![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
431 Cards in this Set
- Front
- Back
|
What are the types of tumors in the salivary glands? |
- Pleomorphic adenoma
- Warthin tumor - Mucoepidermoid carcinoma |
|
|
Where are salivary gland tumors usually located? Benign or malignant?
|
- Most occur in parotid gland
- Generally benign (except mucoepidermoid carcinoma) |
|
|
What is the most common salivary gland tumor?
|
Pleomorphic Adenoma (benign mixed tumor)
|
|
|
Which tumor presents as a painless, mobile mass, in a salivary gland? What does it consist of?
|
Pleomorphic Adenoma (benign mixed tumor)
- Chondromyxoid stroma and epithelium |
|
|
What is the treatment and prognosis for Pleomorphic Adenoma of the salivary gland?
|
- Can recur if incompletely excised or ruptured intraoperatively
- Benign |
|
|
Which tumor presents as a cystic tumor with germinal centers in a salivary gland?
|
Warthin Tumor (papillary cystadenoma lymphomatosum)
- Benign cystic tumor |
|
|
What are the characteristics of a Warthin tumor?
|
- Benign cystic tumor with germinal centers
- Papillary cystadenoma lymphomatosum |
|
|
What is the most common malignant tumor of the salivary glands?
|
Mucoepidermoid Carcinoma
|
|
|
Which tumor presents as a painless, slow-growing mass in a salivary gland? Contents?
|
Mucoepidermoid Carcinoma -
- Most common malignant tumor of salivary glands - Mucinous and squamous components |
|
|
What are the characteristics of a Mucoepidermoid Carcinoma?
|
- Most common malignant tumor of salivary glands
- Mucinous and squamous components - Typically presents as a painless, slow-growing mass |
|
|
What is the term for the failure of relaxation of the lower esophageal sphincter with uncoordinated peristalsis?
|
Achalasia
|
|
|
What are the characteristics of Achalasia? Cause?
|
- Failure of relaxation of LES due to loss of myenteric (Auerbach) plexus
- High LES opening pressure and uncoordinated peristalsis → progressive dysphagia to solids and liquids (vs obstruction - solids only) - May also be secondary to Chagas disease |
|
|
Which test can be used to assess for the presence of Achalasia? Results?
|

Barium Swallow Test = shows "bird's beak" - dilated esophagus with an area of distal stenosis
|
|

