![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
164 Cards in this Set
- Front
- Back
|
change in the normal expression of 1+ CAMs can lead to...
|
... pathologic alteration during tissue differentiation or maturation.
|
|
|
Epithelial cells - general characteristics
|
- closely apposed and tightly adherent (cell-to-cell - adhesion molecules)
- functional & morphologic polarity (usually) - avascular: supplied by blood vessels in the underlying CT |
|
|
3 "sides" of the epithelial cell
|
these sides constitute the polarity of the epithelial cell:
- apical surface: free surface; will face lumen if applicable - basal surface: attaches to the basement membrane - lateral surface: typically attaches to the adjacent cell |
|
|
what 2 tissue types have cell-to-cell adhesion molecules?
|
epithelial and muscle
|
|
|
classification of epithelial cells is based on 3 things
|
cell shape, number of cell layers, surface specializations
NOTE: histological classification refers only to cell shape and # of layers |
|
|
squamos
|
Flat; width greater than height; Nuclei usually also horizontal to surface
|
|
|
cuboidal
|
Width, height, depth about equal
|
|
|
columnar
|
Height significantly greater than width
|
|
|
simple
|
1 layer
|
|
|
stratified
|
multiple layers; classified based on the uppermost layer of cells (closest to lumen)
|
|
|
transitional
|
rounded, dome shaped cells in the top layer
|
|

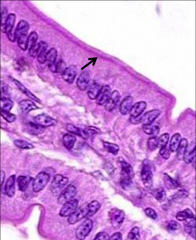
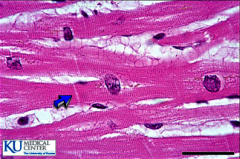
what is the arrow pointing to?
|
basal lamina = basement membrane
|
|
|
simple squamous - functions
|
exchange, lubrication and barrier
|
|
|
simple squamous - locations
|
blood vessels & lymphatics (endothelium)
endocardium body cavities (mesothelium) Bowman's capsule of renal glomerulus alveoli (lung) |
|
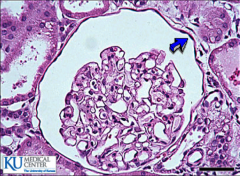
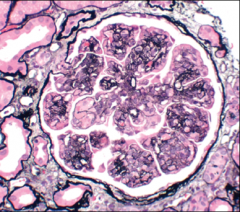
ID the cells indicated by the arrow
|
simple squamous (Bowman's capsule)
|
|
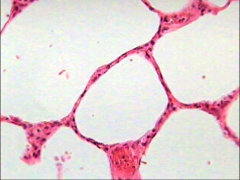
ID the epithelial cells
|
simple squamous (alveoli)
|
|
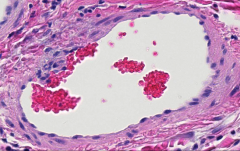
ID the epithelial cells; ID the tissue
|
simple squamous (blood vessel)
|
|
|
simple squamous - nuclei
|
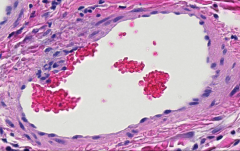
elongated and oriented in the direction of the cytoplasm
in blood vessels, the endothelial cells will orient longitudinally in the direction of the blood flow. a cross section of a vessel will also show a cross sectional cut of the nucleus (it will look round rather than cigar-shaped): will appear round and will protrude into the lumen |
|
|
simple cuboidal - functions
|
barrier, conduit
absorption secretion |
|
|
simple cuboidal - locations
|
small exocrine gland ducts
kidney tubules thyroid follicles surface of ovary |
|
|
simple cuboidal - nucleus
|
often oriented vertically in the cell
|
|
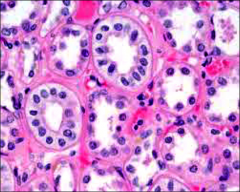
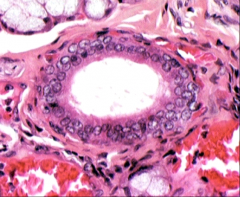
ID the epithelial cells (H&E)
|
simple cuboidal (renal tubules)
|
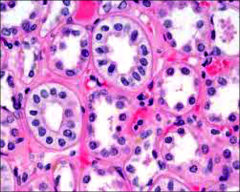
|
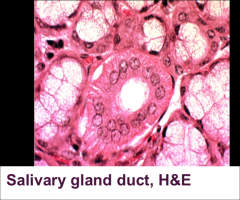
ID the epithelial cells (H&E)
|
simple cuboidal (salivary gland duct)
|
|
|
