped |
|
|
Which bacteria are G- diplococci? How do you distinguish them?
|
Distinguish based on ability to ferment maltose
- Neisseria meningitidis (ferments maltose - meningitiids starts with "m") - Neisseria gonorrhoeae (non-fermenter) |
|
|
Which bacteria are G- coccoid rods? How do you distinguish them?
|
* Haemophilus influenzae (requires factors V and X)
* Bordetella pertussis - Pasteurella (animal bites) - Brucella (brucellosis) |
|
|
Which bacteria are G- rods? How do you distinguish them?
|
Distinguish based on ability to ferment lactose and distinguish non-fermenters by oxidase capability:
Lactose fermenters: - Fast: Klebsiella, E. coli, Enterobacter - Slow: Citrobacter, Serratia, etc. Lactose non-fermenters: - Oxidase (+): Pseudomonas - Oxidase (-): Shigella, Salmonella, Proteus, Yersinia |
|
|
Which bacteria are lactose fermenting G- rods? How do you distinguish them?
|
Fast fermenters:
* Klebsiella * E. coli - Enterobacter Slow fermenters: - Citrobacter - Serratia Lactose is "KEE" - Test with Mac"C"on"KEE'S" agar |
|
|
Which bacteria are non-lactose fermenting G- rods? How do you distinguish them?
|
Oxidase (+):
- Pseudomonas Oxidase (-): - Shigella - Salmonella - Proteus - Yersinia |
|
|
Which bacteria are oxidase (+), comma shaped G-? How do you distinguish them?
|
Grows in 42°C:
- Campylobacter jejuni Grows in alkaline media: - Vibrio cholerae Produces urease: - Helicobacter pylori |
|
|
How do you determine if a bacteria can ferment lactose?
|

*If it can grow pink colonies on MacConkey agar
Remember macConKEE'S agar to remember which bacteria can ferment lactose - - Citrobacter (slow) - Klebsiella (fast) - E. coli (fast) - Enterobacter (fast) - Serratia (slow) *Can also test on EMB agar - lactose fermenters grow as purple/black colonies (E. coli grows purple colonies w/ a green sheen) |
|
|
Can E. coli ferment lactose? Why or why not?
|
Yes - E. coli produces β-galactosidase, which breaks down lactose into glucose and galactose
|
|
|
G- bacilli are resistant to what antibiotics? What are they susceptible to?
|
- Resistant to Penicillin G and Vancomycin (G- outer membrane layer inhibits entry)
- Susceptible to Penicillin derivatives such as Ampicillin and Amoxicillin |
|
|
Neisseria species are what type of bacteria? What can they ferment?
|
G- diplococci
- MeninGococci ferment both Maltose and Glucose (meningitidis) - Gonococci ferment Glucose (gonorrhoeae) |
|
|
What do Neisseria species produce?
|
IgA proteases
|
|
|
Which bacteria is sexually transmitted and can also cause septic arthritis, neonatal conjunctivitis, pelvic inflammatory disease (PID), and Fitz-Hugh-Curtis Syndrome? Treatment?
|
Neisseria gonorrhoeae
Treat: Ceftriaxone (+ Azithromycin or Doxycycline for possible Chlamydia co-infection) |
|
|
Characteristics of Neisseria gonorrhoeae?
|
G- diplococci
- Produces IgA proteases - Ferments glucose only - Often intracellular (within neutrophils) - No polysaccharide capsule - No vaccine (d/t rapid antigenic variation of pilus proteins) |
|
|
What can Neisseria gonorrhoeae infection cause? Prevention?
|
Prevent sexual transmission w/ condoms
- Gonorrhea - Septic arthritis - Neonatal conjunctivitis (prevent transmission w/ erythromycin ointment) - Pelvic Inflammatory Disease (PID) - Fitz-Hugh-Curtis Syndrome |
|
|
Which bacteria is spread via respiratory and oral secretions, causing meningococcemia and meningitis as well as Waterhouse-Friderichsen syndrome? Treatment?
|
Neisseria meningitidis
Treat: Ceftriaxone or Penicillin G |
|
|
Characteristics of Neisseria meningitidis?
