![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
292 Cards in this Set
- Front
- Back
|
What are R→L congenital shunts? |
5 T's:
1. Truncus arteriosus (1 vessel) 2. Transposition (2 switched vessels) 3. Tricuspid atresia (3 = Tri) 4. Tetralogy of Fallot (4 = Tetra) 5. TAPVR (Total Anomalous Pulmonary Venous Return - 5 letters in name) |
|
|
What are the similarities of the R→L congenital shunts?
|
- Cause of early cyanosis: "blue babies"
- Often diagnosed prenatally or becomes evident immediately after birth - Usually requires urgent surgical correction and/or maintenance of a PDA |
|
|
What kind of congenital shunts are Trunctus Arteriosus, Transposition, Tricuspid Atresia, Tetralogy of Fallot, TAPVR? Treatment?
|
- They are all R→L shunts causing early cyanosis (blue babies)
- Requires urgent surgical correction and/or maintenance of PDA |
|
|
What happens in a persistent Truncus Arteriosus?
|
- Failure of truncus arteriosus to divide into a pulmonary trunk and aorta
- Most patients have an accompanying VSD - R→L shunt causes early cyanosis "blue babies" |
|
|
What happens in a D-transposition of the great vessels?
|
- Aorta leaves RV (anterior)
- Pulmonary trunk leaves LV (posterior) - Leads to separation of systemic and pulmonary circuits - Not compatible with life unless a shunt is present to allow mixing of blood (eg, VSD, PDA, or patent foramen ovale) - R→L shunt causes early cyanosis "blue babies" |
|
|
What is the cause of a D-transposition of the great vessels?
|
Failure of the aorticopulmonary septum to SPIRAL
|
|
|
What is the prognosis for patients with D-transposition of the great vessels?
|
- Without surgical intervention, most infants die within the first few months of life
- Need a shunt to allow mixing of blood (eg, VSD, PDA, or patent foramen ovale) |
|
|
What happens in Tricuspid Atresia?
|
- Absence of tricuspid valve and hypoplastic RV
- Requires both ASD and VSD for viability - R→L shunt causes early cyanosis "blue babies" |
|
|
What is the prognosis for patients with Tricuspid Atresia?
|
Non-compatible with life unless there is both an ASD and VSD
|
|
|
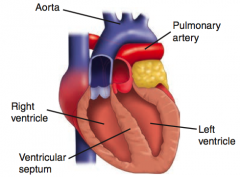
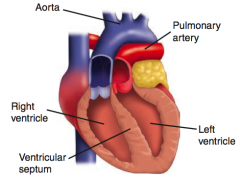
What is the cause of Tetralogy of Fallot?
|
Anterosuperior displacement of the infundibular septum
|
|
|
What is the most common cause of early childhood cyanosis?
|
Tetralogy of Fallot
|
|
|
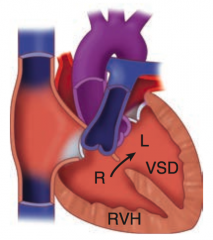
What happens in Tetralogy of Fallot?
|
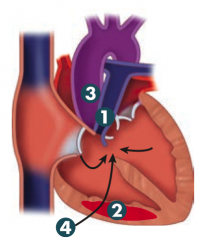
PROVe
1. Pulmonary infundibular stenosis (most important determinant for prognosis) 2. RV hypertrophy (boot shaped heart on CXR) 3. Overriding aorta 4. VSD Pulmonary stenosis forces R→L flow across VSD → early cyanotic "tet spells" and RVH - R→L shunt causes early cyanosis "blue babies" |
|
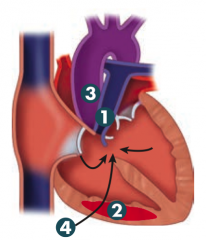
How can you improve symptoms in Tetralogy of Fallot?
|
- Squatting: ↑ SVR (systemic vascular resistance), ↓ R→L shunt, improves cyanosis
- Treatment: early surgical correction |
|
|
What happens in Total Anomalous Pulmonary Venous Return (TAPVR)?
|
- Pulmonary veins drain into right heart circulation (SVC, coronary sinus, etc)
- Associated with ASD and sometimes PDA to allow for R→L shunting to maintain CO - R→L shunt causes early cyanosis "blue babies" |
|
|
What are L→R congenital shunts? Which are more common?
|
VSD > ASD > PDA
- Ventricular Septal Defect - Atrial Septal Defect - Patent Ductus Arteriosus - Eisenmenger Syndrome |
|
|
What are the similarities of the L→R congenital shunts?
|
- Causes late cyanosis
- "Blue kids" - VSD > ASD > PDA |
|
|
Which is the most common congenital cardiac defect?
|
Ventricular Septal Defect
|
|
|
What happens in a Ventricular Septal Defect?
|
- Asymptomatic at birth
- May manifest weeks later or remain asymptomatic throughout life - Most self resolve, larger lesions may lead to LV overload and heart failure - L→R shunt causes late cyanosis ("blue kids") |
|
|
What are the possible complications of a Ventricular Septal Defect?
|
Larger lesions may lead to LV overload and heart failure
|
|
|
What happens with an Atrial Septal Defect?
|
- Defect in interatrial septum, usually occurs in septum secundum; septum primum defects usually occur with another anomalies
- Loud S1; wide fixed split S2 - Symptoms: none to heart failure - L→R shunt causes late cyanosis ("blue kids") |
|
|
How is an Atrial Septal Defect distinct from a Patent Foramen Ovale?
|
Septa is missing tissue rather than unfused
|
|
|
What heart sound are associated with an Atrial Septal Defect?
|
- Loud S1
- Wide, fixed split S2 |
|
|
What happens in Patent Ductus Arteriosus?
|
- In fetal period, shunt is R→L (normal)
- In neonatal period, ↓ lung resistance → shunt becomes L→R → progressive RVH and/or LVH and heart failure - Associated with a continuous "machine-like" murmur |
|
|
How can you maintain the patency of the Ductus Arteriosus?
|
PGE synthesis and low O2 tension
PGE kEEps it open |
|
|
How can you close a patent Ductus Arteriosus?
|
Indomethacin (ends patency of PDA)
|
|
|
What are the potential complications of an uncorrected Patent Ductus Arteriosus?
|
Can eventually result in late cyanosis in the lower extremities (differential cyanosis)
|
|
|
When would you administer PGE to a newborn?
|
To maintain patency of the Ductus Arteriosus (may be necessary to sustain life in conditions such as transposition of the great vessels)
|
|
|
When is PDA normal? When should it close?
|
- Normally open in utero
- Normally closes only after birth |
|
|
Which syndrome consists of an uncorrected L→R cardiac shunt (VSD, ASD, or PDA) that eventually switches to R→L, ultimately leads to pulmonary arteriolar hypertension, compensatory RVH, late cyanosis, clubbing, and polycythemia?
|
Eisenmenger syndrome
|
|
|
What are the characteristics of Eisenmenger syndrome?
|
- Uncorrected L→R shunt (eg, VSD, ASD, PDA) → ↑ pulmonary blood flow → pathologic remodeling of vasculature → pulmonary arteriolar HTN
- RVH occurs to compensate → shunt becomes R→L - Causes late cyanosis, clubbing, and polycythemia - Age of onset varies |
|
|
What are the other heart anomalies besides the R→L and L→R shunts?
|
Coarctation of the Aorta
- Infantile type - Adult type |
|
|
What is coarctation of the aorta associated with?
|
Bicuspid aortic valve, other heart defects
|
|
|
What happens in the infantile type of Coarctation of the Aorta?
|
INfantile: IN close to the heart
- Aorta narrows proximal to the insertion of the ductus arteriosus (PREDUCTAL) - Associated with Turner Syndrome - Can present with closure of the ductus arteriosus (reverse w/ PGE2) |
|
|
What happens in the adult type of Coarctation of the Aorta?
|
aDult: Distal to the Ductus
- Aorta narrows distal to ligamentum arteriosum (POSTDUCTAL) - Associated with notching of the ribs (collateral circulation), HTN in upper extremities, and weak, delayed pulses in lower extremities (radiofemoral delay) |
|
|
What finding is associated with notching of the ribs (collateral circulation), hypertension in upper extremities, and weak, delayed pulses in lower extremities (radiofemoral delay)?
|
Adult type of Coarctation of the Aorta (aorta narrows distal to the ligamentum arteriosum)
|
|
|
Which disorder is associated with Truncus Arteriosus and Tetralogy of Fallot?
|
22q11 syndromes
|
|
|
Which disorder is associated with ASD, VSD, and AV septal defect (endocardial cushion defect)?
|
Down Syndrome
|
|
|
Which disorder is associated with septal defects, PDA, and pulmonary artery stenosis?
|
Congenital Rubella
|
|
|
Which disorder is associated with a bicuspid aortic valve and coarctation of the aorta (preductal)?
|
Turner Syndrome
|
|
|
Which disorder is associated with MVP (mitral valve prolapse, thoracic artery aneurysm and dissection, and aortic regurgitation?
|
Marfan Syndrome
|
|
|
Which disorder is associated with transposition of the great vessels?
|
Infant of diabetic mother
|
|
|
What congenital cardiac defects are associated with 22q11 syndromes?
|
- Truncus arteriosus
- Tetralogy of Fallot |
|
|
What congenital cardiac defects are associated with Down Syndrome?
|
- ASD
- VSD - AV septal defect (endocardial cushion defect) |
|
|
What congenital cardiac defects are associated with Congenital Rubella?
|
- Septal defects
- PDA - Pulmonary artery stenosis |
|
|
What congenital cardiac defects are associated with Turner Syndrome?
|
- Bicuspid aortic valve
- Coarctation of the Aorta (preductal) |
|
|
What congenital cardiac defects are associated with Marfan Syndrome?
|
- MVP (mitral valve prolapse)
- Thoracic aortic aneurysm and dissection - Aortic regurgitation |
|
|
What congenital cardiac defects are associated with an infant of a diabetic mother?
|
Transposition of the great vessels
|
|
|
What is the definition of Hypertension?
|
- Systolic BP ≥ 140 mmHg And/Or
- Diastolic BP ≥ 90 mmHg |
|
|
What are the risk factors for Hypertension?
|
- ↑ Age
- Obesity - Diabetes - Smoking - Genetics - Black > White > Asian |
|
|
What are the causes of hypertension?
|
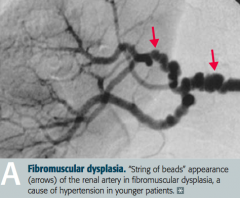
- 90% Primary (Essential), related to ↑ CO or ↑ TPR
- 10% Secondary to renal disease, including fibromuscular dysplasia in young patients |
|
|
What is the definition of a hypertensive emergency?
|
Severe hypertension (≥ 180/120 mmHg) with evidence of acute, ongoing target organ damage (eg, papilledema, mental status change)
|
|
|
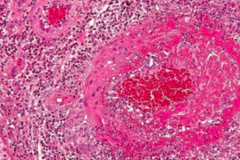
What does hypertension predispose to / risk factor for?
|
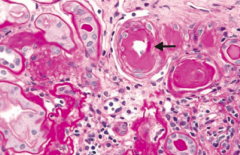
- Atherosclerosis
- LVH - Stroke - CHF - Renal failure (picture - hypertensive nephropathy) - Retinopathy - Aortic dissection |
|
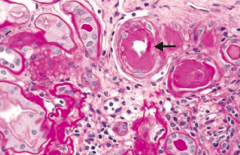
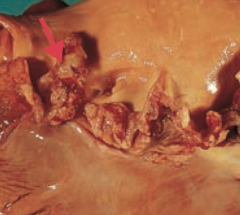
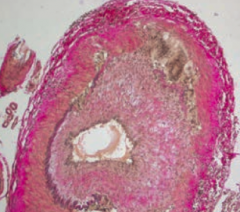
What does this slide show?
|
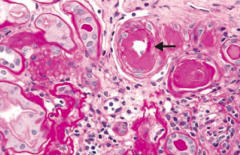
Hypertensive Nephropathy - renal arterial hyalinosis on PAS stain
|
|
|
What are the signs of hyperlipidemia?
|
- Xanthomas
- Tendinous Xanthomas - Corneal Arcus |
|
|
What are xanthomas? Cause?
|
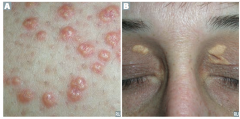
- Plaques or nodules composed of lipid laden histiocytes in the skin = A
- Especially common on the eyelids (xanthelasma = B) - Sign of hyperlipidemia |
|
|
What are Tendinous Xanthomas? Cause?
|

