![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
126 Cards in this Set
- Front
- Back
|
What is the function of erythrocytes? |
Carries O2 to tissues and CO2 to lungs
|
|
|
What is the structure of an erythrocyte?
|
- Anucleate and biconcave
- Large surface area-to-volume ratio for rapid gas exchange |
|
|
How long does an erythrocyte last?
|
120 days
|
|
|
What is the source of energy for erythrocytes?
|
Glucose:
- 90% used in glycolysis - 10% used in HMP shunt |
|
|
How does an erythrocyte eliminate CO2?
|
- Membrane contains Chloride-HCO3- antiporter
- Allows RBCs to export HCO3- and transport CO2 from the periphery to the lungs for elimination |
|
|
What can erythrocytosis lead to?
|
Polycythemia / ↑ Hematocrit
|
|
|
What term is used for varying sizes of erythrocytes?
|
Anisocytosis
|
|
|
What term is used for varying shapes of erythrocytes?
|
Poikilocytosis
|
|
|
What is Anisocytosis mean?
|
Varying sizes of RBCs
|
|
|
What is Poikilocytosis mean?
|
Varying shapes of RBCs
|
|
|
What is an immature RBC called? What does its presence indicate?
|
Reticulocyte - immature RBC is a marker of erythroid proliferation
|
|
|
What structure is involved in primary hemostasis?
|
Platelet (Thrombocyte)
|
|
|
How are platelets made?
|
Small cytoplasmic fragments derived from megakaryocytes
|
|
|
What is the life span of a platelet?
|
8-10 days
|
|
|
What is the function of a platelet?
|
When activated by endothelial injury, aggregates with other platelets and interacts with fibrinogen to form a platelet plug
|
|
|
What are the contents of platelets?
|
- Dense granules: ADP and calcium
- α granules: vWF and fibrinogen |
|
|
What is found in the dense granules of platelets?
|
ADP and Ca2+
|
|
|
What is found in the α granules of platelets?
|
vWF and fibrinogen
|
|
|
Where is a large portion of the platelet pool stored? How much?
|
1/3 of platelet pool is stored in the spleen
|
|
|
What causes petechiae?
|
Thrombocytopenia or decreased platelet function
|
|
|
What is the receptor for von Willebrand Factor?
|
GpIb
|
|
|
What is the receptor for fibrinogen?
|
GpIIb / IIIa
|
|
|
What are the types of leukocytes?
|
Granulocytes:
- Neutrophils - Eosinophils - Basophils Mononuclear cells: - Monocytes - Lymphocytes |
|
|
What is the function of leukocytes? How many are there normally?
|
- Responsible for defense against infections
- Normally 4000 - 10,000 cells / mm3 |
|
|
What is the differential of WBC from highest to lowest?
|
"Neutrophils Like Making Everything Better"
- Neutrophils (54-62%) - Lymphocytes (25-33%) - Monocytes (3-7%) - Eosinophils (1-3%) - Basophils (0-0.75%) |
|
|
What is the acute inflammatory response cell?
|
Neutrophil
|
|
|
What are there increased neutrophils?
|
Bacterial infections
|
|
|
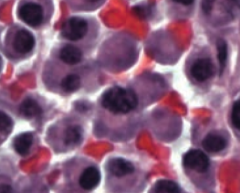
What is the function and appearance of Neutrophils?
|
- Multi-lobed nucleus
- Phagocytic cell that acts in the acute inflammatory response, especially for bacterial infections |
|
|
What are the contents of neutrophils?
|
- Specific granules (smaller and more numerous): ALP, collagenase, lysozyme, and lactoferrin
- Azurophilic granules (larger and less numerous) / lysosomes: proteinases, acid phosphatase, myeloperoxidase, and β-glucuronidase |
|
|
What are the contents of specific granules in neutrophils? How common are they relatively? Size?
