![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
85 Cards in this Set
- Front
- Back
|
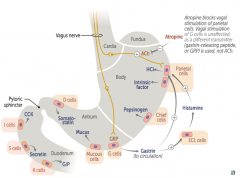
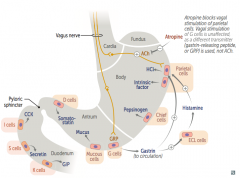
What are the GI regulatory and secretory substances released in the stomach? |
Regulatory:
- Gastrin Secretory: - Intrinsic Factor - Gastric acid - Pepsin - HCO3- |
|
|
What are the GI regulatory and secretory substances released in the duodenum?
|
Regulatory:
- Cholecystokinin - Glucose-dependent insulinotropic peptide - Motilin - Secretin - VIP Secretory: - HCO3- |
|
|
What are the GI regulatory and secretory substances released in the jejunum?
|
Regulatory:
- Cholecystokinin - Glucose-dependent insulinotropic peptide - Motilin - VIP |
|
|
What are the GI regulatory and secretory substances released in the ileum?
|
Regulatory:
- Motilin - VIP |
|
|
What is the source of Cholecystokinin?
|
I cells (duodenum and jejunum)
|
|
|
What is the source of Gastrin?
|
G cells (antrum of stomach)
|
|
|
What is the source of Glucose-dependent insulinotropic peptide?
|
K cells (duodenum and jejunum)
|
|
|
What is the source of Motilin?
|
Small intestine
|
|
|
What is the source of Secretin?
|
S cells (duodenum)
|
|
|
What is the source of Somatostatin?
|
D cells (pancreatic islets and GI mucosa)
|
|
|
What is the source of Vasoactive Intestinal Peptide (VIP)?
|
- Parasympathetic ganglia in sphincters
- Gallbladder - Small intestine |
|
|
What is the source of Intrinsic Factor?
|
Parietal cells in stomach
|
|
|
What is the source of gastric acid?
|
Parietal cells in stomach
|
|
|
What is the source of Pepsin?
|
Chief cells in stomach
|
|
|
What is the source of HCO3-?
|
- Mucosal cells in stomach, duodenum, salivary glands, pancreas
- Brunner glands in duodenum |
|
|
What is secreted from I cells? Location? Action?
|
Cholecystokinin - duodenum and jejunum
- ↑ pancreatic secretion - ↑ gallbladder contraction - ↓ gastric emptying - ↑ sphincter of Oddi relaxation |
|
|
What is secreted from G cells? Location? Action?
|
Gastrin - antrum of stomach
- ↑ gastric H+ secretion - ↑ growth of gastric mucosa - ↑ gastric motility |
|
|
What is secreted from K cells? Location? Action?
|
Glucose-dependent insulinotropic peptide - duodenum and jejunum
- Exocrine: ↓ gastric H+ secretion - Endocrine: ↑ insulin release |
|
|
What is the action of Motilin? Source?
|
Motilin - small intestine
- Produces migrating motor complexes (MMCs) |
|
|
What is secreted from S cells? Location? Action?
|
Secretin - duodenum
- ↑ pancreatic HCO3- secretion - ↓ gastric acid secretion - ↑ bile secretion |
|
|
What is secreted from D cells? Location? Action?
|
Somatostatin - pancreatic islets and GI mucosa
- ↓ gastric acid and pepsinogen secretion - ↓ pancreatic and small intestine fluid secretion - ↓ gallbladder contraction - ↓ insulin and glucagon release |
|
|
What is the action of Nitric Oxide in the GI tract?
|
↑ smooth muscle relaxation, including LES
|
|
|
What is the action of Vasoactive Intestinal Peptide (VIP)? Source?
|
Parasympathetic ganglia in sphincters, gallbladder, and small intestine:
- ↑ intestinal water and electrolyte secretion - ↑ relaxation of intestinal smooth muscle and sphincters |
|
|
What is secreted from Parietal cells? Location? Action?
|
Intrinsic Factor - stomach
- Vitamin B12 binding protein (required for B12 uptake in terminal ileum) Gastric Acid - stomach - ↓ stomach pH |
|
|
What is secreted from Chief cells? Location? Action?
