![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
46 Cards in this Set
- Front
- Back
|
Define the terms flow and velocity with respect to the movement of fluid through tubes and state the relationship between them.
|
Flow: the volume of fluid which passes a certain point per unit of time.
Velocity: the rate of movement of particles in fluid along the tube. Flow = velocity x area ( r2¬¬) At fixed flow ie in the circulation: velocity is inversely proportional to area. So a small vessel eg aorta will have a high velocity whereas capillaries collectively have a large area and so a low velocity. At fixed pressure: velocity is proportional to area, so flow is proportional to radius4. |
|
|
Describe what is meant by laminar and turbulent flow.
|
Laminar flow is the usual flow of blood through vessels. The velocity is zero at the edge and increases towards the middle where the cells are found – velocity gradient. The concentric layers slide over each other (like an onion),
Cells flow centrally and faster and plasma is pushed to the edge where it travels more slowly. Turbulent flow is when the velocity gradient has broken down, fluid tumbles over and fluid resistance is greatly increased. Turbulent flow is achieved when mean velocity is very high, due to decreased viscosity or due to changing size of vessels – narrowing (stenosis) are widening (aneurysm). Turbulent flow can be heard with a stethoscope and the noise is called a bruit (French) - If due to decrease in viscosity - fewer cells/plasma proteins, bruit is heard all over body, in all arteries. - If due to aneurysm or stenosis, bruit is head at one place in artery. |
|
|
Describe what is meant by viscosity and the effect of viscosity upon flow.
|
Viscosity is the difficulty for concentric layers of blood in laminar flow to mover over each other.
A low viscosity, means the layers easily flow over each other and allows a high average velocity. A high viscosity, means the layers don’t easily flow other each other and so there is a low average velocity. Viscosity determines the slope of the gradient of velocity. Therefore at a constant gradient, the wider the tube, the faster the middle layers will move hence the higher the average velocity. Mean velocity is proportional to cross sectional area. As flow = velocity X area, flow = radius4 |
|
|
Under what circumstances will blood become more viscous?
|
Polycythemia - increased mass of red blood cells.
Increased plasma proteins – eg fibrinogen Myeloma – cancer of plasma cells - CRAB – calcium, renal failure, anaemia, bone lesions - Proliferation of haemopoetic cells – plasma cells made at expense of other blood cells - Paraprotein, an immunoglobin, prevents other immunoglobulins being made -> immunodeficiency and damages the kidneys ( bence jones proteins) |
|
|
Describe the effects of changes in tube diameter on velocity ( flow rate)
|
.
If flow is constant: velocity is inversely proportional to cross sectional area. - Increase in tube diameter, decrease in velocity eg capillaries - Decrease in tube diameter, increase in velocity eg aorta If pressure gradient and viscosity is constant: velocity is proportional to cross sectional area. - The wider the tube, the more velocity can increase towards the middle of the tube so the larger the average velocity - The small the tube, the less the velocity can increase an sot the smaller the average velocity. |
|
|
Define the term resistance to flow and state the factors which affect flow resistance.
|
The resistance to flow that must be overcome in order to circulate blood around the body.
Resistance = pressure/ flow - Increase resistance, increases pressure to overcome resistance and allow blood flow Changes in flow of blood: - Resistance increases as viscosity increases - Resistance increases if flow becomes turbulent – stenosis or aneurysm. - Resistance increases due to vasoconstriction |
|
|
Describe the effects of combining flow resistances in series and in parallel.
|
If vessels are in series – resistance adds
If vessels are in parallel – resistance is lower |
|
|
Describe the relationship between flow, resistance and pressure.
|
Resistance = pressure/ flow
- If pressure is constant, the higher the resistance the smaller the flow. - If flow is constant, the higher the resistance the greater the pressure. |
|
|
Describe the pattern of flow resistance and pressure over the systemic circulation.
|
If flow is fixed over the whole circulation:
- Arteries is low resistance -> pressure drop over arteries is small ( does not require pressure to overcome much resistance) - Arterioles is high resistance -> pressure drop over arterioles is large ( requires lots of pressure to overcome resistance) - Capillaries is OVERALL low resistance ( individually high, but there are many arranged in parallel ) -> low pressure drop over capillaries - Veins and venules low resistance -> pressure drop is low |
|
|
Why is pressure in arteries high?
|
The pressure in arteries is high because of the high resistance of the arterioles.
