![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
102 Cards in this Set
- Front
- Back
|
What are the types of studies?
|
- Case-Control Study
- Cohort Study - Cross-Sectional Study - Twin Concordance Study - Adoption Study |
|
|
What kind of study calculates an "ODDS RATIO", eg, "patients with COPD had higher odds of a history of smoking than those without COPD"?
|
Case-Control Study (observational and retrospective)
- Compare a group of people WITH DISEASE to a group WITHOUT DISEASE - Look for prior exposure or risk factor - Asks, "what happened" |
|
|
What kind of study calculates the "RELATIVE RISK", eg, "smokers had a higher risk of developing COPD than non-smokers had"?
|
Cohort Study (observational and prospective or retrospective)
- Compares a group with a given EXPOSURE or risk factor to a group WITHOUT EXPOSURE - See if exposure ↑ likelihood of disease - Can be prospective ("who will develop disease?") or retrospective ("who developed disease [exposed vs non-exposed]?") |
|
|
What kind of study calculates "DISEASE PREVALENCE"?
|
Cross-sectional study (observational)
- Collect data from a group of people to assess frequency of disease (and related risk factors) at a particular time point - Asks "what is happening?" - Can show risk factor association with disease, but does NOT establish causality |
|
|
What kind of study measures "HERITABILITY"?
|
Twin Concordance Study
- Compares the frequency with which both monozygotic twins or both dizygotic twins develop the same disease |
|
|
What kind of study measures "HERITABILITY and influence of ENVIRONMENTAL FACTORS"?
|
Adoption Study
- Compares siblings raised by biological and adoptive parents |
|
|
What does a CASE-CONTROL Study measure? Design?
|
Measures:
- Odds Ratio (OR) - Eg, "patients with COPD had higher odds of a history of smoking than those without COPD" Design: - Observational and retrospective - Compare a group of people WITH DISEASE to a group WITHOUT DISEASE - Look for prior exposure or risk factor - Asks, "what happened" |
|
|
What does a COHORT Study measure? Design?
|
Measures:
- Relative Risk (RR) - Eg, "patients with COPD had higher odds of a history of smoking than those without COPD" Design: - Observational and prospective or retrospective - Compares a group with a given EXPOSURE or risk factor to a group WITHOUT EXPOSURE - See if exposure ↑ likelihood of disease - Can be prospective ("who will develop disease?") or retrospective ("who developed disease [exposed vs non-exposed]?") |
|
|
What does a CROSS-SECTIONAL Study measure? Design?
|
Measure:
- Disease prevalence - Can show risk factor association with disease, but does not establish causality Design: - Observational - Collect data from a group of people to assess frequency of disease (and related risk factors) at a particular time point - Asks "what is happening?" |
|
|
What does a TWIN CONCORDANCE Study measure? Design?
|
Measure:
- Heritability Design: - Compares the frequency with which both monozygotic twins or both dizygotic twins develop the same disease |
|
|
What does a ADOPTION STUDY Study measure? Design?
|
Measure:
- Heritability and influence of environmental factors Design: - Compares siblings raised by biological and adoptive parents |
|
|
What kind of study compares therapeutic benefits of 2 or more treatments, or of treatment and placebo?
|
Clinical Trial
|
|
|
What is the purpose of a Clinical Trial? How do you improve the quality of the data?
|
- Experimental study involving humans
- Compare therapeutic benefits of ≥2 treatments or treatments and placebo - Improved quality with: randomization, control, double-blind |
|
|
What does a double-blind study mean? Triple-blind?
|
- Double-blind: neither patient nor doctor knows whether the patient is in the treatment or control group
- Triple-blind: researcher analyzing the data doesn't know whether the patient is in the treatment or control group either |
|
|
What happens in Phase I of a clinical trial? What are you analyzing?
|
- Small number of healthy volunteers
- Assess safety, toxicity, and pharmacokinetics |
|
|
What happens in Phase II of a clinical trial? What are you analyzing?
|
- Small number of patients with disease of interest
- Assess treatment efficacy, optimal dosing, and adverse effects |
|
|
What happens in Phase III of a clinical trial? What are you analyzing?
|
- Large number of patients randomly assigned either to the treatment under investigation or to the best available treatment (or placebo)
- Compares the new treatment to the current standard of care |
|
|
What happens in Phase IV of a clinical trial? What are you analyzing?
|
- Post-marketing surveillance trial of patients after approval
- Detects rare or long-term adverse effects |
|
|
In what Phase of Clinical Trials do you compare the new treatment to the current standard of care (or placebo)?