|
Pepsin - stomach
- Protein digestion |
|
|
What is secreted from mucosal cells and Brunner glands? Location? Action?
|
HCO3-
- Mucosal cells in stomach, duodenum, salivary glands, and pancreas - Brunner glands in duodenum - Acts to neutralize acid |
|
|
Which regulatory substance ↑ pancreatic secretion, ↑ gallbladder contraction, ↓ gastric emptying, and ↑ sphincter of Oddi relaxation? Source? Regulation? Other?
|
- Cholecystokinin (from I cells in duodenum and jejunum)
- Regulation: ↑ by fatty acids and amino acids - CCK acts on neural muscarinic pathways to cause pancreatic secretion |
|
|
Which regulatory substance ↑ gastric H+ secretion, ↑ growth of gastric mucosa, and ↑ gastric motility? Source? Regulation? Other?
|
- Gastrin (from G cells in antrum of stomach)
- Regulation: ↑ by stomach distention/alkalinization, amino acids, peptides, and vagal stimulation; ↓ if stomach pH <1.5 - Phenylalanine and troptophan are potent stimulators - Gastrin ↑↑ in Zollinger-Ellison Syndrome - Gastrin ↑ by chronic PPI use |
|
|
Which regulatory substance ↓ gastric H+ secretion (exocrine) and ↑ insulin release (endocrine)? Source? Regulation? Other?
|
Glucose-dependent insulinotropic peptide (aka Gastric Inhibitory Peptide = GIP)
- From K cells in duodenum and jejunum - Regulation: ↑ by fatty acids, amino acids, and oral glucose - Oral glucose load is used more rapidly than the equivalent given by IV due to GIP secretion |
|
|
Which regulatory substance produces migrating motor complexes (MMCs)? Source? Regulation? Other?
|
Motilin - from small intestine
- Regulation: ↑ in fasting state - Motilin receptor agonists (eg, erythromycin) are used to stimulate intestinal peristalsis |
|
|
Which regulatory substance ↑ pancreatic HCO3-, ↓ gastric acid secretion, and ↑ bile secretion? Source? Regulation? Other?
|
Secretin - from S cells in duodenum
- Regulation: ↑ by acid and fatty acids in lumen of duodenum - ↑ HCO3- neutralizes gastric acid in duodenum, allowing pancreatic enzymes to function |
|
|
Which regulatory substance ↓ gastric acid and pepsinogen secretion, ↓ pancreatic and SI fluid secretion, ↓ GB contraction, and ↓ insulin and glucagon release? Source? Regulation? Other?
|
Somatostatin - from D cells in pancreatic islets and GI mucosa
- Regulation: ↑ by acid and ↓ by vagal stimulation - Inhibitory hormone - Antigrowth hormone effects (inhibits digestion and absorption of substances needed for growth) |
|
|
Which regulatory substance ↑ smooth muscle relaxation including that of the LES? Other?
|
Nitric Oxide
- Loss of NO secretion is implicated in ↑ LES tone of achalasia |
|
|
Which regulatory substance ↑ intestinal water and electrolyte secretion and ↑ relaxation of intestinal smooth muscle and sphincters? Source? Regulation? Other?
|
Vasoactive Intestinal Polypeptide (VIP)
- Source: parasympathetic ganglia in sphincters, GB, and SI - Regulation: ↑ by distention and vagal stimulation, ↓ by adrenergic input - VIPoma: non-α, non-β islet cell pancreatic tumor that secretes VIP → copious Watery Diarrhea, Hypokalemia, and Achlorhydria = WDHA syndrome |
|
|
What is WDHA syndrome?
|
Watery Diarrhea, Hypokalemia, and Achlorhydria:
- Caused by VIPoma, a non-α, non-β islet cell pancreatic tumor that secretes VIP - VIP ↑ intestinal water and electrolyte secretion, as well as ↑ relaxation of intestinal smooth muscle and sphincters |
|
|
Which secretory substance is responsible for binding vitamin B12 (required for B12 uptake in terminal ileum)? Source? Other?