- Given a total flow, the higher the resistance of the arterioles, the higher the arterial pressure! |
|
|
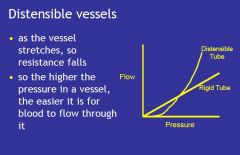
Draw the graph of flow against pressure with a distensible and a rigid vessel.
|
|
|
|
Describe how distensibility of blood vessels affects the relationship between flow and pressure and produces the property of capacitance.
|
Transmural pressure – the pressure difference between the inside and outside of tube, stretches the vessel -> the resistance falls -> flow increases.
As pressure within distensible vessels falls, the walls collapse and blood flow stops before the pressure falls to zero. If pressure changes suddenly, more blood will flow into than out of the tube as it distends. Distensible tubes can store blood – capacitance. Veins are the most distensible – thin walls with little smooth muscle. |
|
|
Define the term systolic and diastolic arterial pressure and the pulse pressure.
|
The systolic pressure is the peak pressure achieved in systole. Eg 120mmHg
The diastolic pressure is the minimum pressure reached in diastole. Eg 80mmHg The pulse pressure is the difference between systolic and diastolic pressures. 120- 80 = 40mmHg. |
|
|
What is the effect of pressure on smooth muscle in vessel walls?
|
Pressure causes contraction of smooth muscle in arterioles which decreases the lumen and increases resistance to flow. This allows flow to be maintained.
flow = pressure/resistance increase pressure, increase flow increase resistance, decreae flow |
|
|
Define the term total peripheral resistance.
|
The total peripheral resistance is the collective resistance of the arterioles.
The high pressure in the arteries is needed to overcome the total peripheral resistance to circulate the cardiac output. Total peripheral resistance is inversely proportional to the body’s need for blood flow. |
|
|
Describe how the elastic nature of arteries acts to reduce arterial pressure fluctuation.
|
The elastic recoil of the arteries maintains arterial pressure during ventricular diastole, when the pressure in the ventricles drops considerably.
If the arteries where rigid, the arterial pressure would rise enough in systole to force the whole stroke volume through the total peripheral resistance and arterial pressure would plummet to zero in diastole as it does in the ventricles. However, arteries have distensible walls so in systole, arteries stretch allowing more blood to flow in than out and so pressure does not rise so much. As arteries recoil in diastole, flow continues through the arterioles, so the arterial pressure is maintained although decreased. |
|
|
Draw the typical arterial pressure wave form.
|
The heart ejects blood intermittingly, in systole it ejects blood, in diastole it does not.
The wave increases during systole, to the systolic pressure and decreases during diastole to the diastolic pressure. The dicrotic notch seen during diastole shows the aortic valve closure where a slight increase in aortic pressure is caused by elastic recoil of the aorta. |
|
|
Describe the pulse wave.
|
The contraction of the ventricle also generates a pulse wave which propagates along the arteries faster than blood. This is felt at a variety of locations where arteries comes close to the surface and can be pushed against a reasonably hard surface. It is formed by the maximum peak being systolic pressure and the minimum point being diastolic pressure.
- rhythm, character, rate, volume |
|
|
Describe the role of arterioles as resistance vessels.
|
The arterioles direct perfusion of organs which are less easily perfused eg the brain by increasing the resistance of easy to perfuse areas.
Pre-capilary sphincters also increase resistance and allow artero-venous shunts. Resistance vessels increase resistance by vasoconstriction, narrowing the lumen. |
|
|
Define the terms vasoconstriction and vasodilation.
|
All vessels have vasomotor tone, a constant supply of sympathetic activity to the smooth muscle in the media.
When sympathetic activity increases to A1 adrenoreceptors, the smooth muscle in the vessel walls contracts further to narrow the lumen – vasoconstriction. When sympathetic activity decreases or B2 adrenoreceptors activated, the smooth muscle relaxes and the lumen widens –vasodilation. |
|
|
Describe what is meant by vasomotor tone and list the main factors which affect it.
|
Vasomotor tone is tonic contraction of smooth muscle in the vessel walls, produced by sympathetic innervations.
Vasodilator metabolites antagonise vasomotor tone. The actual resistance is a balance between sympathetic activity and the effects of vasodilator metabolites. |
|
|
Describe how vasodilator metabolites modify vasomotor activity to permit local control of blood flow.
|
Vasodilatior metabolites = H+, CO2, K+, adenosine – released from metabolically active tissues, which stimulate the smooth muscle in the tunica media to relax causing vasodilation.