simple columnar - functions
|
absorption
secretion |
|
|
simple columnar - locations
|
small intestine
colon stomach lining & gastric glands gallbladder |
|
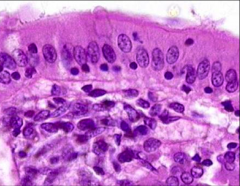
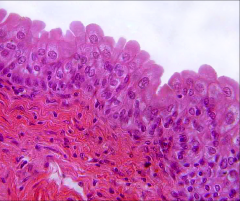
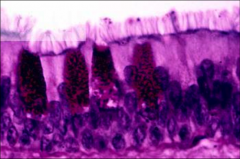
ID the epithelial cell (H&E)
|
simple columnar (mucosa of duodenum)
|
|
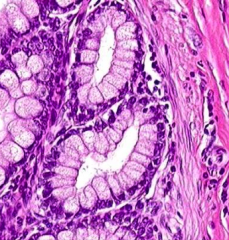
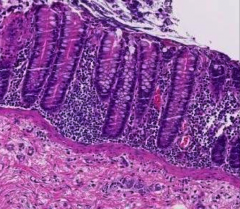
ID the epithelial cell (H&E)
|
simple columnar (gastric gland)
|
|
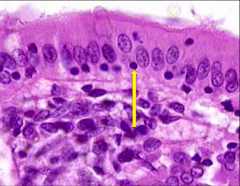
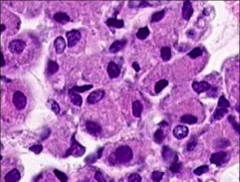
What is this cell (the smaller, dark spot)?
|
small lymphocytes that are moving toward the lumen: present as small, round dark nuclei scattered through this layer. They are scouting for any foreign invaders (immunosurveillance) that might try to breach the barrier and gain entrance into the body. They have heterochromatic nuclei because they have not yet been stimulated. It they encounter an invader, they have the capability to unravel their chromatin (becoming more euchromatic) and begin transcribing the relevant genes needed for a response to the threat.
|
|
|
stratified squamous - function
|
barrier, protection
|
|
|
stratified squamous - location
|
epidermis, Oral cavity, Esophagus, Vagina, Distal urethra
|
|
|
stratified squamous - structure
|
-consist of several distinct layers of cells
-shape and height of the cells vary from layer to layer -only the shape of the uppermost layer is used to classify the type of epithelium - may be cornified |
|
|
keratin
|
- key structural material making up the outer layer of skin, hair and nails
- Keratin monomers assemble into bundles to form tough, insoluble intermediate filaments - water resistant protein that forms a protective barrier against the destructive forces of the environment - found in straiefied squamous epithelial tissue |
|
|
keratinization of cells
|
-cells which have undergone keratinization have an abundant amt of keratin filaments in their keratinocytes in the cornified layer of their epidermis
-process of keratinization leads to cell death. -topmost layer of the epidermis is composed of many layers of dead, scalelike cells lacking nuclei that eventually slough off and are lost. |
|
|
stratified squamous epithelial cells in _____________ will NOT have the distinct keratin (cornified) layer
|
moist cavities; eg. the oral cavity
cell DO contain keratin but FEWER keratin intermediate filaments retain their nuclei |
|
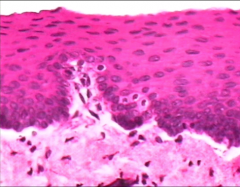
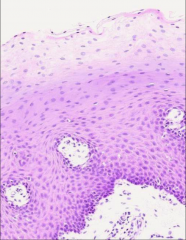
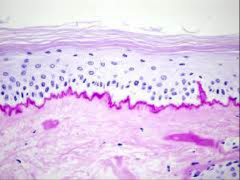
ID the epithelial cell (H&E) - be specific
|
tongue: "noncornified" stratified squamous
|
|
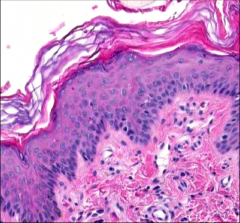
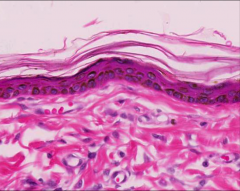
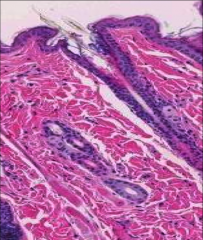
ID the epithelial cell (H&E) - be specific
|
skin: cornified stratified squamous
|
|
|
stratified cuboidal - functions
|
barrier
conduit |
|
|
stratified cuboidal - locations
|
-large ducts (sweat, salivary glands)