|
Intrinsic factor
- Released from parietal cells in stomach - Auto-immune destruction of parietal cells → chronic gastritis and pernicious anemia |
|
|
Which secretory substance ↓ stomach pH? Source? Regulation? Other?
|
Gastric Acid
- Released from parietal cells in stomach - Regulation: ↑ by histamine, ACh, and gastrin; ↓ by somatostatin, GIP, prostaglandin, and secretin - Gastrinoma: gastrin-secreting tumor that causes high levels of acid secretion and ulcers refractory to medical therapy |
|
|
Which secretory substance is responsible for protein digestion? Source? Regulation? Other?
|
Pepsin
- Released from chief cells in stomach - Regulation: ↑ by vagal stimulation and local acid - Inactive pepsinogen → active pepsin via H+ |
|
|
Which secretory substance neutralizes acid? Source? Regulation? Other?
|
HCO3-
- Released from mucosal cells in stomach, duodenum, salivary glands, and pancreas - Released from Brunners glands in duodenum - Regulation: ↑ by pancreatic and biliary secretion with secretin - HCO3- is trapped in mucus that covers the gastric epithelium |
|
|
Which substance is ↑↑ in Zollinger-Ellison syndrome? Action?
|
Gastrin
- ↑ gastric H+ secretion - ↑ growth of gastric mucosa - ↑ gastric motility |
|
|
Which substance is ↑ with chronic use of PPIs? Action?
|
Gastrin
- ↑ gastric H+ secretion - ↑ growth of gastric mucosa - ↑ gastric motility |
|
|
Which drug is a motilin receptor agonist? Action?
|
Erythromycin
- Used to stimulate intestinal peristalsis - Motilin produces migrating motor complexes (MMCs) |
|
|
Which substance is ↑ in VIPoma? Action?
|
Vasoactive Intestinal Polypeptide (VIP)
- ↑ intestinal water and electrolyte secretion - ↑ relaxation of intestinal smooth muscle and sphincters - Leads to copious Watery Diarrhea, Hypokalemia, and Achlorhydria (WDHA syndrome) |
|
|
Which substance is ↑ in Gastrinoma? Action?
|
Gastrin
- Causes high levels of acid secretion and ulcers refractory to medical therapy |
|
|
Which secretory cells are found in the body of the stomach? Action?
|
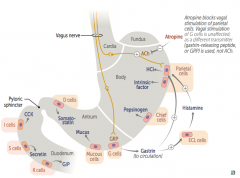
- Parietal cells: release HCl and Intrinsic Factor
- Chief cells: release pepsinogen |
|
|
Which secretory cells are found in the antrum (bottom) of the stomach? Action?
|
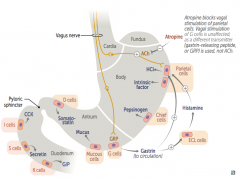
- G cells: release Gastrin to circulation
- Mucous cells: release mucus - D cells: release Somatostatin |
|
|
Which secretory cells are found in the duodenum?
|
- I cells: release CCK
- S cells: release Secretin - K cells: release GIP |
|
|
What is the action of ECL cells? Regulation?
|
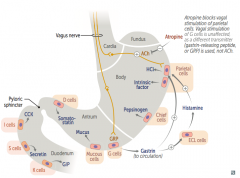
- Release Histamine → activates parietal cells in body of stomach to release HCl and Intrinsic Factor
- Stimulated by Gastrin (from G cells) |
|
|
How does gastrin increase acid secretion?
|
- Primarily through its effects on Enterochromaffin-Like (ECL) cells → release histamine which stimulates Parietal cells
- Also directly stimulates Parietal cells |
|
|
Which receptors are found on gastric parietal cells? What do they bind?
|
- M3 receptor - binds ACh
- CCK-B receptor - binds Gastrin - H2 receptor - binds Histamine - Other receptors that bind prostaglandins/misoprostol and somatostatin |
|
|
What is the action/mechanism of the Vagus nerve on the gastric parietal cell?