|
- Contains: ALP, collagenase, lysozyme, and lactoferrin
- More numerous - Smaller |
|
|
What are the contents of azurophilic granules in neutrophils? How common are they relatively? Size? |
Aka Lysosomes
- Contain: proteinases, acid phosphatase, myeloperoxidase, and β-glucuronidase - Less numerous - Larger |
|
|
Under what circumstances might you see hypersegmented neutrophils (5 or more lobes)?
|
Vitamin B12 or Folate deficiency
|
|
|
Under what circumstances might you see increased band cells? What do these represent?
|
- Band cells are immature neutrophils
- Reflects states of increased myeloid proliferation (bacterial infections and CML) |
|
|
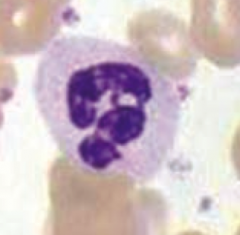
What is the function and appearance of monocytes?
|
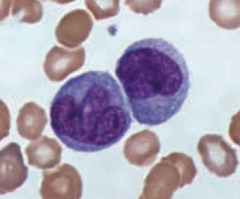
- Differentiates into macrophages in the tissues
- Large, kidney shaped nucleus with extensive "frosted glass" cytoplasm |
|
|
What is the function of macrophages?
|
- Phagocytose bacteria, cellular debris, and senescent RBCs
- Scavenges damaged cells and tissues - Can function as an antigen-presenting cell via MHC II |
|
|
What is the source of macrophages?
|
Differentiates from circulating blood monocytes, activated by γ-interferon
|
|
|
What is the function of IFN-γ?
|
Activates monocytes to macrophages
|
|
|
What is a cell surface marker for macrophages?
|
CD14
|
|
|
What cells are an important component of granuloma formation (eg, TB and sarcoidosis)?
|
Macrophage
|
|
|
What are the functions of Eosinophils?
|
- Defends against helminthic infections via major basic protein
- Highly phagocytic for antigen-antibody complexes - Produces histaminase and arylsulfatase (limits reaction following mast cell degranulation) |
|
|
What is the appearance of eosinophils?
|
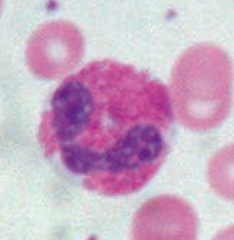
- Bilobate nucleus
- Packed with large eosinophilic granules of uniform size |
|
|
What can cause eosinophilia?
|
- Neoplasia
- Asthma - Allergies - Connective tissue diseases - Parasites (invasive) |
|
|
What do eosinophils produce?
|
- Major basic protein (defends against helminthic infections) |
|
|
What type of cell mediates allergic reactions?
|
Basophilis
|
|
|
What are the contents of basophils?
|
Dense basophilic granules:
- Heparin (anticoagulant) - Histamine (vasodilator) - Leukotrienes |
|
|
What does an isolated basophilia suggest?
|
Uncommon, but can be seen in myeloproliferative disease, particularly CML
|
|
|
What are the functions of mast cells?
|
- Mediates allergic reaction in local tissues
- Can bind to the Fc portion of IgE to membrane - Type I hypersensitivity reactions |
|
|
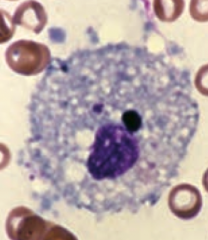
What do mast cells look like?
|
Mast cells resemble basophils structurally and functionally
|
|
|
What is the effect of mast cells on IgE?
|
- Mast cells can bind the Fc portion of IgE to membrane
- IgE cross-links upon antigen binding, causing degranulation, which releases histamine, heparin, and eosinophil chemotactic factors |
|
|
What drug can prevent mast cell degranulation? Function?
|
Cromolyn sodium - used for asthma prophylaxis
|
|
|
What is the function of dendritic cells?
|

Highly phagocytic APCs
- Functions as link between innate and adaptive immune system - Expresses MHC class II and Fc receptor on surface |
|
|
What do dendritic cells express on their surface?
|
- MHC Class II
- Fc receptor |
|
|
What are Langerhans cells?