-junction btw pseudostratified columnar and stratified squamous (urethra, anorectal junction) - stratification isn't uniform from one place to another. -As the duct enlarges it becomes more likely that a section will show very clearly stratified epithelium |
|
ID the epithelial cell (H&E) - be specific
|
stratified cuboidal - salivary duct
|
|
|
stratified columnar - functions
|
protection, conduit, secretion
|
|
|
stratified columnar - locations
|
-large ducts of compound glands
- conjunctiva: thin membrane that covers the inner surface of the eyelid and the white part of the eyeball (the sclera) -transitional zones |
|
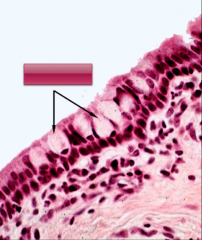
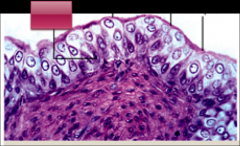
ID the epithelial cell (H&E) - (ignore the arrows & box)
|
conjunctival mucosa - stratified columnar
|
|
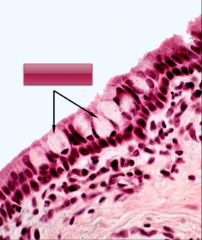
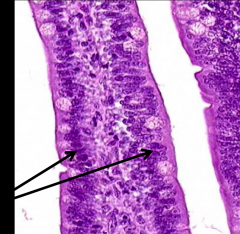
ID the structure indicated by the 2 arrows
|
goblet cells
|
|
|
pseudostratified epithelium
|
- single layer of cells (simple) siting along the basement membrane
- not all cells reach the free surface - look stratified -gives the impression of multiple cell layers |
|
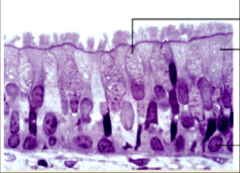
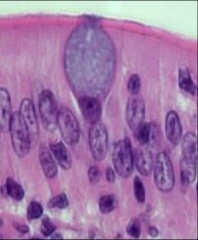
ID the 3 structures ID by the black markers
|
top to bottom: goblet cell, columnar ciliated cell, basal cell
|
|
|
pseudostratified epithelium - functions
|
secretion
absorption conduit |
|
|
pseudostratified epithelium - locations
|
tracheal, large bronchi, ductus deferens, efferent ductules of epididymis
|
|
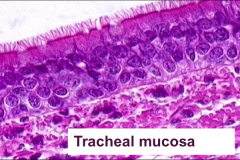
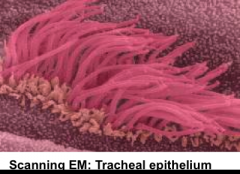
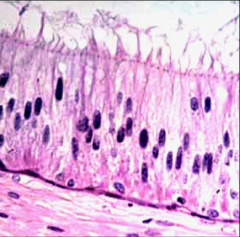
ID the epithelial cell (H&E) - be specific
|
tracheal mucosa - ciliated pseudostratified columnar epithelium
|
|
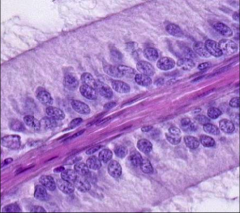
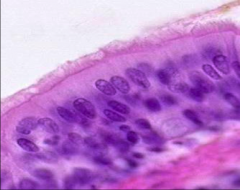
ID the epithelial cell (H&E) - be specific
|
ductules of epididymis - stereociliated pseudostratified columnar epithelium
|
|
|
to classify an epithelium you must always look for...
|
a region of the section showing the simplest, edge-on appearance
|
|
|
villus
|
finger like structure that projects into the intestinal lumen.
The structure has a core of connective tissue ensheathed on all sides by epithelium. |
|
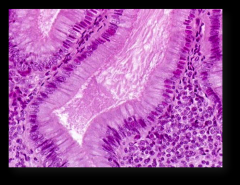
ID the epithelial cell (H&E); specify what the arrows are pointing to
|
- instestinal villus - simple columnar epithelium
Note how epithelium on the right side (arrow) looks pseudostratified due to angle of section - plane of section |
|
|
transitional epithelium
|
A.k.a. urothelium – lines lower urinary tract
Modifications to allow epithelium distension stratified epithelium composed of basal and dome-shaped cells Rounded surface of the apical cells is distinguishing characteristic - contracted the presence of a few binucleated cells along the surface may help to ID transitional cells |
|
|
characteristic appearance of a transitional upper layer cells - EMPTY bladder
|
appear to be cuboidal with a domed apex
|
|
|
characteristic appearance of a transitional upper layer cells - FULL bladder
|
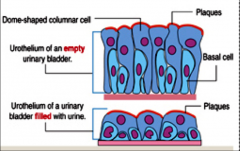
tissue actually compresses and the cells become stretched, and they appear to be flat, irregular, and squamous.