There effect is a balance between the rate that they are produced and the rate at which they are washed away. This increases blood supply to the area, which is needed to maintain oxygen and nutrient demand of active tissue. When the tissues are no longer as active, the metabolites are washed away and the vessel calibre returns. - Skeletal muscle – in exercise, released vasodilator metabolites -> vasodilation - Gut – metabolism of a meal -> released vasodilator metabolites -> vasodialtion - - The force of contraction -> more force, greater pressure - The total peripheral resistance -> more resistance, greater pressure to overcome it. - Stretchiness of the arteries (compliance) -> arteries stiffen with age, pressure increases. What factors affect how far pressure in diastole falls? - Systolic pressure - Total peripheral resistance |
|
|
Describe reactive hyperaemia.
|
When blood flow is blocked, the vasodilator metabolites build up and cause maximum vasodilation.
Thus when the blood flow is returned, resistance is very low so flow is very high. But the high flow washes away the metabolites so the smooth muscle contracts again and vessel calibre is restored. |
|
|
Describe autoregulation.
|
Autoregulation is the intrinsic ability of a tissue to take what blood they need, despite changes in perfusion pressure. This is provided the perfusion pressures stay within limits.
- Eg if pressure increases and so flow increases, more metabolites will be removed causing vasoconstriction which increases resistance and thus returns flow to normal level - If pressure decreases, flow decreases and so metabolites build up causing vasodilation which decreases resistance and thus returns flow to norma. |
|
|
Define the terms central venous pressure and venous return.
|
Central venous pressure is the pressure in the great veins, SVC & IVC that supply the right atrium during diastole. It depends on.
- Return of blood from the body - Pumping of the heart - Muscle pumping and gravity. Venous return: volume of blood returned to right atrium. |
|
|
What factors affect how far pressure rises in systole?
|
- The force of contraction -> more force, greater pressure
- The total peripheral resistance -> more resistance, greater pressure to overcome it. - Stretchiness of the arteries (compliance) -> arteries stiffen with age, pressure increases. What factors affect how far pressure in diastole falls? - Systolic pressure - Total peripheral resistance |
|
|
Describe the effects of changes in total peripheral resistance at a given cardiac output on arterial and venous pressures.
|
Increase in TPR will increase arterial pressure and decrease venous pressure as more blood is taken from the veins and pumped into arteries to overcome resistance.
Decrease in TPR will decrease arterial pressure but increase venous pressure as there is less resistance the blood will flow into veins at a faster rate from the arteries but the blood will be removed from the veins at the same rate by the heart – increased venous volume, increased venous pressure. |
|
|
Describe the effects of arterial and venous pressure changes on cardiac output.
|
Increased arterial pressure
- Increased end systolic volume and decrease stroke volume as not as much blood is pumped out – harder to pump out blood. - Decreased cardiac output - Increased afterload - harder for blood to be ejected into the arteries. Decreased arterial pressure – decreased end systolic volume, increased cardiac output, decreased afterload. Decreased venous pressure - Decreases the end diastolic volume, thus decreases cardiac output. Increased venous pressure, increases end diastolic volume thus increases cardiac output. |
|
|
Describe the effects of changes in cardiac output at a given total peripheral resistance on arterial and venous pressures.
|
Increase in cardiac output will cause increased stroke volume/ heart rate -> decrease venous pressure and increase arterial pressure and vice versa.
|
|
|
What determines venous pressure?
|
Venous pressure is determined by the rate blood is removed from veins by heart ( heart rate) and the rate at which blood fills the veins.
A high venous pressure – blood is filling veins, faster than it is being taken from veins. A low venous pressure – blood is leaving veins, faster than it is being filled. |
|
|
Explain how the cardiovascular system will be stable if the cardiac output is increased by rises in venous pressure and falls in arterial pressure and vice versa.
|
For the cardiovascular system to be demand led and stable, when TPR changes and alters the arterial and venous pressure, the heart changes its pumping action to correct those disturbances.
The heart will respond to falls in arterial pressure and rises in venous pressure by pumping more blood around the body (increased cardiac output) to meet the metabolic demands by the body. When the demands are met the arterial and venous pressures will be brought back to normal and cardiac output decreased. - The venous pressure is reduced by extra pumping of the heart (the rate at which blood is taken out of the veins increases – increased cardiac ouput). - The arterial pressure is raised by increased stroke volume ( more blood in arteries = greater pressure exerted on vessel walls). - Baroreceptors in carotid sinuses and aortic arch– detect fall in arterial pressure and increase heart rate and contractility. - Falls in arterial pressure will increase flow resistance to certain tissues, such as the skin and gut, and this will increase arterial pressure. Falls in arterial pressure will also cause venoconstriction which will increase venous pressure. |
|
|
Define the terms stroke volume, end diastolic volume and end systolic volume. How is force of contraction and difficulty of ejecting blood determined?
|
Stroke volume - the volume of blood ejected from the left ventricle into the aorta. This volume is not the entire volume that is within the ventricle. Stroke volume = end diastolic volume – end systolic volume.