A patient presents with dysphagia to solids and liquids; a barium swallow test shows a "bird's beak" appearance. What is the most likely diagnosis? What is this patient at risk for?
|
Achalasia
- At increased risk for esophageal squamous cell carcinoma |
|
|
What may 2° Achalasia be caused by?
|
Chagas disease
|
|
|
Which pathology causes transmural, usually distal esophageal rupture, due to violent retching? Treatment?
|
Boerhaave Syndrome
- Surgical emergency |
|
|
Which pathology leads to dysphagia, heartburn, and strictures in response to food allergen exposure in atopic patients who are unresponsive to GERD therapy? Characteristics?
|
Eosinophilic Esophagitis
- Infiltration of eosinophils in the esophagus |
|
|
Which pathology is associated with lye ingestion and acid reflux?
|
Esophageal strictures
|
|
|
Which pathology causes painless bleeding of the esophagus? Characteristics?
|
Esophageal Varices
- Bleeding occurs in dilated submucosal veins in lower 1/3 of esophagus - Secondary to portal hypertension |
|
|
Which esophageal pathology is caused by portal hypertension?
|
Esophageal Varices
- Painless bleeding occurs in dilated submucosal veins in lower 1/3 of esophagus |
|
|
Which pathology is associated with reflux, infection in immunocompromised, or chemical ingestion?
|
Esophagitis
|
|
|
What cause cause Esophagitis?
|
- Reflux
- Infection in immunocompromised: Candida, HSV-1, or CMV - Chemical ingestion |
|
|
Which pathology causes white pseudomembranes to form on the esophagus (esophagitis)? Who is it at risk for this?
|
Candida
- Occurs in immunocompromised patients |
|
|
Which pathology causes "punched-out" ulcers to form on the esophagus (esophagitis)? Who is it at risk for this?
|
HSV-1
- Occurs in immunocompromised patients |
|
|
Which pathology causes "linear" ulcers to form on the esophagus (esophagitis)? Who is it at risk for this?
|
CMV
- Occurs in immunocompromised patients |
|
|
Which pathology commonly presents as heartburn and regurgitation upon lying down, may also present with nocturnal cough and dyspnea (adult-onset asthma)? Characteristics?
|
Gastroesophageal Reflux Disease (GERD)
- Decrease in LES tone |
|
|
Which pathology causes mucosal lacerations at the gastroesophageal junction due to severe vomiting? Characteristics?
|
Mallory-Weiss Syndrome
- Leads to hematemesis - Usually found in alcoholics and bulimics |
|
|
Which pathology causes hematemesis in alcoholics and bulimics?
|
Mallory-Weiss Syndrome
- Mucosal lacerations at the gastroesophageal junction due to severe vomiting |
|
|
Which pathology causes dysphagia, iron deficiency anemia, and glossitis?
|
Plummer-Vinson Syndrome
- "Plumbers" DIG: Dysphagia, Iron deficiency anemia, and Glossitis - Dysphagia is due to esophageal webs |
|
|
Which pathology causes acid reflux and dysphagia, which leads to stricture, Barrett esophagus, and aspiration? Characteristics?
|
Sclerodermal Esophageal Dysmotility
- Esophageal smooth muscle atrophy → ↓ LES pressure and dysmotility → acid reflux and dysphagia → stricture, Barrett esophagus, and aspiration - Part of CREST syndrome |
|
|
Which esophageal pathology is part of CREST syndrome?
|
Sclerodermal Esophageal Dysmotility
- Esophageal smooth muscle atrophy → ↓ LES pressure and dysmotility → acid reflux and dysphagia → stricture, Barrett esophagus, and aspiration |
|
|
What happens in Boerhaave Syndrome?
|
- Transmural, usually distal esophagus rupture
- Due to violent retching - Surgical emergency |
|
|
What happens in Eosinophilic Esophagitis?
|
- Infiltration of eosinophils in esophagus of atopic patients
- Food allergens → dysphagia, heartburn, strictures - Unresponsive to GERD therapy |
|
|
What causes Esophageal Strictures?
|
Associated with lye ingestion and acid reflux
|
|
|
What happens with Esophageal Varices? Cause?
|
- Painless bleeding of dilated submucosal veins in lower 1/3 of esophagus
- Secondary to portal hypertension |
|
|
What can cause esophagitis?
|
- Reflux
- Infection in immunocompromised host: * Candida (white pseudomembranes) * HSV-1 (punched-out ulcers) * CMV (linear ulcers) - Chemical ingestion |
|
|
What happens in Gastroesophageal Reflux Disease?
|
- Commonly presents as heartburn and regurgitation upon lying down
- May also present with nocturnal cough and dyspnea, adult-onset asthma - Decrease in LES tone |
|
|
What happens in Mallory-Weiss Syndrome?
|
- Mucosal lacerations at the gastroesophageal junction due to severe vomiting
- Leads to hematemesis - Usually found in alcoholics and bulimics |
|
|
What happens in Plummer-Vinson Syndrome?
|
Triad of (Plumber's DIG):
- Dysphagia (due to esophageal webs) - Iron deficiency anemia - Glossitis |
|
|
What happens in Sclerodermal Esophageal Dysmotility?
|
- Esophageal smooth muscle atrophy → ↓ LES pressure and dysmotility → acid reflux and dysphagia → stricture, Barrett esophagus, and aspiration
- Part of CREST syndrome |
|
|
What change occurs in Barrett Esophagus?
|
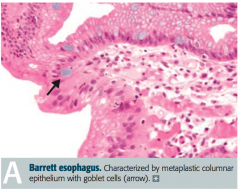
Glandular metaplasia: replacement of non-keratinized (stratified) squamous epithelium with intestinal epithelium (non-ciliated columnar with goblet cells) in distal esophagus
|
|
|
What causes Barrett Esophagus? Risks?
|
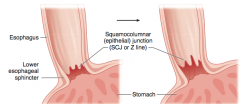
- Caused by chronic acid reflux (GERD)
- Associated with esophagitis, esophageal ulcers, and ↑ risk esophageal adenocarcinoma |
|
|
In a patient with chronic GERD, what do you need to be worried about them potentially developing?
|
- Increased risk for Barrett's esophagus
- Patients with Barrett's esophagus are at increased risk for esophagitis, esophageal ulcers, and esophageal adenocarcinoma |
|
|
What are the types of esophageal cancer?
|
- Squamous cell carcinoma
- Adenocarcinoma |
|
|
If your patient presents with progressive dysphagia (first solids, then liquids) and weight loss, what should you suspect? Prognosis?
|
Esophageal cancer (either squamous cell carcinoma or adenocarcinoma)
- Poor prognosis |
|
|
What are the risk factors for esophageal cancer?
|
AABCDEFFGH:
- Achalasia - Alcohol (squamous cell) - Barrett esophagus (adeno) - Cigarettes (both) - Diverticula (eg, Zenker) (squamous) - Esophageal web (squamous) - Familial - Fat/Obesity (adeno) - GERD (adeno) - Hot liquids (squamous) |
|
|
What are the risk factors for squamous cell carcinoma of the esophagus?
|
- Achalasia
- Alcohol - Cigarettes - Diverticula (eg, Zenker) - Esophageal web - Familial - Hot liquids |
|
|
What are the risk factors for adenocarcinoma of the esophagus?
|
- Achalasia
- Barrett esophagus (adeno) - Cigarettes - Familial - Fat/Obesity - GERD |
|
|
What are the differences between squamous cell carcinoma and adenocarcinoma in terms of prevalence and location in esophagus?
|
Squamous Cell Carcinoma
- More common worldwide - Upper 2/3 Adenocarcinoma - More common in US - Lower 1/3 |
|
|
Which type of cancer more commonly affects the upper part of the esophagus?
|
Squamous cell carcinoma
|
|
|
Which type of cancer more commonly affects the lower part of the esophagus?
|
Adenocarcinoma
|
|
|
What are the types of gastritis?
|
- Acute gastritis (erosive)
- Chronic gastritis (non-erosive): type A (fundus/body) and type B (antrum) |
|
|
What causes acute gastritis?
|
Disruption of mucosal barrier → inflammation:
- Stress * NSAIDs (↓ PGE2 → ↓ gastric mucosa protection) * Alcohol - Uremia - Burns (Curling ulcer: ↓ plasma volume → sloughing of gastric mucosa) - Brain injury (Cushing ulcer: ↑ vagal stimulation → ↑ ACh → ↑ H+ production) |
|
|
What is a Curling ulcer? What does it lead to?
|
- Curling ulcer is caused by burns (think burned by the curling iron)
- Leads to ↓ plasma volume → sloughing of gastric mucosa - Cause of acute gastritis |
|
|
What is a Cushing ulcer? What does it lead to?
|
- Cushing ulcer is caused by brain injury (think always cushion the brain)
- Leads to ↑ vagal stimulation → ↑ ACh → ↑ H+ production - Cause of acute gastritis |
|
|
What is especially common among alcoholics and patients taking daily NSAIDs (eg, patients with rheumatoid arthritis)?
|
Acute Gastritis (erosive)
|
|
|
What is the name of the auto-immune disorder characterized by auto-antibodies to parietal cells? What does this lead to?
|
Chronic gastritis (type A - in fundus/body)
- Leads to pernicious Anemia and Achlorhydria - Associated with other auto-immune disorders |
|
|
What is the name of disorder caused by H. pylori infection? What are you at risk for?
|
Chronic gastritis (type B - in antrum)
- Most common type of chronic gastritis - Increased risk for MALT lymphoma and gastric adenocarcinoma |
|
|
Which type of chronic gastritis affects the fundus, body, and antrum?
|
- Type A (auto-immune): affects fundus / body
- Type B (H. pylori): affects antrum |
|
|
What are the characteristics of type A chronic gastritis?
|
- Affects the fundus/body
- Caused by Auto-Antibodies to parietal cells - Causes pernicious Anemia and Achlorhydria |
|
|
What are the characteristics of type B chronic gastritis?
|
- Most common type
- Affects the antrum - Caused by H. pylori Bacteria infection - Increased risk of MALT lymphoma and gastric adenocarcinoma |
|
|
What disease causes protein loss, parietal cell atrophy, and increased mucus cells?
|
Ménétrier Disease: causes gastric hypertrophy that is so extensive, the rugae of the stomach look like brain gyri
|
|
|
What happens in Ménétrier disease?
|
- Gastric hypertrophy causes protein loss, parietal cell atrophy, and increased mucus cells
- Precancerous!! - Rugae of stomach are so hypertrophied that they look like brain gyri |
|
|
What is the most common kind of stomach cancer?
|
Almost always adenocarcinoma
|
|
|
What are the characteristics and types of stomach cancer?
|
- Almost always adenocarcinoma
- Early aggressive local spread and node/liver metastases - Often presents with acanthosis nigricans (brown to black, velvety hyperpigmentation of skin, often in body folds) - Two types: intestinal and diffuse |
|
|
What type of stomach cancer is associated with H. pylori infection, dietary nitrosamines, tobacco smoking, achlorhydria, and chronic gastritis? Location? Appearance?
|
Intestinal adenocarcinoma
- Commonly on lesser curvature - Looks like an ulcer with raised margins |
|
|
What type of stomach cancer is characterized by grossly thickened walls with leathery appearance (linitis plastica)? Other characteristics?
|
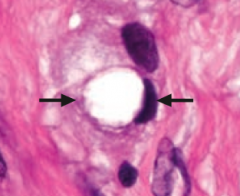
Diffuse adenocarcinoma
- Not associated with H. pylori infection - Signet ring cells on histology |
|
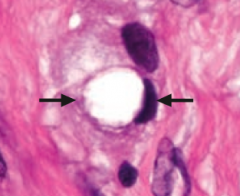
What does this show histologically? Sign of?
|
Signet ring cell - sign of diffuse stomach cancer
- Not associated w/ H. pylori infection - Stomach wall is grossly thickened and leathery (linitis plastica) |
|
|
What is the term for a thickened and leathery stomach wall?
|
Linitis plastica
|
|
|
What is intestinal stomach adenocarcinoma associated with?
|
- H. pylori infection
- Dietary nitrosamines (smoked foods) - Tobacco smoking - Achlorhydria - Chronic gastritis (auto-antibodies would cause achlorhydria) |
|
|
In what patterns does stomach cancer spread?
|
- Virchow node (L supraclavicular node)
- Krukenberg tumor (ovaries) - Sister Mary Joseph nodule (periumbilial) |
|
|
What is the name for the involvement of the L supraclavicular node by metastasis from the stomach?
|