|
|
ID the epithelial cell; specify what the black lines are labeling; NOTE. the 2 lines on the R label the same cell type
|
transitional epithelium (urinary bladder)
L-> R Basal cell Dome-shaped columnar cell plaques: plaques of aggregated proteins are found on the apical plasma membrane of the columnar cells |
|
|
what 2 cell types make up transitional epithelium?
|
Basal cell: attach to the basal lamina
Dome-shaped columnar cell: extend from basal laminam to the lumen |
|
|
transitional epithelial cells - function
|
barrier
distensible property |
|
|
transitional epithelial cells - location
|
renal pelvis
ureters bladder proximal urethra |
|
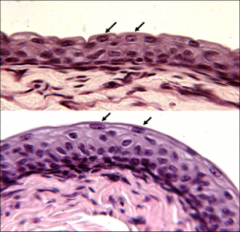
What type of epithelial tissue is this? What distinguishes top tissue from the bottom tissue? What does this mean?
|
- hard to ID transitional epithelium from stratified squamous or cuboidal wo knowing the tissue source
- things to look for: -- in relaxed bladder: uppermost layer cells will often have a dome-shaped (aka umbrella cells), bulging into bladder lumen -- presence of a few binucleated cells along the surface may help identify cells as transitional TOP: contracted bladder BOTTOM: distended bladder |
|
ID the epithelial cell (H&E) and explain how the ID is determined.
|
transitional epithelium:
- dome shaped umbrella cells in upper (luminal) layer positively ID transitional - CONTRACTED - if this tissue were to distend, upper layer would become squamous |
|
ID epithelial tissue (H&E)
|
simple columnar epithelium (gallbladder)
|
|
ID epithelial tissue (H&E)
|
cornified stratified squamous epithelium (skin)
|
|
ID epithelial tissue (H&E)
what is the white tissue in the lower right corner? what is the name for the darkest basophilic band bordering the white region? |
noncornified stratified squamous epithelium
white tissue = CT basophilic band = basement membrane |
|
|
types of apical domain modifications
|
cilia, primary cilia (monocilia), microvilli, stereocilia
|
|
|
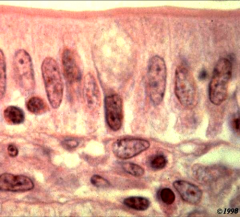
cilia - traits
|
short, fine, hair-like structures
microtubule core basal bodies anchor them protrusions of the cell's plasma motile - move in unison |
|
|
cilia - location
|
Mucociliary clearance in airways
Oviducts: Move ova & fluid toward uterus Sperm (flagellum) brain: move CSF |
|
|
basal body
|
modified centriole that gives rise to the cilia
anchors the base of each cilia and allows it to rotate or bend contains a foot that is always oriented in the drxn of the ciliar stroke |
|
ID apical domain modification
|
cilia
|
|
|
cilia structure
|
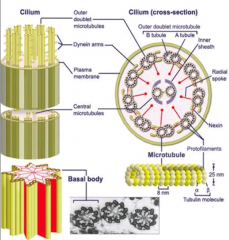
- 9 microtuble doublets ring around periphery of cilia
-- one of which is incomplete and shares portion of wall w the other microtubules -- doublets linked by nexin - 2 microtubles at the center of the microtubule -- radial spokes bind the outer doublets to the inner pair |
|
|
cilial doublets are linked by...
|
nexin
|
|
|
what binds the outer doublets to the inner pair in cilia?
|
radial spokes
|
|
|
what drives cilia movement
|
dynein motor proteins
|
|
|
explain the process by which dynein causes movement in cilia
|
sends “arms” out from each double, and forms temporary cross bridges with the adjacent microtubule.
uses ATP to move along surface of adjacent microtubule facilitates sliding of the microtubules against each other dependent on calcium. as the microtubules slide, the cilium eventually bends as the ends of the microtubules are anchored inside the cell by the basal body |
|
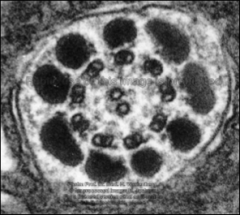
ID this structure
|
cilium cross section
|
|
|
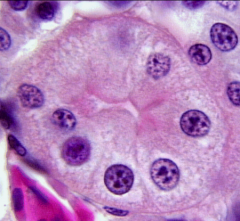
monocilia
|
aka primary cilia
nonmotile 9+0 arrangment: lack the central pair of microtubules; lack dynein |
|
|
what is a structural difference between monocilial and cilial and what does it result in?