|
G- diplococci
- Produces IgA proteases - Ferments glucose AND maltose - Polysaccharide capsule - Vaccine (none for type B) - Spread via respiratory and oral secretions |
|
|
What can Neisseria meningitidis infection cause? Prevention?
|

- Meningococcemia (picture)
- Meningitis - Waterhouse-Friderichsen syndrome Prevent: Rifampin, Ciprofloxacin, or Ceftriaxone prophylaxis in close contacts (Ceftriaxone or Penicillin G can be used for treatment) |
|

Which bacteria causes an infection that leads to the "thumbprint sign" on lateral neck radiograph?
|

Haemophilus influenzae epiglottitis
|
|
|
Characteristics of Haemophilus influenzae?
|
Small G- coccobacillary rod
- Aerosol transmission - Most invasive disease caused by capsular type B - Produces IgA protease - Culture on chocolate agar requires factors V (NAD+) and X (Hematin) for growth |
|
|
Which type of Haemophilus influenzae causes the most invasive disease? What do the other types cause?
|
- Most invasive disease caused by capsular type B
- Nontypeable strains cause mucosa infections (eg, otitis media, conjunctivitis, or bronchitis) |
|
|
What kind of infection is caused by Haemophilus influenzae?
|
HaEMOPhilus causes
- Epiglottitis ("cherry red" in children) - Meningitis - Ototis media - Pneumonia |
|
|
How do you culture Haemophilus influenzae?
|
On Chocolate agar, requires:
- Factor V (NAD+), also can be grown w/ S. aureus which provides Factor V - Factor X (hematin) "When a child has "flu", mom goes to five (V) and dime (X) store to buy some chocolate" |
|
|
How do you treat Haemophilus influenzae infections?
|
- Mucosal infections (eg, otitis media, conjunctivitis, bronchitis) with Amoxicillin +/- Clavulanate
- Meningitis with Ceftriaxone |
|
|
How do you prevent spread / infection of Haemophilus influenzae infections?
|
- Prevention in close contacts exposed to AEROSOL TRANSMISSION: Rifampin
- Prevention w/ vaccine: contains type B capsular polysacchardie (polyribosylribitol phosphate) conjugated to diphtheria toxoid or other protein (given between 2-18 months) |
|
|
Which bacteria causes severe pneumonia, fever, GI and CNS symptoms?
|
Legionella pneumophila (Legionnaire's disease)
|
|
|
Characteristics of Legionella pneumophila?
|
G- rod
- Gram stains poorly (use SILVER stain) - Grow on CHARCOAL yeast extract culture with IRON and CYSTEINE - Detected clinically by presence of antigen in urine - Aerosol transmission from environmental water source habitat (eg, AC systems, hot water tanks); no person-to-person transmission "Think of a French LEGIONNAIRE (soldier) with his SILVER helmet, sitting around a campfire (CHARCOAL) with his IRON dagger - his is no SISSY (CYSTEINE)" |
|
|
How do you diagnose Legionella pneumophila? Other signs?
|
* Presence of antigen in urine is used clinically
- Labs show hyponatremia - G- rod, better stained w/ Silver Stain - Cultured on Charcoal yeast extract with Iron and Cysteine |
|
|
How does Legionella pneumophila get spread?
|
- Aerosol transmission from environmental water source habitat (eg, A/C systems, hot water tanks)
- Not person-to-person |
|
|
What disease states can Legionella pneumophila infection cause? Treatment?
|
- Legionnaires' Disease: severe pneumonia, fever, GI and CNS symptoms |
|
|
Which bacteria is associated with wound and burn infections?
|
Pseudomonas aeruginosa
|
|
|
Characteristics of Pseudomonas aeruginosa?
|
G- Rod:
- Aerobic (AERuginosa - Non-lactose fermenting - Oxidase (+) - Produces pyocyanin (blue-green pigment) - Grape-like odor - Water source - Produces endotoxin (fever, shock) and exotoxin A (inactivates EF-2) |
|
|
What toxins does Pseudomonas aeruginosa produce? Effects?
|
- Endotoxin → fever and shock
- Exotoxin A → inactivates EF-2 |
|
|
What color is Pseudomonas aeruginosa? How?