Virchow Node
|
|
|
What is the name for the bilateral metastases to the ovaries? Sign?
|
Krukenberg Tumor - abundant mucus and signet ring cells (occurs in diffuse stomach cancer)
|
|
|
What is the name for the subcutaneous periumbilical metastasis?
|
Sister Mary Joseph Nodule - occurs in metastasis of stomach cancer
|
|
|
Peptic ulcer disease can affect what areas of the GI tract?
|
- Gastric ulcer (stomach)
- Duodenal ulcer |
|
|
How do Gastric and Duodenal ulcers compare in terms of pain?
|
- Gastric: can be greater with meals → weight loss
- Duodenal: decreases with meals → weight gain |
|
|
How do Gastric and Duodenal ulcers compare in terms of the presence of H. pylori infection?
|
- Gastric: in 70%
- Duodenal: in almost 100% |
|
|
How do Gastric and Duodenal ulcers compare in terms of the mechanism of ulceration?
|
- Gastric: ↓ mucosal protection against gastric acid
- Duodenal: ↓ mucosal protection or ↑ gastric acid secretion |
|
|
How do Gastric and Duodenal ulcers compare in terms of other causes?
|
- Gastric: NSAIDs
- Duodenal: Zollinger-Ellison syndrome |
|
|
How do Gastric and Duodenal ulcers compare in terms of the risk of carcinoma?
|
- Gastric: increased
- Duodenal: generally benign |
|
|
How do Gastric and Duodenal ulcers compare in terms of who is affected?
|
Gastric: often occurs in older patients
|
|
|
How do Gastric and Duodenal ulcers compare in terms of the effect on Brunner glands?
|
Duodenal: hypertrophy of Brunner glands
|
|
|
Gastric Ulcer:
- Pain - Weight change - H. pylori - Mechanism - Other causes - Risk of carcinoma - Other |
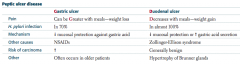
- Pain: can be Greater with meals
- Weight change: weight loss (pain is worse with meals) - H. pylori: in 70% - Mechanism: ↓ mucosal protection from gastric acid - Other causes: NSAIDs - Risk of carcinoma: increased - Other: often occurs in older patients |
|
|
Duodenal ulcer:
- Pain - Weight change - H. pylori - Mechanism - Other causes - Risk of carcinoma - Other |
- Pain: decreases with meals
- Weight change: weight gain (because eating decreases pain) - H. pylori: in almost 100% - Mechanism: ↓ mucosal protection or ↑ gastric acid secretion - Other causes: Zollinger-Ellison syndrome - Risk of carcinoma: generally benign - Other: hypertrophy of Brunner glands |
|
|
What are the potential complications of ulcers?
|
- Hemorrhage
- Perforation |
|
|
Which ulcer complication is more common in gastric ulcers?
|
Hemorrhage
|
|
|
Which ulcer complication is more common in duodenal ulcers?
|
- Perforation (anterior > posterior)
- Hemorrhage (posterior > anterior) |
|
|
If a patient with a gastric ulcer hemorrhages, what is the most likely source of the bleed?
|
Most likely from lesser curvature → bleeding from L gastric artery
|
|
|
If a patient with a duodenal ulcer hemorrhages, what is the most likely source of the bleed?
|
Most likely from posterior wall of duodenum → bleeding from gastroduodenal artery
|
|
|
Perforation as a consequence of a duodenal ulcer is most likely to occur where? Symptoms?
|
- Anterior wall > Posterior wall
- May see free air under diaphragm on CXR - Referred pain to shoulder |
|
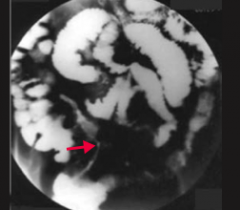
What does this CXR show?
|
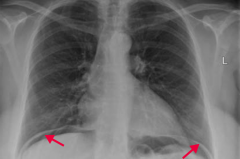
Perforation of duodenal ulcer (anterior wall > posterior wall)
- Leads to free air under the diaphragm - May cause referred pain to shoulder |
|
|
What are the potential consequences of malabsorption syndromes?
|
- Diarrhea
- Steatorrhea - Weight loss - Weakness - Vitamin and mineral deficiencies |
|
|
If your patient presents with diarrhea, steattorhea, weight loss, weakness, and vitamin/mineral deficiencies, what should you consider?
|
Malabsorption Syndromes: "These Will Cause Devastating Absorption Problems"
- Tropical sprue - Whipple disease - Celiac sprue - Disaccharidase deficiency - Abetalipoproteinemia - Pancreatic insufficiency |
|
|
Which malabsorption syndrome should you consider in a patient who recently visited the tropics? Cause? How should they be treated?
|
Tropical Sprue
- Similar to celiac sprue (affects small bowel) - Responds to antibiotics (cause is unknown) |
|
|
Which malabsorption syndrome should you consider in an older man who also presents with cardiac symptoms, arthralgias, and neurologic symptoms? Cause? Other?
|
Whipple Disease
- Infection with Tropheryma whipplei (G+, PAS stain + for foamy macrophages in intestinal lamina propria and mesenteric nodes) *Foamy Whipped cream in a CAN: cardiac sx, arthralgias, neuro sx) |
|
|
Which malabsorption syndrome should you consider in a patient of northern European descent? Cause? How should they be treated?
|
Celiac sprue
- Autoimmune-mediated intolerance of gliadin (wheat) → malabsorption and steatorrhea - Associated with HLA-DQ2 and HLA-DQ8 - Treat with gluten-free diet |
|
|
Which malabsorption syndrome should you consider in a patient intolerant of milk? Symptoms?
|
Disaccharidase deficiency (lactase)
- Osmotic diarrhea - May be self-limited follow an acute injury (eg, viral diarrhea) |
|
|
Which malabsorption syndrome should you consider in a young child with failure to thrive, steatorrhea, acanthocytosis, ataxia, and night blindness? Cause?
|
Abetalipoproteinemia
- ↓ Synthesis of apolipoprotein B → inability to generate chylomicrons → ↓ secretion of cholesterol, VLDL into bloodstream → fat accumulation in enterocytes |
|
|
Which malabsorption syndrome should you consider in a patient with cystic fibrosis?
|
Pancreatic insufficiency
- Causes malabsorption of fat and fat-soluble vitamins (A, D, E, and K) |
|
|
Which malabsorption syndrome should you consider in a patient with obstructing cancer?
|
Pancreatic insufficiency
- Causes malabsorption of fat and fat-soluble vitamins (A, D, E, and K) |
|
|
Which malabsorption syndrome should you consider in a patient with chronic pancreatitis?
|
Pancreatic insufficiency
- Causes malabsorption of fat and fat-soluble vitamins (A, D, E, and K) |
|
|
What are the signs/symptoms of malabsorption syndromes?
|
- Diarrhea
- Steatorrhea - Weight loss - Weakness - Vitamin and mineral deficiencies |
|
|
What are the characteristics of Tropical Sprue?
|
Malabsorption syndrome
- Similar findings as celiac sprue (affects small bowel) - Responds to antibiotics - Cause is unknown, but seen in residents of or recent visitors to tropics |
|
|
What are the characteristics of Whipple disease?
|
Malabsorption syndrome
- Infection with Tropheryma whipplei (G+) - PAS positive for foamy macrophages in intestinal lamina propria - Mesenteric nodes - CAN: Cardiac symptoms, Arthralgias, and Neurologic symptoms common - Most often occurs in older men |
|
|
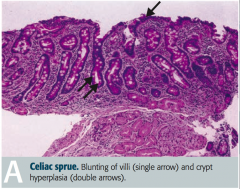
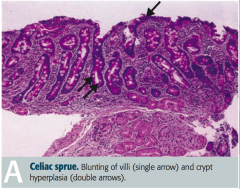
What are the characteristics of Celiac Sprue?
|
Malabsorption syndrome:
- Auto-immune mediated intolerance of gliadin (wheat) → malabsorption and steatorrhea - Associated with HLA-DQ2, HLA-DQ8, and northern European descent - Antibodies: anti-endomysial, anti-tissue transglutaminase, and anti-gliadin antibodies - Blunting of villi and lymphocytes in lamina propria (picture) - ↓ Mucosal absorption, primarily affects distal duodenum and/or proximal jejunum - Diagnosis: serum levels of tissue transglutaminase antibodies - Associated with dermatitis herpetiformis - Moderately ↑ risk of malignancy (eg, T-cell lymphoma) - Treat: gluten-free diet |
|
|
What are the characteristics of Disaccharidase Deficiency?
|
Malabsorption syndrome:
- Most common is lactase deficiency → milk intolerance - Normal-appearing villi - Osmotic diarrhea - Since lactase is located at tips of intestinal villi, self-limited lactase deficiency can occur following injury (eg, viral diarrhea) - Diagnosis: lactose tolerance test (+) if administration of lactose produces symptoms and glucose rises <20 mg/dL |
|
|
What are the characteristics of abetalipoproteinemia?
|
Malabsorption Syndrome:
- ↓ Synthesis of apolipoprotein B → inability to generate chylomicrons → ↓ secretion of cholesterol, VLDL into bloodstream → fat accumulation in enterocytes - Presents in early childhood with failure to thrive, steatorrhea, acanthocytosis (RBCs with spiked membrane), ataxia, and night blindness |
|
|
What are the characteristics of Pancreatic Insufficiency?
|
Malabsorption Syndrome
- Due to cystic fibrosis, obstructing cancer, and chronic pancreatitis - Causes malabsorption of fat and fat-soluble vitamins (A, D, E, and K) - ↑ Neutral fat in stool - Diagnosis: D-xylose absorption test - normal urinary excretion in pancreatic insufficiency; ↓ excretion with intestinal mucosa defects or bacterial overgrowth |
|
|
Which type of malabsorption syndrome is caused by infection?
|
- Tropical Sprue (treat with antibiotics) - cause is unknown
- Whipple Disease - infection with Tropheryma whipplei (G+) - Self-limited lactase deficiency - following viral diarrhea |
|
|
Which type of malabsorption syndrome is characterized by foamy macrophages?
|
Whipple Disease
|
|
|
What is Celiac Sprue associated with?
|
- HLA-DQ2, HLA-DQ8
- Northern European descent - Dermatitis Herpetiformis (watery blisters, not caused by herpes) - Increased risk of malignancy (eg, T-cell lymphoma) |
|
|
What antibodies cause Celiac Sprue?
|
- Anti-endomysial antibody
- Anti-tissue transglutaminase antibody - Anti-gliadin antibody |
|
|
What are the histologic findings in Celiac Sprue?
|
- Blunting of villi
- Lymphocytes in lamina propria |
|
|
Which part of the GI tract has malabsorption in Celiac Sprue?
|
Decreased mucosal absorption primarily affects distal duodenum and / or proximal jejunum
|
|
|
How do you diagnose Celiac Disease?
|
Presence of tissue transglutaminase antibodies in serum
|
|
|
What kind of diarrhea occurs in disaccharidase deficiency (eg, lactase deficiency)?
|
Osmotic diarrhea (too much water is drawn into the bowels)
|
|
|
How do you diagnose a disacharidase deficiency (eg, lactase deficiency)?
|
Lactose Tolerance Test is (+) for lactase deficiency, if:
- Administration of lactose produces symptoms AND - Glucose rises <20 mg/dL |
|
|
What are the implications of a decreased ability to synthesize apolipoprotein B?
|
Inability to generate chylomicrons → ↓ secretion of cholesterol, VLDL into bloodstream → fat accumulates in enterocytes
Abetalipoproteinemia (type of malabsorption disorder) |
|
|
How do you diagnose pancreatic insufficiency (malabsorption syndrome)?
|
D-xylose absorption test:
- Normal urinary excretion in pancreatic insufficiency - ↓ excretion with intestinal mucosa defects or bacterial overgrowth |
|
|
What are the types of Inflammatory Bowel Disease?
|
- Crohn Disease
- Ulcerative Colitis |
|
|
How do Crohn Disease and Ulcerative Colitis compare in terms of possible etiology?
|
- CD: disordered response to intestinal bacteria
- UC: auto-immune |
|
|
How do Crohn Disease and Ulcerative Colitis compare in terms of location of GI tract affected?
|
- CD: any portion of GI tract, usually terminal ileum and colon, skip lesions with rectal sparing
- UC: colitis = colon inflammation, continuous colonic lesions always with rectal involvement |
|
|
How do Crohn Disease and Ulcerative Colitis compare in terms of the effect on the rectum?
|
- CD: rectal sparing
- UC: always involves rectum |
|
|
How do Crohn Disease and Ulcerative Colitis compare in terms of the gross morphology?
|