- Lipid deposits in tendons (C)
- Especially common in Achilles - Sign of hyperlipidemia |
|
|
What are corneal arcus?
|
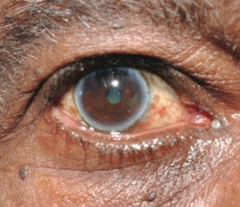
- Lipid deposits in cornea
- Appears early in life with hypercholesterolemia - Common in elderly (arcus senilis = D) |
|

What is this? Cause?
|

Xanthoma
- Plaques or nodules composed of lipid laden histiocytes in the skin - Sign of hyperlipidemia |
|

What is this? Cause?
|

Xanthelasma
- Plaques or nodules composed of lipid laden histiocytes in the skin - Especially common on the eyelids - Sign of hyperlipidemia |
|

What is this? Cause?
|

Tendinous Xanthoma
- Lipid deposits in tendons - Especially common in Achilles - Sign of hyperlipidemia |
|
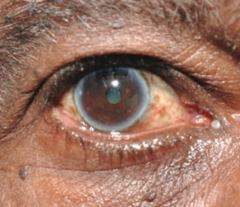
What is this? Cause?
|
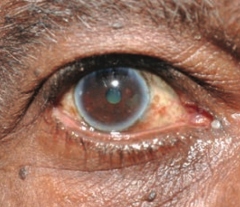
Corneal Arcus
- Lipid deposits in cornea - Appears early in life with hypercholesterolemia - Common in elderly (arcus senilis = D) |
|
|
What are the types of arteriosclerosis?
|
- Arteriolosclerosis (common)
- Mönckeberg (medial calcific sclerosis) |
|
|
What are the types of arteriolosclerosis?
|
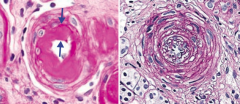
- Hyaline - thickening of small arteries in essential HTN or DM) (left)
- Hyperplastic - "onion skinning" as seen in severe HTN (right) |
|
|
What is the uncommon form of Arteriosclerosis? Characteristics?
|

Mönckeberg (Medial Calcific Sclerosis) Arteriosclerosis
- Uncommon - Calcification in the media of arteries, especially radial or ulnar - Usually benign; "pipestem" arteries on x-ray - Does not obstruct blood flow - Intima not involved |
|
What is the term for the thickening of small arteries in essential hypertension or diabetes?
|
Hyaline Arteriolosclerosis
|
|
What is the term for the "onion skinning" appearance of small arteries seen in severe hypertension?
|
Hyperplastic Arteriolosclerosis
|
|

What is the term for the usually benign process that causes a "pipestem" appearance of arteries on x-ray? Which arteries are typically affected? Implications?
|

Mönckeberg (Medial Calcific Sclerosis) Arteriosclerosis
- Uncommon - Calcification in the media of arteries, especially radial or ulnar - Does not obstruct blood flow - Intima not involved |
|
|
What is affected by atherosclerosis?
|
Disease of elastic arteries and large- and medium-sized muscular arteries
|
|
|
What are the modifiable risk factors for atherosclerosis?
|
- Smoking
- Hypertension - Hyperlipidemia - Diabetes |
|
|
What are the non-modifiable risk factors for atherosclerosis?
|
- Age
- Sex (more in men and postmenopausal women) - Family history |
|
|
How does atherosclerosis progress?
|
- Inflammation important in pathogenesis
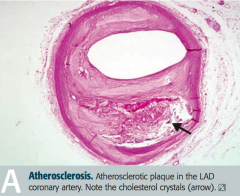
- Endothelial cell dysfunction → macrophage and LDL accumulation → foam cell formation → fatty streaks → smooth muscle cell migration (involves PDGF and FGF), proliferation, and ECM deposition → fibrous plaque → complex atheromas (picture) |
|
|
What is the appearance of atheromas?
|
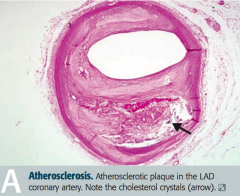
Cholesterol crystals
- Fatty streaks |
|
|
What are the complications of atherosclerosis?
|
- Aneurysms
- Ischemia - Infarcts - Peripheral vascular disease - Thrombus - Emboli |
|
|
What are the more common locations of atherosclerosis?
|