|
Phase III
|
|
|
In what Phase of Clinical Trials is the purpose to detect rare or long-term adverse effects
|
Phase IV
|
|
|
What is the term for the proportion of all people WITH DISEASE who test POSITIVE, ie, the probability that a test detects the disease when the disease is present?
|
Sensitivity (true-positive rate)
(RED) |
|
|
What is the term for the proportion of all people WITHOUT DISEASE who test NEGATIVE, ie, the probability that a test indicates non-disease when disease is absent?
|
Specificity (true-negative rate)
(GREEN) |
|
|
What does "Sensitivity" measure?
|
Proportion of all people WITH DISEASE who test POSITIVE, ie, the probability that a test detects the disease when the disease is present
(RED) |
|
|
What does "Specificity" measure?
|
Proportion of all people WITHOUT DISEASE who test NEGATIVE, ie, the probability that a test indicates non-disease when disease is absent?
(GREEN) |
|
|
What is a desirable "Sensitivity"? What does this mean?
|
- Value approaches 100%
- True positive rate, the higher the value, the greater the likelihood of being able to RULE OUT disease |
|
|
What is a desirable "Specificity"? What does this mean?
|
- Value approaches 100%
- True negative rate, the higher the value, the greater the likelihood of being able to RULE IN disease |
|
|
What quality is important for a screening test for a disease with low prevalence?
|
Test with high SENSITIVITY (true-positive rate) - good at ruling OUT disease if it is negative
If sensitivity is 100%, all negative must be TN (FN = 0) |
|
|
What quality is important for a confirmatory test for a disease with low prevalence, after a positive screening test?
|
Test with high SPECIFICITY (true-negative rate) - good at ruling IN disease if it is positive
If specificity is 100%, all positives must be TPs (FP = 0) |
|
|
How can you remember the difference between SENSITIVITY and SPECFICITY?
|
- SNOUT = SeNsitivity rules OUT
- SPIN = SPecificity rules IN |
|
|
How do you calculate Sensitivity?
|
Sensitivity = TP / (TP + FN) = 1 - false positive rate
TP = True Positive FN = False Negative (RED) |
|
|
How do you calculate Specificity?
|
Specificity = TN / (TN + FP) = 1 - false negative rate
TN = True Negative FP = False Positive (GREEN) |
|
|
What are the equations for Sensitivity and Specificity?
|
Sensitivity = TP / (TP + FN) = 1 - false positive rate
(RED) Specificity = TN / (TN + FP) = 1 - false negative rate (GREEN) TP = True Positive FN = False Negative TN = True Negative FP = False Positive |
|
|
How do sensitivity and specificity relate to HIV testing?
|
- Screen with ELISA (sensitive, high false-positive rate, low threshold)
- Confirm with Western Blot (specific, high false-negative rate, high threshold) |
|
|
What is the term for the probability that a person actually has the disease given a positive test result? How do you calculate this?
|
Positive Predictive Value (PPV)
- Proportion of positive test results that are true positive - PPV = TP / (TP + FP) (BLUE) |
|
|
What is the term for the probability that a person actually is disease free given a negative test result? How do you calculate this?
|
Negative Predictive Value (NPV)
- Proportion of negative test results that are true negative - NPV = TN / (FN + TN) (YELLOW) |
|
|
What are the equations for Positive Predictive Value (PPV) and Negative Predictive Value (NPV)?
|
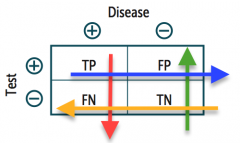
PPV = TP / (TP + FP)
(BLUE) NPV = TN / (FN + TN) (YELLOW) |
|
|
What does Positive Predictive Value (PPV) vary directly with? Negative Predictive Value (NPV)?
|
- PPV: varies directly with prevalence or pretest probability, high pretest probability → high PPV
- NPV: varies inversely with prevalence or pretest probability, high pretest probability → low NPV |
|
|
What is the difference between "INCIDENCE" and "PREVALENCE"?
|
- INCIDENCE: looks at new INCIDENTS
- PrevALence: looks at ALL current cases |
|
|
How do you calculate "Incidence Rate"?
|
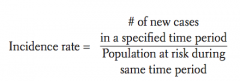
(# of new cases in a specified time period) / (population at risk during same time period)
|
|
|
How do you calculate "Prevalence"?
|
(# of existing cases) / (population at risk)
|
|
|
How do prevalence and incidence relate to each other numerically?
