![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
63 Cards in this Set
- Front
- Back

What kind of RBC is this? What pathology is associated with this? |

Acanthocyte (Spur Cell) |
|

What kind of RBC is this? What pathology is associated with this? |

Basophilic Stippling |
|

What kind of RBC is this? What pathology is associated with this? |

Bite Cell |
|

What kind of RBC is this? What pathology is associated with this? |

Elliptocyte |
|

What kind of RBC is this? What pathology is associated with this? |

Macro-Ovalocyte |
|
What kind of RBC is this? What pathology is associated with this? |
Ringed Sideroblast |
|

What kind of RBC is this? What pathology is associated with this? |

Schistocyte / Helmet Cell |
|

What kind of RBC is this? What pathology is associated with this? |

Sickle Cell |
|

What kind of RBC is this? What pathology is associated with this? |

Spherocyte |
|
What kind of RBC is this? What pathology is associated with this? |
Teardrop cell |
|

What kind of RBC is this? What pathology is associated with this? |

Target Cell |
|
What kind of RBC pathology is this? What causes its formation? What pathology is associated with this? |
Heinz Bodies |
|

What kind of RBC pathology is this? What causes its formation? What pathology is associated with this? |

Howell-Jolly Bodies |
|
|
How can you categorize the types of anemias? |
- Microcytic (MCV <80 fL) |
|
|
What are the types of microcytic anemias? Definition? |
MCV <80 fL |
|
|
What are the types of normocytic anemias? Definition? |
MCV 80-100 fL |
|
|
What are the types of non-hemolytic, normocytic anemias? Definition? |
MCV 80-100 fL and reticulocyte count normal or ↓ |
|
|
What are the types of intrinsic hemolytic, normocytic anemias? Definition? |
MCV 80-100 fL with increased reticulocyte count |
|
|
What are the types of extrinsic hemolytic, normocytic anemias? Definition? |
MCV 80-100 fL with increased reticulocyte count |
|
|
What are the types of macrocytic anemias? Definition? |
MCV >100 fL |
|
|
What are the types of macrocytic, megaloblastic anemias? Definition? |
MCV >100 fL |
|
|
What are the types of macrocytic, non-megaloblastic anemias? Definition? |
MCV >100 fL |
|
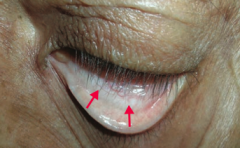
What is the most likely cause of this patient's conjunctival pallor? |
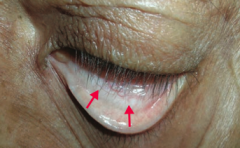
Anemia (possibly due to iron deficiency) |
|
|
What causes iron deficiency anemia? |
Decreased iron due to: |
|
|
What are the implications of an iron deficiency? |
Decreased completion of final step in heme synthesis |
|
|
What lab findings are associated with iron deficiency anemia? |
- MCV < 80 fL (microcytic) |
|
|
What other unrelated symptoms should you look for in a patient with iron deficiency anemia to check for another syndrome? |
Plummer-Vinson Syndrome: |
|
|
What is the term for the triad of iron deficiency anemia, esophageal webs, and atrophic glossitis? |
Plummer-Vinson Syndrome |
|
|
What are the symptoms in Plummer-Vinson Syndrome? |
- Iron deficiency anemia |
|
What does this blood smear tell you? |
Iron Deficiency Anemia |
|
|
What is the defect in α-thalassemia? |
α-globin gene deletions → ↓ α-globin synthesis |
|
|
What kind of deletions can lead to α-thalassemia? |
- Cis deletion prevalent in Asian populations |
|
|
How many copies of the α-globin gene do you have? Implications? |
4 alleles: |
|
|
What causes hydrops fetalis? |
4 α-globin allele deletion: |
|
|
What causes HbH disease? |
3 α-globin allele deletion: |
|
|
What form of α-thalassemia is more common in Asians? |
Cis deletion of α-globin alleles |
|
|
What form of α-thalassemia is more common in Africans? |
Trans deletion of α-globin alleles |
|
|
Who is more likely to have β-thalassemia? |
Prevalent in Mediterranean poulations |
|
|
What causes β-thalassemia? |
Point mutations in splice sites and promoter sequences → ↓ β-globin synthesis |
|
|
What are the types of β-thalassemia? |
- β-thalassemia minor (heterozygote) |
|
|
What is the most severe form of β-thalassemia? |
β-thalassemia major (homozygote) |
|
|
What are the consequences of having absent β chain (β-thalassemia major)? |
- Severe anemia → requires blood transfusion |
|
|
What kind of infection are patients with β-thalassemia major at risk for? Complications? |
Parvovirus B19 → can induce an aplastic crisis |
|
|
What kind of hemoglobin is more common in patients with β-thalassemia major? |
HbF (α2γ2) - protective in the infant and disease only becomes symptomatic after 6 months |
|
|
What is the medium severity form of β-thalassemia? |
HbS / β-thalassemia heterozygote |
|
|
What is the least severe form of β-thalassemia? |
β-thalassemia Minor (heterozygote) |
|
|
How do yo confirm diagnosis of β-thalassemia minor (heterozygote)? |
Confirm diagnosis by ↑ HbA2 (>3.5% on electrophoresis) |
|
|
What happens to RBCs in patients with β-thalassemia major? |
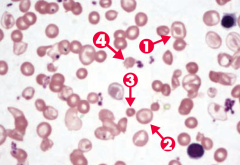
Note anisocytosis, poikilocytosis, target cells (arrows 1 and 2), microcytosis (arrow 3), and schistocytes (arrow 4) |
|
|
How does lead poisoning affect the blood? |
- Lead inhibits ferrochelatase and ALA dehydratase → ↓ heme synthesis and ↑ RBC protoporphyrin |
|
|
Who is at risk for lead poisoning? |
High risk in old houses with chipped paint |
|
|
How does lead poisoning affect other organs besides the blood? |
LEAD: |
|

What does the arrow point at? Sign of? |

- Lead Lines on metaphyses of long bones on x-ray |
|
|
How does lead affect the gums? |
Lead Lines on gingivae = Burton lines |
|
|
How does lead affect the brain? |
Can cause encephalopathy |
|
|
How does lead affect the musculoskeletal system? |
Drops: wrist and foot drops |
|
|
How does lead affect the abdomen? |
Abdominal colic |
|
|
How do you treat lead poisoning? |
First line treatments: |
|
What is wrong in this picture? Cause? |
Sideroblastic Anemia |
|
What causes sideroblastic anemia? |
- Genetic |
|
What causes acquired sideroblastic anemia? |
Myelodysplastic syndromes |
|
|
What causes reversible sideroblastic anemia? |
- Alcohol is most common |
|
|
What are the lab findings in sideroblastic anemia? |
- ↑ Iron |
|
How do you treat Sideroblastic Anemia? |
Pyridoxine (B6, cofactor for δ-ALA synthase) |