Abdominal aorta > Coronary artery > Popliteal artery > Carotid Artery (picture)
|
|
|
What are the symptoms of Atherosclerosis?
|
- Angina
- Claudication - Can be asymptomatic |
|
|
What is an aortic aneurysm? Location?
|
Localized pathologic dilation of the aorta
- Abdominal AA - Thoracic AA |
|
|
What does it mean if the aortic aneurysm is painful?
|
Sign of leaking, dissection, or imminent rupture!!
|
|
|
What is an abdominal aortic aneurysm associated with?
|
- Associated with atherosclerosis
- Occurs more frequently in hypertensive male smokers >50 years old |
|
|
What is a thoracic aortic aneurysm associated with?
|
- Associated with cystic medial degeneration due to hypertension (older patients) or Marfan syndrome (younger patients)
- Also historically associated with 3° syphilis (obliterative endarteritis of the vasa vasorum) |
|
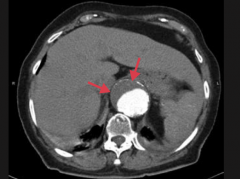
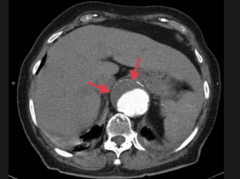
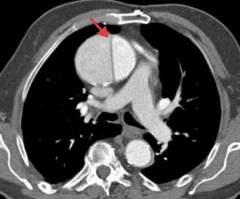
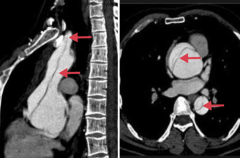
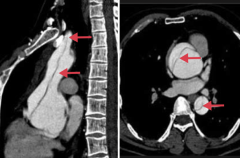
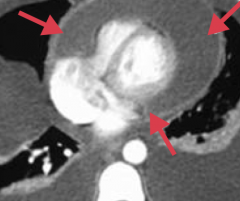
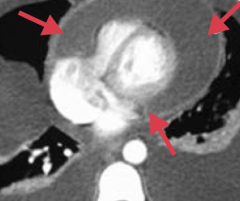
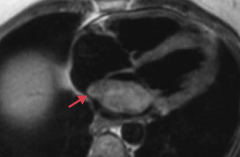
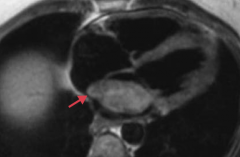
What is this a CT of?
|
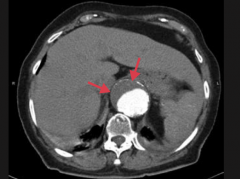
Abdominal aortic aneurysm
- Suprarenal - Eccentric mural thrombus |
|
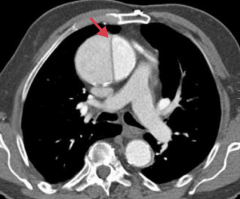
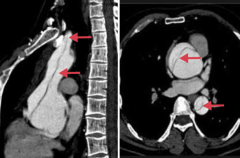
What is this a CT of?
|
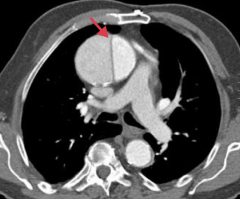
Thoracic aortic aneurysm
- Ascending aorta - Dissection (arrow) |
|
|
What happens with an aortic dissection?
|
Longitudinal intraluminal tear forms a false lumen
- The false lumen can be limited to the ascending aorta, propagate from the ascending aorta, or propagate from the descending aorta |
|
What is aortic dissection associated with?
|
- HTN
- Bicuspid aortic valve - Inherited CT disorders (eg, Marfan syndrome) |
|
|
How does a patient with an aortic dissection present?
|
- Tearing chest pain of sudden onset
- Radiates to back - +/- markedly unequal BP in arms - CXR shows mediastinal widening |
|
|
What are the possible outcomes of a patient with aortic dissection?
|
- Pericardial tamponade (fluid accumulates in the pericardium)
- Aortic rupture - Death |
|
|
What are the manifestations of ischemic heart disease?
|
- Angina (stable, unstable/crescendo, variant/Prinzmetal)
- Coronary steal syndrome - Myocardial infarction - Sudden cardiac death - Chronic ischemic heart disease |
|
|
What is the term for chest pain due to ischemic myocardium 2° to coronary artery narrowing or spasm, without myocyte necrosis?
|
Angina
|
|
|
What are the characteristics and types of angina?
|
- Chest pain due to ischemic myocardium
- 2° to coronary artery narrowing or spasm - No myocyte necrosis - Types: stable, variant / Prinzmetal, and unstable / crescendo |
|
|
What is the cause of Stable Angina? Characteristics?
|
- Usually 2° to atherosclerosis
- Exertional chest pain in classic distribution (usually with ST depression on ECG) - Resolves with rest |
|
|
What is the cause of Variant / Prinzmetal Angina? Characteristics?
|
- Occurs at rest 2° to coronary artery spasm
- Transient ST elevation on ECG - Known triggers include tobacco, cocaine, and triptans (but often unknown) - Treat with CCB, nitrates, and smoking cessation (if applicable) |
|
|
What is the cause of Unstable/Crescendo Angina? Characteristics?
|
- Thrombosis with incomplete coronary artery occlusion
- ST depression on ECG (↑ in frequency or intensity of chest pain; any chest pain at rest) |
|
|
If a patient's angina is triggered by tobacco, cocaine, or triptans, what is the cause?
|
Variant angina (Prinzmetal) = coronary artery vasospasm
|
|
|
What ECG signs are there to distinguish the types of angina?
|
- Stable: ST depression
- Variant / Prinzmetal: ST elevation - Unstable / Crescendo: ST depression |
|
|
What is the principle behind pharmacologic stress tests?
|
Coronary Steal Syndrome
- Distal to coronary stenosis, vessels are maximally dilated at baseline - Administration of vasodilators (eg, dipyridamole, regadenoson) dilates normal vessels and shunts blood toward well-perfused areas - Leads to decreased flow and ischemia in post-stenotic region |
|
|
In the coronary steal syndrome, where is there decreased flow and ischemia?
|
The area distal to the coronary stenosis gets decreased flow and ischemia because after administration of vasodilators the normal vessels dilate and shunt blood towards the well-perfused areas
|
|
|
What is the most common cause of Myocardial Infarction?
|
Acute thrombosis due to coronary artery atherosclerosis with complete obstruction of coronary artery
|
|
|
What happens in tissue that has had a Myocardial Infarction?
|
- Myocyte necrosis
- If transmural, ECG will show ST elevations - If subendocardial, ECG may show ST depressions - Cardiac biomarkers are diagnostic |
|
|
What are the signs on EKG of a Myocardial Infarction?
|
- Transmural: ST elevations
- Subendocardial: ST depressions |
|
|
What is the definition of sudden cardiac death?
|
Death from cardiac causes within 1 hour of onset of symptoms, most commonly due to a lethal arrhythmia (eg, v. fib.)
|
|
|
What is sudden cardiac death associated with?
|
- 70% of cases associated with coronary artery disease
- Cardiomyopathy (hypertrophic, dilated) - Hereditary ion channelopathies (eg, long QT syndrome) |
|
|
What is the definition of chronic ischemic heart disease?
|
Progressive onset of CHF over many years due to chronic ischemic myocardial damage
|
|
|
What are the most commonly occluded coronary arteries in MI?
|
LAD > RCA > Circumflex
|
|
|
What are the symptoms of a patient having an MI?
|
- Diaphoresis
- Nausea and vomiting - Severe retrosternal pain - Pain in L arm and/or jaw - Shortness of breath - Fatigue |
|
|
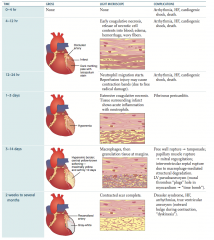
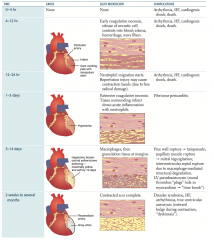
What are the gross and LM features at 0-4 hours after an MI?
|
- Gross: none
- LM: none |
|
|
What are the gross and LM features at 4-12 hours after an MI?
|
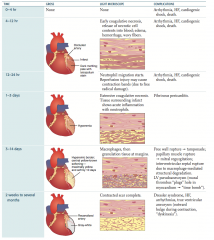
- Gross: dark mottling; pale with tetrazolium stain
- LM: early coagulative necrosis, release of necrotic cell contents into blood; edema, hemorrhage, wavy fibers |
|
|
What are the gross and LM features at 12-24 hours after an MI?
|
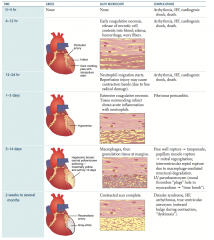
- Gross: dark mottling; pale with tetrazolium stain
- LM: neutrophil migration starts; reperfusion injury may cause contraction bands (due to free radical damage) |
|
|
What are the gross and LM features at 1-3 days after an MI?
|
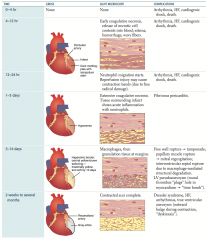
- Gross: hyperemia in affected cardiac tissue
- LM: extensive coagulative necrosis; tissue surrounding infarct shows acute inflammation with neutrophils |
|
|
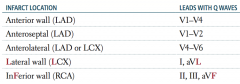
What are the gross and LM features at 3-14 days after an MI?
|
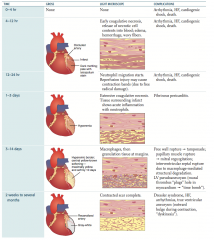
- Gross: hyperemic border with central yellow-brown softening; maximally yellow and soft by 10 days
- LM: macrophages then granulation tissue at margins |
|
|
What are the gross and LM features at 2 weeks to several months after an MI?
|
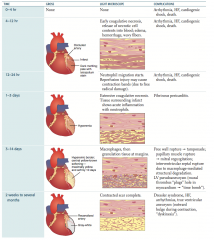