|
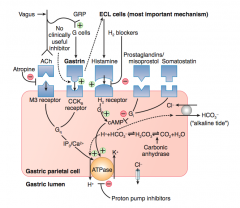
- Releases ACh which stimulates the M3 receptor
- Stimulates Gq → IP3 and Ca2+ → stimulates ATPase on gastric lumen to secrete H+ - Stimulates G cells via GRP to release Gastrin - Gastrin binds to CCK-B receptor - Stimulates Gq → IP3 and Ca2+ → stimulates ATPase on gastric lumen to secrete H+ |
|
|
What is the action/mechanism of the ECL cells on the gastric parietal cell?
|
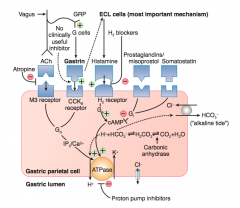
- ECL cells are stimulated by gastrin to release Histamine
- Histamine binds H2 receptor on parietal cell - Stimulates Gs → cAMP → stimulates ATPase on gastric lumen to secrete H+ |
|
|
What is the action/mechanism of the prostaglandins / misoprostol on the gastric parietal cell?
|
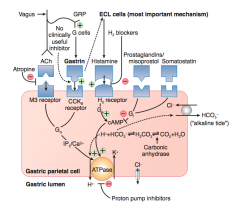
- Binds to receptor on parietal cell
- Stimulates Gi → ↓ cAMP → no activation of ATPase on gastric lumen to secrete H+ |
|
|
What is the action/mechanism of somatostatin on the gastric parietal cell?
|
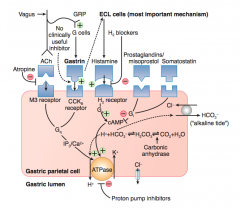
- Binds to receptor on parietal cell
- Stimulates Gi → ↓ cAMP → no activation of ATPase on gastric lumen to secrete H+ |
|
|
How can you inhibit the gastric parietal cell from releasing acid, pharmacologically?
|
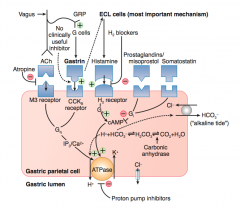
- Atropine: inhibits ACh activation of M3 receptor
- H2 blockers: inhibits Histamine activation of H2 receptor - Proton Pump Inhibitors: inhibits H+/K+ ATPase on gastric lumen of parietal cell |
|
|
What is the function and location of Brunner glands?
|
- Secrete alkaline mucus (hypertrophy seen in peptic ulcer disease)
- Located in duodenal submucosa |
|
|
Which histologic sign would you see in peptic ulcer disease?
|
Hypertrophy of Brunner glands in duodenal submucosa (act to secrete alkaline mucus)
|
|
|
What are the characteristics of pancreatic secretions?
|
- Isotonic fluid
- Low flow → high Cl- - High flow → high HCO3- |
|
|
What enzymes are released by the pancreas?
|
- α-amylase
- Lipase, Phospholipase A, Colipase - Proteases - Trypsinogen |
|
|
What is the action of α-amylase? Source? Other?
|
- Starch digestion
- From pancreas - Secreted in active form |
|
|
Which pancreatic secretions are involved in fat digestion?
|
- Lipase
- Phospholipase A - Colipase |
|
|
Which pancreatic secretions are involved in protein digestion?
|
Proteases secreted as proenzymes (aka zymogens)
- Trypsin - Chymotrypsin - Elastase - Carboxypeptidase |
|
|
What is the action of Trypsinogen? Source?
|
- Converted to active enzyme Trypsin → activates other proenzymes and cleaves additional Trypsinogen molecules into active Trypsin (positive feedback loop)
- From pancreas |
|
|
How does Trypsinogen get activated to Trypsin?
|
- Enterokinase / Enteropeptidase - brush-border enzymes on duodenal and jejunal mucosa
- Activated Trypsin can also self-activate more Trypsinogen molecules (positive feedback loop) |
|
|
How are carbohydrates absorbed?
|
- Only monosaccharides (glucose, galactose, and fructose) are absorbed by enterocytes
- Glucose and Galactose are taken up by SGLT1 (Na+ dependent) - Fructose taken up by facilitated diffusion by GLUT-5 - All transported to blood by GLUT-2 |
|
|
What is the action of SGLT1?