|
monocilia lack motility, the central microtubule doublet, and motor proteins
|
|
|
which apical domain modification plays a role in the left hand anatomical arrangement of organs
|
monocilial
|
|
|
Nonmotile cilia are present in...
|
many types of mammalian cells
cells lining all part of the kidney found in sensory organs (eg. retina & nose) |
|
|
monocilia and the kidney
|
monocilia line all parts of the kidney and act as mechanoreceptors containing Ca++ channels
normal dev of thekidney depends on the ability of monocilia to detect fluid flow and initial Ca++ influx |
|
|
cell polarity properties are associated with...
|
the apical (modifications; directed towards the lumen, enclosed cavity or tube), lateral (cell-to-cell junctions) and basal (basement membranes) domains of a cell
depending on cell type, organelles may be positioned more toward 1 side of a cell |
|
|
defects in 2 genes that control development of the kidney monocilia have been linked to...
|
development of polycystic kidney disease in which cysts develop in the kidney, expanding and ultimately destroying the kidney parenchyma, leading to renal failure
|
|
|
cilium and rods/cones
|
of the vertebrate retina; possess a primary cilium equipped with an expanded tip called the outer segment, which is specialized for the reception and transduction of light.
|
|
|
nodal cilia
|
special 1o cilia; play a role in the L-R anatomic location of internal organs
unlike normal monocilia, CONTAIN motor proteins (dyneins or kinesins): CCW rotational movement gastrulation: nodal cilia in primitive node generates a leftward flow that is detected by the sensory receptors on the L side of the body --> different signaling mechanisms on the L side of the embryo compared to the right |
|
|
immotile or absent cilia during gastrulation ...?
|
development sensory changes do not occur --> random placement of internal organs
|
|

ID this structure
|
monocilia; aka nonmotile cilia; aka primary cilia
|
|
|
microvilli - overview
|
-present on most epithelial cells
-most numerous and best developed in gastrointestinal & renal epithelial cells -striated or brushed border appearance -may contain specific enzymes -- eg. in the gastrointestinal tract, Es resp for digestion of carbs are found in the microvilli |
|
ID this apical modification
|
brush border of intestinal mucosa
|
|
ID this tissue
|
renal tubule epithelial cells
|
|
|
microvilli - structure
|
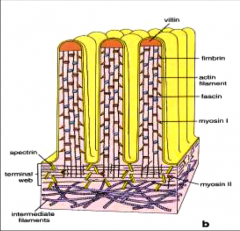
contain a core of actin filaments
- anchored to villin in tip - extend downward to apical cytoplasm and anchors to horizontal actin fibers in the terminal web -- stabilized by spectrin (anchors term web to apical cell membrane) - actin filaments cross-linked by actin bundling proteins: fascin and fimbin -- provides support and gives rigidity to microvilli - myosin I binds actin to plasma membrane of microvilli |
|
|
microvilli - contractile ability
|
-provided by myosin II, tropomysoin, calmodulin (Ca-binding molecule) in terminal web
-cause apex of cell to contract, making the microvilli spread apart, increasing the intermicrovillous space |
|
|
stereocilia - location
|
epididymis, proximal ductus deferens, sensory (hair) cells of the ear
|
|
|
stereocilia - overview
|
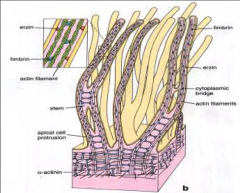
unusually long, immotile microvilli
structurally similar to microvilli except arise from an apical protrusion and have thick stem portions interconnected by cytoplasmic bridges -> makes them appear branched ID: aggregate into pointed bundles - look like hairs of a paint brush |
|

ID this apical modification
|
stereocilia
|
|
ID this apical modification
|
stereocilia
|
|
|
4 kinds of cell junctions
|
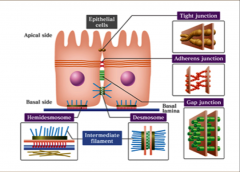
3 types on the lateral surface of the cell:
- occluding junctions - anchoring junctions - communicating junctions (gap junctions) 1 basal surface junction: -hemidesmosomes |
|
|
where junction is found exclusively on the basal surface?
|
hemidesmosomes
|
|
|
T/F: cell junctions are restricted to epithelial cells
|
FALSE: cell junctions can be found in all 4 major tissue groups (nervous, muscle, CT and epithelial)?