|
Dendritic cells in the skin
|
|
|
What are the types of lymphocytes?
|
- B cells
- T cells - NK cells |
|
|
What lymphocytes are involved in the adaptive immunity?
|
B cells and T cells
|
|
|
What lymphocytes are involved in the innate immunity?
|
NK cells
|
|
|
What is the appearance of lymphocytes?
|
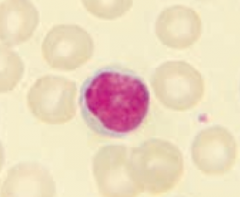
- Round, densely staining nucleus
- Small amount of pale cytoplasm |
|
|
Which cells is part of the humoral immune response? Source? Where does it mature?
|
B lymphocytes
- Arises from stem cells in the bone marrow - Matures in the bone marrow |
|
|
What happens to B cells after they have matured in the bone marrow?
|
Migrates to peripheral lymphoid tissue (follicles of lymph nodes, white pulp of spleen, unencapsulated lymphoid tissue)
|
|
|
What happens when a B lymphocyte encounters an antigen?
|
- B cells differentiate into plasma cells that produce antibodies and memory cells
- Can function as an APC via MHC II |
|
|
What are the cell surface markers of B lymphocytes?
|
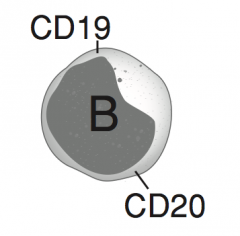
CD19 and CD20
|
|
|
Which cells is part of the cellular immune response? Source? Where does it mature?
|
T lymphocytes
- Originates from stem cells in the bone marrow - Matures in the thymus |
|
|
What happens to T cells after they have matured in the thymus?
|
T cells differentiate into:
- Cytotoxic T cells (express CD8, recognize MHC I) - Helper T cells (express CD4, recognize MHC II) - Regulatory T cells |
|
|
What is necessary for T cell activation?
|
CD28 (costimulatory molecule)
|
|
|
What are the majority of circulating lymphocytes?
|
T cells (80%)
|
|
|
What does CD mean?
|
Cluster of Differentiation
|
|
|
What are the cell surface markers of T lymphocytes?
|
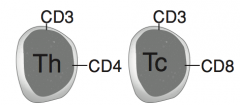
- Helper cells (Th): CD3 and CD4
- Cytotoxic cells (Tc): CD3 and CD8 |
|
|
What is the primary target of HIV?
|
CD4+ Helper T cells
|
|
|
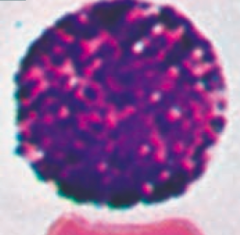
What is the function of plasma cells?
|
Produce large amounts of antibody specific to a particular antigen
|
|
|
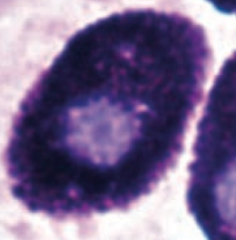
What is the appearance of plasma cells?
|
- Eccentric nucleus
- Clock-face chromatin distribution - Abundant RER - Well-developed Golgi apparatus |
|
|
What is the cancer of plasma cells?
|
Multiple Myeloma
|
|
|
What are the blood group types?
|
- A
- B - AB - O - Rh |
|
|
What kind of antigen and antibodies do patients with blood type A have?
|
- A antigen on RBC surface
- Anti-B antibody in plasma |
|
|
What kind of antigen and antibodies do patients with blood type B have?
|
- B antigen on RBC surface
- Anti-A antibody in plasma |
|
|
What kind of antigen and antibodies do patients with blood type AB have?
|
- A and B antigens on RBC surface
- No antibodies in plasma - Universal recipient of RBCs and universal donor of plasma |
|
|
What kind of antigen and antibodies do patients with blood type O have?
|
- Neither A nor B antigen on RBC surface
- Both A and B antibodies in plasma - Universal donor of RBCs and universal recipient of plasma |
|
|
What blood type if the universal recipient of RBCs?