- Gross: recanalized artery; affected tissue is gray-white
- LM: contracted, scar complete |
|
|
What are the complications of an MI that can occur in the first 24 hours?
|
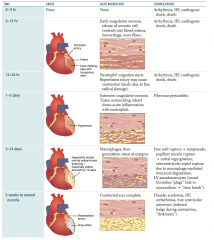
- Arrhythmia
- Heart failure - Cardiogenic shock - Death |
|
|
What are the complications of an MI that can occur on days 1-3?
|
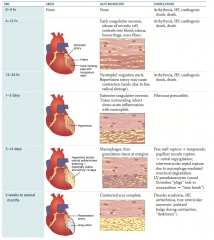
Fibrinous pericarditis
|
|
|
What are the complications of an MI that can occur on days 3-14?
|
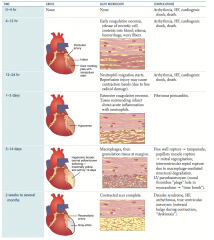
- Free wall rupture → tamponade
- Papillary muscle rupture → mitral regurgitation - Intraventricular septal rupture due to macrophage-mediated structural degradation - LV pseudoaneurysm (mural thrombus "plugs" hole in myocardium → "time bomb") |
|
|
What are the complications of an MI that can occur after 2 weeks to several months?
|
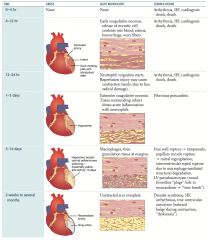
- Dressler syndrome: auto-immune phenomenon resulting in fibrinous pericarditis
- Heart failure - Arrhythmias - True ventricular aneurysm (outward bulge during contraction, dyskinesia) |
|
|
What are the gross findings after an MI by time?
|
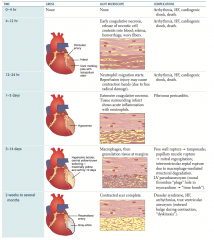
- 0-4 hours: none
- 4-24 hours: dark mottling; pale with tetrazolium stain - 1-3 days: hyperemia - 3-14 days: hyperemic border with central yellow-brown softening; maximally yellow and soft by 10 days - 2 weeks - several months: tissue is gray-white |
|
|
What are the Light Microscope findings after an MI by time?
|
- 0-4 hours: none
- 4-12 hours: early coagulative necrosis, release of necrotic cell contents into blood; edema, hemorrhage, wavy fibers - 12-24 hours: neutrophil migration starts; reperfusion injury may cause contraction bands (due to free radical damage) - 1-3 days: extensive coagulative necrosis, tissue surrounding infarct shows acute inflammation with neutrophils - 3-14 days: macrophages, then granulation tissue at margins - 2 weeks - several months: contracted scar complete |
|
|
What is the gold standard for diagnosing an MI?
|
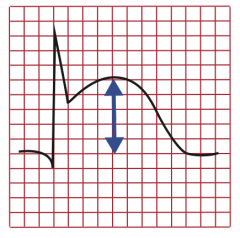
ECG (in first 6 hours)
- ST elevations (ST elevated MI = STEMI, acute transmural infarct) - ST depression (subendocardial infarct) - Pathologic Q waves (evolving or old transmural infarct) |
|
|
Which molecules are analyzed for the diagnosis of MI?
|
- Cardiac troponin I
- CK-MB |
|
|
When is Cardiac Troponin I elevated after an MI? Utility?
|
- Rises after 4 hours
- Increased for 7-10 days - More specific than other protein markers |
|
|
When is CK-MB elevated after an MI? Utility?
|
- Predominantly found in myocardium but can be released from skeletal muscle
- Used in diagnosing reinfarction following acute MI because levels return to normal after 48 hours |
|
|
What are the types of infarcts caused by an MI?
|
- Transmural infarct
- Subendocardial infarct |
|
|
What are the characteristics of a transmural infarct?
|
- ↑ Necrosis
- Affects entire wall - ST elevation on ECG, Q waves |
|
|
What are the characteristics of a subendocardial infarct?
|
- Due to ischemic necrosis of <50% of ventricle wall
- Subendocardium especially vulnerable to ischemia - ST depression on ECG |
|
|
If leads V1-V4 have Q waves, where is the MI? Which artery is affected?
|
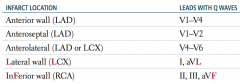
Anterior wall (LAD)
|
|
|
If leads V1-V2 have Q waves, where is the MI? Which artery is affected?
|
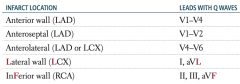
Anteroseptal (LAD)
|
|
|
If leads V4-V6 have Q waves, where is the MI? Which artery is affected?
|
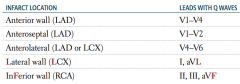
Anterolateral (LAD or LCX)
|
|
|
If leads I and aVL have Q waves, where is the MI? Which artery is affected?
|
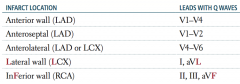
Lateral wall (LCX)
|
|
|
If leads II, III, and aVF have Q waves, where is the MI? Which artery is affected?
|
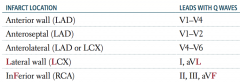
Inferior wall (RCA)
|
|
|
An infarct in the LAD can cause an infarct in which part of the heart? Which leads will have Q waves?
|
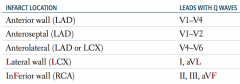
- Anterior wall: V1-V4
- Anteroseptal: V1-V2 - Anterolateral: V4-V6 |
|
|
An infarct in the LCX can cause an infarct in which part of the heart? Which leads will have Q waves?
|
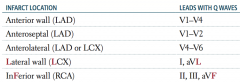
- Anterolateral: V4-V6
- Lateral wall: I, aVL |
|
|
An infarct in the RCA can cause an infarct in which part of the heart? Which leads will have Q waves?
|
Inferior wall: II, III, aVF
|
|
|
What are the possible complications of MI?
|
- Cardiac arrhythmia
- LV failure and pulmonary edema - Cardiogenic shock - Ventricular free wall, papillary muscle, or interventricular septum rupture - Ventricular pseudoaneurysm formation - Post-infarction fibrinous pericarditis - Dressler syndrome |
|
|
What is an important cause of death in patients who had an MI before they reach the hospital?
|
Cardiac arrhythmia
|
|
|
When is cardiogenic shock after MI more likely?
|
Large infarct - high risk of mortality
|
|
|
What are the implications of a ventricular free wall rupture after MI?
|
Cardiac tamponade
|
|
|
What are the implications of a papillary muscle rupture after MI?
|
Severe mitral regurgitation
|
|
|
What are the implications of an interventricular septum rupture after MI?
|
Ventricular Septal Defect (VSD)
|
|
|
When is the greatest risk for a rupture of the heart muscle wall?
|
Greatest 6-14 days post-infarct
|
|
|
What are the implications of a ventricular pseuodaneurysm forming after MI? When is it more likely?
|
- ↓ CO
- Risk of arrhythmia - Embolus from mural thrombus - Greatest risk approx. 1 week post-MI |
|
|
What are the implications of a post-infarction fibrinous pericarditis forming after MI? When is it more likely?
|
- Friction rub (1-3 days post-MI)
- May also be due to an auto-immune phenomenon several weeks after MI = Dressler Syndrome |
|
|
What is Dressler Syndrome? When is it more common?
|
- Auto-immune phenomenon resulting in fibrinous pericarditis (friction rub)
- Occurs more commonly several weeks post MI |
|
|
What are the types of cardiomyopathies?
|
- Dilated
- Hypertrophic - Restrictive / Infiltrative |
|
|
What is the most common cardiomyopathy? How common?
|
Dilated (90% of cases)
|
|
|
What are the causes of Dilated Cardiomyopathy?
|
Often idiopathic or congenital
Other: ABCCCD - Alcohol abuse - Beriberi - Coxsackie B virus myocarditis - chronic Cocaine use - Chagas disease - Doxorubicin toxicity - Hemochromatosis - Peripartum cardiomyopathy |
|
|
Which type of cardiomyopathy is associated with pregnancy?
|
Dilated Cardiomyopathy
|
|
|
What are the findings with Dilated Cardiomyopathy?
|
- Heart failure
- S3 heart sound (in early diastole during rapid ventricular filling phase) - Dilated heart on echocardiogram - Balloon appearance of heart on CXR |
|
|
How do you treat a patient with dilated cardiomyopathy?
|
- Na+ restriction
- ACE inhibitors - β-blockers - Diuretics - Digoxin - Implantable cardioconverter defibrillator (ICD) - Heart transplant |
|
|
What kind of dysfunction is associated with Dilated Cardiomyopathy? What type of growth in the walls of the ventricles?
|
- Systolic dysfunction (plenty of room to fill, but hard to pump that big volume)
- Eccentric hypertrophy (sarcomeres added in series) |
|
|
Which type of cardiomyopathy is associated with sudden death in young athletes? Cause?