|
Prevalence ≈ Incidence Rate x Average Disease Duration
Prevalence > Incidence for chronic diseases (eg, diabetes) Incidence and prevalence are very similar for disease with short duration (eg, common cold) |
|
|
What terms can be used to "quantify risk"?
|
- Odds Ratio (OR)
- Relative Risk (RR) - Attributable Risk - Absolute Risk Reduction (ARR) - Number needed to treat - Number needed to harm |
|
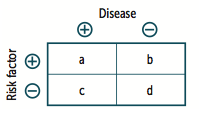
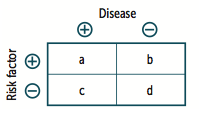
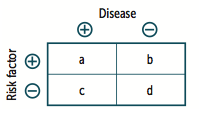
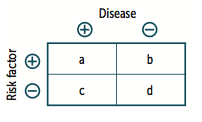
When is the "Odds Ratio" typically calculated? What does this term mean? How do you calculate?
|
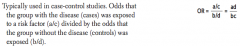
- Used in Case-Control Studies
- Odds that the group with the disease (cases) was exposed to a RISK FACTOR (a/c) divided by the odds that the group without the disease (controls) was exposed (b/d) Odds Ratio = (a/c) / (b/d) = ad/bc |
|
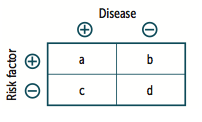
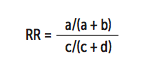
When is the "Relative Risk" typically calculated? What does this term mean? How do you calculate?
|
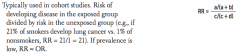
- Used in Cohort Studies
- Risk of developing disease in the exposed group divided by the risk in the unexposed group |
|
What is the "Relative Risk" for this example: 21% of smokers develop lung cancer vs 1% of non-smokers?
|
RR = 21 / 1 = 21
|
|
What does the term "Attributable Risk" mean? How do you calculate?
|
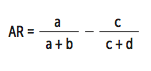
- Difference in risk between exposed and unexposed groups
- The proportion of disease occurrences that are attributable to the exposure |
|
What is the "Attributable Risk" for this example: 21% of smokers develop lung cancer vs 1% of non-smokers?
|
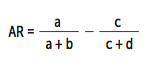
AR = 21 - 1 = 20%
This means that 20% of the 21% risk of lung cancer in smokers is attributable to smoking |
|
|
What does the term "Attributable Risk Reduction" mean?
|
Absolute reduction in risk associated with a treatment as compared to a control
|
|
|
What is the "Attributable Risk Reduction" for this example: 8% of people who receive the placebo vaccine develop the flu vs 2% of people who receive a flu vaccine?
|
ARR = 8 - 2 = 6%
This means that having the flu vaccine reduces your risk of getting the flu by 6% |
|
|
What does the "number needed to treat" value mean? How do you calculate it?
|
- Number of patients who need to be treated for 1 patient to benefit
- Calculated as 1 / absolute risk reduction (ARR) |
|
|
What does the "number needed to harm" value mean? How do you calculate it?
|
- Number of patients who need to be exposed to a risk factor for 1 patient to be harmed
- Calculated as 1 / attributable risk (AR) |
|
|
How do you calculate the "number needed to treat" vs "number needed to harm"?
|
- Number needed to treat: 1 / absolute risk reduction
- Number needed to treat: 1 / absolute risk |
|
|
What is the difference between precision and accuracy?
|
- Precision: consistency and reproducibility of a test (reliability)
- Accuracy: trueness of test measurements (validity) |
|
|
What is missing in a test that is "precise"?
|
Absence of random variation
- Random variation / error reduces the precision of a test (↑ precision → ↓ standard deviation) |
|
|
What is missing in a test that is "accurate"?
|
Absence of systematic error or bias in a test
- Systematic error reduces accuracy in a test |
|

What does this target demonstrate? Is there random error and/or systematic error?
|
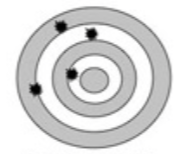
Not accurate, not precise
- Both random error (↓ precision) and systematic error (↓ accuracy) |
|

What does this target demonstrate? Is there random error and/or systematic error?
|

Accurate, but not precise
- Random error → ↓ precision - Low systematic error → accurate |
|

What does this target demonstrate? Is there random error and/or systematic error?
|

Precise, but not accurate
- Systematic error → ↓ accuracy - Low random error → precise |
|

What does this target demonstrate? Is there random error and/or systematic error?