|
|
|
Cell adhesion molecules (CAMS)
|
mechanical stability and structural integrity:
- cell-to-cell & cell-to-ICM adhesion linked with IC filaments & actin that are part of cellular cytoskeleton major role in cell proliferation and migration. All stages of tissue differentiation that occurs during embryonic development is defined by the expression of specific CAMs on the cell surface. |
|
|
changes in the normal expression of 1 or more CAMs can lead to...
|
pathologic alteration during tissue differentiation or maturation
|
|
|
4 classifications of CAMs
|
cadherins, intergrins, selections, immunoglobulin superfamily
|
|
|
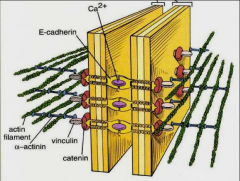
cadherins
|
Ca++ dependent CAMs located mainly in the zonula adherens
|
|
|
integrins
|
CAMs that interact w extracellular matrix molecules such as collagen
|
|
|
selectins
|
CAMs found on WBCs (leukocytes) and endothelial cells
|
|
|
immunoglobulin superfamily (IgSF)
|
glycoproteins w a wide variety of functions incudling cell adhesion, differentiation, angiogenesis (new blood vessel formation), microbial attachment, inflammation, neoplasia (formation of new tissue), and tumor metastasis
|
|
|
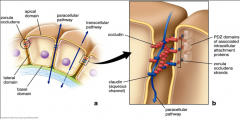
zonula occludens - function
|
aka tight (occluding) junctions
-located in apical region of the lateral surface of the cell -prevent the passage of molecules and ions through the space btw cells - ensures that materials must enter the cells to pass through the tissue -prevent the movement of integral membrane proteins btw the apical and basolateral surfaces of the cell - preserves the polarity of the cell's surfaces -particularly impo in epithelial cells that serve as a physiologic barrier |
|
|
zonula occluden - structure
|
-contain transmembrane proteins embedded in both plasma membranes that join each other
- junction is formed into a band that goes around entire apical perimeter -major cell adhesion molecules: claudins & occludins -CAMS bind actin & regulatory and signaling proteins called PDZ-domain proteins -tightness of junction depends on # of protein strands |
|
|
what are PDZ-domain proteins?
|
regulatory and signaling proteins involved in the structure and function of PDZ-domain proteins
|
|
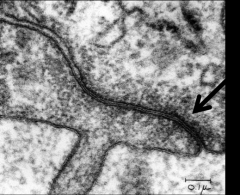
identify this structure
|
zonula occluden
|
|
|
tight epithelia
|
-contain tight junctions that prevent water and solute movement
-distal convoluted tubule -collecting duct part of the kidney |
|
|
leaky epithelia
|
-lack tight junctions or have less complex tight junctions
-tight junctions in kidney proximal tubule have only 2--3 junctional strans -> leaky |
|
|
zona adherens
|
- anchoring junctions btw cells to guard against physical disruption of the barrier
-- E-cadherin binds cells -- require Ca++ -junction forms a band that completely encircles that apical perimeter of the cell - req'd by tissues needing a strong attachment: skin, cardiac -- typically contain numerous anchoring jnxns btw cells -cell membranes will be separated by regular extracellular space -cytoplasmic face is linked to the actin cytoskeleton (terminal web) - 3 types |
|
|
term: zonula, in reference to junctions
|
means that the junction completely encircles the region/face of the cell on which it is attached
- eg. zonula adheren and occluden: band completely encircles the apical perimeter |
|
ID the prominent structure
|
zonula adheren; anchoring junction
|
|
|
3 types of zonla adherens
|
zonula adherens - belt desmosome
fascia adheren macula adherens or desmosome |
|
|
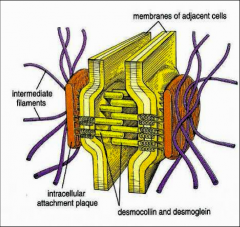
demosome
|
aka macula adherens
-impo in epithilial that acts as physical barrier: skin, cardiac -anchoring jnxn btw cells - cytoplasmic side of plasma mem: demosomal attachment plaque (disc-shaped dense structure) --made from demoplakins and plakoglobins -- anchors intermediate filaments (loop through plaque and extend back into cyto) -ECM-side of plasma: transmembrane glycoproteins hold adjacent cells together: desmoglein & desmocollin -- extend through intercell space and bind to glycoprotein on adjacent cell -- (Ca-dependent) cadherin CAMs |
|
|
intercellular bridges