|
Hypertrophic Cardiomyopathy - cause of death is due to ventricular arrhythmia
|
|
|
What are the possible causes of Hypertrophic Cardiomyopathy?
|
*60-70% familial, autosomal dominant (commonly a β-myosin heavy-chain mutation)
- Rarely associated with Friedreich ataxia |
|
|
What are the findings in a patient with Hypertrophic Cardiomyopathy?
|
- S4 heart sound ("atrial kick" - in late diastole)
- Systolic murmur |
|
|
How do you treat a patient with Hypertrophic Cardiomyopathy?
|
- Cessation of high-intensity athletics (at risk for sudden cardiac death)
- Use of β-blocker or non-dihydropyridine CCB (eg, verapamil) - Implantable cardioverter defibrillator (ICD) if patient is at high risk |
|
|
What kind of dysfunction is associated with Hypertrophic Cardiomyopathy? What type of growth in the walls of the ventricles?
|
- Diastolic dysfunction
- Marked concentric hypertrophy of ventricles (often septal predominance; sarcomeres added in parallel) |
|
|
What is the appearance of a heart with Hypertrophic Cardiomyopathy?
|
- Marked ventricular hypertrophy (often septal predominance)
- Myofibrillar disarray and fibrosis |
|
|
What are the findings in a subset of patients with Hypertrophic Cardiomyopathy?
|
Obstructive HCM:
- Hypertrophied septum too close to anterior mitral leaflet - Leads to outflow obstruction - Causes dyspnea and possible syncope |
|
|
What are the major causes of restrictive / infiltrative cardiomyopathy?
|
- Sarcoidosis
- Amyloidosis - Postradiation fibrosis - Endocardial fibroelastosis (thick fibroelastic tissue in endocardium of young children) - Löffler syndrome - Hemochromatosis |
|
|
What is Löffler Syndrome?
|
- Endomyocardial fibrosis (causes restrictive / infiltrative cardiomyopathy)
- Prominent eosinophilic infiltrate |
|
|
What kind of cardiomyopathy does hemochromatosis cause?
|
- Restrictive / infiltrative cardiomyopathy
- Also can cause dilated cardiomyopathy |
|
|
What kind of dysfunction is associated with Restrictive Cardiomyopathy?
|
Diastolic dysfunction
|
|
|
What are the findings on EKG of some patients with Restrictive Cardiomyopathy?
|
Low-voltage EKG despite thick myocardium (especially amyloid)
|
|
|
What kind of dysfunction occurs in the three types of cardiomyopathy?
|
- Dilated CM: systolic
- Hypertrophic CM: diastolic - Restrictive CM: diastolic |
|
|
What happens if there is thick fibroelastic tissue in the endocardium? Who is most commonly affected by this?
|
Restrictive / Infiltrative Cardiomyopathy
- Endocardial fibroelastosis - More common in young children |
|
|
What is the term for the clinical syndrome of cardiac pump dysfunction?
|
Chronic Heart Failure
|
|
|
What are the symptoms of Chronic Heart Failure?
|
- Dyspnea
- Orthopnea - Fatigue |
|
|
What are the signs of Chronic Heart Failure?
|
- Rales
- JVD (jugular venous distention) - Pitting edema |
|
|
What kind of dysfunction can occur in Chronic Heart Failure?
|
- Systolic
- Diastolic |
|
|
What are the characteristics of Chronic Heart Failure with systolic dysfunction?
|
- Low Ejection Fraction (EF)
- Poor contractility - Often 2° to ischemic heart disease or DCM |
|
|
What are the characteristics of Chronic Heart Failure with diastolic dysfunction?
|
- Normal Ejection Fraction (EF)
- Normal contractility - Impaired relaxation - Decreased compliance |
|
|
What is the most common cause of R heart failure?
|
- Most commonly due to L heart failure
- Isolated R heart failure is usually due to cor pumonale |
|
|
What treatments can decrease the mortality of patients with Chronic Heart Failure?
|
- ACE-inhibitors
- β-blockers (except in decompensated HF) - ARBs (AngII receptor blockers) - Spironolactone (aldosterone antagonist) - Hydralazine + Nitrate therapy (improves symptoms and mortality in select patients) |
|
|
What treatments can be used for symptomatic relief in patients with Chronic Heart Failure, but don't decrease mortality?
|
Thiazide or loop diuretics
|
|
|
What is the cause of cardiac dilation in Chronic Heart Failure?
|
Greater ventricular end-diastolic volume (EDV)
|
|
|
What is the cause of dyspnea on exertion in Chronic Heart Failure?
|
Failure of CO to increase during exercise
|
|
|
What are the abnormalities seen in L heart failure?
|
- Pulmonary edema
- Orthopnea - Paroxysmal nocturnal dyspnea |
|
|
What are the abnormalities seen in R heart failure?
|
- Hepatomegaly (nutmeg liver)
- Peripheral edema - Jugular venous distention |
|
|
What causes pulmonary edema? Signs of pulmonary edema?
|
- ↑ Pulmonary venous pressure → pulmonary venous distention and transudation of fluid
- Presence of hemosiderin-laden macrophages ("heart failure" cells) in the lungs - Caused by L heart failure |
|
|
What is the meaning of "hemosiderin-laden macrophages" in the lungs?
|
These are "heart failure" cells - they indicate L heart failure which caused pulmonary edema
|
|
|
What causes orthopnea?
|
- Shortness of breath when supine: ↑ venous return from redistribution of blood (immediate gravity effect) exacerbates pulmonary vascular congestion
- Caused by L heart failure |
|
|
What causes paroxysmal nocturnal dyspnea?
|
Breathless awakening from sleep:
- ↑ Venous return from redistribution of blood, reabsorption of edema, etc Caused by L heart failure |
|
|
What causes hepatogmegaly (nutmeg liver)?
|
↑ Central venous pressure → ↑ resistance to portal flow
- Rarely leads to cardiac cirrhosis Caused by R heart failure |
|
|
What causes peripheral edema?
|
- ↑ Venous pressure → fluid transudation
- Caused by R heart failure |
|
|
What causes jugular venous distention (JVD)?
|
↑ venous pressure
Caused by R heart failure |
|
|
What are the direct implications of ↓ LV contractility?
|
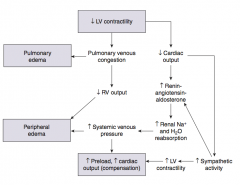
- Pulmonary venous congestion → Pulmonary Edema
- ↓ Cardiac output |
|
|
What are the implications of ↓ CO due to ↓ LV contractility?
|
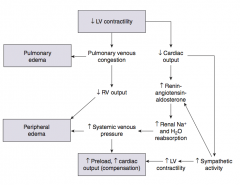
- Sympathetic activity → ↑ LV contractility
- ↑ Renin-angiotensin-aldosterone → - ↑ Renal Na+ and H2O reabsorption |
|
|
What are the implications of the increased renal Na+ and H2O reabsorption (d/t ↑renin-ang-aldosterone) that occurs in the context of L heart failure?
|
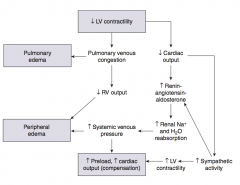
- ↑ Systemic venous pressure →
- ↑ Preload, ↑ Cardiac Output (compensation) AND - Peripheral edema |
|
|
What are the implications of pulmonary venous congestion that occurs in the context of L heart failure?
|
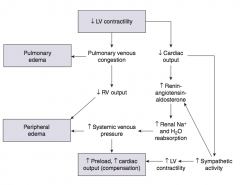
- Pulmonary edema AND
- ↓ RV output → Peripheral edema |
|
|
What is the most common symptom in a patient with bacterial endocarditis?
|
Fever
|
|
|
What are the symptoms of a patient with bacterial endocarditis?
|
♥︎ Bacteria FROM JANE ♥︎
Fever Roth spots Osler nodes Murmur (new) Janeway lesions Anemia Nail-bed hemorrhage Emboli |
|
|
What is the term for the round white spots on the retina, surrounded by hemorrhage? Sign of?
|
Roth spots - sign of bacterial endocarditis
|
|
|
What is the term for the tender raised lesions on fingers or toe pads? Sign of?
|
Osler nodes - sign of bacterial endocarditis
|
|
|
What is the term for the small, painless, erythematous lesions on the palm or sole? Sign of?
|
Janeway lesions - sign of bacterial endocarditis
|
|