|
AB
|
|
|
What blood type if the universal donor of RBCs?
|
O
|
|
|
What blood type if the universal recipient of plasma?
|
O
|
|
|
What blood type if the universal donor of plasma?
|
AB
|
|
|
What are the potential implications of an incompatible blood transfusion?
|
- Immunologic response
- Hemolysis - Renal failure - Shock - Death |
|
|
What type of antibodies are the blood group antibodies? Implications for crossing the placenta?
|
- Anti-A and anti-B are IgM antibodies (do not cross placenta)
- Anti-Rh are IgG antibodies (cross placenta) |
|
|
What is the significance of an Rh- mother exposed to fetal Rh+ blood? When?
|
- Often exposure occurs during delivery, mother may make anti-Rh IgG
- If there is a subsequent pregnancy, the anti-Rh IgG can cross the placenta and cause hemolytic disease of the newborn in the next fetus that is Rh+ |
|
|
What causes erythroblastosis fetalis?
|
- If an Rh- mother is exposed to an Rh+ newborn, often occurs during delivery, mother may make anti-Rh IgG
- If there is a subsequent pregnancy, the anti-Rh IgG can cross the placenta and cause hemolytic disease of the newborn in the next fetus that is Rh+ |
|
|
How do you treat an Rh- mother?
|
Rho(D) immune globulin for mother during every pregnancy to prevent initial sensitization of Rh- mother to Rh antigen
|
|
|
What factors are involved in the extrinsic coagulation cascade pathway?
|

- Factor VII activated by Thromboplastin / Tissue Factor to Factor VIIa
- Factor X activated by Factor VIIa to Factor Xa - Factor II (Pro-thrombin) activated by Factor Xa and Va to Factor IIa (Thrombin) - Fibrinogen activated by Thrombin to Fibrin monomers |
|
|
What factors are involved in the intrinsic coagulation cascade pathway?
|

- Factor XII activated by collagen, basement membrane, and activated platelets to XIIa
- Factor XI activated by XIIa to XIa - Factor IX activated by XIa to IXa - Factor X activated by IXa and VIIIa to Xa - Factor II (Prothrombin) activated by Xa and Va to IIa (Thrombin) - Fibrinogen activated by Thrombin to Fibrin monomers |
|
|
What is the effect of Bradykinin?
|

- ↑ Vasodilation
- ↑ Permeability - ↑ Pain |
|
|
What molecule causes the fibrin / platelet plug to break down to fibrin degradation products?
|
Plasmin
|
|
|
What is Hemophilia A?
|
Deficiency of Factor VIII
|
|
|
What is Hemophilia B?
|
Deficiency of Factor IX
|
|
|
What forms the fibrin clot?
|

- Fibrin monomers aggregate with Ca2+ and Factor XIIIa to form a fibrin meshwork
- Fibrin mesh acts to stabilize platelet plug |
|
|
What enzyme converts oxidized vitamin K to reduced vitamin K?
|
Epoxide Reductase
|
|
|
What is the function of reduced vitamin K?
|
Acts as a cofactor to activate the coagulation cascade precursors: II, VII, IX, X, and Protein C and S
|
|
|
What is the mechanism of Warfarin?
|

Warfarin inhibits the enzyme vitamin K epoxide reductase
|
|
|
Why do neonates require Vitamin K injections when they are born?
|
- Neonates lack enteric bacteria, which produce vitamin K
- Vitamin K is necessary for maturing coagulation cascade components |
|
|
What are the implications of a Vitamin K deficiency?
|
↓ Synthesis of factors II, VII, IX, X, protein C, and protein S
|
|
|
What carries / protects Factor VIII?
|
von Willebrand Factor
|
|
|
What is the action of Protein C?
|
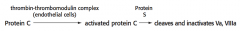
Cleaves and inactivates factors Va and VIIIa
|
|
|
How does Protein C get activated to exert its inactivating effects on Factors Va and VIIIa?