|

Accurate and Precise
- Low systematic error → accurate - Low random error → precise |
|
|
When does "bias" occur?
|
Occurs when there is systematic error in a particular direction
|
|
|
What are the types of biases?
|
- Selection bias
- Recall bias - Sampling bias - Late-look bias - Procedure bias - Confounding bias - Lead-time bias - Observer-expectancy effect - Hawthorne effect |
|
|
What type of bias occurs when there is non-random assignment to participation in a study group? How can you reduce this type of bias?
|
Selection Bias
- Reduce bias with randomization and ensure the choice of the right comparison/reference group |
|
|
What type of bias occurs when awareness of the disorder alters recall by subjects? How can you reduce this type of bias?
|
Recall Bias
- Common in retrospective studies (eg, patient knows they have depression, they are more likely to tell you about the depressive symptoms than someone who hasn't been diagnosed with depression) Reduce bias: - Decrease time between exposure and follow-up |
|
|
What type of bias occurs when subjects are not representative of the general population? Implications for results?
|
Sampling Bias (type of selection bias)
- Results are not generalizable |
|
|
What type of bias occurs when information is gathered at an inappropriate time (eg, using a survey to study a fatal disease, only those still alive will be able to answer)?
|
Late-Look Bias
|
|
|
What type of bias occurs when subjects in different groups are not treated the same (eg, more attention is paid to treatment group, stimulating greater adherence)?
|
Procedure Bias
|
|
|
What type of bias occurs when a factor is related to both exposure and outcome but is not on the causal pathway; the factor distorts or confuses the effect of exposure on outcome? How can you reduce this type of bias?
|
Confounding Bias
Reduce bias: - Multiple / repeated studies - Crossover studies (subjects act as their own controls) - Matching (patients with similar characteristics in both treatment and control groups) |
|
|
What type of bias occurs when early detection is confused with increased survival (seen with improved screening even though natural history of disease is not changed)? How can you reduce this type of bias?
|
Lead-Time Bias
(makes it seem like the survival is improving, but this is partly due to the better screening) Reduce bias: - Measure "back-end" survival (adjust survival according to severity of disease at the time of diagnosis) |
|
|
What type of bias occurs when a researcher's belief in the efficacy of a treatment changes the outcome of that treatment?
|
Observer-Expectancy Effect
|
|
|
What type of bias occurs when the group being studied changes its behavior because they know they are being studied?
|
Hawthorne Effect
|
|
|
What is selection bias? What are the types of selection bias?
|
Non-random assignment to participate in a study group. Most commonly a sampling bias.
Examples: - Berkson Bias: eg, study looking only at inpatients - Loss to follow-up: eg, studying a disease with early mortality - Healthy worker and volunteer biases: eg, study populations are healthier than the general population |
|
|
What is recall bias? What are the ways to reduce bias?
|
- Awareness of disorder alters recall by subjects
- Common in retrospective studies - Patients with disease recall exposure after learning of similar cases Reduce bias: - Decrease time from exposure to follow-up |
|
|
What is measurement bias? What are the ways to reduce bias?
|
- Information is gathered in a way that distorts it
Reduce bias: - Use of placebo control groups with blinding to reduce influence of participants and researchers on experimental procedures and interpretation of outcomes |
|
|
What are the ways to reduce bias in a study?
|
- Blind studies to limit influence of participants and researchers on interpretation of outcome
- Placebo control studies - Crossover studies (each subject acts as own control) to limit confounding bias - Randomization to limit selection bias and confounding bias - Matching to reduce confounding bias |
|
|
What are the measures of central tendency?
|
- Mean: (sum of total values) / (total number of values)
- Median: middle value of a list of data sorted from least to greatest - Mode: most common value |
|
|
What are the measures of dispersion?
|
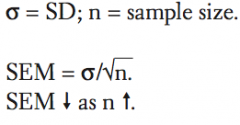
- Standard deviation: how much variability exists from the mean in a set of values
- Standard error of the mean: estimation of how much variability exists between the sample mean and the true population mean - Z-score - Confidence interval |
|
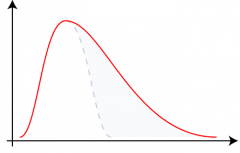
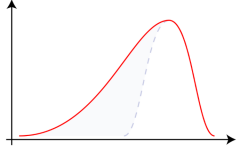
What distribution does this graph show? Implications?