What is this an image of? Sign of?
|

Nail-bed splinter hemorrhages - sign of bacterial endocarditis
|
|
|
How do you diagnose bacterial endocarditis?
|
Multiple blood cultures are necessary
|
|
|
What is the most common cause of ACUTE bacterial endocarditis? Characteristics?
|
S. aureus (high virulence)
- Large vegetations form on previously normal valves - RAPID onset |
|
|
What is the most common cause of SUB-ACUTE bacterial endocarditis? Characteristics?
|
Viridans Streptococci (low virulence)
- Smaller vegetations on congenitally abnormal or diseased valves - Sequela of dental procedures - GRADUAL onset |
|
|
What is the most common cause of CULTURE-NEGATIVE endocarditis? Characteristics?
|
- Most likely Coxiella burnetii and Bartonella species
- May also be non-bacterial 2° to malignancy, hypercoagulable state, or lupus (marantic / thrombotic endocarditis) - S. bovis is present in colon cancer, S. epidermidis on prosthetic valves |
|
|
What is the difference between acute and subacute bacterial endocarditis in terms of rate of onset?
|
- Acute: rapid onset
- Subacute: gradual onset |
|
|
What is the difference between acute and subacute bacterial endocarditis in terms of the most common cause? Virulence?
|
- Acute: S. aureus (high virulence)
- Subacute: Viridans streptococci (low virulence) |
|
|
What is the difference between acute and subacute bacterial endocarditis in terms of the characteristics of the valves that are affected?
|
- Acute: large vegetations on previously normal valve
- Subacute: smaller vegetations on congenitally abnormal or diseased valves |
|
|
If a patient has healthy valves, what is the more likely cause of bacterial endocarditis? Characteristics?
|
- S. aureus (high virulence)
- Large vegetations - Rapid onset |
|
|
If a patient has congenitally abnormal or diseased valves, what is the more likely cause of bacterial endocarditis? Characteristics?
|
- Viridans streptococci (low virulence)
- Smaller vegetations - Sequela of dental procedures - Gradual onset |
|
|
What is the most likely cause of bacterial endocarditis in a patient with colon cancer?
|
S. bovis
|
|
|
What is the most likely cause of bacterial endocarditis in a patient with prosthetic valves?
|
S. epidermidis
|
|
|
Which valves are affected by bacterial endocarditis?
|
- Mitral valve most common (left side of heart)
- Tricuspid valve endocarditis is associated with IV drug abuse (don't "tri" drugs) |
|
|
When the tricuspid valve has bacterial endocarditis, what is the most likely cause?
|
- IV drug abuse
- S. aureus, Pseudomonas, and Candida |
|
|
What are the potential complications of bacterial endocarditis?
|
- Choradae rupture
- Glomerulonephritis - Suppurative pericarditis - Emboli |
|
|
What is the cause of Rheumatic Fever?
|
Consequence of pharyngeal infection with group A β-hemolytic streptococci
|
|
|
What causes early deaths in patients with Rheumatic Fever?
|
Myocarditis
|
|
|
What is the effect of Rheumatic Fever on the heart?
|
Affects heart valves: Mitral > Aortic >> Tricuspid (high-pressure valves affected most)
- Early lesion is mitral valve regurgitation - Late lesion is mitral stenosis |
|
|
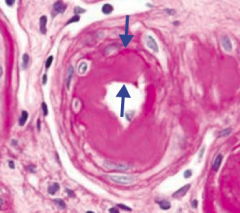
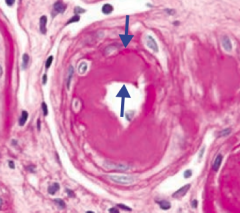
What are the histologic correlates of Rheumatic fever?
|
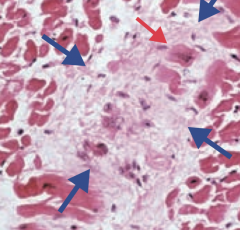
- Aschoff bodies (granuloma with giant cells - blue arrow)
- Anitschkow cells (enlarged macrophages with ovoid, wavy, rod-like nucleus - red arrow) |
|
|
What are Aschoff bodies? Sign of?
|

- Granuloma with giant cells (blue arrows)
- Sign of Rheumatic fever |
|
|
What are Anitschow cells?
|
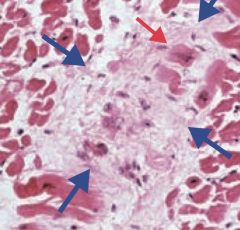
- Enlarged macrophages with ovoid, wavy, rod-like nucleus (red arrow)
- Sign of Rheumatic fever |
|
|
What labs are consistent with a diagnosis of Rheumatic fever?
|
- ↑ ASO titers (Anti-Streptolysin O)
- Antibodies to M protein - ↑ ESR |
|
|
How is the heart valve damage in Rheumatic fever mediated?
|
- Immune mediated (type II hypersensitivity) - not a direct effect of bacteria
- Antibodies to M protein cross react with self-antigens |
|
|
What are the characteristics of Rheumatic Fever?
|
FEVERSS:
- Fever - Erythema marginatum - Valvular damage (vegetation and fibrosis) - ESR ↑ - Red-hot joints (migratory polyarthritis) - Subcutaneous nodules - St. Vitus' dance (Sydenham chorea) |
|
|
What pathology presents with sharp pain, aggravated by inspiration, and relieved by sitting up and leaning forward?
|
Acute Pericarditis
|
|
|
What are the symptoms of Acute Pericarditis?
|
- Sharp pain
- Aggravated by inspiration - Relieved by sitting up and leaning forward - Friction rub |
|
|
What are the signs on EKG that support a diagnosis of Acute Pericarditis?
|
Widespread ST segment elevation and/or PR depression (whereas MI would have focal ST elevation)
|
|
|
What are the forms of Acute Pericarditis?
|
- Fibrinous
- Serous - Suppurative / Purulent |
|
|
What is the cause of fibrinous Acute Pericarditis? Signs?
|
- Caused by Dressler syndrome (auto-immune phenomenon that occurs several weeks post-MI)
- Also caused by uremia or radiation - Presents with loud friction rub |
|
|
What is the cause of serous Acute Pericarditis? Signs?
|
- Viral pericarditis - often resolves spontaneously
- Non-infectious inflammatory diseases - eg, rheumatoid arthritis, SLE |
|
|
What is the cause of suppurative / purulent Acute Pericarditis? Signs?
|
- Usually due to bacterial infections (eg, Pneumococcus, Streptococcus)
- Rare now with antibiotics |
|
|
What is the term for compression of the heart by fluid (eg, blood or effusions)?
|
Cardiac Tamponade
|
|
|
What happens in Cardiac Tamponade?
|
- Heart is compressed by fluid (eg, blood or effusions) in the pericardium
- Leads to ↓ CO - Equilibration of diastolic pressures in all 4 chambers |
|
|
What are the findings of Cardiac Tamponade?
|
- Beck triad (hypotension, distended neck veins, distant heart sounds)
- ↑ HR - Pulsus paradoxus - Kussmaul sign - EKG shows low-voltage QRS and electrical alternans (d/t swinging movement of heart in a large effusion) |
|
|
What is the Beck triad? Sign of?
|
- Hypotension
- Distended neck veins - Distant heart sounds - Sign of Cardiac Tamponade |
|
|
What is Pulsus Paradoxus? Sign of?
|
- ↓ in amplitude of systolic BP by ≥ 10 mmHg during inspiration
- Seen in cardiac tamponade, asthma, obstructive sleep apnea, pericarditis, and croup |
|
|
What is the term for a decreased amplitude of systolic BP by ≥ 10 mmHg during inspiration? Sign of?
|
Pulsus Paradoxus
- Seen in cardiac tamponade, asthma, obstructive sleep apnea, pericarditis, and croup |
|
|
What is Kussmaul sign? Sign of?
|
- Paradoxical ↑ in jugular venous pressure (JVP) on inspiration (should be ↓)
- Inspiration → negative intrathoracic pressure not transmitted to heart → impaired filling of RV → blood backs up in vena cavae → JVD - Seen in cardiac tamponade, constrictive pericarditis, restrictive cardiomyopathies, RA or RV tumors |
|
|
What are the signs on EKG in a patient with Cardiac Tamponade?
|
- Low voltage QRS
- Electrical alternans (due to swinging motion of heart in large effusion) |
|
|
If someone's aorta is described as looking like "tree bark" what should you think of?
|
Syphilitic heart disease (3° syphilis causes calcification of the aortic root and ascending aortic arch)
|
|
|
How can syphilis affect the heart?
|
- 3° Syphilis disrupts the vasa vasorum of the aorta
- Leads to atrophy of the vessel wall and dilation of the aorta and valve ring - May see calcification of the aortic root and ascending aortic arch - Leads to "tree bark" appearance of aorta |
|
|
What can be the consequences of syphilitic heart disease?
|
Can result in aneurysm of the ascending aorta or aortic arch and aortic insufficiency
|
|
|
What are the types of cardiac tumors? Most common?
|
- Most common: metastasis (eg, from melanoma or lymphoma)
- Myxoma (most common 1° cardiac tumor in adults) - Rhabdomyoma (most common 1° cardiac tumor in children) |
|
|
What is the most common 1° cardiac tumor in adults? Where do they occur?
|
Myxomas - 90% occur in atria (mostly LA)
|
|
|
What should you think of if there is a "ball valve" obstruction in the LA, associated with multiple syncopal episodes?
|
Myxoma
|
|
|
What is the appearance of a Myxoma?
|
Ball valve obstruction, usually in LA
|
|
|
What symptoms may a Myxoma present with?
|
Multiple syncopal episodes (because it obstructs blood flow to brain and elsewhere)
|
|
|
What is the most common 1° tumor in children? What is it associated with?
|
Rhabdomyomas - associated with tuberous sclerosis
|
|
|
What is the term for decreased blood flow to the skin due to arteriolar vasospasms, in response to cold temperature or emotional stress?
|