- CD: transmural inflammation → fistulas; cobblestone mucosa, creeping fat, bowel wall thickening ("string sign" on barium swallow x-ray), linear ulcers, and fissures
- UC: mucosal and submucosal inflammation only; friable mucosal pseudopolyps with freely hanging mesentery; loss of haustra → "lead pipe" appearance on imaging |
|
|
How do Crohn Disease and Ulcerative Colitis compare in terms of microscopic morphology?
|
- CD: non-caseating granulomas and lymphoid aggregates (Th1 mediated)
- UC: crypt abscesses and ulcers, bleeding, no granulomas (Th2 mediated) |
|
|
How do Crohn Disease and Ulcerative Colitis compare in terms of potential complications?
|
- CD: strictures (leading to obstruction), fistulas, perianal disease, malabsorption, nutritional depletion, colorectal cancer, and gallstones
- UC: malnutrition, sclerosing cholangitis, toxic megacolon, colorectal carcinoma (worse with R sided colitis or pancolitis) |
|
|
How do Crohn Disease and Ulcerative Colitis compare in terms of their intestinal manifestations?
|
- CD: diarrhea that may or may not be bloody
- UC: bloody diarrhea |
|
|
How do Crohn Disease and Ulcerative Colitis compare in terms of their extra-intestinal manifestation?
|
- CD: migratory polyarthritis, kidney stones
- UC: 1° sclerosing cholangitis, - Both: pyoderma gangrenosum, erythema nodosum, ankylosing spondylitis, aphthous ulcers, uveitis |
|
|
How do Crohn Disease and Ulcerative Colitis compare in terms of their treatment?
|
- CD: corticosteroids, azathioprine, methotrexate, infliximab, adalimumab
- UC: ASA preparations (sulfasalazine), 6-mercaptopurine, infliximab, colectomy |
|
|
What mnemonic can be used to remember the characteristics of Crohn's Disease?
|
for CROHN, think of a FAT GRANny and an old CRONE SKIPping down a COBBLESTONE road away from the WRECK
- Crohn's disease - Creeping fat - Granulomas (non-caseating) - Skip lesions - Cobblestone mucosa - Rectal sparing |
|
|
What mnemonic can be used to remember the characteristics of Ulcerative Colitis?
|
UC causes ULCCCERS:
- Ulcers - Large intestine - Continuous - Colorectal carcinoma - Crypt abscesses - Extends proximally - Red diarrhea (bloody) - Sclerosing cholangitis |
|
|
What is the possible etiology and location of the lesions in Crohn's Disease?
|
- Disordered response to intestinal bacteria
- Any portion of GI tract can be affected, usually the terminal ileum and colon - Skip lesions and rectal sparing |
|
|
What is the possible etiology and location of the lesions in Ulcerative Colitis?
|
- Auto-immune etiology
- Inflammation of colon is continuous, always with rectal sparing |
|
|
What is the gross morphological appearance of Crohn's Disease?
|
- Transmural inflammation → fistulas
- Cobblestone mucosa - Creeping fat - Bowel wall thickening ("string sign" on barium swallow x-ray) - Linear ulcers - Fissures |
|
|
What is the gross morphological appearance of Ulcerative Colitis?
|
- Mucosal and submucosal inflammation ONLY
- Friable mucosal pseudopolyps with freely hanging mesentery - Loss of haustra → lead pipe appearance on imaging |
|
|
What is the microscopic morphological appearance of Crohn's Disease?
|
- Non-caseating granulomas
- Lymphoid aggregates - Th1 mediated |
|
|
What is the microscopic morphological appearance of Ulcerative Colitis?
|
- Crypt abscesses and ulcers
- Bleeding - No granulomas - Th2 mediated |
|
|
What are the potential complications of Crohn's Disease?
|
- Strictures (leading to obstruction)
- Fistulas - Perianal disease - Malabsorption - Nutritional depletion - Colorectal cancer - Gallstones |
|
|
What are the potential complications of Ulcerative Colitis?
|
- Malnutrition
- Sclerosing cholangitis - Toxic megacolon - Colorectal carcinoma (worse with right-sided colitis or pancolitis) |
|
|
What are the intestinal manifestations of Crohn's Disease?
|
Diarrhea that may or may not be bloody
|
|
|
What are the intestinal manifestations of Ulcerative Colitis?
|
Bloody diarrhea
|
|
|
What are the extra-intestinal manifestations of Crohn's Disease?
|
* Migratory polyarthritis
* Kidney stones - Erythema nodosum - Ankylosing spondylitis - Pyoderma gangrenosum - Aphthous ulcers - Uveitis * = unique to CD |
|
|
What are the extra-intestinal manifestations of Ulcerative Colitis?
|
* 1° sclerosing cholangitis
- Pyoderma gangrenosum - Erythema nodosum - Ankylosing spondylitis - Apthous ulcers - Uveitis * = unique to UC |
|
|
What are the treatment strategies for Crohn's Disease?
|
- Corticosteroids
- Azathioprine - Methotrexate - Infliximab (TNF-α antibody) - Adalimumab (TNF antibody) |
|
|
What are the treatment strategies for Ulcerative Colitis?
|
- ASA preparations (sulfasalazine)
- 6-mercaptopurine - Infliximab (TNF-α antibody) - Colectomy |
|
|
Which form of IBD is characterized by Th1 mediated inflammation?
|
Crohn's Disease
|
|
|
Which form of IBD is characterized by Th2 mediated inflammation?
|
Ulcerative Colitis
|
|
|
Which form of IBD is characterized by skip lesions and rectal sparing?
|
Crohn's Disease
|
|
|
Which form of IBD is characterized by transmural inflammation?
|
Crohn's Disease
|
|
|
Which form of IBD is characterized by mucosal and submucosal inflammation?
|
Ulcerative Colitis
|
|
Which form of IBD is characterized by "string sign" on barium swallow x-ray?
|
Crohn's Disease
|
|
|
Which form of IBD is characterized by "lead pipe" appearance on imaging?
|
Ulcerative Colitis
|
|
|
Which form of IBD is characterized by non-caseating granulomas?
|
Crohn's Disease
|
|
|
Which form of IBD is characterized by crypt abscesses?
|
Ulcerative Colitis
|
|
|
Which form of IBD is characterized by fistulas?
|
Crohn's Disease
|
|
|
Which form of IBD is characterized by Sclerosing Cholangitis?
|
Ulcerative Colitis
|
|
|
Which form of IBD is characterized by bloody diarrhea?
|
Ulcerative colitis always has bloody diarrhea; Crohn's may or may not have bloody diarrhea
|
|
|
Which form of IBD can be associated with migratory polyarthritis?
|
Crohn's Disease
|
|
|
How do you diagnose Irritable Bowel Syndrome?
|
Recurrent abdominal pain associated with ≥2 of the following:
- Pain improves with defecation - Change in stool frequency - Change in appearance of stool |
|
|
When is Irritable Bowel Syndrome most common?
|
Middle-aged women
|
|
|
What are the symptoms of Irritable Bowel Syndrome? Gross findings?
|
- Diarrhea, constipation, or alternating symptoms
- No structural abnormalities; pathophysiology is multifaceted |
|
|
How do you treat Irritable Bowel Syndrome?
|
Treat symptoms (diarrhea / constipation)
|
|
|
What causes appendicitis?
|
Acute inflammation of appendix due to obstruction by fecalith (in adults) or lymphoid hyperplasia (in children)
|
|
|
What are the signs / symptoms of appendicitis?
|
- Initial diffuse periumbilical pain migrates to McBurney point (1/3 distance from anterior superior iliac spine to umbilicus)
- Nausea - Fever - Psoas, Obturator, and Rovsing signs |
|
|
What is a potential complication of appendicitis?
|
Perforation → Peritonitis
|
|
|
What is included on a differential for appendicitis?
|
- Diverticulitis (elderly)
- Ectopic pregnancy (use β-hCG to rule out) |
|
|
How do you treat appendicitis?
|
Appendectomy
|
|
What is this?
|
Diverticulum: blind pouch
|
|
|
What is a diverticulum?
|
A blind pouch that protrudes from the alimentary tract and communicates with the lumen of the gut
|
|
|
How do you get a diverticulum?
|
Most (esophagus, stomach, duodenum, colon) are acquired and are termed "false" in that they lack or have an attenuated muscularis externa
|
|
|
Where are most diverticulum found?
|
Sigmoid colon
|
|
|
What is the difference between a "true" and "false" diverticulum?
|
- True: all 3 gut wall layers outpoutch (eg, Meckel)
- False: only mucosa and submucosa outpouch; occurs where vasa recta perforate muscularis externa |
|
|
What does "diverticulosis" mean? Cause?
|
Many false diverticula (only mucosa and submucosa outpouch)
- Caused by ↑ intraluminal pressure and focal weakness in colonic wall - Associated with low-fiber diets |
|
|
How common is diverticulosis?
|
Common: in ~50% of people >60 years (associated with low fiber diets)
|
|
|
What are the symptoms of a patient with diverticulosis (many false diverticula of colon)?
|
- Often asymptomatic
- Can be associated with vague discomfort - Common cause of hematochezia (passage of fresh blood through anus) |
|
|
What are the potential complications of diverticulosis (many false diverticula of colon)?
|