|
-demosomal attachments btw stratified squamous cells of the skin
- preparation of skin tissue w formalin causes epithelial cells to shrink and pull apart; where demosomes are present, the cells remain in contact -RESULT: lines between squamous cells = intercellular bridges |
|
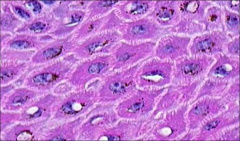
ID the intercellular structure
|
intercellular bridges = desmosome
|
|
|
desmoglein 1
|
Ca-binding transmembrane glycoprotein component of desmosomes in vertebrate epithelial cells
|
|
|
pemphigus foliaceus & pemphigus vulgarus
|
autoimmune diseases that target the desmoglein proteins (3 and 1, respectively) causing disruption to the desmosome-keratin filament complex leading to a breakdown in cell adhesion
-symptoms: pustular eruptions w hair loss and crust |
|
|
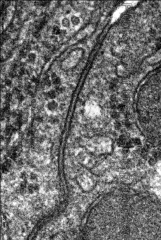
junctional complex
|
epithelia of most glands and cavitary organs have a characteristic tripartite junctional complex found between adjacent cells where apical margins touch:
- zonula occluden jnxns: water-tight seal around the apex of the columnar epithelial cells - zonula adjerens jnxns: attaches adjacent cells firmly together -(often) a number of desmosomes btw zonula adherens VISUALIZE: terminal bar: dark line near (and parallel to) the apical membrane of the cells |
|
ID this structure
|
junctional complex = terminal bar
intestine: terminal bar is just below the brush border |
|

ID the structure that encompasses this enter intercellular area
|
junctional complex
ZA: zonula adherens D1 & D2: desmosomes TW: terminal web actin filaments insert into the SA and intermediate filaments (IF) insert into the desmosome |
|
|
hemidesmosomes
|
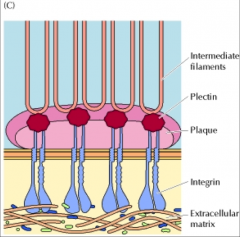
variant of desmosome
- desmosomal plaque w desmoplakin-like protein - CAM = integrin class of matrix receptor provides stable connection between cell and CT (compare cell-to-cell w desmosome) most common in tissue subject to abrasion and mechanical shearing: - oral cavity & esophagus - cornea - skin |
|
|
gap junctions
|
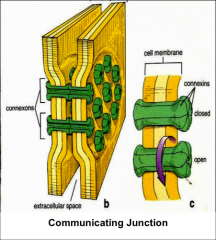
aka communicating junctions
- grp of transmembrane pores -- connexins form communicating channels -- undergo reversible conformational changes that open/close their pore --- "close" = Ca - mediate the diffusion of small signaling molecules btw cells - coordinate activity btw adjacent cells: -- cardiac m -- smooth m -- tubular epithelial c |
|
ID the structure indicated
|
communicating jnxn = gap jnxn
|
|
|
basement membrane - composition
|
collagen (depending on the cell: type IV, III, VII, XVII), fibronectin, laminins, proteoglycans (esp heparin sulfate)
|
|
|
basement membrane - overview
|
anchors the basal surfaces of epithelial cells to the underlying CT
found in epithelial cells, muscle cells, peripheral nerves, and adipose tissue aka basal lamina |
|
|
basement membrane - functions
|
-anchors epithilieum/endothelium to underlying CT
-filtration -guide for call adhesion and migration -regulation and signaling |
|
|
laminins
|
-lg trimeric proteins w a, B, gamma chain
-part of the basement layer -influence cell differentiation, migration and adhesion |
|
|
fibronectin
|
glycoprotein that exists as a dimer
binds to EXM components, such as collagen, and to grp of membrane spanning receptor proteins called integrins -binding helps it to play a role in cell adhesion and migration |
|
|
reticulofibers
|
aka reticulin
a type of fiber composed of type III collage |
|
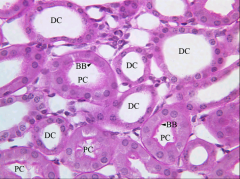
ID the various structures (H&E)
|
DC: distal convoluted tubule
PC: proximal convoluted tubule BB: brush border basement membrane is hard to visualize |
|
|
visualizing the basement membrane
|
not readily seen in H&E
better visualized w PAS (magenta) and silver stain (black) |
|
ID the magenta layer
|
PAS stain; basement membrane
renal tubules |
|
ID the black ring
|
silver stain; basement membrane
renal tubules |
|
|
basement membrane - location
|
epithelia
smooth, cardiac, skeletal m cells adipocytes neurolemmocytes = Schwann cells |
|
|
2 types of glands
|
exocrine and endocrine
|
|
|
exocrine glands
|
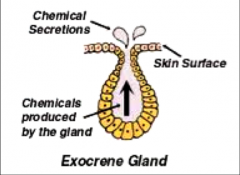