Raynaud Phenomenon
|
|
|
What is the mechanism of Raynaud Phenomenon? Where does it occur?
|

- Decreased blood flow to skin due to arteriolar vasospasm
- May be in response to cold temperature or emotional stress - Most often in the fingers and toes |
|
|
What causes Raynaud Phenomenon?
|
- Raynaud disease (1°, idiopathic)
- Raynaud syndrome (2° to a disease process such as mixed CT disease, SLE, or CREST (limited form of systemic sclerosis) syndrome) |
|
|
What blood vessels are affected by Raynaud Phenomenon?
|
Small vessels (arterioles)
|
|
|
What are the types of vascular tumors?
|
- Strawberry hemangioma
- Cherry hemangioma - Pyogenic granuloma - Cystic hygroma - Glomus tumor - Bacillary angiomatosis - Angiosarcoma - Lymphangiosarcoma - Kaposi sarcoma |
|
|
What is the name of the benign capillary hemangioma of infancy that appears in the first few weeks of life (1/200), grows rapidly, and regresses spontaneously at 5-8 years of age?
|

Strawberry hemangioma
|
|
|
What is the name of the benign capillary hemangioma of the elderly that does not regress and increases in frequency with age?
|

Cherry hemangioma
|
|
|
What is the name of the polypoid capillary hemangioma that can ulcerate and bleed? What is it associated with?
|
Pyogenic granuloma
- Associated with trauma and pregnancy |
|
|
What is the name of the cavernous lymphangioma of the neck? What is it associated with?
|
Cystic Hygroma
- Associated with Turner Syndrome |
|
|
What is the name of the benign, painful, red-blu tumor under fingernails? What does it arise from?
|
Glomus tumor
- Arises from modified smooth muscle cells of glomus body |
|
|
What is the name of the benign capillary skin papules caused by Bartonella hensalae infections? Who is it associated with?
|
Bacillary Angiomatosis
- Found in AIDS patients - Frequently mistaken for Kaposi sarcoma |
|
|
What is the name of the rare blood vessel malignancy that occurs on the head, neck, and breast areas (sun-exposed areas), usually in the elderly? What is it associated with?
|
Angiosarcoma
- Associated with radiation therapy and arsenic exposure - Very aggressive and difficult to resect due to the delay in diagnosis |
|
|
What is the name of the lymphatic malignancy associated with persistent lymphedema (eg, post-radical mastectomy)?
|
Lymphangiosarcoma
|
|
|
What is the name of the endothelial malignancy most commonly of the skin, but also mouth, GI tract, and respiratory tract? What is it associated with?
|
Kapsoi Sarcoma
- Associated with HHV-8 and HIV - Frequently mistaken for bacillary angiomatosis |
|

What are the characteristics of a Strawberry Hemangioma?
|
- Benign capillary hemangioma of infancy
- Appears in first few weeks of life (1/200 births) - Grows rapidly and regresses spontaneously at 5-8 years old |
|

What are the characteristics of a Cherry Hemangioma?
|
- Benign capillary hemangioma of elderly
- Does not regress - Frequency increases with age |
|
|
What are the characteristics of a Pyogenic Granuloma?
|
- Polypoid capillary hemangioma
- Can ulcerate and bleed - Associated with trauma and pregnancy |
|
|
What are the characteristics of a Cystic Hygroma?
|
- Cavernous lymphangioma of neck
- Associated with Turner Syndrome |
|
|
What are the characteristics of a Glomus Tumor?
|
- Benign, painful, red-blue tumor under fingernails
- Arises from modified smooth muscle cells of glomus body |
|
|
What are the characteristics of a Bacillary Angiomatosis?
|
- Benign capillary skin papule found in AIDS patients
- Caused by Bartonella henselae infections - Frequently mistaken for Kaposi sarcoma |
|
|
What are the characteristics of an Angiosarcoma?
|
- Rare blood vessel malignancy typically occurring in the head, neck, and breast areas
- Usually in elderly or sun-exposed areas - Associated with radiation therapy and arsenic exposure - Very aggressive and difficult to resect due to delay in diagnosis |
|
|
What are the characteristics of a Lymphangiosarcoma?
|
Lymphatic malignancy associated with persistent lymphedema (eg, post radical mastectomy)
|
|
|
What are the characteristics of a Kaposi Sarcoma?
|
- Endothelial malignancy most commonly of the skin, but also mouth, GI tract, and respiratory tract
- Associated with HHV-8 and HIV - Frequently mistaken for bacillary angiomatosis |
|
|
Which vascular tumor is associated with infancy?
|
Strawberry hemangioma
|
|
|
Which vascular tumor is associated with trauma and pregnancy?
|
Pyogenic granuloma
|
|
|
Which vascular tumor is associated with Turner Syndrome?
|
Cystic Hygroma
|
|
|
Which vascular tumor is associated with the fingernails?
|
Glomus Tumor
|
|
|
Which vascular tumor is associated with AIDS patients and is caused by Bartonella henselae?
|
Bacillary Angiomatosis
|
|
|
Which vascular tumor is associated with radiation therapy and arsenic exposure?
|
Angiosarcoma
|
|
|
Which vascular tumor is associated with persistent lymphedema (eg, post-radical mastectomy)?
|
Lymphangiosarcoma
|
|
|
Which vascular tumor is associated with HHV-8 and HIV?
|
Kaposi Sarcoma
|
|
|
What are the large-vessel vasculitides?
|
- Temporal (giant cell) arteritis
- Takayasu arteritis |
|
|
What are the medium-vessel vasculitides?
|
- Polyarteritis nodosa
- Kawasaki disease - Buerger disease (thromboangiitis obliterans) |
|
|
What are the small-vessel vasculitides?
|
- Granulomatosis with polyangiitis (Wegener)
- Microscopic polyangiitis - Churg-Strauss Syndrome - Henoch-Schönlein Purpura |
|
|
What are the large-vessel vasculitides?
|
- Temporal (giant cell) arteritis
- Takayasu arteritis |
|
|
Which vasculitis is generally seen in elderly females with unilateral headaches, jaw claudication, which may lead to irreversible blindness? What is it associated with? Pathology / Labs?
|
Temporal (giant cell) arteritis - large vessel vasculitis
- Unilateral headache due to temporal artery - Irreversible blindness due to ophthalmic artery occlusion - Associated with polymyalgia rheumatica - Most commonly affects branches of carotid artery - Focal granulomatous inflammation (picture) - ↑ ESR - Treat w/ high-dose corticosteroids prior to temporal artery biopsy to prevent vision loss |
|
|
Which vasculitis is generally seen in Asian females <40 years old, presents as "pulseless disease" (weak upper extremity pulses), fever, night sweats, arthritis, myalgias, skin nodules, and ocular disturbances? Pathology / Labs?
|
Takayasu arteritis - large vessel vasculitis
- Granulomatous thickening and narrowing of aortic arch and proximal great vessels - ↑ ESR - Treat with corticosteroids |
|
|
What are the medium-vessel vasculitides?
|
- Polyarteritis nodosa
- Kawasaki disease - Buerger disease (thromboangiitis obliterans) |
|
|
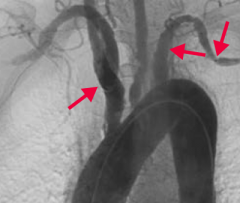
Which vasculitis is generally seen in young adults, 30% of which have HepB seropositivity? Other characteristics? Pathology / Labs?
|