- Diverticulitis: inflammation of diverticula (picture)
- Fistulas |
|
|
What should you consider in a patient presenting with LLQ pain, fever, and leukocytosis (looks like appendicitis but on left side)? What is the treatment?
|
* Diverticulitis: inflammation of diverticula (most commonly in sigmoid colon - hence LLQ)
- Give antibiotics |
|
|
What are the potential complications of an inflamed diverticula (diverticulitis)?
|
- Perforation → peritonitis
- Abscess formation - Bowel stenosis |
|
|
What findings / complications might you see in a patient with diverticulitis?
|
- Stool occult blood common +/- hematochezia (fresh blood passes through anus)
- Colovesical fistula (fistula with bladder) → pneumaturia (bubbles in urine) |
|
|
What diagnosis should you consider in an elderly male presenting with dysphagia, obstruction, and foul breath?
|
Zenker Diverticulum
|
|
|
What is the name of the pharyngoesophageal false diverticulum (only through mucosa and submucosa)?
|
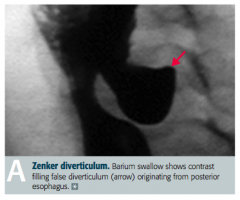
Zenker Diverticulum
|
|
|
What is a Zenker Diverticulum? Location?
|
- False diverticulum
- Pharyngoesophageal - Herniation of mucosal tissue at Killian triangle between thyropharyngeal and cricopharyngeal parts of inferior pharyngeal constrictor |
|
|
What symptoms does a patient with a Zenker Diverticulum show? Who is most likely to get it?
|
- Dysphagia
- Obstruction - Foul breath from trapped food particles (halitosis) - Most commonly in elderly males |
|
|
Which pathology is characterized by the five 2's: 2 inches long, 2 feet from the ileocecal valve, 2% of population, commonly presents in first 2 years of life, and may have 2 types of epithelia (gastric/pancreatic)?
|
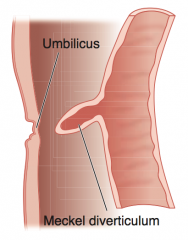
Meckel Diverticulum
|
|
|
What is the term for the true diverticulum that forms because of the persistence of the vitelline duct?
|
Meckel Diverticulum
|
|
|
What is a Meckel Diverticulum? Cause?
|
- True diverticulum
- Persistence of vitelline duct - May contain ectopic acid-secreting gastric mucosa and/or pancreatic tissue |
|
|
What is the most common congenital anomaly of the GI tract?
|
Meckel Diverticulum
- True diverticulum - Persistence of vitelline duct - May contain ectopic acid-secreting gastric mucosa and/or pancreatic tissue |
|
|
What should you suspect in a patient <2 years old with melena (dark sticky feces containing partly digested blood) and RLQ pain?
|
Meckel Diverticulum
|
|
|
What can Meckel Diverticulum cause?
|
- Melena (dark sticky feces containing partially digested blood)
- RLQ pain - Intussusception - Volvulus - Obstruction (near terminal ileum) |
|
|
What is the term for the cystic dilation of the vitelline duct?
|
Omphalomesenteric Cyst
|
|
|
How do you diagnose Meckel Diverticulum?
|
Pertechnetate study - for uptake by ectopic gastric mucosa
|
|
|
What is the mnemonic to remember the characteristics of the Meckel Diverticulum?
|
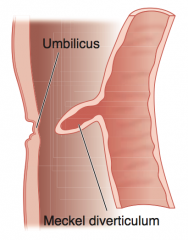
Five 2's:
- 2 inches long - 2 feet from ileocecal valve - 2% of population (most common congenital anomaly of GI tract) - Commonly presents in first 2 years - May have 2 types of epithelia (gastric and/or pancreatic) |
|
|
Which pathology causes "currant jelly" stools?
|
Intussusception
|
|
|
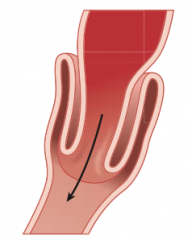
What is the term for "telescoping" of 1 bowel segment into a distal segment? Most common location?
|
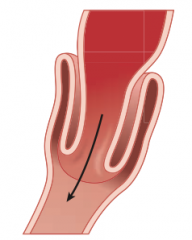
Intussusception - commonly at ileocecal junction
|
|
|
What are the consequences of Intussusception?
|
- Compromised blood supply → intermittent abdominal pain
- Often with currant jelly stools |
|
|
Who is more likely to get Intussusception? Associated with?
|
- Unusual in adults (associated with intraluminal mass or tumor that acts as lead point that is pulled into lumen)
- Majority of cases are in children (usually idiopathic, may be associated with recent enteric or respiratory viral infection) |
|
|
How severe is intussusception?
|
Abdominal emergency in early childhood
|
|
|
What is the term for the twisting of portions of the bowel around its mesentery?
|
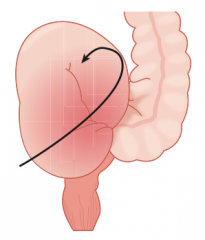
Volvulus
|
|
|
What can Volvulus lead to?
|
Obstruction and infarction
|
|
|
Where can Volvulus occur? Who is more likely to get it?
|
- Midgut volvulus: more common in infants and children
- Sigmoid volvulus: more common in elderly |
|
|
What diagnosis should you consider in a newborn (<48 hours) that has bilious emesis, abdominal distention, and a failure to pass meconium? Cause?
|
Hirschsprung Disease (congenital megacolon)
- Lack of ganglion cells / enteric nervous plexuses (Auerbach and Meissner plexuses) in segment of intestine - Due to failure of neural crest cell migration - Associated with mutations in RET gene |
|
|
What genetic problem is Hirschsprung disease associated with?
|
- Mutations in RET gene
- Risk ↑ with Down Syndrome |
|
|
What are the signs / symptoms of Hirschsprung disease?
|
- Bilious emesis
- Abdominal distention - Failure to pass meconium in first 48 hours = chronic constipation - Dilated portion of colon proximal to aganglionic segment |
|
|
How do you diagnose Hirschsprung disease?
|
Rectal suction biopsy - confirm the lack of ganglion cells / enteric nervous plexuses in segment of intestine
|
|
|
How do you treat Hirschsprung disease?
|
Resection of aganglionic portion of colon
|
|
|
Which intestinal disorder is the most common cause of small bowel obstruction? Pathology?
|
Intestinal Adhesion:
- Fibrous band of scar tissue - Commonly after surgery - Can have well-demarcated necrotic zones |
|
|
Which intestinal disorder causes tortuous dilation of vessels leading to hematochezia? Where is it found? How is diagnosis confirmed?
|
Angiodysplasia
- Most often in cecum, terminal ileum, and ascending colon - More common in older patients - Confirmed by angiography |
|
|
Which intestinal disorder causes early bilious vomiting with a double bubble sign on x-ray? What is it associated with?
|
Duodenal atresia
- Proximal stomach distention - Failure of small bowel recanalization - Associated with Down Syndrome |
|
|
Which intestinal disorder causes hypomotility? Signs? Causes?
|
Ileus
- Hypomotility without obstruction → constipation and ↓ flatus - Distended / tympanic abdomen with ↓ bowel sounds - Associated with abdominal surgeries, opiates, hypokalemia, and sepsis |
|
|
Which intestinal disorder is associated with reduced intestinal blood flow? Location? Other?
|
Ischemic Colitis
- Pain after eating → weight loss - Commonly at splenic flexure (watershed zone) and distal colon - Typically affects elderly |
|
|
Which intestinal disorder is associated with cystic fibrosis?
|
Meconium Ileus
- Meconium plug obstructs intestine - Prevents stool passage at birth |
|
|
Which intestinal disorder is more common in preemies? Why? Location?
|
Necrotizing Enterocolitis
- Necrosis of intestinal mucosa and possible perforation - More common in preemies because they have decreased immunity - Colon is usually involved, but can involve entire GI tract |
|
|
What does an intestinal adhesion cause?
|
- Fibrous band of scar tissue, commonly after surgery
- Most common cause of small bowel obstruction - Can have well de-marcated necrotic zones |
|
|
What does angiodysplasia cause?
|
- Tortuous dilation of vessels → hematochezia
- Most often found in cecum, terminal ileum, and ascending colon - More common in older patients - Confirmed by angiography |
|
|
What does duodenal atresia cause?
|
- Causes early bilious vomiting with proximal stomach distention
- Double bubble sign on x-ray - Due to failure of small bowel recanalization - Associated with Down syndrome |
|
|
What does ileus cause?
|
- Intestinal hypomotility without obstruction → constipation and ↓ flatus
- Distended / tympanic abdomen with ↓ bowel sounds - Associated with abdominal surgeries, opiates, hypokalemia, and sepsis |
|
|
What does Ischemic Colitis cause?
|
- Reduction in intestinal blood flow causes ischemia
- Pain after eating → weight loss - Commonly occurs at splenic flexure and distal colon - Typically affects elderly |
|
|
What does Meconium Ileus cause?
|
- In cystic fibrosis, meconium plug obstructs intestine
- Prevents stool passage at birth |
|
|
What does Necrotizing Enterocolitis cause?
|
- Necrosis of intestinal mucosa and possible perforation
- Colon is usually involved, but can involve entire GI tract - In neonates, more common in preemies (↓ immunity) |
|
|
What is the term for masses that protrude into the gut lumen? Appearance?
|
Colonic polyps - sawtooth appearance
|
|
|
What are the types of colonic polyps?
|
- Adenomatous
- Hyperplastic - Juvenile - Hamartomatous |
|
|
Are colonic polyps cancerous?
|
90% are non-neoplastic
|
|
|
Where are colonic polyps usually found?
|
Rectosigmoid portion of colon
|
|
|
What are the two histologic appearances of colonic polyps?
|