|
Positive skew
- Asymmetry with longer tail on right - Mean > Median > Mode - Mode is least affected by outliers in the sample |
|
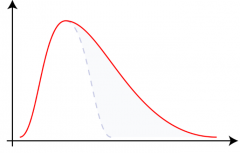
What distribution does this graph show? Implications?
|
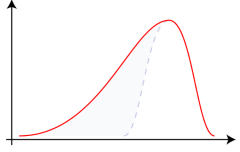
Negative Skew
- Asymmetry with longer tail on left - Mode > Median > Mean |
|
|
What is a "Null Hypothesis" (Ho)?
|
Hypothesis of no difference (eg, there is no association between the disease and the risk factor in the population)
|
|
|
What is a "Alternative Hypothesis" (H1)?
|
Hypothesis of some difference (eg, there is some association between the disease and the risk factor in the population)
|
|
|
What is "Type 1 error"? What is the probability of making a "Type 1 error"?
|
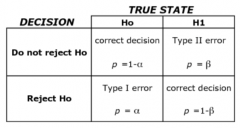
False-Positive Error
- States that there IS an effect or difference when NONE exists (mistakenly accept the alternative hypothesis and reject the null hypothesis) - α: probability of making a type 1 error, "p" value is judged against a preset α level of significance (usually <0.05) |
|
|
What is "Type 2 error"? What is the probability of making a "Type 2 error"?
|
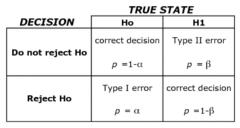
False-Negative Error
- States that there is NOT an effect or difference when one exists (to fail to rejecting the null hypothesis when it is false) - β: probability of making a type 2 error |
|
|
What is the difference between α and β?
|
- α: probability of making a type 1 error (you sAw a difference that did not exist)
- β: probability of making a type 2 error (you are Blind to a difference that did exist) |
|
|
What is Power? How do you calculate it?
|
Power = 1 - β
- Probability of rejecting the null hypothesis when it is in fact false - Likelihood of finding a difference if one in fact exists |
|
|
How do you increase the power of your study?
|
- ↑ Sample size
- ↑ Expected effect size - ↑ Precision of measurement |
|
|
How do you do a "meta-analysis"? Limitations?
|
- Pool data and integrate results from several similar studies to reach an overall conclusion
- ↑ Statistical power - Limited by quality of individual studies or bias in study selection |
|
|
What is the term for the range of values in which a specified probability of the means of repeated samples would be expected to fall?
|
Confidence Interval
|
|
|
What is a "Confidence Interval"? What is the typical Confidence Interval used?
|
- Range of values in which a specified probability of means of repeated samples would be expected to fall
- 95% Confidence Interval (corresponds to p < .5) |
|
|
If the 95% Confidence Interval for a mean difference between two variables includes 0, what does this mean?
|
There is no significant difference, Ho is not rejected
|
|
|
If the 95% Confidence Interval for an odds ratio or relative risk includes 1, what does this mean?
|
There is no significant difference, Ho is not rejected
|
|
|
If the 95% Confidence Interval between two groups do not overlap, what does this mean?
|
Significant difference exists, reject Ho
|
|
|
If the 95% Confidence Interval between two groups overlaps, what does this mean?
|
Usually no significant difference exists, Ho is not rejected
|
|
|
What statistical test is used to check the difference between the means of two groups?
|
t-test
|
|
|
What statistical test is used to check the difference between the means of three or more groups?
|
ANOVA (ANalysis Of VAriance of 3 or more groups)
|
|
|
What statistical test is used to check the difference between two or more percentages or proportions of categorical outcomes (not mean values)?
|
Chi-Square (Χ^2)
|
|
|
What is a primary form of disease prevention?
|
Prevent disease occurrence (eg, vaccination)
|
|
|
What is a secondary form of disease prevention?
|
Early detection of disease (eg, Pap smear)
|
|
|
What is a tertiary form of disease prevention?
|
Reduce disability from disease (eg, chemotherapy)
|
|
|
How do you remember the difference between Primary / Secondary / Tertiary levels of disease prevention?
|
PDR:
- 1: Prevent - 2: Detect - 3: Reduce disability |
|
|
What did Medicare and Medicaid originate from?
|
Federal programs that originated from amendments to the Social Security Act
|
|
|
Who qualifies for Medicare?
|
- Patients ≥65 years of age
- Patients <65 years of age with certain disabilities - Patients <65 years of age with end-stage renal disease (MedicarE is for the Elderly) |
|
|
Who qualifies for Medicaid?
|
Joint federal and state health assistance for people with very low income (MedicaiD is for the Destitute)
|