secrete via ducts opening to a surface
|
|
|
endocrine glands
|
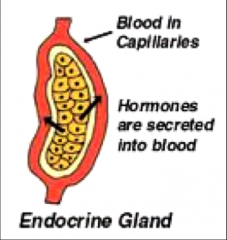
secrete into surrounding blood vessels
|
|
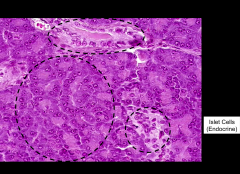
Starting at the top and working CW, ID the tissue types/structures within the 4 dashed circles
|
Top: exocrine duct
lower R: islet cells (endocrine) lower L: exocrine cells |
|
|
types of secretion
|
serous & mucinous
|
|
|
serous secretion
|
-thin, watery secretion
-glands have pink secretory granules in apical salivary gland eg. pancreas, parotid salivary gland |
|
|
mucinous secretion
|
thick, viscous secretion
mucin stains light blue nuclei flattened against basal part of cell |
|
|
mucins
|
-family of high MW, heavily glycosylated proteins produced by epithelial tissues
-mucins' key characteristic is their ability to form gels -key componeny in most gel-like secretions -functions: lubrication, cell signaling, chemical barriers VISUALIZE: PAS stains carbs magenta, including glycoproteins that make up mucin |
|
what secretory gland is this (based on secretion types)
|
parotid gland - serous secretion
|
|
what secretory gland is this (based on secretion types)
|
mandibular salivary gland - mucinous secretion
|
|
|
goblet cells
|
-only unicellular gland in the mammalian body
- contain mucin in a protective function locations: nasal turbinate epithelium, salivary glands, gastric mucosa, colon |
|
|
gland classification based on structure
|
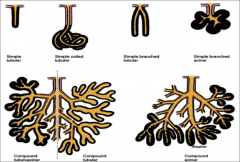
simple vs compound
|
|
|
simple gland
|
-gland classification based on structure
-cluster of secretory cells that connect to unbranched duct simple tubular, coiled tubular, branched tubular, branched acinar |
|
|
compound gland
|
-gland classification based on structure
-branching system of ducts w multiple secretory units surrounded by CT capsule that sends partitions inside the gland to organize it into large units called lobes --lobes are further subdivided into lobules -parenchyma can be divided into aggregates of secretory units: lobes, lobules, acini -compound tubuloacinar, tubular, acinar |
|
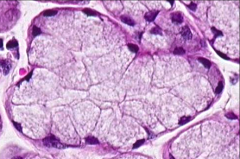
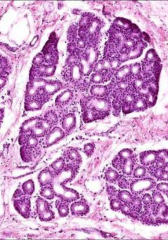
ID this structure (H&E)
|
goblet cell
|
|
ID this structure (PAS)
|
goblet cell
|
|
|
tubular gland
|
has a tube-shaped secretory portion;
secretory portion may be straight, branched or coiled; wall of the tubule are parallel w relatively wide lumens |
|
|
acinar
|
aka alveolar
has a globe-shaped secretory portion w a small lumen secretory portion may be single or branched |
|
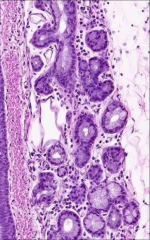
ID this structure and tissue type
|
simple tubular
large intestine |
|
ID this structure and tissue
|
simple coiled tubular
sweat gland |
|
ID this structure and tissue
|
compound tubular
brunners glands, duodenum |
|
ID this structure and tissue
|
compound tubuloacinar
tracheal glands |
|
|
gland classification based on secretion
|

eg. exocrine pancreas - merocrine secretion
apocrine gland & mammary gland - apocrine secretion sebaceous gland - holocrine secretion paracrine gland - type of hormone function in which hormone synthesized in and released from endocrine cells and binds to its receptor in nearby cells (rather then entering the blood stream), affecting their function |
|
|
merocinre secretion
|
secretory prod is delivered in membrane-bound vesicles to the apical region of the cell where they fuse and release their content by exocytosis
eg. pancreatic acinar cells |
|
|
apocrine secretion
|
secretory prod is released at the apical region of the cell surrounded by a thin layer of cytoplasm surrounded by a protion of the cell membrane
eg. mammary glands, ceruminous glands of the ear canal |
|
|
holocrine secretion
|
secretory product accumulates wi the cell which undergoes apoptosis
both secretory product and remains of the dead cell are discharged into the lumen of the gland |
|
|
paracrine secretion
|
type of hormone function in which hormone synthesized in and released from endocrine cells and binds to its receptor in nearby cells (rather then entering the blood stream), affecting their function
|