- Tubular (left)
- Villous (right) |
|
|
Which type of colonic polyp is precancerous? What increases the malignant risk?
|
Adenomatous Colonic Polyps
- ↑ Size - Villous histology (more villous = more villainous) - ↑ Epithelial dysplasia |
|
|
Which type of colonic polyp is a precursor or associated with increased risk of colorectal cancer?
|
- Adenomatous = precursor to CRC
- Hamartomatous = increased risk of CRC |
|
|
What are the symptoms of adenomatous colonic polyps?
|
- Often asymptomatic
- Lower GI bleed - Partial obstruction - Secretory diarrhea (villous adenomas) |
|
|
What is the most common non-neoplastic polyp in the colon? Location?
|
Hyperplastic colonic polyps (>50% found in rectosigmoid colon)
|
|
|
Which type of colonic polyp is seen in children <5 years old? Malignant potential? Location?
|
Juvenile
- If single, no malignant potential - Juvenile polyposis syndrome: multiple juvenile polyps in GI tract, ↑ risk of adenocarcinoma - 80% in rectum |
|
|
Which type of colonic polyp is associated with increased risk of adenocarcinoma?
|
Juvenile colonic polyp in Juvenile Polyposis Syndrome (multiple polyps)
|
|
|
Which type of colonic polyp has an autosomal dominant inheritance pattern?
|
Hamartomatous:
- Peutz-Jeghers Syndrome |
|
|
What are the signs/symptoms of Peutz-Jeghers Syndrome? How is it inherited?
|
- Autosomal dominant syndrome
- Multiple non-malignant hamartomas throughout GI tract - Hyperpigmented mouth, lips, hands, and genitalia - Associated with ↑ risk of CRC and other visceral malignancies |
|
|
What are the characteristics of Adenomatous Colonic Polyps?
|
- Adenomatous polyps are PRE-CANCEROUS
- Malignant risk associated with ↑ size, villous histology, and ↑ epithelial dysplasia - Precursor to colorectal cancer (CRC) - Polyp symptoms: asymptomatic, lower GI bleed, partial obstruction, or secretory diarrhea |
|
|
What are the characteristics of Hyperplastic Colonic Polyps?
|
- Most common non-neoplastic polyp in colon
- >50% found in rectosigmoid colon |
|
|
What are the characteristics of Juvenile Colonic Polyps?
|
- Mostly sporadic lesions in children <5 years old
- 80% in rectum - If single, no malignant potential - Juvenile Polyposis Syndrome: multiple juvenile polyps in GI tract, ↑ risk of adenocarcinoma |
|
|
What are the characteristics of Hamartomatous Colonic Polyps?
|
Peutz Jeghers Syndrome
- Autosomal dominant - Multiple non-malignant hamartomas throughout GI tract - Hyperpigmented mouth, lips, hands, genitalia - Associated with ↑ risk of CRC and other visceral malignancies |
|
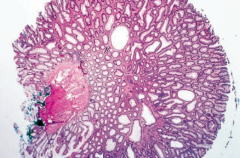
What does this histology show?
|
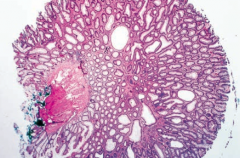
Tubular Adenoma
- Smaller, more rounded villi - More likely to be benign colonic polyp |
|
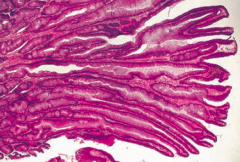
What does this histology show?
|
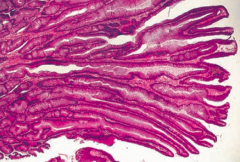
Villous Adenoma
- Long finger-like villi - More likely to be malignant (villous = villainous) |
|
|
Who is most likely to get colorectal cancer?
|
- Most patients >50 years
- 25% have a family history |
|
|
What genetic syndromes can contribute to Colorectal Cancer?
|
- Familial Adenomatous Polyposis (FAP)
- Gardner Syndrome - Turcot Syndrome - Hereditary Non-Polyposis Colorectal Cancer (HNPCC / Lynch Syndrome) |
|
|
How are the different genetic syndromes that can cause Colorectal Cancer inherited?
|
All Autosomal Dominant
|
|
|
What mutation is responsible for Familial Adenomatous Polyposis (FAP)? Location?
|
Autosomal Dominant mutation of APC gene on chromosome 5q
- Requires 2-hits |
|
|
If you have 2 hits of the mutated APC gene on chromosome 5q, what do you have? What will it cause?
|
Familial Adenomatous Polyposis (FAP)
- 100% progress to Colorectal Cancer unless the colon is resected |
|
|
What are the signs of Familial Adenomatous Polyposis (FAP)?
|
- Thousands of polyps arise starting at a young age
- Pancolonic - Always involves RECTUM |
|
|
What is it called if you have Familial Adenomatous Polyposis (FAP) + osseous and soft tissue tumors, with congenital hypertrophy of retinal pigment epithelium?
|
Gardner Syndrome
|
|
|
What is it called if you have Familial Adenomatous Polyposis (FAP) + a malignant CNS tumor?
|
Turcot Syndrome (think TURban)
|
|
|
What mutation is responsible for Hereditary Non-Polyposis Colorectal Cancer (HNPCC / Lynch Syndrome)?
|
Autosomal dominant mutation of DNA mismatch repair genes
|
|
|
If you have a mutation of DNA mismatch repair genes, what do you have? What will it cause?
|
Hereditary Non-Polyposis Colorectal Cancer (HNPCC / Lynch Syndrome)
- 80% progress to Colorectal Cancer (CRC) |
|
|
Which part of the colon is affected by Hereditary Non-Polyposis Colorectal Cancer (HNPCC / Lynch Syndrome)?
|
Proximal colon is ALWAYS involved
|
|
|
What mutations cause a predisposition for colorectal cancer?
|
- Mutation of APC gene on chromosome 5q → Familial Adenomatous Polyposis (FAP) → 100% progress to CRC
- Mutation of DNA mismatch repair genes → Hereditary Non-Polyposis Colorectal Cancer (HNPCC / Lynch Syndrome) → 80% progress to CRC |
|
|
What is Gardner Syndrome?
|
Familial Adenomatous Polyposis (FAP) + osseous and soft tissue tumors, congenital hypertrophy of retinal pigment epithelium
|
|
|
What is Turcot Syndrome?
|
Familial Adenomatous Polyposis (FAP) + malignant CNS tumor (TURcot = TURban)
|
|
|
What are the risk factors for Colorectal Cancer?
|
- Inflammatory Bowel Disease
- Tobacco use - Large villous adenomas (polyps) - Juvenile polyposis syndrome - Peutz-Jeghers Syndrome (hamatromatous polyps) |
|
|
What part of the colon is most commonly affected by Colorectal Cancer?
|
Rectosigmoid > Ascending > Descending
|
|
|
What are the characteristics of Colorectal Cancer in the ascending colon?
|
- Exophytic mass
- Iron deficiency anemia - Weight loss RIGHT SIDE BLEEDS, left side obstructs |
|
|
What are the characteristics of Colorectal Cancer in the descending colon?
|
- Infiltrating mass
- Partial obstruction - Colicky pain - Hematochezia Right side bleeds, LEFT SIDE OBSTRUCTS |
|
|
What is a rare presentation of Colorectal Cancer?
|
Streptococcus bovis bacteremia
- S. bovis colonizes the gut - Can also cause subacute endocarditis Bovis in the Blood = Cancer in the Colon |
|
|
If you have a patient with iron deficiency anemia who is male or postmenopausal female, what must you rule out?
|
Colorectal Cancer
|
|
|
How should patients be screened for Colorectal Cancer?
|
- Screen patients >50 years old
- Colonoscopy or stool occult blood test |
|
|
What finding occurs in Colorectal Cancer on barium enema x-ray?
|

"Apple core" lesion
|
|

Your patient gets a barium enema x-ray, and this is the finding in the sigmoid colon, what do you think of?
|

Apple core lesion → think Colorectal Cancer
|
|
|
What tumor marker is good for monitoring recurrence of Colorectal Cancer? Can it be used for screening?
|
CEA tumor marker can be used to monitor for recurrence, but not useful for screening
|
|
|
What are the two molecular pathways that lead to Colorectal Cancer? How common?
|
- Microsatellite instability pathway (~15%)
- APC / β-catenin (chromosomal instability) pathway (~85%) |
|
|
What is wrong in the microsatellite instability pathway? What does it cause?
|
- DNA mismatch repair gene mutations → sporadic and HNPCC syndrome
- Mutations accumulate, but no defined morphologic correlates - Responsible for 15% of cases of CRC |
|
|
What is wrong in the APC/β-catenin pathway? What does it cause?
|

- Chromosomal instability → sporadic cancer
- Responsible for 85% of cases of CRC - Normal colon → loss of APC gene → - Colon at risk → K-ras mutation → - Adenoma → Loss of tumor suppressor gene(s) (p53, DCC) → - Carcinoma |
|
|
What gene events occur in the APC/β-catenin pathway leading to colorectal cancer
|

Order of gene events: AK-53
- Normal colon → loss of APC gene (↓ intercellular adhesion and ↑ proliferation) → - Colon at risk → K-ras mutation (unregulated intracellular signal transduction) → - Adenoma → Loss of tumor suppressor gene(s) (p53, DCC) (increased tumorigenesis) → - Carcinoma |
|
|
What are the implications of the loss of the APC gene in the progression to colorectal cancer?
|