Polyarteritis nodosa - medium vessel vasculitis
- Symptoms: fever, weight loss, malaise, headache, abdominal pain, melena - Hypertension, neurologic dysfunction cutaneous eruptions, renal damage - Typically involves renal and visceral vessels, not pulmonary arteries - Immune complex mediated - Transmural inflammation of the arterial wall with fibrinoid necrosis - Innumerable microaneurysms and spasm on arteriogram - Treat with corticosteroids, cyclophosphamide |
|
|
Which vasculitis is generally seen in Asian children <4 years old and can be treated with aspirin? Other characteristics? Pathology / Labs?
|

Kawasaki Disease - medium-vessel vasculitis
- Fever, cervical lymphadenitis, conjunctival infection, changes in lips/oral mucosa (strawberry tongue), hand-foot erythema, and desquamating rash - May develop coronary artery aneurysms, thrombosis → MI, rupture - Treat with IV immunoglobulin and aspirin (only time when it is okay to give a child aspirin |
|
|
Which vasculitis is generally seen in males <40 years old who are heavy smokers? Other characteristics? Pathology / Labs?
|
Buerger Disease (Thromboangiitis Obliterans)
- Intermittent claudication may lead to gangrene, auto-amputation of digits, superficial nodular phlebitis - Raynaud phenomenon is often present - Segmental thrombosing vasculitis - Treat with smoking cessation |
|
|
Which vasculitis is associated with the triad of focal necrotizing vasculitis, necrotizing granulomas in the lung and upper airway, and necrotizing glomerulonephritis?
|
Granulomatosis with Polyangiitis (Wegener) - small-vessel vasculitis
- URT: perforation of nasal septum, chronic sinusitis, otitis media, mastoiditis - LRT: hemoptysis, cough, dyspnea - Renal: hematuria, red cell casts - PR3-ANCA / c-ANCA (anti-proteinase 3) - CXR: large nodular densities - Treat with cyclophosphamide, corticosteroids |
|
|
Which vasculitis causes necrotizing vasculitis similar to granulomatosis with polyangiitis (Wegener's) but is without nasopharyngeal involvement? Other characteristics? Treatment?
|
Microscopic Polyangiitis - small-vessel vasculitis
- Necrotizing vasculitis affects the lungs, kidneys, and skin with pauci-immune glomerulonephritis and palpable purpura - No granulomas - MPO-ANCA / p-ANCA (anti-myeloperoxidase) - Treat with cyclophosphamide and corticosteroids |
|
|
Which vasculitis causes asthma, sinusitis, palpable purpura, peripheral neuropathy (eg, wrist/foot drop), but can also involve the heart, GI, and kidneys (pauci-immune glomerulonephritis)?
|
Churg-Strauss Syndrome - small-vessel vasculitis
- Granulomatous, necrotizing vasculitis with eosinophilia - MPO-ANCA / p-ANCA - ↑ IgE level |
|
|
Which vasculitis is the most common childhood systemic vasculitis that often follows URIs?
|

Henoch-Schönlein Purpura - small-vessel vasculitis
- Classic triad: palpable purpura on buttocks/legs; arthralgias; abdominal pain, melena, multiple lesions of same age - Vasculitis 2° to IgA complex deposition - Associated with IgA nephropathy |
|
|
What is the presentation and pathology / labs associated with Temporal (Giant Cell) Arteritis?
|
Large-Vessel Vasculitis
- Generally elderly females - Unilateral headache (temporal artery), jaw claudication - May lead to irreversible blindness d/t ophthalmic occlusion - Associated with polymyalgia rheumatica - Most commonly affects branches of carotid artery - Focal granulomatous inflammation - ↑ ESR - Treat with high-dose corticosteroids prior to temporal artery biopsy to prevent vision loss |
|
|
What is the presentation and pathology / labs associated with Takayasu Arteritis?
|
Large-vessel vasculitis:
- Asian females <40 years old - Pulseless disease (weak upper extremity pulses), fever, night sweats, arthritis, myalgias, skin nodules, and ocular disturbances - Granulomatous thickening and narrowing of aortic arch and proximal great vessels - ↑ ESR - Treat with corticosteroids |
|
|
What is the presentation and pathology / labs associated with Polyarteritis Nodosa?
|
Medium-Vessel Vasculitis
- Young adults - Hepatitis B seropositivity in 30% of patients - Fever, weight loss, malaise, headache - GI: abdominal pain, melena - HTN, neuro dysfunction, cutaneous eruptions, renal damage - Typically involves renal and visceral vessels, not pulmonary arteries - Immune complex mediated - Transmural inflammation of the arterial wall with fibrinoid necrosis - Innumerable microaneurysms and spasm on arteriogram - Treat with corticosteroids and cyclophosphamide |
|
|
What is the presentation and pathology / labs associated with Kawasaki Disease?
|
Medium-Vessel Vasculitis
- Asian children <4 years old - Fever, cervical lymphadenitis, conjunctival injection, changes in lips/oral mucosa ("strawberry tongue"), hand-foot erythema, desquamating rash - May develop coronary artery aneurysms, thrombosis → MI, rupture - Treat with IV immunoglobulin and aspirin |
|
|
What is the presentation and pathology / labs associated with Buerger Disease (Thromboangiitis Obliterans)?
|
Medium-Vessel Vasculitis
- Heavy smokers, males <40 years - Intermittent claudication may lead to gangrene, auto-amputation of digits, superficial nodular phlebitis - Raynaud phenomenon is often present - Segmental thrombosing vasculitis - Treat with smoking cessation |
|
|
What is the presentation and pathology / labs associated with Granulomatosis with Polyangiitis (Wegener)?
|
Small-Vessel Vasculitis
- URT: perforation of nasal septum, chronic sinusitis, otitis media, mastoiditis - LRT: hemoptysis, cough, dyspnea - Renal: hematuria, red cell casts Triad: - Focal necrotizing vasculitis - Necrotizing granulomas in lung and upper airway - Necrotizing glomerulonephritis - PR3-ANCA / c-ANCA (anti-proteinase 3) - CXR: large nodular densities - Treat with cyclophosphamide and corticosteroids |
|
|
What is the presentation and pathology / labs associated with Microscopic Polyangiitis?
|
Small-Vessel Vasculitis
- Necrotizing vasculitis commonly involving lungs, kidneys, and skin with pauci-immune glomerulonephritis - Palpable purpura - Presentation similar to granulomatosis with polyangiitis but without nasopharyngeal involvement - No granulomas - MPO-ANCA/p-ANCA (anti-myeloperoxidase) - Treat with cyclophosphamide and corticosteroids |
|
|
What is the presentation and pathology / labs associated with Churg-Strauss Syndrome?
|
Small-Vessel Vasculitis
- Asthma, sinusitis, palpable purpura, peripheral neuropathy (eg, wrist/foot drop) - Can involve heart, GI, kidneys (pauci-immune glomerulonephritis - Granulomatous, necrotizing vasculitis with eosinophilia - MPO-ANCA/p-ANCA - ↑ IgE level |
|
|
What is the presentation and pathology / labs associated with Henoch-Schönlein Purpura?
|
Small-Vessel Vasculitis
- Most common childhood systemic vasculitis - Often follows URI Classic Triad: - Skin: palpable purpura on buttocks/legs - Arthralgias - GI: abdominal pain, melena, multiple lesions of same age - Vasculitis 2° to IgA complex deposition - Associated with IgA nephropathy |