End diastolic volume – the volume of blood within the left ventricle just before systole. It is determined by the central venous pressure, the driving force of blood from great veins into the right atrium. End systolic volume – the volume of blood within the left ventricle after contraction. How much the ventricle empties is determined by the force of contraction and the difficulty of ejecting blood. Force of contraction is determined by end diastolic volume and contractility (preload). Difficulty of ejecting blood is determined by aortic impedance (factors that resist ventricular ejection i.e. obstruction) and TPR. The harder it is to eject blood, the higher the pressure rises in the arteries. |
|
|
Define the terms ‘pre-load’ and ‘after-load’ of the ventricular myocardium and what factors affect them.
|
After load – the pressure the ventricle must generate in order to expel blood from the heart into the aorta ie force of contraction.
- It is increased by aortic stenosis (calcified and stenotic valve) and by hypertension as the left ventricle must work harder to open the aortic valve as it has to generate a pressure greater than the aortic pressure. - After load is decreased in mitral regurgitation as blood from the left atrium regurgitates into the left ventricle and so the left ventricle does not need to work as hard. - Increased by increased TPR -> decreases stroke volume Preload – (end diastolic stretch) the pressure stretching the ventricle of the heart after passive filling of the ventricle and subsequent atrial contraction. Preload is determined by venous pressure - Increased venous pressure, increased preload – increased end diastolic volume. - Sympathetic innervations increases contractility -> increases preload |
|
|
Describe how changes in end-diastolic volume affect the force of contraction of the myocardium during the following systole.
|
An increase in end-diastolic volume causes the sarcomeres of the ventricular myocardium to stretch more, increases contractility . Increased contractility, increases the force of contraction of myocytes ( as they are stretched more) thus increases the stroke volume.
|
|
|
Draw a graph of the relationship between venous pressure and stroke volume at a constant after load eg constant TPR- the starling curve.
|
STARLINGS LAW: the more the heart fills, the more the myocytes stretch and thus the harder the heart contracts ( up to a limit). The harder it contracts the bigger the stroke volume and thus cardiac output. Rises in venous pressure cause rises in stroke volume – more in = more out!!
As end diastolic volume ( determined by venous pressure) increases, the stroke volume also increases as the extra volume causes the sarcomeres to stretch more and more until they reach the maximum sarcomere length and then recoil and are no longer effective, hence the drop in stroke volume. The pericardium prevents the heart from over expanding. |
|
|
Define the term contractility and describe how the starling curve is changed by factors which increase the contractility of the ventricular myocardium
|
Contractility ( preload) is the capacity of a muscle fibre to stretch AND is the slope of the starling curve - ventricular end diastolic volume against stroke volume.
The steeper the curve, the greater the contractility of the myocardium and so the greater the force of contraction. Contractility is increased by the sympathetic nervous system (noradrenalin and adrenalin) acting on the myocardium and has a +ve ionotrophic effect. |
|
|
Describe the effects of increases in venous return eg due to exercise, on venous pressure and cardiac output. Are there any problems associated with this? How can they be prevented.
|
Increases in venous return increase cardiac output as more blood is forced into the right atrium and the right and left heart are matched – both sides beat at same time, matched by stroke volume!
Pulmonary oedema: If venous return is greatly increased eg during exercise due to muscle pumping, the venous pressure will rise greatly and the arterial pressure will drop greatly. The high venous pressure will tend to fill the heart and cause maximum end diastolic volume. Usually if the right ventricle pumps more blood, the left ventricle can match the right ventricle by filling more and so pumping more. However in this situation the left ventricle can’t fill anymore and so blood accumulates in the lungs and causes pulmonary oedema. SOLUTION: overfilling of the ventricles is prevented by a rise in heart rate at the onset of exercise, triggered by the sympathetic nervous system. This rise in heart rate prevents venous pressure rising too much by pumping the extra blood immediately into arteries, keeping the stroke volume down. |
|
|
Describe the effect of decreases in venous return eg standing up, the problems associated with this and how they are prevented.