|
Blue/green pigment called Pyocyanin
|
|
|
What kind of infections does Pseudomonas aeruginosa cause?
|
PSEUDOmonas associated with wound and burn infections:
- Pneumonia (especially in cystic fibrosis) - Sepsis - External otitis (swimmer's ear) - UTI - Drug use - Diabetic Osteomyelitis (and malignant otitis externa in diabetics) - And hot tub folliculitis |
|
|
Which bacteria causes hot tub folliculitis?
|
Pseudomonas aeruginosa
|
|
|
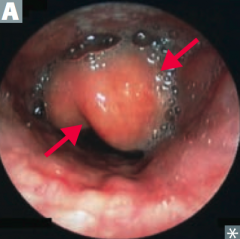
How does Pseudomonas aeruginosa affect immunocompromised patients?
|
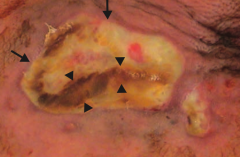
Ecthyma gangrenosum
- Rapidly progressive - Large ulcer (arrows) - Necrotic cutaneous lesions (arrowheads) |
|
|
What bacteria is associated with chronic pneumonia in cystic fibrosis patients?
|
Pseudomonas aeruginosa (associated with biofilms)
|
|
|
What are the virulence factors of E. coli?
|
- Fimbriae
- K capsule - LPS endotoxin |
|
|
What kind of infections are enhanced by the E. coli virulence factor "fimbriae"?
|
- Cystitis |
|
|
What kind of infections are enhanced by the E. coli virulence factor "K capsule"?
|
- Pneumonia
- Neonatal meningitis |
|
|
What kind of infections are enhanced by the E. coli virulence factor "LPS endotoxin"?
|
Septic shock
|
|
|
What are the strains of E. coli?
|
- EIEC
- ETEC - EPEC - EHEC |
|
|
Which bacteria causes invasive dysentery (severe diarrhea with the presence of blood and mucus in the feces)? Mechanism?
|
EIEC (Invasive)
- Microbe invades intestinal mucosa and causes necrosis and inflammation - Clinical manifestation is similar to Shigella |
|
|
Which bacteria causes Travelers' Diarrhea (watery)? Mechanism?
|
ETEC (Travelers')
- Produces heat-labile and heat-stable enteroToxins - No inflammation or invasion |
|
|
Which bacteria causes diarrhea usually in children? Mechanism?
|
EPEC (Pediatrics)
- No toxin produced - Adheres to apical surface - Flattens villi - Prevents absorption |
|
|
Which bacteria causes non-invasive dysentery (severe diarrhea with the presence of blood and mucus in the feces)? Mechanism?
|
EHEC (O157:H7 is the most common serotype) |
|
|
What are the components of Hemolytic Uremic Syndrome? Cause?
|
- Anemia
- Thrombocytopenia - Acute renal failure - Caused by EHEC - Microthrombi form on endothelium damaged by toxin → mechanical hemolysis (forms schistocytes) and ↓ renal blood flow - Microthrombi consume platelets → thrombocytopenia |
|
|
What is the difference between EIEC and EHEC?
|
- EIEC: invasive, the microbe invades intestinal mucosa, causing necrosis and inflammation leading to dysentery
- EHEC: not-invasive, toxin alone causes necrosis and inflammation leading to dysentery |
|
|
Besides the presentation and mechanism, how does EHEC differ from other forms of E. coli?
|
Does not ferment sorbitol
|
|
|
Which form of E. coli does not ferment sorbitol?
|
EHEC
|
|
|
Which bacteria is associated with the 4 A's (Aspiration pneumonia, Abscess in lungs and liver, Alcoholics, and di-A-betics)?
|
Klebsiella
|
|
|
Characteristics of Klebsiella?
|
G- Rod
- Fast lactose fermenter - Part of intestinal flora |
|
|
What does Klebsiella cause? Who is affected?