- Decreased intercellular adhesions
- Increased proliferations - Colon at risk |
|
|
What are the implications of the K-RAS mutation after loss of the APC gene in the progression to colorectal cancer?
|
- Unregulated intracellular signal transduction
- At risk colon → Adenoma |
|
|
What are the implications of the loss of tumor suppressor genes (p53, DCC), after the K-RAS mutation and loss of the APC gene in the progression to colorectal cancer?
|
- Increased tumorigenesis
- Adenoma → Carcinoma |
|
|
What are the signs of portal hypertension?
|
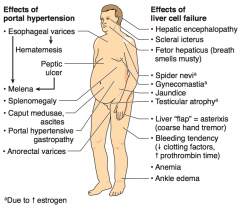
- Esophageal varices → hematemesis and melena
- Peptic ulcer → melena - Splenomegaly - Caput medusae, ascites - Portal hypertensive gastropathy - Anorectal varices |
|
|
What are the signs of liver cell failure?
|
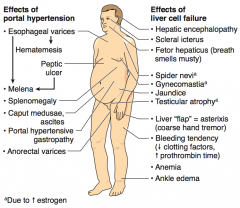
- Hepatic encephalopathy
- Scleral icterus - Fetor hepaticus (breath smells musty) - Spider nevi (d/t ↑ Estrogen) - Gynecomastia (d/t ↑ Estrogen) - Jaundice - Testicular atrophy (d/t ↑ Estrogen) - Liver "flap" = asterixis (coarse hand tremor) - Bleeding tendency (↓ clotting factors, ↑ prothrombin time) - Anemia - Ankle edema |
|
What is the term for the diffuse fibrosis and nodular regeneration that destroys the normal architecture of the liver?
|
Cirrhosis
|
|
|
What are the characteristics of cirrhosis?
|
- Diffuse fibrosis
- Nodular regeneration - Destroys normal architecture of liver |
|
|
What does cirrhosis put you at risk for?
|
Increased risk for Hepatocellular Carcinoma (HCC)
|
|
|
What are the most common causes of cirrhosis?
|
- Alcohol (60-70%)
- Viral hepatitis - Biliary disease - Hemochromatosis |
|
|
What can alleviate portal hypertensino?
|
Portosystemic shunts:
- Esophageal varices - Caput medusae |
|
|
What are these signs indicative of?
- Esophageal varices - Hematemesis - Peptic ulcer - Melena - Splenomegaly - Caput medusae, ascites - Portal gastropathy - Anorectal varices |
Portal Hypertension
|
|
|
What are these signs indicative of?
- Hepatic encephalopathy - Scleral icterus - Fetor hepaticus (breath smells musty) - Spider nevi - Gynecomastia - Jaundice - Testicular atrophy - Liver "flap" = asterixis (coarse hand tremor) - Bleeding tendency (↓ clotting factors, ↑ prothrombin time) - Anemia - Ankle edema |
Liver cell failure
|
|
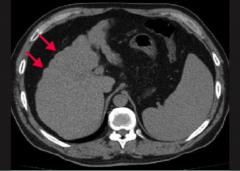
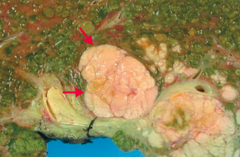
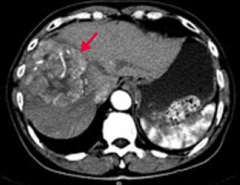
What does this CT show?
|
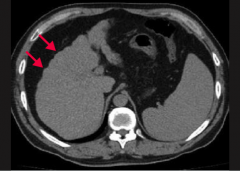
Nodularity (arrows) of the liver contour secondary to regenerating macronodules = Cirrhosis
|
|
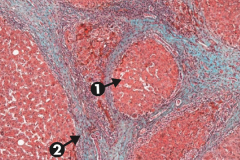
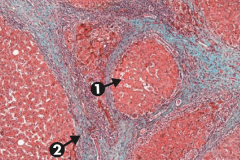
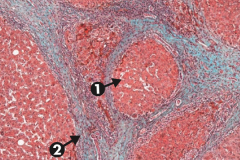
What does this slide show?
|
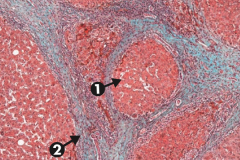
Cirrhosis, microscopic: typical regenerative nodules (arrow 1) and bridging fibrosis (arrow 2)
|
|
|
What are the serum markers of liver and pancreas pathology?
|
- Alkaline phosphatase (ALP)
- Aminotransferases (AST and ALT) - often called liver enzymes - Ceruloplasmin - γ-Glutamyl Transpeptidase (GGT) - Amylase - Lipase |
|
|
What is the major diagnostic use of Alkaline Phosphatase (ALP)?
|
- Obstructive hepatobiliary disease
- HCC - Bone disease |
|
|
What is the major diagnostic use of Aminotransferases (AST and ALT) - often called "liver enzymes"?
|
- Viral hepatitis (ALT > AST)
- Alcoholic hepatitis (AST > ALT) |
|
|
What is the major diagnostic use of Ceruloplasmin?
|
↓ in Wilson Disease
|
|
|
What is the major diagnostic use of γ-Glutamyl Transpeptidase (GGT)?
|
↑ in various liver and biliary diseases (just as ALP can), but not in bone disease; associated with alcohol use
|
|
|
What is the major diagnostic use of Amylase?
|
- Acute pancreatitis
- Mumps |
|
|
What is the major diagnostic use of Lipase?
|
Acute Pancreatitis (most specific)
|
|
|
Which serum marker is most specific to acute pancreatitis?
|
Lipase
|
|
|
What can develop in children to take aspirin?
|
Reye Syndrome - rare, often fatal childhood hepatoencephalopathy
|
|
|
What are these findings associated with:
- Hepatoencephalopathy - Mitochondrial abnormalities - Fatty liver (microvesicular fatty change) - Hypoglycemia - Vomiting - Hepatomegaly - Coma Cause? |
Reye Syndrome - associated with viral infection (especially VZV and influenza B) that has been treated with aspirin
|
|
|
What is the mechanism by which aspirin causes Reye Syndrome?
|
Aspirin metabolites ↓ β-oxidation by reversible inhibition of mitochondrial enzyme
|
|
|
What are the signs of Reye Syndrome?
|
- Hepatoencephalopathy (often fatal)
- Mitochondrial abnormalities - Fatty liver (microvesicular fatty change) - Hypoglycemia - Vomiting - Hepatomegaly - Coma |
|
|
What is the only exception for use of aspirin in children?
|
Kawasaki disease
|
|
|
What are the stages of alcoholic liver disease?
|
- Hepatic steatosis
- Alcoholic hepatitis - Alcoholic cirrhosis |
|
|
What are the characteristics of Hepatic Steatosis?
|
- First stage in alcoholic liver disease
- Reversible change with moderate alcohol intake - Macrovesicular fatty changes that may be reversible with alcohol cessation |
|
|
What are the characteristics of Alcoholic Hepatitis?
|
- Second stage in alcoholic liver disease
- Requires sustained, long-term consumption of alcohol - Swollen and necrotic hepatocytes with neutrophilic infiltration - Mallory bodies (intracytoplasmic eosinophilic inclusions) are present - AST > ALT (ratio usually >1.5) |
|
|
What are the characteristics of Alcoholic Cirrhosis?
|
- Final stage of alcoholic liver disease
- Irreversible changes - Micronodular, irregularly shrunken liver with "hobnail" appearance - Sclerosis around central vein (zone III) - Has manifestations of chronic liver disease (eg, jaundice, hypoalbuminemia) |
|
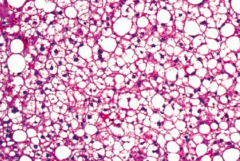
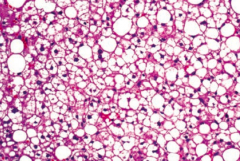
When might you see macrovesicular fatty change in the liver?
|
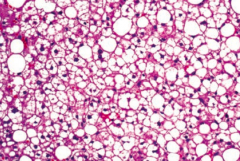
Macrovesicular fatty change is a sign of hepatic steatosis (stage 1 of alcoholic liver disease); reversible with alcohol cessation
|
|
|
When might you see swollen and necrotic hepatocytes with neutrophilic infiltration and Mallory bodies?
|
Alcoholic Heptitis (stage 2 of alcoholic liver disease)
- Mallory Bodies: intracytoplasmic eosinophilic inclusions |
|
|
When might you see a micronodular with a "hobnail" appearance?
|
Alcoholic cirrhosis (stage 3 of alcoholic liver disease); irreversible and final form
|
|
|
Where is there sclerosis in the liver with alcoholic cirrhosis?
|
Around the central vein (zone III)
|
|
|
What causes non-alcoholic fatty liver disease? What changes happen?
|
Metabolic syndrome (insulin resistance) → fatty infiltration of hepatocytes → cellular "ballooning" and eventual necrosis
ALT > AST (lipids) (independent of alcohol use) |
|
|
What can non-alcoholic fatty liver disease lead to?
|
May cause cirrhosis and hepatocellular carcinoma
|
|
|
What causes hepatic encephalopathy?
|
Cirrhosis → portosystemic shunts → ↓ NH3 metabolism → neuropsychiatric dysfunction
|
|
|
How severe is hepatic encephalopathy?
|
Spectrum from disorientation / asterixis (mild) to difficult arousal or coma (severe)
|
|
|
What an trigger hepatic encephalopathy?
|
- ↑ NH3 production: dietary protein, GI bleed, constipation, infection
- ↓ NH3 removal: renal failure, diuretics, post-TIPS |
|
|
What can lead to ↑ NH3 production? Implications?
|
- Dietary protein
- GI bleed - Constipation - Infection - Can be a trigger for hepatic encephalopathy |
|
|
What can lead to ↓ NH3 removal? Implications?
|
- Renal failure
- Diuretics - Post-TIPS (Transjugular Intrahepatic Portosystemic Shunt) |
|
|
How do you treat patients with hepatic encephalopathy?
|
- Lactulose (removes NH3 by converting to NH4+)
- Low protein diet - Rifaximin (kills intestinal bacteria) |
|
|
What is the most common 1° malignant tumor of the liver in adults?
|
Hepatocellular Carcinoma (HCC)
|
|
|
What is Hepatocellular Carcinoma (HCC) associated with?
|
- Hepatitis B & C
- Wilson disease - Hemochromatosis - α1-antitrypsin deficiency - Alcoholic cirrhosis - Aflatoxin from Aspergillus (carcinogen) |
|
|
What can Hepatocellular Carcinoma (HCC) lead to?
|
Budd-Chiari Syndrome
- Caused by occlusion of the hepatic veins that drain the liver - Presents with the classical triad of abdominal pain, ascites and hepatomegaly |
|
|
What are the findings in patients with Hepatocellular Carcinoma?
|
- Jaundice
- Tender hepatomegaly - Ascites - Anorexia - May lead to Budd-Chiari Syndrome |
|
|
How do you diagnose Hepatocellular Carcinoma (HCC)?
|
- ↑ α-Fetoprotein
- Ultrasound - Contrast CT (enhancing heterogenous mass) |
|
|
How does Hepatocellular Carcinoma (HCC) spread?
|
Hematogenously
|
|
|
What are the liver tumors?
|
- Hepatocellular Carcinoma (most common)
- Cavernous Hemangioma - Hepatic Adenoma - Angiosarcoma |
|
|
What is the common, benign liver tumor that typically occurs at age 30-50 years?
|
Cavernous Hemangioma
|
|
|
What is the rare, benign liver tumor, often related to oral contraceptive or anabolic steroid use?
|
Hepatic Adenoma
|
|
|
What is the malignant liver tumor of endothelial origin associated with exposure to arsenic and vinyl chloride?
|
Angiosarcoma
|
|
|
What are the characteristics of Cavernous Hemangioma?
|
- Common, benign liver tumor
- Typically occurs at age 30-50 years - Biopsy contraindicated because of a risk of hemorrhage |
|
|
What are the characteristics of Hepatic Adenoma?
|
- Rare, benign liver tumor
- Often related to oral contraceptive or anabolic steroid use - May regress spontaneously or rupture (abdominal pain and shock) |
|
|
What are the characteristics of Angiosarcoma?
|
- Malignant tumor of endothelial organ
- Associated with exposure to arsenic and vinyl chloride |
|
|
What causes the liver to have a "nutmeg" appearance?
|
- Backup of blood into liver
- Commonly caused by R-sided heart failure and Budd-Chiari Syndrome - Appears mottled by a nutmeg |
|
|
What can nutmeg liver progress to?
|
If the condition persists, centrilobular congestion and necrosis can result in cardiac cirrhosis
|
|
|
What causes Budd-Chiari Syndrome?
|
Occlusion of IVC or hepatic vein with centrilobular congestion and necrosis
|
|
|
What does Budd-Chiari Syndrome lead to?
|
- Congestive liver disease → hepatomegaly, ascites, abdominal pain, and eventual live failure
- May develop varices - May have visible abdominal and back veins |
|
|
What is Budd-Chiari Syndrome associated with?
|
- Hypercoagulable states
- Polycythemia vera - Pregnancy - Hepatocellular Carcinoma (HCC) - Absence of JVD |
|
|
How does α1-antitrypsin deficiency cause liver damage?
|
Misfolded gene product protein aggregates in hepatocellular ER → cirrhosis
|
|
|
What is the histologic finding of α1-antitrypsin deficiency in the liver?
|
Cirrhosis with PAS (+) globules (made of aggregations of misfolded gene product)
|
|
|
How do you inherit α1-antitrypsin deficiency?
|
Codominant trait
|
|
|
How does α1-antitrypsin deficiency affect other organs besides the liver?
|
In lungs, ↓ α1-antitrypsin → uninhibited elastase in alveoli → ↓ elastic tissue → panacinar emphysema
|
|
|
What causes jaundice?
|
- Bilirubin deposition in the skin and/or sclera causing yellowing
- Occurs at high bilirubin levels (>2.5 mg/dL) in the blood 2° to ↑ production or defective metabolism |
|
|
How high does bilirubin need to be to cause jaundice?
|
>2.5 mg/dL in blood
|
|
|
What are the types of hyperbilirubinemia?
|
- Unconjugated (indirect) hyperbilirubinemia
- Conjugated (direct) hyperbilirubinemia - Mixed (direct and indirect) hyperbilirubinemia |
|
|
What is the level of urine urobilinogen in unconjugated (indirect) hyperbilirubinemia? What diseases have this finding?
|
- Increased urine urobilinogen
- Diseases: hemolytic, physiologic (newborns), Crigler-Najjar, Gilbert syndrome |
|
|
What is the level of urine urobilinogen in conjugated (direct) hyperbilirubinemia? What diseases have this finding?
|
- Decreased urine urobilinogen
Diseases: - Biliary tract obstruction: gallstones, pancreatic liver cancer, liver fluke - Biliary tract disease: 1° sclerosing cholangitis and 1° biliary cirrhosis - Excretion defect: Dubin-Johnson syndrome, Rotor syndrome |
|
|
What is the level of urine urobilinogen in mixed (direct and indirect) hyperbilirubinemia? What diseases have this finding?
|
- Normal or ↑
- Diseases: hepatitis or cirrhosis |
|
|
What type of hyperbilirubinemia is seen in patients with hemolysis?
|
Unconjugated (indirect) hyperbilirubinemia
- ↑ urine urobilinogen |
|
|
What type of hyperbilirubinemia is seen in newborns?
|
Physiologic (don't have enzymes to convert to conjugated form)
- Unconjugated (indirect) hyperbilirubinemia - ↑ urine urobilinogen |
|
|
What type of hyperbilirubinemia is seen in patients with Crigler-Najjar syndrome?
|
Unconjugated (indirect) hyperbilirubinemia
- ↑ urine urobilinogen |
|
|
What type of hyperbilirubinemia is seen in patients with Gilbert syndrome?
|
Unconjugated (indirect) hyperbilirubinemia
- ↑ urine urobilinogen |
|
|
What type of hyperbilirubinemia is seen in patients with a biliary tract obstruction? What can cause this?
|
Causes of biliary tract obstruction:
- Gallstones - Pancreatic liver cancer - Liver fluke Conjugated (direct) hyperbilirubinemia - ↓ urine urobilinogen |
|
|
What type of hyperbilirubinemia is seen in patients with a biliary tract disease? What can cause this?
|
Causes of biliary tract disease:
- 1° sclerosing cholangitis - 1° biliary cirrhosis Conjugated (direct) hyperbilirubinemia - ↓ urine urobilinogen |
|
|
What type of hyperbilirubinemia is seen in patients with an excretion defect? What can cause this?
|
- Dubin-Johnson Syndrome
- Rotor Syndrome Conjugated (direct) hyperbilirubinemia - ↓ urine urobilinogen |
|
|
What type of hyperbilirubinemia is seen in patients with hepatitis and cirrhosis?
|
Mixed (direct and indirect) hyperbilirubinemia
- Normal or ↑ urine urobilinogen |
|
|
What is the most common cause of jaundice in a neonate?
|
Physiologic Neonatal Jaundice
- At birth, immature UDP-glucuronosyltrasnferase --> unconjugated hyperbilirubinemia --> jaundice / kernicterus |
|
|
How do you treat a neonate with physiologic jaundice?
|
Phototherapy (converts unconjugated bilirubin to water-soluble form
|
|
|
Which hereditary hyperbilirubinemia is associated with mildly DECREASED UDP-glucuronosyltransferase conjugation activity? What does this lead to?
|
Gilbert Syndrome
- Decreased bilirubin uptake by hepatocytes - Asymptomatic or mild jaundice (no clinical consequences) - Elevated unconjugated bilirubin without overt hemolysis - Bilirubin increases with fasting and stress |
|
|
Which hereditary hyperbilirubinemia is associated with ABSENT UDP-glucuronosyltransferase conjugation activity? What does this lead to?
|
Crigler-Najjar Syndrome (type I)
- Presents early in life, patients die within a few years - Causes jaundice, kernicterus (bilirubin depostion in brain), and ↑ unconjugated bilirubin |
|
|
Which hereditary hyperbilirubinemia is associated with a black liver? Why?
|
Dubin-Johnson Syndrome
- Conjugated hyperbilirubinemia is due to defective liver excretion - Benign |
|
|
Which hereditary hyperbilirubinemia causes a mild conjugated hyperbilirubinemia but without turning th eliver black?
|
Rotor Syndrome
|
|
|
Which syndrome causes bilirubin to increase with fasting or stress? Consequences?
|
Gilbert Syndrome
- Mildly ↓ UDP-glucuronosyltransferase conjugation activity - Leads to ↓ bilirubin uptake by hepatocytes - Can be asymptomatic or cause mild jaundice - Elevated unconjugated bilirubin without overt hemolysis |
|
|
What is wrong in Gilbert Syndrome? Symptoms? Other characteristics?
|
- Very common, no clinical consequences
- Mildly ↓ UDP-glucuronosyltransferase conjugation activity - Leads to ↓ bilirubin uptake by hepatocytes - Can be asymptomatic or cause mild jaundice - Elevated unconjugated bilirubin without overt hemolysis - Bilirubin ↑ with fasting and stress |
|
|
What is wrong in Crigler-Najjar Syndrome, type 1? Symptoms? Other characteristics?
|
- Absent UDP-glucuronosyltransferase
- Presents early in life, patients die within a few years - Findings: jaundice, kernicterus (bilirubin deposition in brain), ↑ unconjugated bilirubin - Treat with plasmapheresis and phototherapy |
|
|
What is wrong in Crigler-Najjar Syndrome, type 2? Symptoms? Other characteristics?
|
- Type 2 is less severe
- Responds to phenobarbital which ↑ liver enzyme synthesis |
|
|
What is wrong in Dubin-Johnson Syndrome? Symptoms? Other characteristics?
|
- Conjugated hyperbilirubinemia
- Due to defective liver excretion - Grossly black liver - Benign |
|
|
What is wrong in Rotor Syndrome? Symptoms? Other characteristics?
|
- Similar to Dubin-Johnson Syndrome (problem with liver excretion of bilirubin)
- Mild conjugated hyperbilirubinemia - Even milder, and doesn't cause black liver |
|
|
What does hemoglobin get converted to during its destruction? Where?
|