|
Na+ dependent uptake up Glucose and Galactose on lumenal border of enterocytes
|
|
|
What is the action of GLUT-5?
|
Facilitated diffusion uptake of Fructose on lumenal border of enterocytes
|
|
|
What is the action of GLUT-2?
|
Transports Galactose, Glucose, and Fructose into blood from enterocytes
|
|
|
What test distinguishes GI mucosal damage from other causes of malabsorption?
|
D-xylose absorption test
|
|
|
What is the function of the D-xylose absorption test?
|
Distinguishes GI mucosal damage from other causes of malabsorption
|
|
|
Which important vitamins/minerals are absorbed in the small intestine? Which part?
|
- Iron (Fe2+) in duodenum
- Folate in jejunum and ileum - B12 in terminal ileum along with bile acids, requires intrinsic factor |
|
|
What are Peyer Patches? Location?
|
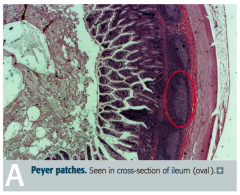
- Unencapsulated lymphoid tissue
- Found in lamina propria and submucosa of ileum |
|
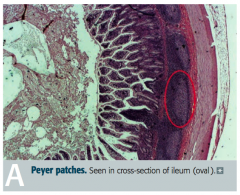
What takes place in Peyer Patches?
|
- Specialized M cells sample and present antigens to immune cells
- B cells stimulated in germinal centers differentiate into IgA-secreting plasma cells - Plasma cells ultimately reside in lamina propria - IgA receives protective secretory component and is then transported across the epithelium to gut to deal with intraluminal antigen |
|
|
Which antibody is important in the gut?
|
IgA = the Intra-gut Antibody
Always say SECRETORY IgA - this is important so it can be transported into the gut out of the Peyer patch to deal with the intraluminal antigen |
|
|
What are the contents of bile?
|
- Bile salts (bile acids conjugated to glycine or taurine)
- Phospholipids - Cholesterol - Bilirubin - Water - Ions |
|
|
How are bile salts made? Why?
|
- Bile acids are conjugated to glycine or taurine to form bile salts
- This makes them water soluble |
|
|
What enzyme catalyzes the rate-limiting step of bile synthesis?
|
Cholesterol 7α-hydroxylase
|
|
|
What are the functions of bile?
|
- Digestion and absorption of lipids and fat-soluble vitamins
- Cholesterol excretion (body's only means of eliminating cholesterol) - Antimicrobial activity (via membrane disruption) |
|
|
What is bilirubin made from?
|

Product of heme metabolism - removed from blood by liver, conjugated with glucuronate, and excreted inb ile
|
|
|
What are the two forms of bilirubin? Difference?
|
- Direct bilirubin: conjugated with glucuronic acid, water soluble
- Indirect bilirubin: unconjugated, water insoluble |
|
|
How is unconjugated bilirubin made?
|
Takes place in macrophages:
RBCs → Heme → Unconjugated bilirubin |
|
|
How is conjugated bilirubin made?
|
- Unconjugated/indirect bilirubin (from macrophages) is bound to albumin to travel in bloodstream to liver
- Once in liver, it is conjugated via UDP-glucuronosyl-transferase to Direct Bilirubin |
|
|
What happens to conjugated bilirubin made in the liver?
|
- Released into gut
- Gut bacteria convert it to Urobilinogen - 80% of urobilinogen is excreted in feces as Stercobilin (giving it brown color) - 2% sent to kidney and excreted as Urobilin (giving it yellow color) - 18% sent through enterohepatic circulation back to liver |
|
|
What form of bilirubin is excreted in feces?
|
Stercobilin
- Conjugated bilirubin → Urobilinogen via gut bacteria - Urobilinogen → Stercobilin (excreted in feces giving stool its brown color) |
|
|
What form of bilirubin is excreted in urine?
|
Urobilin
- Conjugated bilirubin → Urobilinogen via gut bacteria - Urobilinogen → Urobilin (excreted in urine giving it its yellow color) |