|
*Causes lobar pneumonia (via Aspiration)
- Forms Abscesses in lungs and liver - Common in Alcoholics and di-A-betics - Forms mucoid colonies d/t abundant polysaccharide capsules - Red "currant jelly" sputum (remember 4 A's) *Also cause of nosocomial UTIs |
|
|
Which bacteria causes patients to have a lobar pneumonia that leads to red "currant jelly" sputum?
|
Klebsiella
|
|
|
What are the similarities of Salmonella and Shigella?
|
G- rods
- Invades intestinal mucosa and cause bloody diarrhea - Do not ferment lactose - Oxidase (-) |
|
|
How do Salmonella and Shigella differ in movement?
|
Salmonella:
- Flagella (salmon swim) Shigella: - No flagella |
|
|
How do Salmonella and Shigella differ in dissemination?
|
Salmonella
- Hematogenously (salmon swimming) Shigella - Cell-to-cell transmission - No hematogenous spread |
|
|
How do Salmonella and Shigella differ in reservoirs?
|
Salmonella
- Many animal reservoirs (salmon is an animal) Shigella - Only in humans and primates |
|
|
How do Salmonella and Shigella differ in production of hydrogen sulfide?
|
Salmonella
- Produces hydrogen sulfide Shigella - Does not produce hydrogen sulfide |
|
|
How do Salmonella and Shigella differ in their response to antibiotics?
|
Salmonella
- Antibiotics may PROLONG fecal excretion of organism Shigella - Antibiotics SHORTEN duration of fecal excretion of organism |
|
|
How do Salmonella and Shigella differ in their immune system response?
|
Salmonella
- Invades intestinal mucosa and causes a MONOCYTIC response Shigella - Invades intestinal mucosa and causes a PMN infiltration |
|
|
Which disease is characterized by rose spots on the abdomen, fever, headache, and diarrhea and can remain in the gallbladder causing a carrier state? Cause?
|
Typhoid Fever (caused by Salmonella typhi) - only found in humans
|
|
|
What are the symptoms of Typhoid Fever (Salmonella typhi)?
|
- Rose spots on abdomen
- Fever - Headache - Diarrhea - Can remain in gallbladder and cause a carrier state |
|
|
Characteristics of Salmonella?
|
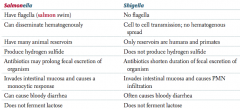
- Flagella (salmon swim)
- Can disseminate hematogenously - Have many animal reservoirs - Produce hydrogen sulfide - Antibiotics may PROLONG fecal excretion of organism - Invades intestinal mucosa and causes a monocytic response - Can cause bloody diarrhea - Does not ferment lactose |
|
|
Characteristics of Shigella?
|
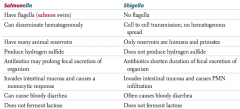
- No flagella
- Cell to cell transmission, no hematogenous spread - Only reservoirs are humans and primates - Does not produce hydrogen sulfide - Antibiotics shorten duration of fecal excretion of organism - Invades intestinal mucosa and causes a PMN infiltration - Often causes bloody diarrhea - Does not ferment lactose |
|
|
What bacteria is a major cause of bloody diarrhea (especially in children), and is spread through foods such as poultry, meat, and unpasteurized milk?
|
Campylobacter jejuni |
|
|
Characteristics of Campylobacter jejuni?
|
G- Comma or S-shaped
- Oxidase (+) - Grows at 42°C ("Campylobacter likes the hot campfire") |
|
|
How is Campylobacter jejuni acquired?
|
Fecal-oral transmission through foods such as:
- Poultry - Meat - Unpasteurized milk |
|
|
What does Campylobacter jejuni cause?
|
- Major cause of bloody diarrhea (especially in children)
- Common antecedent to Guillain-Barré syndrome and reactive arthritis |
|
|
Which bacteria produces profuse "rice-water diarrhea"? Mechanism? Treatment?
|
Vibrio cholerae
- Enterotoxin permanently activates Gs → ↑cAMP → rice-water diarrhea - Treat with prompt oral rehydration |
|
|
Characteristics of Vibrio cholerae?
|
G- comma shaped
- Oxidase (+) - Grows in alkaline media |
|
|
Where is Vibrio cholerae more common? Treatment?
|
- Endemic to developing countries
- Prompt oral rehydration is necessary |