Bilirubin - takes place in hepatic sinussoid
|
|

Which hereditary syndromes cause a problem with bilirubin uptake and conjugation (1)? Leads to?
|

Gilbert Syndrome
- Leads to unconjugated bilirubinemia |
|

Which hereditary syndromes cause a problem with bilirubin conjugation (2)? Leads to?
|

Crigler-Najjar Syndrome
- Leads to unconjugated bilirubinemia |
|

Which hereditary syndromes cause a problem with conjugated bilirubin excretion (3) and (4)? Leads to?
|

Dubin-Johnson Syndrome
- Leads to conjugated hyperbilirubinemia Rotor Syndrome - Leads to MILD conjugated hyperbilirubinemia |
|
|
What is the mnemonic to remember the characteristics of Wilson Disease (hepatolenticular degeneration)?
|
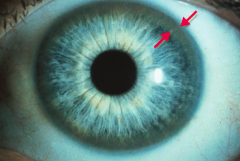
Copper is Hella BAD:
- C: ↓ Ceruloplasmin, Cirrhosis, Corneal deposits (Kayser-Fleischer rings), Copper accumulations, Carcinoma (hepatocellular) - H: Hemolytic anemia - B: Basal ganglia degeneration (parkinsonian symptoms) - A: Asterixis (tremor of the hand when the wrist is extended) - D: Dementia, Dyskinesia, Dysarthria |
|
|
What causes Wilson Disease?
|
Inadequate hepatic copper excretion and failure of copper to enter circulation as ceruloplasmin
|
|
|
What are the implications of inadequate hepatic copper excretion and failure of copper to enter circulation as ceruloplasmin? Where does it go?
|
Wilson Disease
- Leads to copper accumulation - Especially in liver, brain, cornea (Kayser-Fleischer ring), kidneys, and joints |
|
|
How do you treat Wilson Disease?
|
Penicillamine or Trientine
|
|
|
How do you get Wilson disease?
|
Autosomal recessive inheritance (chromsome 13 = 13 letters in Wilson disease)
- Copper is normally excreted into bile by hepatocyte copper transporting ATPase (ATP-7B gene) |
|
|
What is the mnemonic to remember the characteristics of Wilson Disease (hepatolenticular degeneration)?
|
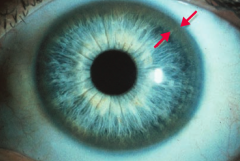
Copper is Hella BAD:
- C: ↓ Ceruloplasmin, Cirrhosis, Corneal deposits (Kayser-Fleischer rings), Copper accumulations, Carcinoma (hepatocellular) - H: Hemolytic anemia - B: Basal ganglia degeneration (parkinsonian symptoms) - A: Asterixis (tremor of the hand when the wrist is extended) - D: Dementia, Dyskinesia, Dysarthria |
|
|
What disease should you consider in a patient who is very tan with Diabetes Mellitus ("bronze Diabetes")? Cause?
|
Hemochromatosis
- Disease caused by deposition of hemosiderin (iron) |
|
|
What is the classic triad in Hemochromatosis?
|
- Micronodular Cirrhosis
- Diabetes mellitus - Skin pegmentation |
|
|
What are the potential consequences of Hemochromatosis?
|
- CHF
- Testicular atrophy - ↑ Risk of HCC |
|
|
What can cause Hemochromatosis?
|
- 1° - autosomal recessive C282Y or H63D mutation on HFE gene, associated with HLA-A3
- 2° - chronic transfusion therapy (eg, β-thalassemia major) |
|
|
What are the lab results in a patient with Hemochromatosis?
|
- ↑ Ferritin
- ↑ Iron (may reach 50g, enough to set off metal detectors at airports) - ↓ Total Iron Binding Capacity → ↑ Transferrin Saturation |
|
|
What mutation is responsible for hereditary hemochromatosis? What is it associated with?
|
- C282Y or H63D mutation on HFE gene (autosomal recessive)
- Associated with HLA-A3 |
|
|
Is hemochromatosis worse in young men or young women? Why?
|
Young men - in women, iron can be lost through menstruation which slows the progression
|
|
|
How do you treat hereditary hemochromatosis?
|
- Repeated phlebotomy
- Deferasirox - Deferoxamine |
|
|
What are the types of biliary tract diseases?
|
- Primary Biliary Cirrhosis
- Secondary Biliary Cirrhosis - Primary Sclerosing Cholangitis |
|
|
How do Primary Biliary Cirrhosis, Secondary Biliary Cirrhosis, and Primary Sclerosing Cholangitis present?
|
Same presentation
- Pruritus - Jaundice - Dark urine - Light stools - Hepatosplenomegaly |
|
|
What is the pathologic cause of Primary Biliary Cirrhosis (PBC)?
|
- Auto-immune reaction →
- Lymphocytic infiltrate + Granulomas → - Destruction of intralobular bile ducts |
|
|
What is the pathologic cause of Secondary Biliary Cirrhosis (SBC)?
|
- Extrahepatic biliary obstruction (gallstone, biliary stricture, chronic pancreatitis, carcinoma of pancreatic head) →
- ↑ Pressure in intrahepatic ducts → - Injury / fibrosis and bile stasis |
|
|
What is the pathologic cause of Primary Sclerosing Cholangitis (PSC)?
|
- Unknown cause of concentric "onion skin" bile duct fibrosis →
- Alternating strictures and dilation with "beading" of intra- and extra-hepatic bile ducts on ERCP |
|
|
Which biliary tract disease is complicated by ascending cholangitis?
|
Secondary Biliary Cirrhosis
|
|
|
Which biliary tract disease has ↑ serum mitochondrial antibodies, including IgM?
|
Primary Biliary Cirrhosis
|
|
|
Which biliary tract disease is associated with other auto-immune conditions? Which ones?
|
Primary Biliary Cirrhosis is associated with:
- CREST syndrome - Sjögren syndrome - Rheumatoid arthritis - Celiac disease |
|
|
Which biliary tract disease has hypergammaglobulinemia (IgM)?
|
Primary Sclerosing Cholangitis
|
|
|
Which biliary tract disease is associated with Ulcerative Colitis?
|
Primary Sclerosing Cholangitis
|
|
|
What can Primary Sclerosing Cholangitis progress to?
|
- 2° biliary cirrhosis
- Cholangiocarcinoma |
|
|
Which biliary tract disease is associated with extrahepatic biliary obstruction (eg, gallstone, biliary stricture, chronic pancreatitis, or carcinoma of pancreatic head)? Presentation? Labs? Additional information?
|
Secondary Biliary Cirrhosis
- Presentation: pruritus, jaundice, dark urine, light stools, hepatosplenomegaly - Labs: ↑ conjugated bilirubin, ↑ cholesterol, ↑ ALP - Additional: ↑ pressure in intrahepatic ducts → injury/fibrosis and bile stasis; complicated by ascending cholangitis |
|
|
Which biliary tract disease is associated with an auto-immune reaction, leading to a lymphocytic infiltrate and granulomas? Presentation? Labs? Additional information?
|
Primary Biliary Cirrhosis
- Presentation: pruritus, jaundice, dark urine, light stools, hepatosplenomegaly - Labs: ↑ conjugated bilirubin, ↑ cholesterol, ↑ ALP - Additional: destruction of intralobular bile ducts; ↑ serum mitochondrial antibodies, including IgM; associated with other auto-immune conditions (eg, CREST, Sjögren syndrome, rheumatoid arthritis, and celiac disease) |
|
|
Which biliary tract disease is associated with "onion skin" bile duct fibrosis? Presentation? Labs? Additional information?
|
Primary Sclerosing Cholangitis
- Presentation: pruritus, jaundice, dark urine, light stools, hepatosplenomegaly - Labs: ↑ conjugated bilirubin, ↑ cholesterol, ↑ ALP - Additional: alternating strictures and dilation with "beading" of intra- and extra-hepatic bile ducts on ERCP; hypergammaglobulinemia (IgM); associated with ulcerative colitis; can lead to 2° biliary cirrhosis and cholangiocarcinoma |
|
|
What is the term for the presence of gallstones?
|
Cholelithiasis
|
|
|
What is Cholelithiasis? What can cause them?
|
Gallstones:
- ↑ cholesterol and/or bilirubin - ↓ bile salts - Gallbladder stasis |
|
|
What are the types of gallstones?
|
- Cholesterol stones (80%)
- Pigment stones |
|
|
What increases your risk for gallstones?
|
4 F's:
- Female - Fat - Fertile (pregnant) - Forty |
|
|
What is associated with developing cholesterol stones?
|
- Obesity
- Crohn Disease - Advanced age - Clofibrate - Estrogen therapy - Multiparity - Rapid weight loss - Native American origin |
|
|
What is associated with developing pigment stones?
|
- Patients with chronic hemolysis
- Alcoholic cirrhosis - Advanced age - Biliary infection |
|
|
What is the appearance of cholesterol stones?
|
Radiolucent w/ 10-20% opaque due to calcifications
|
|
|
What is the appearance of pigment stones?
|
- Black: radiopaque, hemolysis
- Brown: radiolucent, infection |
|
|
What can gallstones cause?
|
- Cholecystitis (inflammation of gallbladder)
- Ascending cholangitis (infection of bile duct) - Acute pancreatitis - Bile stasis - Biliary colic - Fistula between gallbladder and small intestine - Gallstone ileus |
|
|
What is the term for neurohormonal activation (by CCK after a fatty meal) that triggers contraction of the gallbladder, forcing a stone into the cystic duct, which may present with pain (eg, in diabetics)?
|
Biliary Colic
|
|
|
What is Biliary Colic?
|
- Neurohormonal activation (by CCK after a fatty meal)
- Triggers contraction of the gallbladder - Forces a stone into the cystic duct - May present with pain (eg, in diabetics) |
|
|
In a patient with a history of gallstones, what may cause air in the biliary tree?
|
Fistula between gallbladder and small intestine
|
|
|
What causes gallstone ileus?
|
Gallstone obstruction of the ileocecal valve
|
|
|
How do you diagnose cholelithiasis? How do you treat?
|
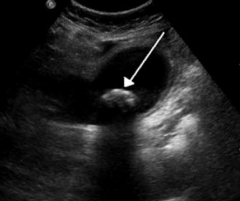
- Diagnose with ultrasound
- Treat with cholecystectomy if symptomatic |
|

What does this ultrasound show?
|

Cholelithiasis (gallstones): distended gallbladder containing a large gallstone
|
|
|
What is the triad of symptoms seen in cholangitis (infection of bile duct)?
|
Charcot triad of cholangitis:
- Jaundice - Fever - RUQ pain |
|
|
What is the term for gallstones?
|
Cholelithiasis
|
|
|
What is the term for inflammation of the gallbladder?
|
Cholecystitis
|
|
|
What causes Cholecystitis?
|
Usually from cholelithiasis (gallstone)
- Most commonly blocking the cystic duct → 2° infection - Rarely ischemia or 1° infection (CMV) |
|
|
What physical exam test is present with Cholecystitis (inflammation of gallbladder)?
|
Murphy Sign: inspiratory arrest on RUQ palpation d/t pain
|
|
|
What is the Murphy Sign physical exam test? What does it indicate?
|
- RUQ palpation, if there is pain patient will have inspiratory arrest
- Diagnostic of Cholecystitis |
|
|
How do you diagnose Cholecystitis?
|
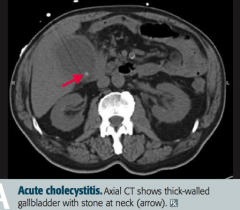
- Ultrasound
- HIDA - Murphy's sign (+) |
|

When would you see a "porcelain" gallbladder?
|
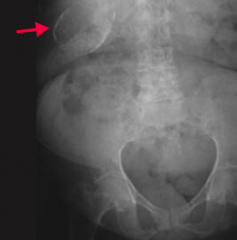
Chronic Cholecystitis (inflammation of gallbladder) - calcified gallbladder
|
|
|
How is "porcelain" gallbladder usually detected? How do you treat?
|
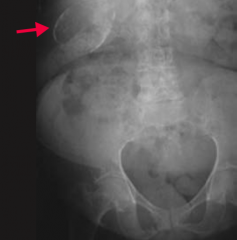
- Usually found incidentally on imaging
- Treat: prophylactic cholecystectomy d/t high rates of gallbladder carcinoma |
|
|
What are the possible causes of Acute Pancreatitis?
|
GET SMASHED or idiopathic:
- Gallstones - Ethanol - Trauma - Steroids - Mumps - Auto-immune disease - Scorpion sting - Hypercalcemia / Hypertriglyceridemia (>1000mg/dL) - ERCP - Drugs (eg, Sulfa drugs) |
|
|
What should you consider as a diagnosis in a patient with epigastric abdominal pain radiating to the back, with anorexia and nausea? How do you confirm diagnosis?
|
Acute Pancreatitis
- ↑ Amylase and Lipase (higher specificity) |
|
|
What happens in acute pancreatitis? What can it lead to?
|
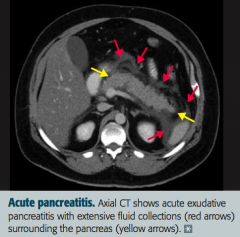
- Auto-digestion of pancreas by pancreatic enzymes
- Can lead to DIC, ARDS, diffuse fat necrosis, hypocalcemia (Ca2+ collects in pancreatic Ca2+ soap deposits), pseudocyst formation, hemorrhage, infection, and multi-organ failure |
|
|
What are the potential complications of acute pancreatitis?
|
Pancreatic pseudocyst (lined by granulation tissue, not epithelium; can rupture and hemorrhage)
|
|
|
What are the possible causes of Acute Pancreatitis?
|
GET SMASHED or idiopathic:
- Gallstones - Ethanol - Trauma - Steroids - Mumps - Auto-immune disease - Scorpion sting - Hypercalcemia / Hypertriglyceridemia (>1000mg/dL) - ERCP - Drugs (eg, Sulfa drugs) |
|
|
What happens in chronic pancreatitis?
|
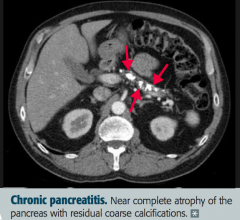
- Chronic inflammation
- Atrophy - Calcification of pancreas (image) |
|
|
What are the major causes of chronic pancreatitis?
|
- Alcohol abuse
- Idiopathic |
|
|
What can chronic pancreatitis lead to?
|
Pancreatic insufficiency → steatorrhea, fat-soluble vitamin deficiency, diabetes mellitus, and ↑ risk of pancreatic adenocarcinoma
|
|
|
How do the levels of amylase and lipase compare in acute vs chronic pancreatitis?
|
- Almost always elevated in acute pancreatitis
- May or may not be elevated in chronic pancreatitis |
|
|
What is the very aggressive tumor arising from the pancreatic ducts? Prognosis?
|
Pancreatic Adenocarcinoma
- Average prognosis is 1 year - Typically has already metastasized at presentation |
|
|
What is the histologic appearance of Pancreatic Adenocarcinoma?
|
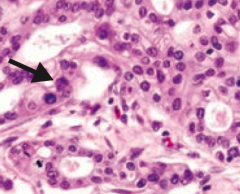
- Disorganized glandular structure with cellular infiltration
- Tumor arises from pancreatic ducts |
|
|
What part of the pancreas is typically affected by Pancreatic Adenocarcinoma? Consequences?
|
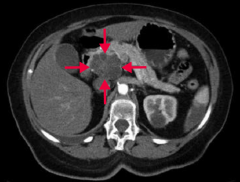
Tumors more common in pancreatic head → obstructive jaundice
|
|
|
What tumor marker is associated with Pancreatic Adenocarcinoma?
|
CA-19-9 tumor marker (also CEA but less specific)
|
|
|
What are the risk factors for Pancreatic Adenocarcinoma?
|
- Tobacco use
- Chronic pancreatitis (especially >20 years) - Diabetes - Age > 50 years - Jewish and African-American males |
|
|
How does Pancreatic Adenocarcinoma typically present?
|
- Abdominal pain radiating to back
- Weight loss (d/t malabsorption and anorexia) - Migratory thrombophlebitis (redness and tenderness on palpation of extremities = Trousseau syndrome) - Obstructive jaundice w/ palpable non-tender gallbladder = Courvoisier sign |
|
|
What is Trousseau Syndrome? Sign of?
|
Migratory Thrombophlebitis - redness and tenderness on palpation of extremities
- Sign of Pancreatic Adenocarcinoma |
|
|
What is Courvoisier Sign? Sign of?
|
Obstructive jaundice with palpable, NON-TENDER gallbladder
- Sign of Pancreatic Adenocarcinoma |
|
|
How do you treat a patient with Pancreatic Adenocarcinoma?
|
- Whipple procedure
- Chemotherapy - Radiation therapy |