|
Decreases in venous return
Standing up results in blood pooling in the legs and thus producing a transient fall in central venous pressure. This is caused by gravity increasing transmural pressure of the superficial veins in the lower extremities causing them to distend. As the central venous pressure falls the cardiac output will fall, so arterial pressure will fall. As the venous pressure and arterial pressure both fall this cannot be corrected by normal mechanisms. SOLUTION: the fall in arterial pressure is detected by baroreceptors which trigger - Rises in heart rate, - vasoconstriction in skin and gut to increase TPR - venoconstriction to force more blood back towards the heart. The rise in TPR stabilises arterial pressure and maintains perfusion of vital organs such as brain. POSTURAL HYPOTENSION – sometimes the reflexes don’t work as seen in Addison’s disease and is very common in elderly – low arterial pressure, brain does not receive enough oxygen -> syncope. |
|
|
Describe how changes in after load affect stroke volume and peak systolic pressure at a given pre-load.
|
Afterload is the pressure required to force blood out of the ventricles and into the arteries. Afterload depends on the ease to eject blood, the TPR.
Falls in TPR reduce after load and so increase stroke volume. Increase in TPR increases afterload and so decreases stroke volume. |
|
|
Describe the way in which arterial receptors detect changes in arterial pressure
|
Baroreceptors are stretch receptors found in the wall of the aorta and in the carotid sinus ( bifurcation point of the common carotid artery) that detect changes in arterial pressure and transmit this information to the cardiovascular centres in the medulla of the brain where they modify the heart via the ANS.
|
|
|
Describe the effects of a fall in arterial pressure, detected by arterial baroreceptors, upon (i) heart rate (ii) ventricular contractility, and the autonomic mechanism which mediate them.
|
A fall in arterial pressure will be detected by the baroreceptors and will inhibit the parasympathetic innervations so that sympathetic innervations predominate. The heart rate increases, and the contractility of the heart of the heart increases.
|
|
|
Under what circumstances might a sudden increase in parasympathetic activity to the heart occur? What would this treat? How can parasympathetic activity by reduced?
|
Carotid sinus massage – baroreceptors detect increased pressure in arteries and cause activation of parasympathetic innervations.
Sudden stimulus of cold water – triggers parasympathetic stimulation Valsavas manoeuvre – expire against a closed glottis ( imagine you’d having a poo) All the above techniques may be used to treat tachycardia however in an individual with normal heart rate the great increase in parasympathetic activity may cause no cardiac output and collapse. To treat bradycardia atropine is given which blocks muscarinic receptors in parasympathetic innervations, increasing heart rate and contractility. ( +ve ionotrophic and chronotrophic). |
|
|
What happens to the output of the baroreceptors if there is a sustained rise in arterial pressure – lasting hours or days?
|
Accommodation occurs where the baroreceptors become used to the stimulus, prolonged hypertension, thus they require gradual treatment to bring chronic hypertension down and reset the baroreceptors.
|
|
|
Describe the effects of rises in venous pressure on heart rate.
|
There are also stretch receptors in the atria and great veins which detect venous pressure. If the venous pressure rises, then heart rate rises. This is called the Bainbridge reflex!!
|
|
|
What happens with a haemorrhage?
|
The reduced blood volume lowers venous pressure and so lowers cardiac output. The arterial pressure then falls which is detected by baroreceptors and causes heart rate to rise and TPR to rise. The rise in heart rate lowers the venous pressure further and the rise in TPR helps to raise arterial pressure but also lowers venous pressure making problem much worse.
The venous pressure is increased by veno-constriction which forces more blood back to heart and by auto transfusion where more fluid moves back into capillaries from tissues. Treatment is to give fluids to increase blood volume and thus venous pressure and prevent shock – toxins are released into blood during ischaemia and these cause vasodilation which further decreases arterial pressure! |
|
|
Describe how the CVS adapts to sustained increases in blood volume.What condition can arise? What treatment is given?
|
The blood volume can increase due to changes in the kidney or in the diet.
- The blood volume rises -> sustained increase in venous pressure - Increased venous pressure -> increased end diastolic volume -> increased cardiac output -> increased arterial pressure - Autoregulation of the tissues as they are receiving too much blood -> vasoconstriction -> increases TPR - Cardiac output returns to normal but hypertension persists - accomodation of barorecepors! Hypertension is resolved by reduction of blood volume, diuretics eg spirinolactone( ROMK – cortical collecting duct, triamzide ( Na-Cl cotransporter – distal convoluted), loop diuretic ( Na-K- 2Cl – cotransporter –loop), amiloride ( epithelial- Na channel – cortical collecting tubule) |

