![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
23 Cards in this Set
- Front
- Back
|
Hypoxaemia is defined as a reduction in blood O2. What are the 4 potential causes of hypoxemia? |
1. Hypoxic hypoxia: too little oxygen available to the lungs; this may be caused by low oxygen atmosphere, airway obstruction, drowning etc. 2. Stagnant hypoxia: inability of the heart to pump blood in sufficient quantities to meet the needs of the body 3. Anaemic hypoxia: reduced levels of functioning haemoglobin (this may be related to blood loss, conditions such as sickle cell disease where the shape of the haemoglobin is altered, or anaemia itself) 4. Histotoxic hypoxia: the inability of cells to take up the circulating oxygen. |
|
|
Why are COPD patient’s more susceptible to rightside heart failure? |
If a section of lung is poorly ventilated the pulmonary circulation constricts so that blood is not delivered to the hypoventilated region. In COPD there is likely to be widespread poor pulmonary ventilation and therefore widespread pulmonary constriction. Pulmonary vasoconstriction leads to pulmonary hypertension, which in turn increases the work load of the Heart in the Right Ventricle. This can result in cor pulmonale. |
|
|
What is hypercapnia? |
Hypercapnia refers to an increase in the PCO2 of arterial blood. PCO2 is proportional to carbon dioxide production and inversely related to alveolar ventilation (the greater the alveolar ventilation the lower the PCO2 and vice versa). |
|
|
Hypercapnia (elevated PCO2 levels) lead to a reduced pH (respiratory acidosis). The extent of acidosis is dependent on whether respiratory failure is acute or chronic. How do their presentations differ? |
Acute – Large increase in PCO2 with minimal increase in HCO3- as a buffer. Results in a significant drop in pH. Chronic – the kidneys retain HCO3- which leads to increased serum bicarbonate levels and relatively normal pH levels. The body adapts such that chronic increases in CO2 so that patients with chronic hypercapnia may not show symptoms until PCO2 becomes significantly raised. |
|
|
What are the components of the Respiratory Centre and where are the located? |
Rhythmicity Area (Medulla Oblongata). Pneumotaxic Area (Pons). Apneustic Area (Pons) |
|
|
The Medullary Rhymicity Area controls the basic rhythm of respiration, describe the control it exerts. |
Inhalation is an active process. In quiet breathing. Inspiratory centre active for 2 seconds – impulses to External Intercostal Muscles (intercostals nerves) and Diaphragm (phrenic nerve). Contraction causes inhalation. When impulses stop, passive elastic recoil causes exhalation for 3 seconds. In forceful breathing, impulses from Expiratory Centre cause contraction of Internal Intercostal Muscles and Abdominal Muscles causing forceful exhalation. |
|
|
What does the Pneumotaxic Area do? |
Pneumotaxic Area – transmits inhibitory impulses to the inspiratory area, turning off inspiratory area before the lungs over inflate. When the pneumotaxic area is more active, breathing rate is more rapid. |
|
|
Role of the respiratory system |
ventilate the lungs Transfer oxygen CO2 at the alveoli transport CO2 and 02 to and from the tissues after internal respiration. this maintains acid base balance. |
|
|
Haemaglobin |
Relaxed state when bound to 4 oxygen molecules. Taut state when unbound. increased affinity for oxygen as more is oxygen is bound. CO2 has a higher affinity for haemaglobin than oxygen. |
|
|
Oxygen dissociation curve |
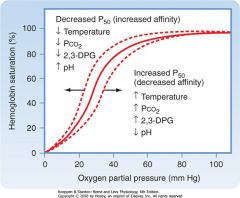
|
|
|
Bhor effect |
haemaglobin has a lower affinity for oxygen as CO2 increase, temp increases or H+ increases. |
|
|
Saturation |
Under normal circumstances 60mmHg of oxygen will provide saturation.
As the curve falls rapidly, if sats are 75% there could be a very quick decline. quicker release of oxygen in cells that are working hard as more CO2. |
|
|
Gas laws |
Boyle's law - pressure of a gas increases as the volume its contained within becomes smaller - change in altitude Henry's law - Increased pressure on a gas in liquid will increase the amount dissolved in a liquid - decompression sickness Dalton's law - Each gas in a mixture of gassess will exert it's own partial oressure as if the other gassess were not present. Charles law - volume of gas reduces as temp decreases. |
|
|
Lung volumes |
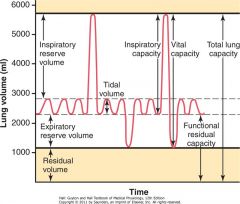
|
|
|
Respiratory acidosis |
high PCO2, High H+, low pH, normal bicarb caused by inadequate ventilation so retain CO2 causes - Acute resp faliure, CCF, Pulmonary oedema, CNS depression, COPD |
|
|
Resp alkalosis |
Low H+, low PCO2, pH high, normal bicarb caused by low CO2 due to hypervenntilation, mechanical over ventilation, pregnancy |
|
|
compensation |
high CO2 (low pH) will cause faster resps and visa versa. |
|
|
VQ mismatch |
Shunt- blockage / thickening of alveoli Dead space - Reduced blood flow |
|
|
resp faliure |
Type 1 - hypoxia without hypercapnnia (compensating) - VQ mismatch Type 2 - hypoxia plus hypercapnia - airway resistance |
|
|
respiratory anatomy |
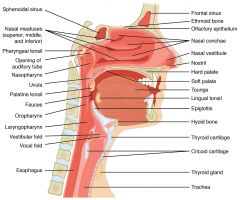
|
|
|
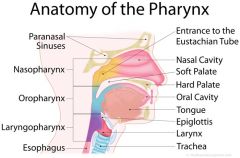
naso pharynx oropharynx laryngopharynx |
|
|
|
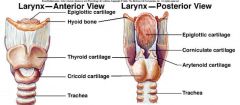
Laryngopharynx |
|
|
|
larynx 2 |

|