|
- Protein C converted to Activated Protein C via thrombin-thrombomodulin complex (on endothelial cells)
- Protein S helps allow activated Protein C to exert its effects |
|
|
What happens in fibrinolysis?
|
- Cleavage of fibrin mesh
- Destruction of coagulation factors |
|
|
What mediates fibrinolysis?
|
Plasminogen activation to Plasmin mediates Fibrinolysis
|
|
|
What medication can help activate Plasminogen to Plasmin? Utility?
|
tPA - used as a thrombolytic
|
|
|
What is the action of Antithrombin?
|
Inhibits activated forms of factor II, VII, IX, X, XI, and XII
|
|
|
What is the action of Heparin?
|
Heparin enhances the activity of antithrombin; antithrombin inhibits activated forms of factor II, VII, IX, X, XI, and XII
|
|
|
What are the principal targets of antithrombin?
|
Thrombin and Factor Xa
|
|
|
What is the effect of the Factor V Leiden mutation?
|
Produces a factor V resistant to inhibition by activated Protein C
|
|
|
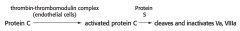
What are the steps of platelet plug formation (primary hemostasis)?
|
1. Injury
2. Adhesion 3. Activation 4. Aggregation |
|
|
What is the first step of platelet plug formation (primary hemostasis)?
|
Injury
- vWF binds to exposed collagen upon endothelial damage |
|
|
What is the second step of platelet plug formation (primary hemostasis), after injury?
|
Adhesion:
- Platelets bind vWF via GpIb receptor at the site of injury only (specific) - Platelets release ADP and Ca2+ (necessary for coagulation cascade) - ADP helps platelet adhere to endothelium |
|
|
What is the third step of platelet plug formation (primary hemostasis), after adhesion?
|
Activation
- ADP binding to receptor induces GpIIb/IIIa expression at platelet surface |
|
|
What is the fourth step of platelet plug formation (primary hemostasis), after activation?
|
Aggregation
- Fibrinogen binds GpIIb/IIIa receptors and links platelets - Temporary plug stops bleeding |
|
|
What are the pro-aggregation factors?
|

- TXA2 (released by platelets)
- ↓ Blood flow - ↑ Platelet aggregation |
|
|
What are the anti-aggregation factors?
|
- PGI2 and NO (released by endothelial cells)
- ↑ Blood flow - ↓ Platelet aggregation |
|
|
What is the mechanism of aspirin?
|
Inhibits cyclooxygenase (TXA2 synthesis)
|
|
|
What is the mechanism of ticlopidine?
|
Inhibits ADP-induced expression of GpIIb/IIIa
|
|
|
What is the mechanism of clopidogrel?
|
Inhibits ADP-induced expression of GpIIb/IIIa
|
|
|
What is the mechanism of abciximab?
|
Inhibits GpIIb/IIIa directly
|
|
|
What is the mechanism of ristocetin?
|
Activates vWF to bind to GpIb
|
|
|
What is useful for diagnosis of von Willebrand disease?
|
Normal platelet aggregation response is not seen in von Willebrand disease
|
|
|
What disease occurs if there is a deficiency of GpIb?
|
Bernard-Soulier Syndrome
|
|
|
What disease occurs if there is a deficiency of GpIIb/IIIa?
|
Glanzmann Thombasthenia
|
|
|
What molecules are inside of endothelial cells?
|
- vWF
- Thromboplastin - tPA and PGI2 |
|
|
What can acute phase reactants in the plasma lead to?
|
RBC aggregation, thereby ↑ RBC sedimentation rate (RBC aggregates have a higher density than plasma)
|
|
|
What causes an increased erythrocyte sedimentation rate (ESR)?
|
- Infections
- Autoimmune diseases (SLE, rheumatoid arthritis, temporal arteritis) - Malignant neoplasms - GI disease (ulcerative colitis) - Pregnancy |
|
|
What causes a decreased erythrocyte sedimentation rate (ESR)?
|
- Polycythemia
- Sickle cell anemia - CHF - Microcytosis - Hypofibrinogenemia |

